Introduction
Sepsis is a serious systemic inflammatory response
syndrome (SIRS) caused by infection with bacteria, fungi, viruses
or parasites (1). The pathogenesis
of sepsis is associated with disorder of whole-body inflammatory
reaction networks (2). When the
immune system becomes overactivated in response to an existing
infection, the inflammatory response may lead to dysfunction of
vital organs, such as the lung, heart, kidney and liver (3). The liver plays a critical role in the
host defense mechanism (4), and is
one of the organs most frequently affected by organ dysfunction in
sepsis (5). The liver modulates
inflammatory processes, and produces and releases high amounts of
various cytokines (6), which play an
important role in the regulation and transduction of inflammatory
signals (7). During sepsis,
pro-inflammatory cytokines, including tumor necrosis factor (TNF)-α
and interleukin (IL)-6, have a crucial effect on the initiation of
the inflammatory process (8).
Anti-inflammatory cytokines, such as IL-10, are also found to be
extensively released in septic patients (9). Moreover, cytokines mediate and amplify
inflammatory signals through the Janus kinase-signal transducer and
activator of transcription JAK-STAT pathway in a number of diseases
(10). A recent study has revealed
that suppressors of cytokine signaling (SOCS) are able to suppress
cytokine-mediated inflammatory signaling as feedback regulators in
the JAK-STAT pathway (11). SOCS-1,
a member of the SOCS family, has been experimentally demonstrated
to be effective in reducing the inflammatory response in
inflammatory diseases (12,13). Mice deficient in SOCS-1 have
exhibited liver degeneration and lymphoid deficiencies (14). Furthermore, a previous study has
shown that sepsis induces SOCS-1 expression in rat liver and muscle
(15), and it has been recognized
that SOCS1 plays an important role in LPS-induced liver injury.
Therefore, SOCS-1 may be involved in the pathogenesis of liver
injury in cecal ligation and puncture (CLP)-induced septic
rats.
Xuebijing injection is a newly developed Chinese
herbal injection consisting of Chuangxiong Rhizoma (the dried
rhizome of Ligusticum chuanxiong Hort.), Paeoniae Radix
Rubra (the dried roots of Paeonia lactiflora Pall.), Salviae
Miltiorrhizae Radix et Rhizoma (the dried roots and rhizome of
Salvia miltiorrhiza Bge.) and Carthami Flos (the dried
flower of Carthamus tinctorius L.). It has anti-inflammatory
and anti-endotoxic effects in the treatment of sepsis (16). Experimental and clinical studies have
revealed that Xuebijing injection is effective for the treatment of
SIRS, pyemia and multiple organ dysfunction syndrome (17–19). In
addition, Xuebijing injection has been formally approved by the
State Food and Drug Administration of China for use in clinical
practice and is widely used to treat sepsis in China. However, the
underlying molecular mechanisms of Xuebijing injection remain
unclear. Thus, the aim of the present study was to investigate the
effect of Xuebijing injection on liver injury in CLP-induced septic
rats and to explore the underlying mechanism. In particular, the
study aimed to focus on the effect of Xuebijing injection on
hepatic inflammatory cytokine secretion and SOCS1 expression in
rats with sepsis-induced liver injury.
Materials and methods
Chemicals and antibodies
Xuebijing injection was supplied by Tianjin Chase
Sun Pharmaceutical Co., Ltd. (Tianjin, China; lot no. Z20070410).
Antibodies targeting SOCS-1 (sc-9021) and β-actin (sc-130656) were
purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA).
Horseradish peroxidase (HRP)-conjugated anti-rabbit IgG antibody
(RPN4301) for the western blotting assay was purchased from
Amersham (GE Healthcare Life Sciences, Piscataway, NJ, USA).
Enzyme-linked immunosorbent assay (ELISA) kits for TNF-α, IL-6 and
IL-10 were purchased from R&D Systems, Inc. (Minneapolis, MN,
USA). The ABI StepOnePlus Real-Time PCR System was purchased from
Applied Biosystems (Thermo Fisher Scientific, Inc., Waltham, MA,
USA). All other chemicals used were of analytical grade.
Animals
Male Sprague-Dawley (SD) rats, weighing 240–280 g,
were provided by the Experimental Animal Center of Nantong
University (Nantong, China) and housed in a temperature- and
humidity-controlled environment with a 12-h light-dark cycle. The
animals had access to food and water ad libitum. The study
protocol was approved by the ethics committee (Institutional Review
Board) of Nantong University.
Animal model and treatment
A total of 72 rats were divided into three
experimental groups: Control group, CLP group and Xuebijing
injection-treated (XT) group. The rats in the latter group were
treated with 10 mg/kg Xuebijing injection, intraperitoneally, i.p.
Each group contained 24 rats. The septic rat model was induced by
CLP as previously described (20).
Briefly, all rats underwent fasting for 12 h and water deprivation
for 6 h prior to undergoing CLP surgery. Following pentobarbital
sodium anesthesia (45 mg/kg, i.p.), the abdominal region was
disinfected with iodophor and a 2-cm incision was made, the cecum
was then gently isolated with tight ligation and punctured twice
with an 18-gauge needle. Thereafter, the cecum was repositioned,
and the abdomen was subsequently closed. For the control group
alone, rats underwent the same surgical procedures, but the cecum
was neither ligated nor punctured. Saline (50 ml/kg body weight)
was administered subcutaneously to the rats for fluid
resuscitation. For the TX group, rats received an intraperitoneal
administration of Xuebijing injection (10 ml/kg body weight) twice
per day after CLP surgery for 3 consecutive days. Rats in the
control and CLP groups were administered equal volumes of saline
instead.
Alanine aminotransferase (ALT) and
aspartate aminotransferase (AST) activity measurements
To measure ALT and AST activities, 5-ml blood
samples were obtained from the aorta abdominalis of rats in
different groups at 6, 12, 24 and 24 h after CLP surgery. The ALT
and AST activities were then measured using a Hitachi 7600-020
Automatic Analyzer (Hitachi High-Technologies Corporation, Tokyo,
Japan).
ELISA analysis of TNF-α, IL-6, and
IL-10
Homogenized liver samples (0.5–1 g; 10%) from the
different groups, sampled at 6, 12, 24 and 24 h after CLP surgery,
were centrifuged at 1,500 × g for 15 min at 4°C) to obtain a
supernatant. The amounts of TNF-α, IL-6 and IL-10 in the liver
tissue homogenates were analyzed using commercial ELISA kits
specific for rats according to the manufacturer's protocol.
Cytokine levels are expressed in units of pg/ml.
Histological examination
The liver tissues from rats in each group were
collected at 6 and 48 h after CLP surgery. The tissue samples were
fixed in 10% formalin solution, embedded in paraffin, and
sectioned. The tissue sections were then stained with hematoxylin
and eosin reagent according to standard protocols and observed
using light microscopy.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
To determine the mRNA level of SOCS-1, RT-qPCR
analysis was performed. Briefly, liver tissues samples (50–100 mg)
were collected from rats in the various groups at 6, 12, 24 and 48
h after surgery. Total RNA was then extracted from homogenized
liver samples using TRIzol reagent (Gibco Life Technologies; Thermo
Fisher Scientific, Inc.) according to the manufacturer's protocol.
Total RNAs were treated with DNase I (Fermentas; Thermo Fisher
Scientific, Inc.) to remove any contaminating DNA at 37°C for 30
min, followed by deactivation at 65°C for 10 min. The RNA was then
reverse transcribed into cDNA using an M-MLV reverse transcription
kit (Takara Biotechnology Co., Ltd., Dalian, China) according to
the manufacturer's protocol with the ABI StepOnePlus Real-Time PCR
system. Following the reverse transcription, fluorescence qPCR was
performed using SYBR Green I dye (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) according to the manufacturer's protocol. The
following primers were used: SOCS-1 forward,
5′-CCGCTCCCACTCTGATTACC-3′ and reverse, 5′-CCCGAAGCCATCTTCACG-3′;
β-actin forward, 5′-CGGTTCCGATGCCCTGAGGCACTT-3′ and reverse,
5′-CGTCACACTTCATGATGGAATTGA-3′. The samples for RT-qPCR analysis
were evaluated using a single predominant peak as a quality
control. The comparative Ct (2−∆∆Ct) method (21) was used to analyze the relative
expression levels of SOCS1 mRNA, which were normalized to
β-actin.
Western blot analysis
Western blot analysis was performed using a similar
method to that previously described (22). Briefly, homogenized liver tissues
from different groups, sampled at 12 and 48 h, were centrifuged at
13,000 × g for 30 min at 4°C to generate a supernatant containing
the extracted protein. The protein concentration was measured using
a bicinchoninic acid (BCA) protein assay kit as previously
described (23,24). A 50 µg portion of each sample was
electrophoresed on polyacrylamide gel (10%) and transferred onto a
polyvinylidene difluoride membrane (EMD Millipore, Bedford, MA,
USA). After blocking with blocking buffer, the blots were incubated
2 h at 4°C with diluted primary antibodies against SOCS-1 (1:200).
The membrane was then washed three times in Tris-buffered saline
with Tween-20 (0.1%) and incubated with HRP-conjugated anti-rabbit
IgG antibody (dilution, 1:2,500) for 1.5 h at room temperature. The
membrane was again washed three times for 10 min each time, and
finally the immunoreactive proteins were detected using an enhanced
chemiluminescence Western blotting detection kit. The β-actin
protein served as an internal control.
Statistical analysis
The data were analyzed using STATA version 10.0
(StataCorp LP, College Station, TX, USA). One-way analysis of
variance (ANOVA) was used to analyze the significant differences
among different groups. P<0.05 was considered to indicate a
statistically significant difference.
Results
Xuebijing injection ameliorates
sepsis-induced histological liver injury in rats
Hematoxylin and eosin staining clearly revealed
liver injury characterized by edema, ballooning degeneration, fatty
degeneration, thrombosis and infiltration of inflammatory cells in
the liver tissues at 6 h after CLP surgery (Fig. 1). When examined at 48 h after CLP
surgery, hepatic cords were largely broken and all liver injury
symptoms become much more severe. However, these histological
alterations induced by CLP surgery were ameliorated by Xuebijing
injection treatment (Fig. 1).
Xuebijing injection decreases ALT and
AST levels in rats with septic liver injury
ALT and AST levels of rats from different groups
were measured at 6, 12, 24 and 24 h after CLP surgery. Sepsis
induced an increase of serum ALT and AST levels in rats in
comparison with those in the control group (P<0.05), which was
indicative of liver injury. However, as shown in Fig. 2, treatment with Xuebijing injection
significantly decreased ALT and AST levels in this model
(P<0.05).
Xuebijing injection regulates the
secretion of inflammatory cytokines in CLP-induced septic rats
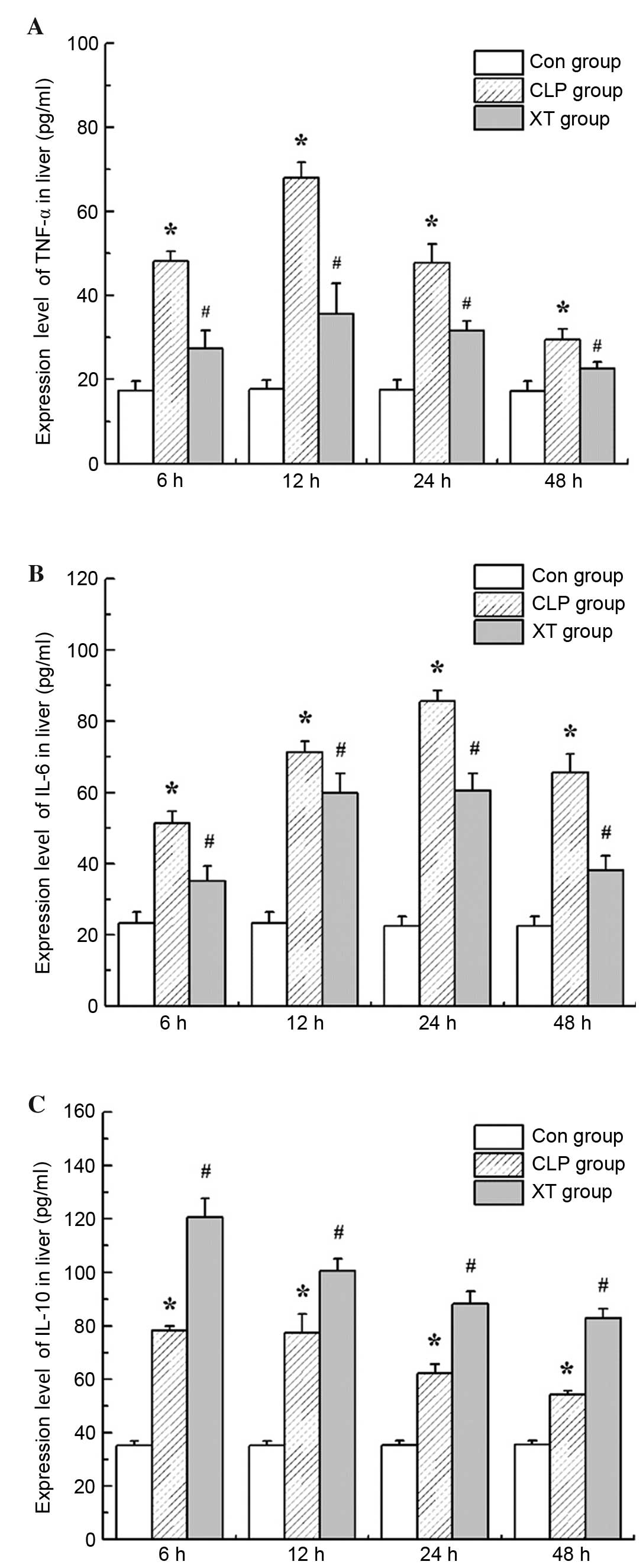
Sepsis is characterized by the uncontrollable
release of pro-inflammatory and anti-inflammatory cytokines
(25). In the present study, two
pro-inflammatory cytokines, TNF-α and IL-6, and one
anti-inflammatory cytokine, IL-10 were detected at 6, 12, 24 and 24
h after CLP surgery using ELISA kits. The results in Fig. 3 show that hepatic TNF-α, IL-6 and
IL-10 levels were significantly elevated in CLP-induced septic rats
in comparison with those in the control group (P<0.05). However,
Xuebijing injection treatment significantly downregulated hepatic
TNF-α and IL-6 levels, while upregulating hepatic IL-10 levels in
CLP-induced septic rats (P<0.05 for each).
Xuebijing injection elevates the
expression of SOCS-1 in CLP-induced septic rats
Numerous studies have found that SOCS proteins are
negative-feedback regulators in the JAK-STAT pathway (11). In the present study, the expression
of SOCS-1 was analyzed by RT-qPCR and western blotting. As shown in
Fig. 4, elevated SOCS-1 mRNA and
protein expression levels were observed in CLP-induced septic rats
(P<0.05 for mRNA), and the increases were further increased by
the Xuebijing injection treatment (Fig.
4).
Discussion
In the present study, it was demonstrated that
Xuebijing injection treatment attenuated liver injury induced by
sepsis. Furthermore, the results showed that Xuebijing injection
treatment downregulated TNF-α and IL-6 levels, and upregulated
IL-10 levels in the livers of septic rats, which was associated
with the expression of SOCS1. Therefore, the present study suggests
that Xuebijing injection protects against sepsis-induced liver
injury by regulating the secretion of inflammatory cytokines and
increasing the expression of SOCS1 in the livers of septic
rats.
A previous clinicopathological study reported that
patients dying from sepsis typically had inflammation and necrosis
in the liver; increased levels of markers of abnormal liver
biochemistry, including ALT and AST, were also observed in septic
patients prior to death (26). In
the present study, CLP-induced sepsis caused an inflammatory
response and damage in the liver, which was characterized both
histologically and biochemically. The treatment with Xuebijing
injection ameliorated the pathological changes in liver tissues
caused by sepsis, and also decreased ALT and AST levels in the rats
with septic liver injury.
Evidence indicates that inflammatory cytokines play
an important role in sepsis; pro-inflammatory cytokines and
anti-inflammatory cytokines counteract each other and reach an
immunological equilibrium, which leads to various types of tissue
damage and organ injury (8). In the
present study, elevated TNF-α, IL-6 and IL-10 levels were observed
in the livers of rats in the CLP group in comparison with those in
the control group, which is consistent with previous studies
(27,28). Moreover, Xuebijing injection has been
found to reduce the secretion of TNF-α and IL-6 by Kupffer cells in
livers of rats with heart stroke (29), and promote IL-10 expression in
rabbits with oleic acid-induced acute lung injury (30). The present study found that Xuebijing
injection significantly downregulated pro-inflammatory cytokine
levels, specifically TNF-α and IL-6, while upregulating the levels
of the anti-inflammatory cytokine IL-10 in rats with septic liver
injury. These data suggest that the protective effects of Xuebijing
injection on septic liver injury may occur via the regulation of
the secretion of inflammatory cytokines.
Cytokine signaling induces SOCS1, a protein that can
inhibit the signaling pathways that stimulated its production
(31,32). SOCS-1 is a negative-feedback
regulator not only in the JAK-STAT pathway but also in the
lipopolysaccharide-nuclear factor-κB (LPS-NF-κB) signaling pathway
(33). SOCS-1 has been found to
inhibit cytokine signaling in all systems tested, including TNF-α
and IL-6 (34). TNF-α-mediated
inflammatory signals can be transduced through the JAK-STAT pathway
(35,36). The results of the present study
demonstrated that SOCS-1 expression was upregulated by Xuebijing
injection, which corresponded with its relieving effects on
inflammatory response and liver injury. Collectively, those results
indicate that Xuebijing injection ameliorates liver injury in
CLP-induced septic rats by promoting SOCS-1 expression at the
protein and mRNA levels.
In summary, the present study demonstrated that
Xuebijing injection can effectively alleviate liver injury in a rat
model of CLP-induced sepsis. The protective effects of Xuebijing
injection on septic liver injury are associated with the regulation
of inflammatory cytokine secretions and the promotion of SOCS1
expression. This study provides valuable insights into the role of
Xuebijing injection in septic liver injury, and reveals its
therapeutic potential in CLP-induced liver injury treatment.
Acknowledgements
This study was supported by grants from the China
Postdoctoral Science Foundation (2013M541707), Jiangsu Postdoctoral
Science Foundation, Natural Science Fund Project in Zhejiang
Province (Y2100917) and Nantong Science and Technology Project
(HS149095, HS149137 and HS2014075).
Glossary
Abbreviations
Abbreviations:
|
SOCS
|
suppressors of cytokine signaling
|
|
TNF-α
|
tumor necrosis factor-α
|
|
NF-κB
|
nuclear factor κB
|
|
IL-6
|
interleukin-6
|
|
IL-10
|
interleukin-10
|
|
SIRS
|
systemic inflammatory response
syndrome
|
|
CLP
|
cecal ligation and puncture
|
|
ALT
|
alanine aminotransferase
|
|
AST
|
aspartate aminotransferase
|
|
RT-qPCR
|
reverse transcription-quantitative
polymerase chain reaction
|
|
ELISA
|
enzyme-linked immunosorbent assay
|
|
JAK-STAT
|
janus kinase-signal transducer and
activator of transcription
|
|
LPS-NF-κB
|
lipopolysaccharide-nuclear
factor-κB
|
References
|
1
|
Jones AE and Puskarich MA: The surviving
sepsis campaign guidelines 2012: Update for emergency physicians.
Ann Emerg Med. 63:35–47. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hotchkiss RS and Karl IE: The
pathophysiology and treatment of sepsis. N Engl J Med. 348:138–150.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abraham E and Singer M: Mechanisms of
sepsis-induced organ dysfunction. Crit Care Med. 35:2408–2416.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Spapen H: Liver perfusion in sepsis,
septic shock, and multiorgan failure. Anat Rec (Hoboken).
291:714–720. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Regel G, Grotz M, Weltner T, Sturm JA and
Tscherne H: Pattern of organ failure following severe trauma. World
J Surg. 20:422–429. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dhainaut JF, Marin N, Mignon A and
Vinsonneau C: Hepatic response to sepsis: Interaction between
coagulation and inflammatory processes. Crit Care Med. 29(Suppl 7):
S42–S47. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang JM and An J: Cytokines, inflammation
and pain. Int Anesthesiol Clin. 45:27–37. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schulte W, Bernhagen J and Bucala R:
Cytokines in sepsis: Potent immunoregulators and potential
therapeutic targets-an updated view. Mediators Inflamm.
2013:1659742013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Friedman G, Jankowski S, Marchant A,
Goldman M, Kahn RJ and Vincent JL: Blood interleukin 10 levels
parallel the severity of septic shock. J Crit Care. 12:183–187.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Villarino AV, Kanno Y, Ferdinand JR and
O'Shea JJ: Mechanisms of Jak/STAT signaling in immunity and
disease. J Immunol. 194:21–27. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Alexander WS: Suppressors of cytokine
signalling (SOCS) in the immune system. Nat Rev Immunol. 2:410–416.
2002.PubMed/NCBI
|
|
12
|
Yamana J, Yamamura M, Okamoto A, Aita T,
Iwahashi M, Sunahori K and Makino H: Resistance to IL-10 inhibition
of interferon gamma production and expression of suppressor of
cytokine signaling 1 in CD4+T cells from patients with rheumatoid
arthritis. Arthritis Res Ther. 6:R567–R577. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Egan PJ, Lawlor KE, Alexander WS and Wicks
IP: Suppressor of cytokine signaling-1 regulates acute inflammatory
arthritis and T cell activation. J Clin Invest. 111:915–924. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Starr R, Metcalf D, Elefanty AG, Brysha M,
Willson TA, Nicola NA, Hilton DJ and Alexander WS: Liver
degeneration and lymphoid deficiencies in mice lacking suppressor
of cytokine signaling-1. Proc Natl Acad Sci USA. 95:14395–14399.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Johnson TS, O'Leary M, Justice SK, Maamra
M, Zarkesh-Esfahani SH, Furlanetto R, Preedy VR, Hinds CJ, El Nahas
AM and Ross RJ: Differential expression of suppressors of cytokine
signalling genes in response to nutrition and growth hormone in the
septic rat. J Endocrinol. 169:409–415. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chen S, Dai G, Hu J, Rong A, Lv J, Su L
and Wu X: Discovery of Xuebijing injection exhibiting protective
efficacy on sepsis by inhibiting the expression of HMGB1 in septic
rat model designed by cecal ligation and puncture. Am J Ther. Aug
25–2015.(Epub ahead of print). View Article : Google Scholar
|
|
17
|
Yin Q and Li C: Treatment effects of
Xuebijing injection in severe septic patients with disseminated
intravascular coagulation. Evid Based Complement Alternat Med.
2014:9492542014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
He XD, Wang Y, Wu Q, Wang HX, Chen ZD,
Zheng RS, Wang ZS, Wang JB and Yang Y: Xuebijing protects rats from
sepsis challenged with Acinetobacter baumannii by promoting annexin
A1 expression and inhibiting proinflammatory cytokines secretion.
Evid Based Complement Alternat Med. 2013:8049402013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Liu MW, Wang YH, Qian CY and Li H:
Xuebijing exerts protective effects on lung permeability leakage
and lung injury by upregulating Toll-interacting protein expression
in rats with sepsis. Int J Mol Med. 34:1492–1504. 2014.PubMed/NCBI
|
|
20
|
Rittirsch D, Huber-Lang MS, Flierl MA and
Ward PA: Immunodesign of experimental sepsis by cecal ligation and
puncture. Nat Protoc. 4:31–36. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yu B, Xu P, Zhao Z, Cai J, Sternberg P and
Chen Y: Subcellular distribution and activity of mechanistic target
of rapamycin in aged retinal pigment epithelium. Invest Ophthalmol
Vis Sci. 55:8638–8650. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yang Y, Dou SX, Ren H, Wang PY, Zhang XD,
Qian M, Pan BY and Xi XG: Evidence for a functional dimeric form of
the PcrA helicase in DNA unwinding. Nucleic Acids Res.
36:1976–1989. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yang Y, Dou SX, Xu YN, Bazeille N, Wang
PY, Rigolet P, Xu HQ and Xi XG: Kinetic mechanism of DNA unwinding
by the BLM helicase core and molecular basis for its low
processivity. Biochemistry. 49:656–668. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Adrie C and Pinsky MR: The inflammatory
balance in human sepsis. Intensive Care Med. 26:364–375. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Koskinas J, Gomatos IP, Tiniakos DG, Memos
N, Boutsikou M, Garatzioti A, Archimandritis A and Betrosian A:
Liver histology in ICU patients dying from sepsis: A
clinico-pathological study. World J Gastroenterol. 14:1389–1393.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhu W, Bao R, Fan X, Tao T, Zhu J, Wang J,
Li J, Bo L and Deng X: PD-L1 blockade attenuated sepsis-induced
liver injury in a mouse cecal ligation and puncture model. Mediat
Inflamm. 2013:3615012013. View Article : Google Scholar
|
|
28
|
Zhang H, Wang W, Fang H, Yang Y, Li X, He
J, Jiang X, Wang W, Liu S, Hu J, et al: GSK-3β inhibition
attenuates CLP-induced liver injury by reducing inflammation and
hepatic cell apoptosis. Mediators Inflamm. 2014:6295072014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen Y, Tong H, Zhang X, Tang L, Pan Z,
Liu Z, Duan P and Su L: Xuebijing injection alleviates liver injury
by inhibiting secretory function of Kupffer cells in heat stroke
rats. J Tradit Chin Med. 33:243–249. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang Y, Ji M, Wang L, Chen L and Li J:
Xuebijing injection improves the respiratory function in rabbits
with oleic acid-induced acute lung injury by inhibiting IL-6
expression and promoting IL-10 expression at the protein and mRNA
levels. Exp Ther Med. 8:1593–1598. 2014.PubMed/NCBI
|
|
31
|
Chung CS, Chen Y, Grutkoski PS, Doughty L
and Ayala A: SOCS-1 is a central mediator of steroid-increased
thymocyte apoptosis and decreased survival following sepsis.
Apoptosis. 12:1143–1153. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Davey G, Heath W and Starr R: SOCS1: A
potent and multifaceted regulator of cytokines and cell-mediated
inflammation. Tissue Antigens. 67:1–9. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Shuai K and Liu B: Regulation of JAK-STAT
signalling in the immune system. Nat Rev Immunol. 3:900–911. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Fujimoto M and Naka T: Regulation of
cytokine signaling by SOCS family molecules. Trends Immunol.
24:659–666. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Guo D, Dunbar JD, Yang CH, Pfeffer LM and
Donner DB: Induction of Jak/STAT signaling by activation of the
type 1 TNF receptor. J Immunol. 160:2742–2750. 1998.PubMed/NCBI
|
|
36
|
Miscia S, Marchisio M, Grilli A, Di
Valerio V, Centurione L, Sabatino G, Garaci F, Zauli G, Bonvini E
and Di Baldassarre A: Tumor necrosis factor alpha (TNF-alpha)
activates Jak1/Stat3-Stat5B signaling through TNFR-1 in human B
cells. Cell Growth Differ. 13:13–18. 2002.PubMed/NCBI
|