Introduction
Cancer of the uterine cervix is the third most
common gynecological cancer type and a cause of cancer-associated
mortality in females worldwide (1).
The treatment of locally advanced uterine cervical cancer includes
concomitant chemoradiotherapy and intracavitary brachytherapy as
the definitive treatment. Cervical cancer consists of a several
histopathological types, of which the most common type is squamous
cell carcinoma (SQCC). The incidence of invasive uterine cervical
adenocarcinoma (AC) and its variants has increased over the last
few decades (1–3), and it has been demonstrated to be
associated with poor prognosis. Possible explanations for the
growing incidence are obesity and estrogen exposure (2). However, the majority of the current
knowledge with regard to the treatment of cervical cancer has been
established through studies in which the majority of patients
suffered from SQCC. Only a limited number of studies have focused
on the treatment of cervical AC; therefore, the present
understanding regarding the optimal treatment of uterine cervical
AC is limited. The aim of the present study was to investigate the
response of advanced cervical AC to definitive chemoradiotherapy in
comparison to that of cervical SQCC.
Patients and methods
Patients
A retrospective study was conducted using the
medical records of consecutive patients with AC of the uterine
cervix who had been treated at a single tertiary center (Rambam
Health Care Campus, Haifa, Israel) between 1998 and 2013. No
inclusion/exclusion criteria was used, and all patients were
included. The patients had received concomitant external beam
radiotherapy (EBRT) combined with weekly chemotherapy and
intracavitary high-dose rate (HDR) brachytherapy. All the patients
were treated with curative intent. In addition, the data of 39
patients with SQCC of the uterine cervix were also reviewed. As
there were more patients with SQCC, the data of every third patient
was collected, to avoid a bias. Medical records were reviewed to
obtain information regarding disease stage, radiotherapy doses,
response, time to recurrence and survival. Overall survival data
were available for all the patients and were based on the results
of the population census as recorded in the population registry of
the Ministry of Interior of Israel. The study was approved by the
ethics committee of Rambam Medical Center, Haifa, Israel.
Statistical analysis
The Kolmogorov-Smirnov test was used to test for
normality of the distribution, and according to the results a
parametric and non-parametric models were used. The differences
between the two histology groups for continuous parameters (such as
age) were evaluated by t-test or Mann-Whitney U test.
Categorical parameters were evaluated by Fisher exact test or the
Pearson χ2 test. Overall survival was defined as the
time from the first day of treatment to mortality (all causes).
Survivors were censored at the last follow-up. Time to tumor
progression was defined as the time from the first day of treatment
to the first recorded evidence of progression. Alive patients
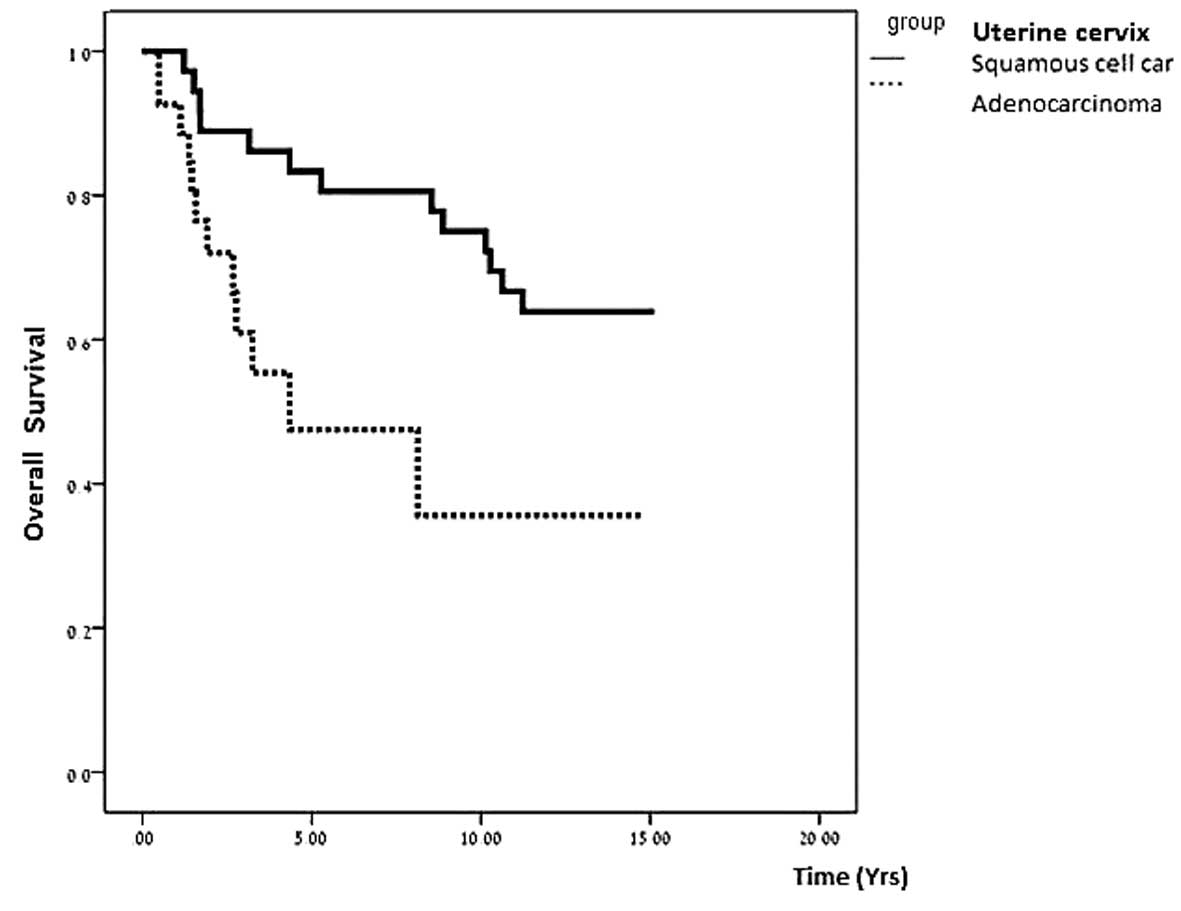
without progression were censored at last follow-up. Kaplan-Maier
curves were used to illustrate main results. Two-tailed P<0.05
was considered to indicate a statistically significant difference.
Statistical analyses was performed using SPSS (Statistics Products
Solutions Services) 21.0 software for Windows (IBM SPSS; Armonk,
NY, USA).
Results
Patient characteristics
A total of 68 patients were included in the present
study, including 29 patients with cervical AC and 39 patients with
cervical SQCC. The median follow-up period was 10 years (range,
0.5–15 years). The majority of patients were of Jewish descent
(89.7% in the SQCC group and 72.4% in the AC group). The disease
stages and treatment of patients in the two groups are summarized
in Table I. The rate of bulky disease
(>4 cm) was similar between the groups.
 | Table I.Clinical characteristics of
patients. |
Table I.
Clinical characteristics of
patients.
| Characteristic | SQCC | AC | P-value |
|---|
| Patients, n | 39 | 29 |
|
| Jewish decent, n
(%) | 35 (89.7) | 21 (72.4) | 0.11 |
| BMI, n (%) |
|
| 0.09 |
| ≤25
kg/m2 | 10 (62.5) | 6 (30.0) |
|
| >25
kg/m2 | 6 (37.5) | 14 (70.0) |
|
| BMIa | 26.05±6.3 (23.5) | 30.31±6.1 (32.0) | 0.05 |
| Age at diagnosis,
yearsa | 54.4±13.36
(52.5) | 54.34±13.07
(54.0) | 0.98 |
| Histological grade, n
(%) |
|
|
|
| 1 | 0 (0.0) | 9 (32.0) | 0.006 |
| 2 | 13 (43.0) | 11 (39.0) | 0.79 |
| 3 | 17 (57.0) | 8 (29.0) | 0.037 |
| FIGO stage, n
(%) |
|
|
|
| I | 12 (31.0) | 12 (43.0) | 0.37 |
| II | 24 (62.0) | 11 (39.0) | 0.09 |
| III | 3 (8.0) | 4 (14.0) | 0.42 |
| IV | 0 (0.0) | 1 (4.0) | 0.15 |
| Treatment, n |
|
|
|
|
Brachytherapy | 0 | 1 | 0.15 |
|
Chemoradiotherapy (EBRT +
brachytherapy) | 38 | 23 | 0.014 |
| EBRT +
brachytherapy only | 1 | 5 | 0.09 |
Treatment strategies
For all the patients, EBRT was performed prior to
HDR brachytherapy. Cisplatin (40 mg/m2) was used
concomitantly with pelvic irradiation in all patients, with the
exception of two patients in the SQCC group, for whom carboplatin
was used (area under the curve, 2) due to renal insufficiency. In
addition, concomitant chemotherapy was not administered to one
patient in the SQCC group and 5 in the AC group due to
comorbidities (Table I). Furthermore,
three patients in each group did not receive the planned
chemotherapy cycles due to acute gastrointestinal toxicity
(diarrhea), which was the main indication to discontinue
chemotherapy.
The intended treatment included external
radiotherapy to the pelvis, at a dose of 45–50.4 Gy (25–28
fractions, 1.8 Gy per fraction, five fractions per week) using 6 MV
or 18 MV beams, according to the protocol of the Division of
Oncology, Rambam Health Care Campus. Depending on the patient's
body habitus, two opposing (anterior-posterior) fields (for the
majority of patients) or the 4-fields box technique (for those with
a larger body habitus) were used. Patients with parametrium
involvement were given a 5.4 Gy (1.8 Gy per fraction) boost with a
central block in the vagina and uterine-cervical area. The average
EBRT dose administered did not differ significantly between the
groups (4914 cGY vs. 5055 cGY for the AC and SQCC groups,
respectively; P=0.19). HDR brachytherapy was performed using an
Ir192 source. Prior to the first HDR brachytherapy
fraction, the patients underwent intrauterine stent insertion and
evaluation for response under anesthesia. The HDR fractionation
scheme was planned for five fractions of 5–5.5 Gy each (depending
on clinical evaluation of tumor size). Treatment doses were
prescribed at point A. HDR doses did not differ between the two
groups.
In total, nine cervical AC patients required surgery
following chemoradiotherapy due to residual disease, compared with
two patients in the SQCC group (31% vs. 5%, respectively;
P=0.0065). No statistically significant difference in mortality
rate was observed between the two subgroups (36% vs. 44% for AC and
SQCC groups, respectively; P=0.61). The median follow-up period was
10 years, revealing that patients with cervical AC presented a
reduced overall survival (7.4 years in the cervical AC group, vs.
11 years in the cervical SQCC group; P=0.01). Furthermore, the
differences in recurrence rate (40.7% vs. 34.4%; P=0.79) and
disease-free interval (1.2 years vs. 2 years; P=0.11) were not
statistically significant. However, significant differences were
observed in overall survival between the two groups (Fig. 1). The majority of recurrences in the
two groups were distant; four patients in the AC group exhibited
local recurrence (within the irradiated field), and five patients
exhibited distant recurrences (outside the irradiated field,
including the lung, skeleton and liver), which was similar to that
exhibited by patients of the SQCC group, where five patients
exhibited local recurrence and six patients exhibited distant
recurrences. Furthermore, a higher number of AC patients required
surgical treatment for residual disease when compared with SQCC
patients. These results indicate that cervical AC is less
responsive to chemoradiotherapy than SQCC.
Discussion
The overall survival of patients with uterine
cervical AC has been previously described to be poorer compared
with that of SQCC patients, in studies conducted over the last two
decades ago (1,3). However, the management of these patients
did not change, which may be attributed to the rarity of the
disease and the lack of randomized trials. However, the incidence
of invasive uterine cervical AC and its variants has increased over
the last decades (2). Possible
explanations for the growing incidence include obesity and estrogen
exposure (4). In the present study,
no statistically significant differences were observed between the
AC and SQCC groups with regards to BMI (below or above 25
kg/m2), with 70% of patients in the AC group having a
BMI of >25 kg/m2, compared with 37.5% in the SQCC
group.
The growing incidence and aggressiveness of AC of
the uterine cervix, irrespective of the primary treatment (2,4,6), requires the re-evaluation of treatment
options for these patients. In the present study, more patients in
the cervical AC group required surgery following chemoradiotherapy
due to residual disease. The patients who were treated by
chemoradiotherapy did not differ with regard to tumor size (bulky
vs. non-bulky disease) or radiation dose between the SQCC and AC
groups. Thus, the lack of response was likely to be due to the
histological features of the tumor rather than the treatment. In
contrast to the study by Eifel et al (2), which reported a trend towards improved
survival in patients undergoing adjuvant hysterectomy (78% vs.
71%), no statistically significant differences in survival were
observed in the present study (P=0.09). Additionally, surgery
conferred no survival advantage in the present study. This may be
due to the fact that surgery was performed as a treatment for
unresponsive disease, rather than true adjuvant treatment.
Although the present study used a small sample size
and was conducted retrospectively, its results support those of
previous studies. Due to the growth in the prevalence of this
disease, further investigation into treatment options is required
(7); this may include the use of
alternative chemotherapy regimens, such as the combined use of
carboplatin and paclitaxel has been demonstrated to have
radiosensitizing properties in various types of adenocarcinoma
(8) and is a treatment strategy that
is commonly used for uterine AC.
Lee et al (9)
evaluated this regimen in the context of pelvic radiotherapy in
patients with SQCC of the uterine cervix. The study included 33
patients, who were treated with concurrent chemoradiotherapy,
including two cycles of paclitaxel (135 mg/m2) and
carboplatin (area under the time-concentration curve, 4.5 mg ×
min/ml) at four-week intervals. All the patients received EBRT at a
dose of 41.4–51.4 Gy (median, 50.4 Gy) to the entire pelvic area.
Boost irradiation was administered to the cervix in 28 patients by
brachytherapy at a dose of 25.6–43.3 Gy (median, 34.6 Gy) and in 5
patients by external beam radiotherapy at a dose of 10.8–14.4 Gy
(median, 14.4 Gy). The authors concluded that concurrent
chemoradiotherapy with paclitaxel and carboplatin is effective to
achieve pelvic control; however, the rate of toxicity was higher
compared with that reported for platinum only (9). Acute hematological toxicity of grade 3
or 4 was reported in ≤61% of the patients (9). With current advances in EBRT treatment
planning and the potential to perform intensity modulation planning
(IMRT), it may be possible to reduce doses to the iliac crest in
order to reduce hematologic toxicity (10). However, the use of IMRT in the
treatment of intact uterine cervical cancer is not the standard of
care. This may be due to the increased prevalence of the disease in
developing countries and to pelvic organ movement and tumor
regression, which increase the set-up variability when compared
with other diseases, thus requiring larger margins and possible
re-planning during the course of treatment. Therefore, data is
available with regard to the use of IMRT as part of definitive
chemoradiotherapy in uterine cervical cancer (11).
In conclusion, the current study shows that a higher
number of AC patients required surgery following chemoradiotherapy
due to a lack of response to the initial treatment and at a median
follow up period of 10 years, patients with AC exhibited shorter
overall survival. Based on the results of the present study,
further multicenter prospective trials are required for the
improvement of treatment in patients with uterine cervical AC.
Advances in radiotherapy treatment planning and recent progress in
chemotherapy regimens combined with radiotherapy in adenocarcinomas
occurring at various sites may provide new opportunities for the
investigation of novel effective treatments.
Acknowledgements
The authors would like to thank Mrs. Ronit Leiba
(Rambam Health Care Campus) for the assistance in statistical
analysis.
References
|
1
|
Fujiwara K, Monk B and
Devouassoux-Shisheboran M: Adenocarcinoma of the uterine cervix:
why is it different? Curr Oncol Rep. 16:4162014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Eifel PJ, Burke TW, Morris M and Smith TL:
Adenocarcinoma as an independent risk factor for disease recurrence
in patients with stage IB cervical carcinoma. Gynecol Oncol.
59:38–44. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Smith HO, Tiffany MF, Qualls CR and Key
CR: The rising incidence of adenocarcinoma relative to squamous
cell carcinoma of the uterine cervix in the United States - a
24-year population-based study. Gynecol Oncol. 78:97–105. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen JL, Huang CY, Huang YS, et al:
Differential clinical characteristics, treatment response and
prognosis of locally advanced adenocarcinoma/adenosquamous
carcinoma and squamous cell carcinoma of cervix treated with
definitive radiotherapy. Acta Obstet Gynecol Scand. 93:661–668.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lacey JV Jr, Swanson CA, Brinton LA, et
al: Obesity as a potential risk factor for adenocarcinomas and
squamous cell carcinomas of the uterine cervix. Cancer. 98:814–821.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Huang YT, Wang CC, Tsai CS, et al:
Clinical behaviors and outcomes for adenocarcinoma or adenosquamous
carcinoma of cervix treated by radical hysterectomy and adjuvant
radiotherapy or chemoradiotherapy. Int J Radiat Oncol Biol Phys.
84:420–427. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wakatsuki M, Kato S, Ohno T, et al:
Working Group of the Gynecological Tumor: Clinical outcomes of
carbon ion radiotherapy for locally advanced adenocarcinoma of the
uterine cervix in phase 1/2 clinical trial (protocol 9704). Cancer.
120:1663–1669. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee MY, Wu HG, Kim K, Ha SW, Kim JS, Kim
IA and Lee HP: Concurrent radiotherapy with paclitaxel/carboplatin
chemotherapy as a definitive treatment for squamous cell carcinoma
of the uterine cervix. Gynecol Oncol. 104:95–99. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
van Hagen P, Hulshof MC, van Lanschot JJ,
Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al: CROSS
Group: Preoperative chemoradiotherapy for esophageal or junctional
cancer. N Engl J Med. 366:2074–2084. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Menkarios C, Azria D, Laliberté B,
Moscardo CL, Gourgou S, Lemanski C, et al: Optimal organ-sparing
intensity-modulated radiation therapy (IMRT) regimen for the
treatment of locally advanced anal canal carcinoma: a comparison of
conventional and IMRT plans. Radiat Oncol. 2:412007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goldie SJ, Gaffikin L, Goldhaber-Fiebert
JD, et al: Alliance for Cervical Cancer Prevention Cost Working
Group: Cost-effectiveness of cervical-cancer screening in five
developing countries. N Engl J Med. 353:2158–2168. 2005. View Article : Google Scholar : PubMed/NCBI
|