Introduction
Intraventricular meningiomas are rare tumors that
account for 0.5–3% of all intracranial meningiomas (1), however, they remain one of the most
challenging problems in neurosurgery. Among meningiomas of the
central nervous system (CNS), cystic meningiomas are a distinct
histological variant of meningiomas accounting for ~1.6% of all CNS
meningiomas. Thus, cystic meningiomas located in the ventricle are
particularly rare and may be misdiagnosed along with other brain
tumors, including ependymoma, choroid plexus papilloma and
neurocytoma. The present study discusses two cases of lateral
ventricular meningiomas that exhibited intratumoral or peritumoral
cystic changes with magnetic resonance imaging (MRI). The two cases
were misdiagnosed prior to surgery. Written informed patient
consent was obtained from the 2 patients. The aim of the present
study was to provide additional data for this rare meningioma
variant.
Case reports
Case 1
Patient history
A 48-year-old female presented with a chronic
headache and vertigo that had persisted over a period of 2 months,
but had progressively worsened in the last 10 days. Neurological
examination, laboratory tests and other systemic evaluations (i.e.,
surgical and medical examination of the whole body) revealed no
abnormalities, with the exception of hypertension.
Examination
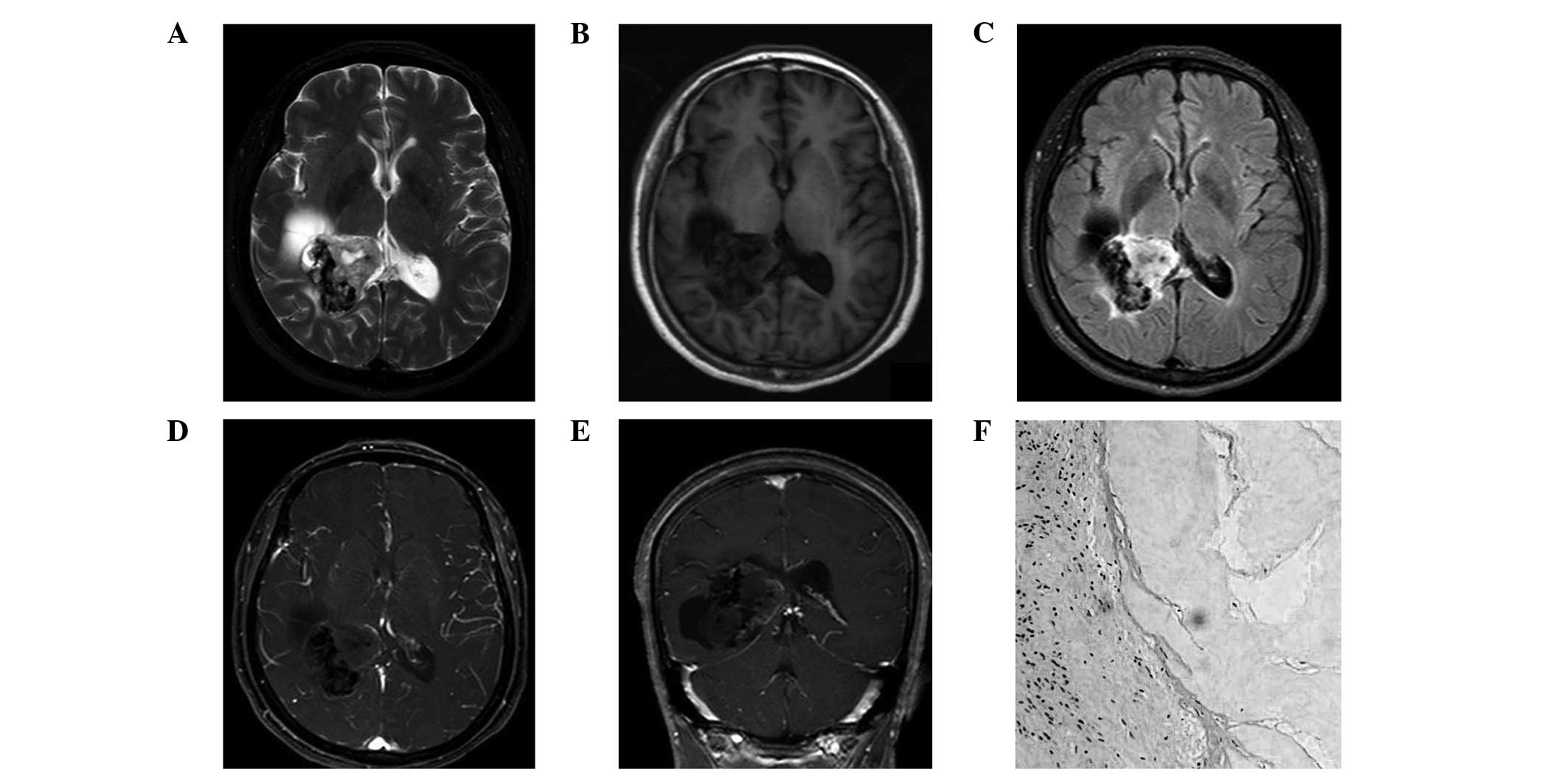
MRI scans revealed a 4.5×5.0×4.0 cm heterogeneously
irregular mass located in the trigone of the right lateral
ventricle. An intratumoral cystic change was also observed. The
tumoral parenchyma was hyperintense on T2-weighted images (WIs) and
fluid attenuated inversion-recovery images, while appearing iso- to
hypointense on T1WIs (Fig. 1A–E).
Patchy calcification, which appeared hypointense in every sequence,
was also observed in the marginal area of the tumor. Contrast
enhanced MRI revealed mild enhancement in the tumoral parenchyma.
The inferior and posterior horn of the right lateral ventricle
revealed moderate obstructive hydrocephalus. Based on previous
manifestations, the tumor was diagnosed as an ependyma or a choroid
plexus papilloma prior to surgery.
Treatment
Surgery via temporal-occipital craniotomy revealed
that the tumor was an ivory-colored hard mass which was
well-circumscribed in the right trigone of the lateral ventricle.
Evident calcification was observed without a visible blood supply.
Pathological examination confirmed the mass to be a metaplastic
meningioma [World Health Organization (WHO) grade I; Fig. 1F].
Case 2
Patient history
A 43-year-old female presented with a persistent
headache and blurred vision which has lasted for longer than one
month. Neurological examination revealed papilla edematous and
increased intracranial pressure.
Examination
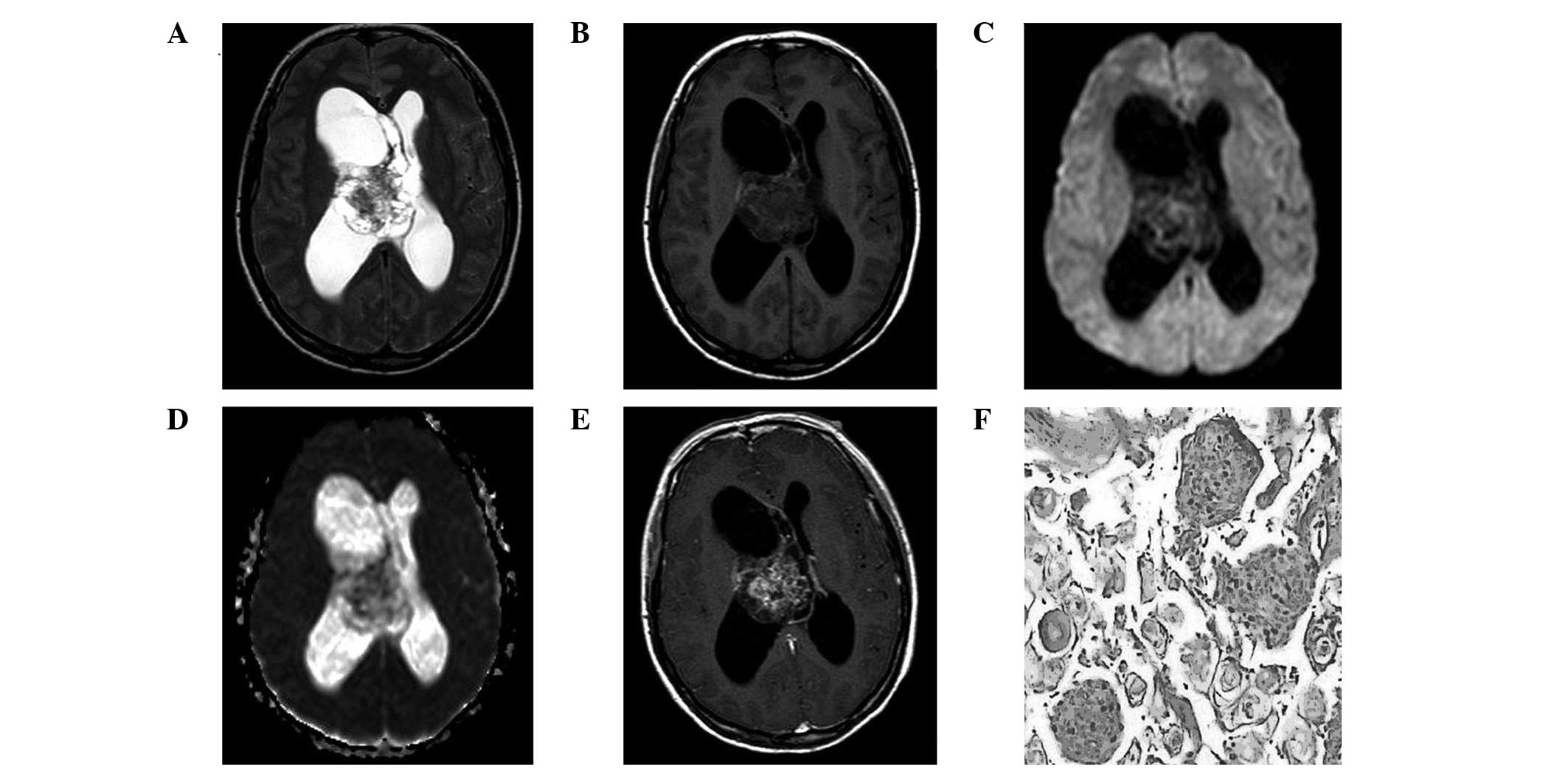
MRI scans revealed a heterogeneously cystic-solid
mass of 4.8×5.0×5.5 cm in the right lateral ventricle. The solid
area of the tumor exhibited an iso- to hypointense signal on T2WIs
and an isointense signal on T1WIs and diffusion weighted imaging.
On an apparent diffusion coefficient map, the parenchyma of the
tumor exhibited an isointense signal. Overt enhancement was
observed on T1-weighted post-gadolinium contrast images in the
solid area instead of the cystic component (Fig. 2A–E). The tumor was diagnosed as an
ependymoma or a neurocytoma prior to surgery.
Treatment
Surgery via a right temporoparietal craniotomy
revealed that the tumor was a well-defined, yellowish in color,
intact and encapsulated mass that adhered slightly to the walls of
the lateral ventricle and the septum pellucidum. The marginal area
of the tumor was cystic and the root originated from the choroid
plexus. Pathological examination confirmed the mass to be a
psammomatous meningioma (WHO grade I; Fig. 2F).
Discussion
Meningiomas are the most common extra-axial neoplasm
with the general characteristic imaging appearance of isointense or
hypointense on T1WIs and isointense or hyperintense on T2WIs,
exhibiting marked homogeneous contrast enhancement. Lateral
ventricular and cystic meningiomas are rare meningioma variants
(1). To the best of our knowledge,
cystic changes in intraventricular meningiomas have not previously
been reported in adult patients.
Cystic meningioma, used to describe meningiomas with
intratumoral or peritumoral cysts, are uncommon and account for
2–4% of all intracranial meningiomas (2). Rengachary et al classified
cystic meningiomas as intratumoral or extratumoral (3). Pathophysiological mechanisms of
peritumoral cysts may be caused by loculated widened subarachnoid
space, edema of the surrounding brain, demyelination or
hemorrhaging near the tumor, while intratumoral cysts are the
outcome of cystic degeneration, ischemic necrosis or hemorrhaging
within the tumor. Cystic meningioma may often be misdiagnosed as
other neoplasms, including gliomas or metastatic tumors, on
preoperative MRI (4). However, due
to the specific lesion location (the lateral ventricle), the tumors
in the present study were misdiagnosed as ependymomas, choroid
plexus papillomas or neurocytomas, which are the most common tumor
types to appear with cysts and calcifications in the ventricular
system.
Although differential diagnosis is difficult to
separate cystic meningiomas from common tumors in the ventricular
system, specific signs may aid differentiation. The majority of
supratentorial ependymomas (70%) arise within the brain parenchyma
of the cerebral hemispheres rather than from the ependymal cells
lining the ventricular surfaces (5). In addition, neurocytomas tend to
occur in younger patients and are located at the foramen of Monro
and the roof of the lateral ventricle. Intraventricular choroid
plexus papillomas are more common in childhood with occasional
calcification of punctate foci in lesions. However, meningiomas are
most common in adult females (6).
Notably, the current two cases had histologically
different subtypes, which may be associated with their various MRI
manifestations. Case 1 is a metaplastic meningioma, characterized
by mesenchymal elements, including osseous, cartilaginous and
myxoid tissue, which may lead to calcification or ossification and
cystic formation as exhibited in the MRI scans. A previous case
report (7) regarding a metaplastic
meningioma in a child also revealed similar MRI features; for
example, the meningioma was located in the lateral ventricle and
cystic changes were observed within the tumor. By contrast, case 2
is of a psammomatous meningioma, which is mainly composed of hyalin
and calcifies to form the characteristic concentric calcifications
known as psammoma bodies, thus, is shown as a densely calcified
mass on MRI and CT scans. The cystic-solid feature of psammomatous
meningioma has not been reported previously. Thus, we hypothesized
that the cystic change in this case may be associated with the
penetration of cerebrospinal fluid around the tumor, which leads to
the multiple cystic changes within the tumor. Metaplastic and
psammomatous meningiomas are classified as WHO grade 1 with a low
risk of recurrence and aggressive growth. Total tumor resectioning
is important to reduce the risk of recurrence. The two patients
were completely recovered without positive neurological symptoms
and signs of recurrence at one year follow-up.
In conclusion, to the best of our knowledge, this is
the first case report of cystic meningioma localized in the lateral
ventricle in adult females. Although cystic meningioma located in
the lateral ventricle is rare, this clinical entity should be
included in the differential diagnosis of neoplasms in the lateral
ventricle, particularly in adult female patients.
Reference
|
1
|
Kim EY, Kim ST, Kim HJ, Jeon P, Kim KH and
Byun HS: Intraventricular meningiomas: radiological findings and
clinical features in 12 patients. Clin Imaging. 33:175–180. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen TY, Lai PH, Ho JT, et al: Magnetic
resonance imaging and diffusion-weighted images of cystic
meningioma: correlating with histopathology. Clin Imaging.
28:10–19. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rengachary S, Batnitzky S, Kepes JJ,
Morantz RA, O’Boynick P and Watanabe I: Cystic lesions associated
with intracranial meningiomas. Neurosurgery. 4:107–114. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yamada SM, Fujimoto Y, Kawanishi Y and
Shimizu K: A cystic meningioma misdiagnosed as malignant glioma by
radiologic and intraoperative histological examinations. Brain
Tumor Pathol. 27:111–115. 2010. View Article : Google Scholar
|
|
5
|
Yuh EL, Barkovich AJ and Gupta N: Imaging
of ependymomas: MRI and CT. Childs Nerv Syst. 25:1203–1213. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rockhill J, Mrugala M and Chamberlain MC:
Intracranial meningiomas: an overview of diagnosis and treatment.
Neurosurg Focus. 23:E12007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dulai MS, Khan AM, Edwards MS and Vogel H:
Intraventricular metaplastic meningioma in a child: case report and
review of the literature. Neuropathology. 29:708–712. 2009.
View Article : Google Scholar : PubMed/NCBI
|