Introduction
Intrahepatic cholangiocarcinomas (ICCs) are the
second most common primary liver malignancy, and they arise from
bile duct epithelium within the liver. While 90% of primary liver
cancers are hepatocellular carcinomas (HCCs), ICC cases account for
the remaining 5–10% (1,2). ICCs are relatively rare malignancies
with an age-adjusted incidence rate of 461 per 100,000 individuals
reported between 1973 and 2007, as per a recent SEER (Surveillance,
Epidemiology and End Results) report (2). While the incidence and mortality of
the more common malignancies such as colon, breast and lung are
reported to be on a decline nationwide, the incidence of ICC has
been on the rise (3–5). In a study based on the SEER database,
the incidence and mortality rates of ICC have markedly increased
between 1973 and 1997, with an estimated annual percent change
(EAPC) of 9.11 and 9.44%, respectively (4).
ICC usually presents sporadically as a discrete
intrahepatic mass in patients over 65 years of age (6). These tumors are lethal malignancies
with a median survival of 6.5 months from the time of diagnosis, in
untreated patients (7). The main
risk factor for ICC is primary sclerosing cholangitis (PSC). Recent
studies have reported a few additional risk factors including HIV
infection, smoking, diabetes, cirrhosis and hepatitis C (HCV)
infection (5,8–10). The
association between HCV and ICC has gained special attention since
the incidences of both are on the rise. A cohort study of a large
group of US veterans suggested that HCV infection conferred a
>2-fold rise in the risk of ICC (11). However, regardless of etiology,
surgical resection offers the only prospect of cure. Yet, only a
small percentage of patients with ICC are resectable at the time of
diagnosis. For patients with unresectable disease, palliative
chemoradiotherapy or palliative ablation/chemoembolization are the
major options.
Given the rising incidence of ICC, its poor
prognosis and lack of adequate treatment options, further studies
clarifying its risk factors, outcomes and prognostic factors are
warranted. Most of the existing studies in the US are on surgical
patients, and they usually span over a period of decades since this
is a rare tumor. A number of questions remain regarding the
pathogenesis, criteria for resectability, appropriate adjuvant
therapy and palliative therapy. Hence, we conducted a 10-year
retrospective study of all patients with ICC treated between 2000
and 2009 at a single institution to evaluate the outcome of various
treatments and to assess prognostic factors.
Patients and methods
The present study was conducted after obtaining
approval from the University of Florida Institutional Review Board.
Patients diagnosed with ICC who underwent treatment at our
institution between 2000 and 2009 were included in our study group.
The following data were collected for all patients: age, gender,
race, date of diagnosis, presenting complaint, liver function tests
at diagnosis, CA 19–9 and CEA levels, stage at diagnosis, presence
of metastases, resectability of tumor, date of surgery, pathologic
characteristics of tumor, chemotherapy or radiotherapy, recurrence
date and site, and date and cause of death.
At the time of diagnosis the tumor stage was
assessed by abdominal computed tomography (CT) or abdominal
magnetic resonance imaging (MRI) with cholangiopancreatography
(MRCP). Preoperative evaluation of vascular involvement was carried
out with CT/MRI to determine resectability. In appropriate
patients, the tumor was staged by an exploratory laparotomy with
intra-operative ultrasound and biopsy. Pre-operative assessment was
also performed for extrahepatic primary tumors and metastatic
disease. The American Joint Committee on Cancer
(AJCC)/International Union Against Cancer (UICC) staging system
(7th edition) TNM classification was used for staging the resected
tumors in patients who underwent surgery (12).
The treatment modality that each patient received
was determined by a multidisciplinary tumor board. Patients did not
undergo curative resection if they had metastatic disease at
diagnosis, or extensive local vascular invasion or multiple medical
comorbidities making them poor surgical candidates. In patients who
did not have any of the above, macroscopic curative resection was
carried out. Hepatic resection was the main surgery performed, and
its extent depended on the segments involved by the tumor.
Extrahepatic bile duct resection with Roux-en-Y reconstruction was
carried out in patients with bile duct invasion or lymph node
metastases. All patients undergoing surgery underwent assessment of
lymph node status unless intraperitoneal spread or clear
unresectability was identified prior to lymph node assessment.
Lymph node dissection included the hepatoduodenal ligament and the
porta hepatis. Patients with nodal positivity or positive resection
margins were considered to be at high risk for recurrence and were
offered adjuvant chemo/radiotherapy. Patients with unresectable
tumors were treated with palliative chemotherapy or radiotherapy or
transarterial chemoembolization. Some patients declined these
treatments and received best supportive care.
Pathologic examination was carried out on all
resected tumors. They were examined for tumor size and number,
histologic differentiation, and the presence of vascular and
perineural invasion. In situations where nodes were dissected, they
were examined for the presence of tumor. Surgical margins were
examined for the presence of residual tumor. Surrounding liver
parenchyma was examined for the presence of changes suggestive of
PSC or cirrhosis or other predisposing factors.
After diagnosis, all patients were followed up
closely in the clinic. Patients who underwent resection receive
regular clinical follow-up along with blood draw for blood
chemistry, liver function tests, CA 19-9 level and were screened
for recurrence at 6 monthly intervals with CT scans of the chest,
abdomen and pelvis.
Study objectives aimed to determine the risk
factors, clinical features, treatment outcome and prognostic
factors for survival in patients with ICC.
Statistical significance of the difference between
the means of quantitative variables was tested using the
independent t-test, and the Chi-square test was used for comparing
categorical variables. A P-value of 0.05 was held as significant.
The Kaplan-Meier method was used to estimate survival, and the
duration of survival was derived from the survival curves. Survival
of patients in the study group was calculated from the time of
diagnosis. Survival curves were compared using the log-rank test.
Multivariate analysis was performed using Cox proportional hazards
method with backward Wald. Only factors found to be significant on
univariate analysis were included in the regression mode, l and a
P-value of 0.10 was used to determine if the variable was to be
included in the next step.
Results
Of the 314 patients diagnosed with
cholangiocarcinoma during the study period, 105 (33.4%) had
intrahepatic tumors. Table I
describes the demographic and clinical features of the patients in
the study group. An equal percentage of the genders was present
(male 50.5%). The majority of patients were older than 40 years
(63.8%) and Caucasian (88.6%). The most common presenting complaint
was abdominal pain (34.3%), and in a similar percentage of patients
the tumor was found incidentally on imaging (30.5%). The tumors
arose de novo in 82.9% patients without underlying
hepatobiliary disease (87/105). Only a minority of the patients had
underlying cirrhosis (9.5%) and PSC/UC (6.7%). A majority of
patients presented with a solitary tumor (73.3%). The mean tumor
size was 5.9 cm (range 1.8–15.0)
 | Table IDemographic and clinical
characteristics of the study group. |
Table I
Demographic and clinical
characteristics of the study group.
| Variables | n (%) |
|---|
| Age (years) | |
| <59 | 38 (36.20) |
| ≥60 | 67 (63.80) |
| Gender | |
| Male | 53 (50.50) |
| Female | 52 (49.50) |
| Ethnicity | |
| Caucasian | 93 (88.60) |
|
African-American | 6 (5.70) |
| Other | 6 (5.70) |
| Presenting
complaint | |
| Abdominal pain | 36 (34.30) |
| Incidental | 32 (30.50) |
| Painless
jaundice | 19 (18.10) |
| Abnormal LFT | 7 (6.70) |
| Weight loss | 5 (4.80) |
| Pain + jaundice | 3 (92.90) |
| High CA 19-9 | 1 (1.00) |
| Metastatic
disease | 1 (1.00) |
| Risk factor | |
| None | 87 (82.90) |
| UC + PSC | 4 (3.90) |
| UC | 2 (1.90) |
| Hep C | 8 (7.60) |
| Cirrhosis (non-Hep
C) | 2 (1.90) |
| PBC | 1 (1.00) |
| Stage at
diagnosis | |
| I | 11 (10.50) |
| II | 23 (21.90) |
| III | 47 (44.80) |
| IV | 24 (22.90) |
| Tumor focality | |
| Unifocal | 77 (73.30) |
| Multifocal | 18 (17.10) |
| Presence of
metastases at diagnosis | |
| No | 80 (77.10) |
| Yes | 24 (22.90) |
| Site of
metastases | |
| Lung | 8 (7.60) |
| Peritoneum | 8 (7.60) |
| Liver | 4 (3.80) |
| Bone | 2 (1.90) |
| Other | 2 (1.90) |
| Surgery | |
| Curative
surgery | 53 (50.50) |
| Palliative
surgery/staging surgery | 12 (11.40) |
| No surgery | 40 (38.10) |
| Reason for
unresectability | |
| Metastases | 30 (28.60) |
| Local invasion | 15 (14.30) |
| Comorbidities | 6 (5.70) |
| Patient death | 1 (1.00) |
| Radiotherapy | |
| Adjuvant
post-operative | 11 (10.50) |
| Palliative | 13 (12.40) |
| Chemotherapy | |
| Adjuvant
post-operative | 18 (17.10) |
| Palliative | 27 (25.70) |
| Treatment | |
| Surgery alone | 32 (30.50) |
| Surgery + adjuvant
chemo/RT | 21 (20.00) |
| Palliative
chemo/RT | 28 (26.70) |
| TACE | 4 (3.80) |
| No treatment | 12 (11.40) |
| Albumin | |
| <3.0 gm/dl | 14 (13.30) |
| ≥3.0 gm/dl | 79 (75.20) |
| Bilirubin | |
| ≥2 mg/dl | 22 (21.00) |
| <2 mg/dl | 72 (68.60) |
| CA 19-9 | |
| ≥100 ng/ml | 38 (36.20) |
| <100 mg/ml | 67 (63.80) |
| CEA | |
| ≤2.5 ng/ml | 21 (20.00) |
| >2.5 ng/ml | 32 (30.50) |
| AST | |
| ≤55 IU/ml | 48 (45.70) |
| >55 IU/ml | 47 (44.80) |
| ALT | |
| ≤40 IU/ml | 33 (31.40) |
| >40 IU/ml | 62 (59.00) |
| Alkaline
phosphatase | |
| ≤140 IU/ml | 40 (38.10) |
| >140 IU/ml | 55 (52.40) |
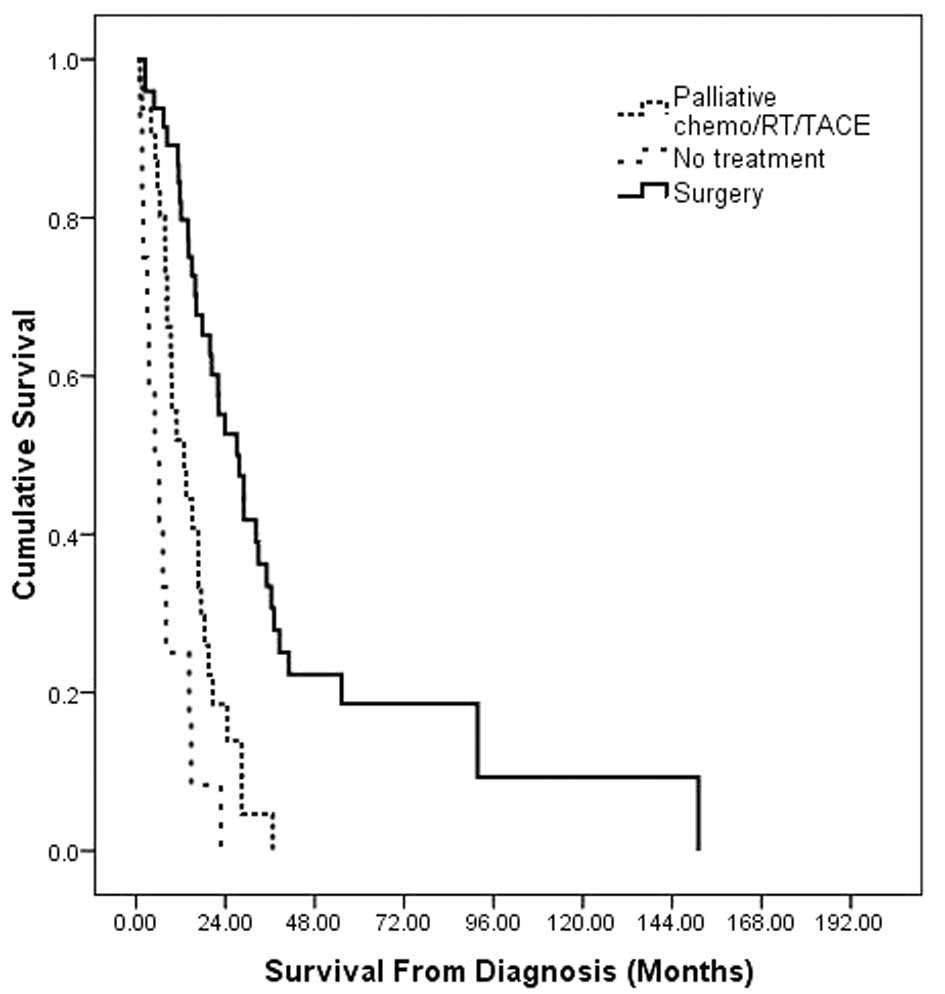
Median overall survival was 16.1 months (95% CI
13.1–19.2). The survival rates were 63% at 1 year, 17% at 3 years
and 9% at 5 years. The median survival after surgical resection was
27.6 months (17.7–37.6), with palliative treatment it was 12.9
months (6.5–19.2) and with best supportive care it was 4.9 months
(0.4–9.7) (Fig. 1). Metastatic
disease was present at diagnosis in 24 patients (22.9%). The most
common sites of metastases were the lung in 8 patients (33.3%) and
the peritoneum in 8 patients (33.3%). On univariate analysis,
factors associated with survival included tumor stage at diagnosis
(P<0.001), total bilirubin >2 mg/dl (P=0.032), presence of
metastases at diagnosis (P=0.008) and treatment received
(P<0.001) (Table II). Age,
gender, ethnicity, albumin <3 gm/dl, underlying risk factors,
and elevated CA 19–9 were not associated with survival. On
multivariate analysis, advanced stage at diagnosis (P=0.027) and
treatment received (P<0.001) were significant independent
predictors of survival (Table
II).
 | Table IIUnivariate and multivariate analysis
of factors associated with the survival of all patients with
intrahepatic cholangiocarcinoma. |
Table II
Univariate and multivariate analysis
of factors associated with the survival of all patients with
intrahepatic cholangiocarcinoma.
| Variables | n | Median
survival | 95% CI
survival | Univariate analysis
P-value | Multivariate
analysis P-value | HR (95% CI) |
|---|
| Age (years) | | | | | | |
| <59 | 38 | 17.7 | 15.5–19.9 | 0.292 | | |
| ≥60 | 67 | 14.2 | 11.0–17.5 | | | |
| Gender | | | | | | |
| Male | 53 | 16.6 | 10.0–23.3 | 0.822 | | |
| Female | 52 | 15.9 | 12.3–19.5 | | | |
| Ethnicity | | | | | | |
| Caucasian | 93 | 15.9 | 13.0–18.8 | 0.141 | | |
|
African-American | 6 | 22.7 | 0.0–65.2 | | | |
| Other | 6 | 14.9 | 5.6–24.3 | | | |
| Risk factor | | | | | | |
| None | 87 | 15.0 | 12.0–18.1 | 0.659 | | |
| Cirrhosis | 10 | 23.8 | 6.4–41.2 | | | |
| UC/PSC | 7 | 7.1 | 0.0–34.2 | | | |
| Stage at
diagnosis | | | | | | |
| I–II | 71 | 28.9 | 20.5–37.2 |
<0.001 | 0.027 | |
| III–IV | 34 | 13.5 | 9.1–17.8 | | | 2.0 (1.1–3.7) |
| Presence of
metastases at diagnosis | | | | | | |
| No | 80 | 17.7 | 13.6–21.8 | 0.008 | 0.204 | |
| Yes | 25 | 9.6 | 6.2–13.0 | | | 1.5 (0.8–2.83) |
| Treatment | | | | | | |
| Surgery | 53 | 27.6 | 17.6–37.6 |
<0.001 |
<0.001 | |
| Palliative
treatment | 32 | 12.8 | 6.5–19.2 | | | 2.2 (1.1–4.1) |
| Best supportive
care | 12 | 4.9 | 0.3–9.6 | | | 5.9 (2.8–12.7) |
| Albumin | | | | | | |
| <3.0 gm/dl | 14 | 14.9 | 0.0–95.3 | 0.887 | | |
| ≥3.0 gm/dl | 79 | 35.0 | 12.4–17.5 | | | |
| Bilirubin | | | | | | |
| ≥2.0 mg/dl | 22 | 9.4 | 5.7–13.1 | 0.032 | 0.081 | |
| <2.0 mg/dl | 72 | 16.6 | 11.2–22.0 | | | 0.6 (0.3–1.1) |
| CA 19-9 | | | | | | |
| ≥100 ng/ml | 38 | 16.6 | 12.3–20.9 | 0.991 | | |
| <100 mg/ml | 67 | 16.1 | 12.2–20.0 | | | |
Of the 105 patients, 53 patients underwent curative
surgical resection (50.5%). The type of surgery they underwent was
as follows: trisegmentectomy (44.9%), hepatectomy (right 32.6%,
left 16.2%) and transplantation (6.1%). The distribution of
patients on the basis of their T stage was as follows: T1 (40.8%),
T2 (36.7%), T3 (14.3%) and T4 (8.2%). On lymph node dissection
24.5% were node positive. Histopathologic examination revealed the
presence of microvascular invasion in 54.7%. The distribution in
the different AJCC 7 stages was as follows: I (34.7%), II (18.4%),
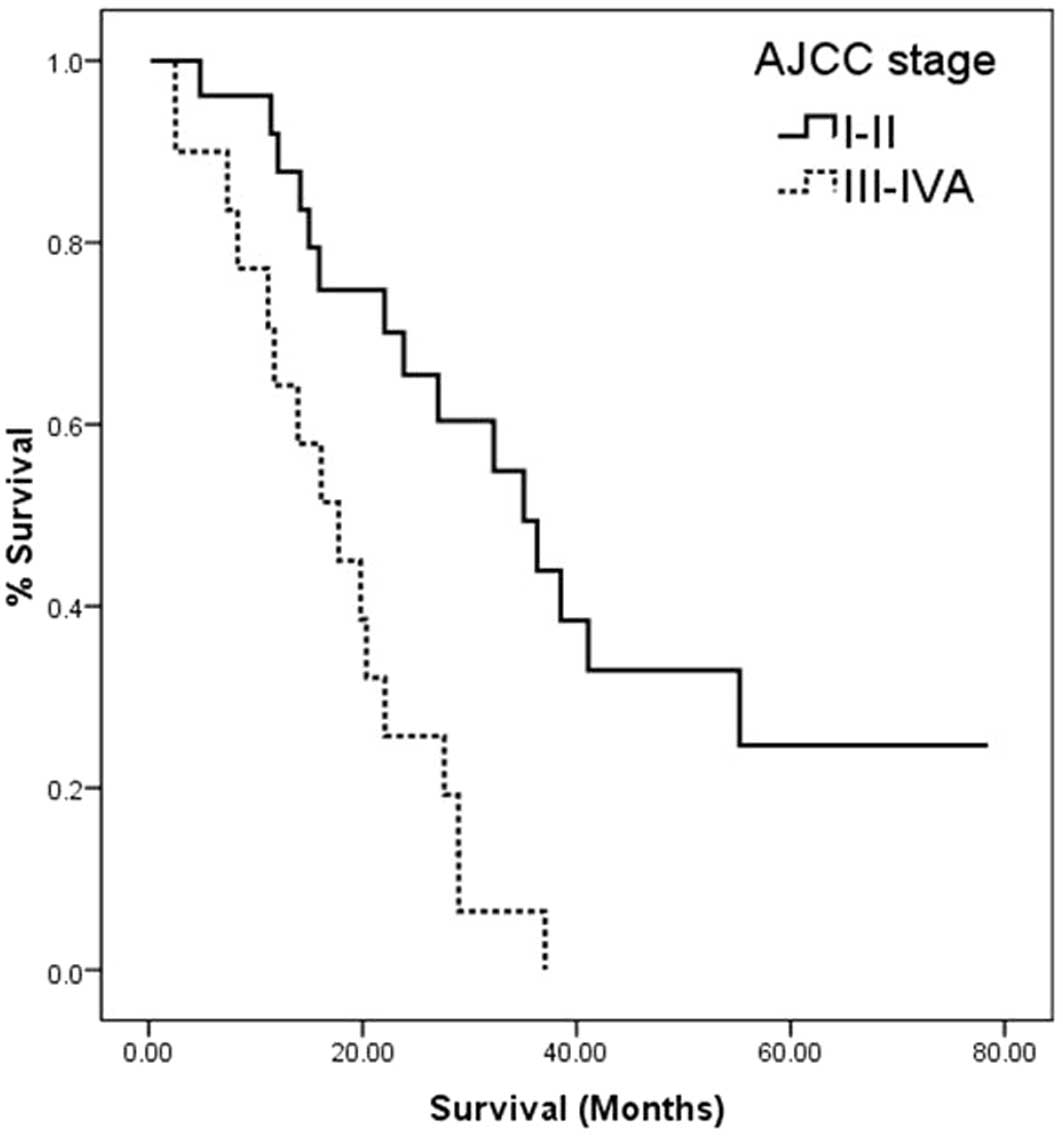
III (12.2%) and IVa (34.7%). The median survival of patients with
stage I was 36.3 months, stage II was 27.1 months, stage III 20.3
months, and stage Iva was 16.1 months (P<0.001). When tumors
were classified on the basis of diameter of the largest lesion,
53.1% of tumors were found to be >5 cm. Yet, size was not noted
to influence survival when considered as a continuous or as a
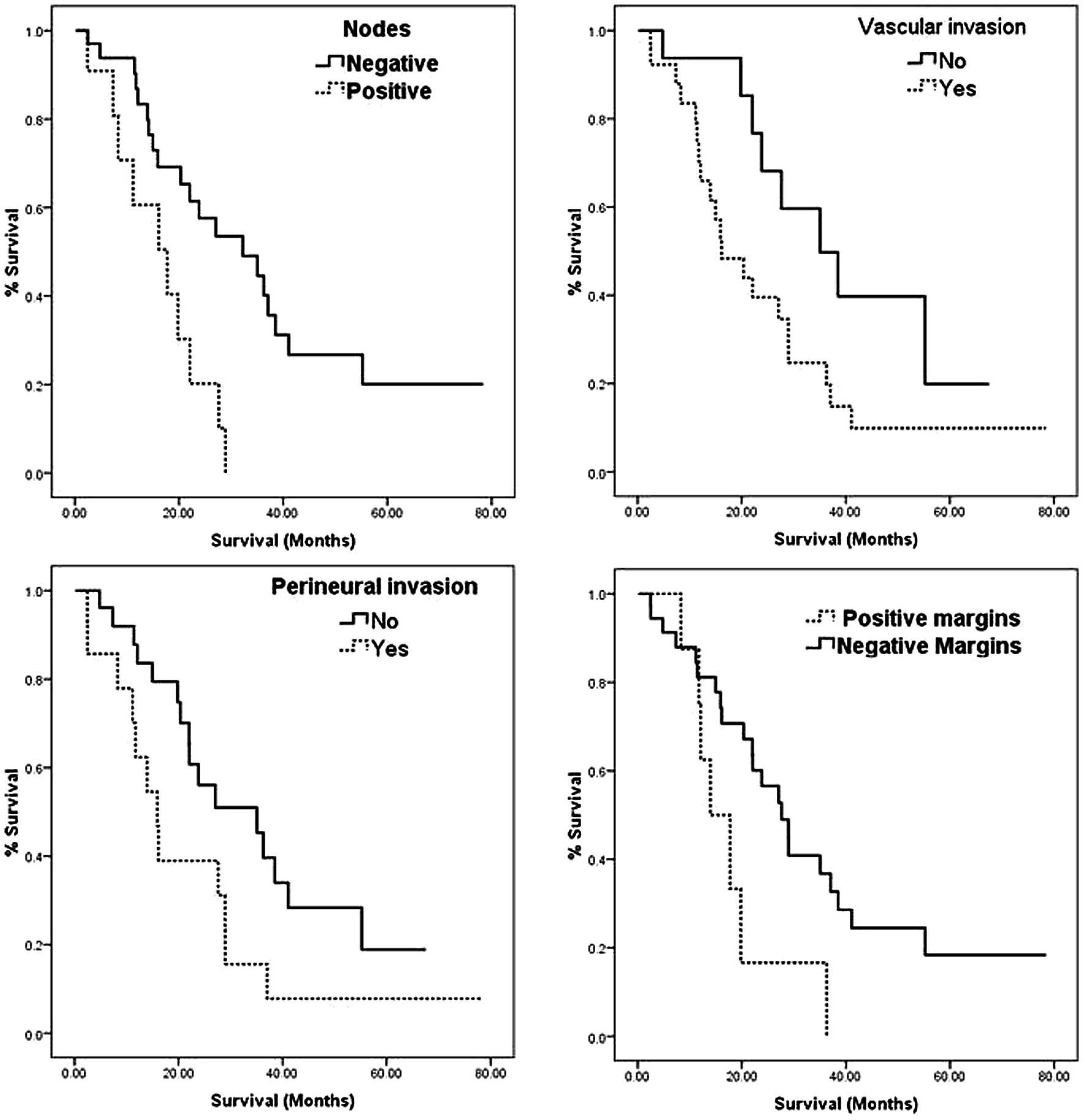
categorical variable (0.875). Among the components of AJCC staging,
nodal positivity was found to most strongly influence staging
(P<0.001 on Chi-square test), and the strength of association as
assessed by Kendall’s Tau-B for this relationship was 0.753.
In 21 patients, surgery was followed by adjuvant
chemoradiotherapy (39.6%). The median survival after resection was
27.6 months (17.7–37.6). The survival rates were 82% at 1 year, 33%
at 3 years and 19% at 5 years. The median survival in patients with
a microscopic negative margin on final pathology (R0 resection) was
28.9 months (22.7–35.1). Table
III describes the prognostic factors for survival after
resection. On univariate analysis, the AJCC stage of the tumor
(P<0.001), the presence of microvascular invasion (P=0.006),
perineural invasion (P=0.004), nodal positivity (P=0.002) and
positive margins (P=0.028) were factors influencing survival. On
multivariate analysis, advanced AJCC stage (P=0.007) and presence
of microvascular invasion (P=0.013) were found to be significant
and independent predictors of poor survival (Figs. 2 and 3).
 | Table IIIUnivariate and multivariate analysis
of factors associated with survival of the patients who underwent
curative resection. |
Table III
Univariate and multivariate analysis
of factors associated with survival of the patients who underwent
curative resection.
| Variables | n (%) | Median
survival | 95% CI
survival | Univariate analysis
P-value | Multivariate
analysis P-value | HR (95% CI) |
|---|
| Age (years) |
| <59 | 19 (35.8) | 32.2 | 9.9–54.6 | 0.386 | | |
| ≥60 | 34 (64.2) | 27.07 | 18.1–35.9 | | | |
| Gender |
| Male | 29 (54.7) | 28.9 | 21.8–36.0 | 0.812 | | |
| Female | 24 (45.3) | 20.3 | 15.4–24.1 | | | |
| Risk factor |
| None | 44 (83.0) | 27.0 | 17.2–36.8 | | | |
| Cirrhosis | 5 (9.4) | 23.8 | 10.0–37.6 | 0.79 | | |
| UC/PSC | 3 (5.7) | 32.2 | - | | | |
| AJCC stage |
| I–II | 26 (56.6) | 35.1 | 22.9–47.2 |
<0.001 | 0.007 | - |
| III–IVa | 2123 (39.6) | 17.7 | 10.5–24.9 | | | 3.1 (1.4–7.0) |
| Treatment |
| Surgery alone | 32 (60.4) | 23.8 | 5.0–42.6 | 0.174 | | |
| Surgery + adjuvant
chemo/RT | 21 (39.6) | 27.6 | 16.9–38.2 | | | |
| Recurrence |
| Yes | 24 (45.3) | 28.9 | 16.7–41.2 | 0.314 | | |
| No | 29 (54.7) | 17.7 | 0–36.4 | | | |
|
Differentiation |
| Well | 7 (13.2) | - | - | 0.094 | | |
| Moderate | 31 (58.5) | 22.0 | 9.6–34.5 | | | |
| Poor | 9 (17.0) | 28.9 | 2.6–55.3 | | | |
| Tumor size
(cm) |
| <5 | 18 (33.9) | 27.1 | 19.4–34.7 | 0.875 | | |
| ≥5 | 26 (49.1) | 22.0 | 13.2–30.8 | | | |
| Microvascular
invasion |
| Yes | 29 (54.7) | 16.1 | 7.8–24.4 | 0.006 | 0.013 | - |
| No | 19 (35.8) | 38.5 | 21.4–55.5 | | | 3.0 (1.3–7.0) |
| Perineural
invasion |
| Yes | 17 (32.1) | 16.1 | 12.1–20.0 | 0.004 | 0.897 | - |
| No | 31 (58.5) | 35.0 | 18.8–51.2 | | | 0.9 (0.4–2.3) |
| Surgical
margins |
| Positive | 9 (17.0) | 13.9 | 7.2–20.6 | 0.028 | 0.131 | - |
| Negative | 40 (75.5) | 28.9 | 22.7–35.1 | | | 0.5 (0.2–1.3) |
| Lymph nodes |
| Positive | 13 (24.5) | 17.7 | 7.8–27.6 | 0.002 | 0.420 | - |
| Negative | 36 (67.9) | 35.0 | 21.3–48.7 | | | 1.7 (0.5–5.8) |
| CA 19-9 level |
| <100 ng/ml | 16 (30.2) | 35.0 | 19.8–50.2 | 0.295 | | |
| ≥100 ng/ml | 37 (69.8) | 22.0 | 15.1–29.0 | | | |
| Albumin level |
| ≥3.0 gm/dl | 39 (73.6) | 22.0 | 13.1–30.9 | 0.661 | | |
| <3.0 gm/dl | 8 (15.1) | 37.0 | 33.7–40.3 | | | |
| Bilirubin
level |
| <2.0 mg/dl | 40 (75.5) | 27.6 | 17.3–37.7 | 0.816 | | |
| ≥2.0 mg/dl | 7 (13.2) | 22.0 | 12.2–31.8 | | | |
| NLR |
| <5 | 24 (45.3) | 23.8 | 15.4–32.2 | 0.349 | | |
| ≥5 | 12 (22.6) | 32.8 | 16.6–49.0 | | | |
After resection, the tumor recurred in 24 patients
(45.3%). The mean time to recurrence after resection was 16.7
months (0.7–125.9). The most common site of recurrence was the
liver (75%) followed by the lung (25%). AJCC stage, tumor
differentiation, microvascular invasion, perineural invasion, nodal
positivity, positive margins after resection or adjuvant
chemoradiotherapy did not influence the development of
recurrence.
Of the overall study group, 52 patients were not
eligible for resection (49.5%). The median survival for patients
not undergoing resection was 9.5 months (6.3–12.6). The survival
rates were 45% at 1 year, 13% at 2 years and 2.6% at 3 years. The
reasons for unresectability were the presence of metastatic disease
(57.6%), local tumor invasion (28.8%) and presence of comorbidities
(11.5%). Palliative chemo/radiotherapy was used in 28 patients
(53.8%) and transarterial chemoembolization was performed in 4
patients (7.7%). A minority of patients received best supportive
care alone (23.1%). The median survival of patients treated with
palliative therapies was 12.9 months (6.5–19.2), while the median
survival with best supportive care alone was 5.0 months (0.4–9.6;
P=0.007).
Discussion
The incidence of ICC is on the rise, generating
clinical interest in improving outcomes and identifying prognostic
factors. In this large series of ICC, we found that only 50% of the
patients were resectable based on pre-operative imaging.
Furthermore, approximately 60% of those operated on already had
local invasion, microvascular invasion or lymph node involvement.
Lymph node status was the most important component of staging,
stressing the importance of intra-operative lymph node assessment.
The most favorable survival was observed in patients operated on
with single tumors without vascular invasion or nodal involvement
who received R0 resection (with negative surgical margins) (38.5
months vs. 19.8 months). This experience confirms the importance of
achieving R0 resection as the key treatment for optimal outcome.
The present study also revealed that use of chemoradiotherapy in
the adjuvant setting failed to improve survival but its palliative
use in those with unresectable ICC offered a modest survival
advantage over best supportive care. While the size of the tumor
was not a relevant prognostic factor, both stage and surgical
treatment independently influenced survival. Furthermore,
microvascular invasion on pathology also significantly and
independently affected overall survival in patients who underwent
resection.
Cholangiocarcinoma is well known to be a cancer more
common in older patients (13). In
our study, the mean age of patients at the time of ICC diagnosis
was 61.8 years, but in those patients with underlying PSC or
inflammatory bowel disease, ICC diagnosis occurred at an earlier
age, with the mean age at presentation being 53.4 years. While
painless jaundice is the most common presenting complaint in
patients with hilar or distal cholangiocarcinoma, ICC is known to
present more like hepatocellular carcinoma with symptoms of
abdominal pain (13–15). Other common presenting symptoms were
weight loss and jaundice. However, one third of the patients with
ICC were asymptomatic and were incidentally diagnosed upon
abdominal imaging. Traditionally, elevated CA 19-9 or high CEA or
their combination has been used as diagnostic clues for ICC
(14). In our study only about one
third of the patients had an elevated CA 19-9 or CEA (36% had a CA
19-9 >100 IU/ml and 30.5% had CEA >2.5 IU/ml) and fewer had
an elevation in both, stressing the lack of useful biomarkers in
this disease. The lack of specific presenting symptoms, absence of
effective tumor markers and the non-existence of screening
strategies together often leads to the late diagnosis of
cholangiocarcinoma (16).
ICC developed in the background of cirrhosis in
close to 10% of the patients, of which the majority (80%) were
patients with HCV-related cirrhosis. Epidemiological studies from
Eastern nations such as Japan have reported an even higher
incidence of HCV infection up to 36% among patients with ICC
(1,17–19). A
recent large cohort study from the US which included 718,687
veterans also reported a significant association between HCV and
ICC (11). HCV RNA has been
detected in cholangiocarcinoma cells. This finding indicates that
HCV may promote cholangiocyte proliferation and dysplasia of the
intrahepatic bile duct epithelium that eventually leads to tumor
development (20–22). We were unable to examine the
association between HCV and ICC in our data due to the small number
of patients with HCV and a lack of a control group.
In our study, 50.5% of patients underwent surgery
with curative intent. Curative resection offers the best hope of
cure in patients with localized disease. The 5-year survival rate
among patients who underwent curative resection was 19% with a
median survival of 27.6 months. Previous studies report a variable
5-year survival ranging from 16 to 44% with a median survival rate
ranging between 12–59 months (23–31).
The AJCC 7th edition staging does not include the size of tumor as
a factor for staging tumors when compared to the AJCC 6th edition.
Keeping in line with this, we did not find tumor size to influence
outcome. Patients who were considered to be at high risk for
recurrence due to local invasion and/or positive surgical margins
were treated with adjuvant chemoradiotherapy. We did not find a
significant survival benefit for patients who received adjuvant
chemoradiotherapy over those who did not receive adjuvant therapy
(Table III, P=0.174). However,
the median survival was slightly longer in the group receiving
adjuvant therapy when compared to the group not receiving
treatment. The lack of difference in survival probably explains why
margin positivity did not turn out to be a prognostic factor on
multivariate analysis while AJCC stage and microvascular invasion
were found to be predictors of long-term survival after curative
resection. Other studies have reported nodal positivity to be an
important prognostic factor (27,30,31)
yet, this factor was not found to be independently predictive of
survival on multivariate analysis. A possible explanation for this
finding is the strong correlation between AJCC stage and nodal
positivity, as demonstrated by the high Kendall’s Tau-B for this
relationship.
After curative resection, the tumor recurred in
nearly half of the patients, but the recurrence did not adversely
affect long-term survival. Most of the patients who developed
recurrence were treated for disease control with palliative
chemoembolization or systemic therapy. These interventions probably
skewed the survival rates among these patients by eliminating the
survival disadvantage one would expect with recurrence. In
addition, the mean time to recurrence from surgery was relatively
long. In this series established factors such as
vascular/perineural invasion or size were not found to predict
recurrence. However, most patients with these high-risk factors
were treated with adjuvant chemoradiotherapy which probably
decreased the chances of recurrence.
In our study, at the time of diagnosis a third of
the patients had metastatic disease and about half the patients had
unresectable tumors. Only 25% of these patients treated with
supportive therapy alone were living at one year from diagnosis. A
clear role for the use of palliative treatments in patients with
ICC has not been defined. Most studies on palliative
chemoradiotherapy concerned patients with hilar or distal
cholangiocarcinoma. In this series we showed that palliative
radiotherapy/chemotherapy were associated with a more favourable
survival when compared with no treatment. Given the rarity of this
cancer, prospective randomized clinical trials to confirm this
result would be difficult to perform.
Limitations of the study include its small sample
size and the long study period during which significant changes in
therapy occurred. Yet, among the reported literature for this rare
cancer, our study has one of the largest cohorts. While our study
included patients treated over the past decade it represents more
recent data compared with the older US studies in the literature.
Upon our review of the literature (Table IV), these earlier US studies from
more than a decade ago had a smaller number of patients and
included only patients who underwent resection. The present study
presented outcomes for all stages and treatments, including the
patients who receive palliative care.
 | Table IVStudies on intrahepatic
cholangiocarcinoma. |
Table IV
Studies on intrahepatic
cholangiocarcinoma.
| Study (ref.) | Year | Location | Study period | N
total/resected | Median survival
(months) | Survival rate | Prognostic
factors |
|---|
| Chu et
al(23) | 1997 | Hong Kong,
Philippines | 28 years | 77 | 12.2 | 16%, 5-year | Lymphatic
permeation, hilar nodal metastases |
| Harrison et
al (24) | 1998 | USA | 26 years | 32 | 59 | 42%, 5-year | Vascular invasion,
satellite lesions |
| Roayaie et
al(25) | 1998 | USA | 1991–1997 | 26/16 | 42.9 | 44%, 5-year | Positive margins,
tumor size, presence of satellite nodules, degree of tumor
necrosis |
| Leiser et
al(26) | 1998 | USA | 31 years | 61/28 | - | 60%, 3-year | Tumor stage |
| Valverde et
al(27) | 1999 | France | 1990–1997 | 30 | 28 | 22%, 3-year | Satellite nodules,
lymph node positivity |
| Weber et
al(28) | 2001 | USA | 1992–2000 | 53/33 | 37.4 | 55%, 3-year | Vascular invasion,
positive margins, multiple tumors |
| Ohtsuka et
al(29) | 2002 | Japan | 1984–2001 | 62 | 25.5 | 23%, 5-year | Multiple tumors,
high CA 19-9 levels |
| Li et
al(31) | 2009 | China | 1995–2005 | 136/65 | 20 | 20.1%, 5-year | Higher TNM, lymph
node metastasis |
| Guglielmi et
al(30) | 2009 | Italy | 1990–2007 | 81/43 | 40.0 | 20%, 5-year | Macroscopic tumor
type, lymph node, metastases, vascular invasion |
In conclusion, intrahepatic cholangiocarcinomas is
associated with poor prognosis and demands improved understanding
of the factors that determine development, outcomes and prognosis.
In this large series concerning a rare malignancy, surgery offers
the most advantageous curative option and outcome, emphasizing the
importance of resectability as a major prognostic factor. The
present study also revealed that use of chemoradiotherapy in the
adjuvant setting failed to improve survival but its palliative use
in those with unresectable ICC offered a modest survival advantage
over best supportive care. The overriding factors influencing
outcome were stage and the presence of microvascular invasion.
References
|
1
|
Chang KY, Chang JY and Yen Y: Increasing
incidence of intrahepatic cholangiocarcinoma and its relationship
to chronic viral hepatitis. J Natl Compr Cancer Netw. 7:423–427.
2009.PubMed/NCBI
|
|
2
|
Surveillance E, End Results (SEER)
Program(www.seer.cancer.gov) SEER*Stat Database
Incidence - SEER 9 Regs Research Data, Nov 2009 Sub (1973–2007)
National Cancer Institute, DCCPS, Surveillance Research Program,
Cancer Statistics Branch, released April 2010, based on the
November 2009 submission
|
|
3
|
Espey DK, Wu XC, Swan J, et al: Annual
report to the nation on the status of cancer, 1975–2004 featuring
cancer in American Indians and Alaska Natives. Cancer.
110:2119–2152. 2007.
|
|
4
|
Patel T: Increasing incidence and
mortality of primary intrahepatic cholangiocarcinoma in the United
States. Hepatology. 33:1353–1357. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shaib YH, Davila JA, McGlynn K and
El-Serag HB: Rising incidence of intrahepatic cholangiocarcinoma in
the United States: a true increase? J Hepatol. 40:472–477. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lowe R, Afdhal N and Anderson C:
Epidemiology, pathogenesis, and classification of
cholangiocarcinoma. UpToDate. Basow DS: UpToDate Waltham, MA:
2010
|
|
7
|
Helms RA and Quan DJ: Intrahepatic
cholangiocarcinoma. Textbook of Therapeutics: Drug and Disease
Management. 8th. Lipincott Williams & Wilkins; Philadelphia,
PA: pp. 23802006
|
|
8
|
Wideroff L, Gridley G, Mellemkjaer L, et
al: Cancer incidence in a population-based cohort of patients
hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst.
89:1360–1365. 1997. View Article : Google Scholar
|
|
9
|
Donato F, Gelatti U, Tagger A, et al:
Intrahepatic cholangiocarcinoma and hepatitis C and B virus
infection, alcohol intake, and hepatolithiasis: a case-control
study in Italy. Cancer Causes Control. 12:959–964. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Welzel TM, Graubard BI, El-Serag HB, et
al: Risk factors for intrahepatic and extrahepatic
cholangiocarcinoma in the United States: a population-based
case-control study. Clin Gastroenterol Hepatol. 5:1221–1228. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
El-Serag HB, Engels EA, Landgren O, et al:
Risk of hepatobiliary and pancreatic cancers after hepatitis C
virus infection: a population-based study of U.S. veterans.
Hepatology. 49:116–123. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Edge SB and Compton CC: The American Joint
Committee on Cancer: the 7th edition of the AJCC cancer staging
manual and the future of TNM. Ann Surg Oncol. 17:1471–1474. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Anderson CD, Pinson CW, Berlin J and Chari
RS: Diagnosis and treatment of cholangiocarcinoma. Oncologist.
9:43–57. 2004. View Article : Google Scholar
|
|
14
|
Ustundag Y and Bayraktar Y:
Cholangiocarcinoma: a compact review of the literature. World J
Gastroenterol. 14:6458–6466. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gatto M and Alvaro D: Cholangiocarcinoma:
risk factors and clinical presentation. Eur Rev Med Pharmacol Sci.
14:363–367. 2010.PubMed/NCBI
|
|
16
|
Carriaga MT and Henson DE: Liver,
gallbladder, extrahepatic bile ducts, and pancreas. Cancer.
75(Suppl 1): 171–190. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamamoto S, Kubo S, Hai S, et al:
Hepatitis C virus infection as a likely etiology of intrahepatic
cholangiocarcinoma. Cancer Sci. 95:592–595. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kobayashi M, Ikeda K, Saitoh S, et al:
Incidence of primary cholangiocellular carcinoma of the liver in
Japanese patients with hepatitis C virus-related cirrhosis. Cancer.
88:2471–2477. 2000. View Article : Google Scholar
|
|
19
|
Shin HR, Lee CU, Park HJ, et al: Hepatitis
B and C virus, Clonorchis sinensis for the risk of liver
cancer: a case-control study in Pusan, Korea. Int J Epidemiol.
25:933–940. 1996.PubMed/NCBI
|
|
20
|
Perumal V, Wang J, Thuluvath P, Choti M
and Torbenson M: Hepatitis C and hepatitis B nucleic acids are
present in intrahepatic cholangiocarcinomas from the United States.
Hum Pathol. 37:1211–1216. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chen RF, Li ZH, Zou SQ and Chen JS: Effect
of hepatitis C virus core protein on modulation of cellular
proliferation and apoptosis in hilar cholangiocarcinoma.
Hepatobiliary Pancreat Dis Int. 4:71–74. 2005.PubMed/NCBI
|
|
22
|
Torbenson M, Yeh MM and Abraham SC: Bile
duct dysplasia in the setting of chronic hepatitis C and alcohol
cirrhosis. Am J Surg Pathol. 31:1410–1413. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chu KM, Lai EC, Al-Hadeedi S, et al:
Intrahepatic cholangiocarcinoma. World J Surg. 21:301–306. 1997.
View Article : Google Scholar
|
|
24
|
Harrison LE, Fong Y, Klimstra DS, Zee SY
and Blumgart LH: Surgical treatment of 32 patients with peripheral
intrahepatic cholangiocarcinoma. Br J Surg. 85:1068–1070. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Roayaie S, Guarrera JV, Ye MQ, et al:
Aggressive surgical treatment of intrahepatic cholangiocarcinoma:
predictors of outcomes. J Am Coll Surg. 187:365–372. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lieser MJ, Barry MK, Rowland C, Ilstrup DM
and Nagorney DM: Surgical management of intrahepatic
cholangiocarcinoma: a 31-year experience. J Hepatobiliary Pancreat
Surg. 5:41–47. 1998.PubMed/NCBI
|
|
27
|
Valverde A, Bonhomme N, Farges O, Sauvanet
A, Flejou JF and Belghiti J: Resection of intrahepatic
cholangiocarcinoma: a Western experience. J Hepatobiliary Pancreat
Surg. 6:122–127. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Weber SM, Jarnagin WR, Klimstra D,
DeMatteo RP, Fong Y and Blumgart LH: Intrahepatic
cholangiocarcinoma: resectability, recurrence pattern, and
outcomes. J Am Coll Surg. 193:384–391. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ohtsuka M, Ito H, Kimura F, et al:
Extended hepatic resection and outcomes in intrahepatic
cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 10:259–264.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Guglielmi A, Ruzzenente A, Campagnaro T,
et al: Intrahepatic cholangiocarcinoma: prognostic factors after
surgical resection. World J Surg. 33:1247–1254. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li SQ, Liang LJ, Hua YP, et al: Long-term
outcome and prognostic factors of intrahepatic cholangiocarcinoma.
Chin Med J. 122:2286–2291. 2009.PubMed/NCBI
|