Introduction
Cesarean section rates have been increasing
worldwide, particularly in Asian countries, and accordingly, there
has been demand for improved healthcare for maternal females
undergoing cesarean section (1).
Post-cesarean analgesia has an important role in the entire
analgesia, not only improving the subjective pain, but also
accelerating post-operative recovery and reducing the incidence of
venous thrombosis (2). Multiple
modes of analgesia are available for cesarean section, including
epidural analgesia, peripheral nerve blocks, oral painkillers and
intravenous morphine. Despite its high efficacy, epidural analgesia
is usually terminated immediately after the surgery, and its
residual effect gradually disappears within 24 h (3). Subsequent to termination of epidural
anesthesia, other methods of analgesia must be selected, while
intravenous morphine is less preferred due to its adverse effects
(4).
With the application of ultrasound guidance, local
nerve block has recently gained worldwide popularity. Transversus
abdominis plane block (TAPB) is a regional analgesic technique
applied in post-operative analgesia for lower abdominal surgeries.
Numerous studies have demonstrated that TAPB reduces post-operative
opioid consumption and opioid-associated side effects.
Iliohypogastric/ilioinguinal block (IHINB) is another means of
post-operative analgesia for lower abdominal surgeries (5). IHINB is also proven to be effective in
reducing cumulative morphine consumption but not the side effects
(6). Various studies have compared
the analgesic effects of TAPB and IHINB in abdominal surgeries,
including inguinal hernia repair (7–9).
However, they are limited to a relatively small sample size and the
results are inconsistent. Furthermore, previously provided evidence
for comparing the analgesic effects and complications between TAPB
and IHINB in cesarean section is limited. In the present study, by
retrospectively collecting clinical data of propensity-matched
maternal females undergoing cesarean section, the analgesic effects
and complications of TAPB and IHINB were compared.
Materials and methods
Patients
The clinical data of 368 maternal females who
underwent cesarean section at Yueqing Third People's Hospital
(Yueqing, China) between June 2016 and June 2017 were
retrospectively collected. The inclusion criteria were as follows:
i) Cesarean section under epidural analgesia; ii) peripheral nerve
block, including TAPB or IHINB; iii) age of 18–40 years; iv) ASA
grade I or II according to the American Society of
Anesthesiologists (ASA) classification (10); v) complete data of pain evaluation,
morphine request and consumption. A total of 242 patients met the
above criteria, and after the propensity score match, 124 patients
were finally included in the study, who were divided into the TAPB
group and the IHINB group according to their post-operative
analgesic treatment modality. The study design is presented in the
flow chart in Fig. 1.
Demographic characteristics and clinical data of the
subjects were collected from the electronic database of the
hospital for analysis, with written informed consent provided by
the patients on admission for inclusion of their data in scientific
studies. The present study was approved by the Medical Ethics
Committee of Yueqing Third People's Hospital (Yueqing, China).
Anesthesia
All patients were given combined spinal-epidural
anesthesia in the operating room, with monitoring of arterial blood
pressure, electrocardiogram and peripheral pulse oximetry
performed. The patients were placed in the left lateral decubitus
position, and epidural anesthesia was given by a
needle-through-needle technique at the L3/4 interspace. The first
dose of intrathecal hyperbaric bupivacaine (12 mg) and fentanyl (10
µg) was injected, and an epidural catheter was then secured 4–5 cm
into the epidural space. If hypesthesia to ice up to Th4 was not
achieved, incremental doses of 5 ml 2% lidocaine were administered
into the epidural space. At the time of closing the peritoneum, 2
mg morphine hydrochloride with 5 ml saline was administered through
the epidural catheter.
Post-operative analgesia
As previously described, TAPB or IHINB was performed
after the surgery (11,12). For TAPB, the skin was first prepared
with an antiseptic solution. The convex 3.5-MHz ultrasound probe
(Sonosite EDGE Portable Ultrasound System; SonoSite) was
transversally placed on the anterior axillary line halfway between
the costal margin and the iliac crest and then moved toward the
navel until the three layers of muscles (external and internal
oblique muscles and transversus abdominis muscle), the peritoneum
and intraperitoneal structures were clearly visible. Under the
guidance of ultrasound, the 22G 100-mm echo-lucent needle was
chosen and then inserted posteriorly into the transversus abdominis
fascial plane. A test injection of 1–2 ml glucose was given to
confirm the correct position of the block needle in the transversus
abdominis fascial plane. After the confirmation, 20 ml 0.375%
ropivacaine or 0.3% levobupivacaine (decided by the
anesthesiologists according to their preference) was injected into
the fascial plane on each side in 5-ml increments after
aspiration.
For IHINB, the convex 3.5-MHz ultrasound probe
(Sonosite EDGE Portable Ultrasound System; SonoSite) was placed on
the line between the anterior superior iliac spine and the
umbilicus, where 3 layers of muscles (extra-abdominal oblique,
intra-abdominal oblique and transverse abdominis) were visible on
the inner side of the anterior superior iliac spine.
The inferior tibiofibular and iliac crest nerves
were identified between the abdominal oblique muscle and the
transverse abdominis muscle. Under the guidance of ultrasound, the
22G 100-mm echo-lucent needle was selected and then inserted next
to the iliohypogastric/ilioinguinal nerve. The dose and selection
of local anesthetics were the same as those used for TAPB.
All patients were given a standardized
patient-controlled intravenous analgesia (PCIA) regimen. The
disposable PCIA device (Coopdech Syrinjector PCA set; Daiken
Medical) contained 30 mg morphine in 45 ml saline. Patients were
instructed on how to use the PCIA device, which was set with a
bolus of 2 mg morphine and a minimum interval of 30 min. In
addition, the first time of using PCIA was recorded in hospital
documents. If the analgesic effect was not satisfactory,
complementary use of intravenous morphine was applied.
Data collection
Demographics and clinical characteristics, including
age, gender, body mass index, level of education and ASA grade were
all collected from the electric database of the hospital. The time
to first request of morphine, visual analog scale (VAS) score and
dose of morphine used after the surgery were also recorded. The VAS
score and dose of morphine were evaluated at different time-points
after surgery. The VAS score was determined using a 10-cm scale to
represent the extent of pain, with 0 points resembling no pain and
10 points indicating the most severe pain imaginable.
Statistical analysis
In the present study, SPSS version 19.0 (IBM Corp.,
Armonk, NY, USA) was used for statistical analysis. Continuous
variables meeting the criteria for normal distribution were
expressed as the mean ± standard deviation and categorical
variables were presented as proportions. The propensity score was
calculated using multivariate logistic regression, taking into
account demographical and clinical variables. Patients with the
highest similarity in propensity scores were matched using the
‘greedy match’ method. Following the propensity score matching, a
normal distribution test using the Kolmogorov-Smirnov method was
adopted for all variables. Continuous data meeting the normal
distribution criteria were analyzed using Student's t-test, while
those not meeting those criteria were assessed with a
non-parametric Mann-Whitney U-test. The χ2 test was
adopted for categorical variables in the analysis.
As for the Kaplan-Meier analysis, the Cox
proportional hazard model was adopted as the regression method to
compare the relative hazard ratio of morphine requests for various
covariates, while Kaplan-Meier curves and log-rank tests were used
for comparing the time to first request of morphine between the
groups. P<0.05 was considered to indicate statistical
significance.
Results
Demographic and clinical
characteristics
As presented in Table
I, there were significant differences between the TAPB group
and the IHINB group in age (P=0.013) and education (P=0.009) prior
to the propensity match. However, these differences were eliminated
by screening the patients by means of propensity score match.
Table II indicates that after the
match, there was no difference between the two groups in
demographics and clinical characteristics (all P>0.05).
Furthermore, the local anesthetics used in the different groups
were similar (P=0.206).
 | Table I.Demographical and clinical
characteristics of all maternal females undergoing cesarean section
prior to propensity match. |
Table I.
Demographical and clinical
characteristics of all maternal females undergoing cesarean section
prior to propensity match.
| Variables | TAPB group
(n=122) | IHINB group
(n=120) | t/χ2 | P-value |
|---|
| Demographics |
|
|
|
|
| Age
(years) |
28.0±4.2 |
29.3±4.2 |
2.497 | 0.013 |
| Weight
(kg) |
78.8±12.5 |
80.8±12.7 |
1.249 | 0.213 |
| Height
(cm) | 160.2±5.8 | 160.5±5.7 |
0.274 | 0.784 |
| BMI
(kg/m2) |
30.8±5.1 |
31.5±5.5 |
1.139 | 0.256 |
| Education |
|
| 11.564 | 0.009 |
|
Illiteracy | 28 (23.0) | 37 (21.7) |
|
|
|
Elementary school | 36 (29.5) | 47 (13.3) |
|
|
| High
school | 33 (27.0) | 36 (31.7) |
|
|
| College
or higher | 25 (20.5) | 22 (33.3) |
|
|
| ASA grade |
|
|
0.081 | 0.775 |
| I | 71 (58.2) | 72 (60.0) |
|
|
| II | 51 (41.8) | 48 (40.0) |
|
|
| Local
anesthetics |
|
|
3.096 | 0.078 |
|
Ropivacaine | 91 (74.6) | 77 (64.2) |
|
|
|
Levobupivacaine | 31 (25.4) | 43 (35.8) |
|
|
| Gestational week |
38.5±1.8 |
38.6±1.6 |
0.605 | 0.546 |
 | Table II.Demographical and clinical
characteristics of propensity scoring-matched maternal females
undergoing cesarean section. |
Table II.
Demographical and clinical
characteristics of propensity scoring-matched maternal females
undergoing cesarean section.
| Variables | TAPB group
(n=62) | IHINB group
(n=62) | t/χ2 | P-value |
|---|
| Demographics |
|
|
|
|
| Age
(years) |
28.2±3.3 |
28.6±3.8 | 0.586 | 0.559 |
| Weight
(kg) |
81.7±12.4 |
80.2±10.7 | 0.698 | 0.487 |
| Height
(m) | 160.0±5.8 | 161.0±5.6 | 1.021 | 0.309 |
| BMI
(kg/m2) |
32.0±5.4 |
31.0±4.6 | 1.083 | 0.281 |
| Education |
|
| 1.382 | 0.710 |
|
Illiteracy | 19 (30.6) | 16 (25.8) |
|
|
|
Elementary school | 10 (16.1) | 9
(14.5) |
|
|
| High
school | 16 (25.8) | 22 (35.5) |
|
|
| College
or higher | 17 (27.4) | 15 (24.2) |
|
|
| ASA grade |
|
| 0.132 | 0.716 |
| I | 37 (59.7) | 35 (56.5) |
|
|
| II | 25 (40.3) | 27 (43.5) |
|
|
| Local
anesthetics |
|
| 1.601 | 0.206 |
|
Ropivacaine | 31 (50.0) | 38 (61.3) |
|
|
|
Levobupivacaine | 31 (50.0) | 24 (38.7) |
|
|
| Gestational
week |
38.5±1.8 |
38.5±1.6 | 0.159 | 0.874 |
Time to first morphine request
The Kaplan-Meier curves depicting the time to first
morphine request in the two groups are provided in Fig. 2. Although the mean value in the TAPB
group was lower than that in the IHINB group (1,327±960 vs.
1,504±834 min), the log-rank test demonstrated that there was no
significant difference (P=0.575).
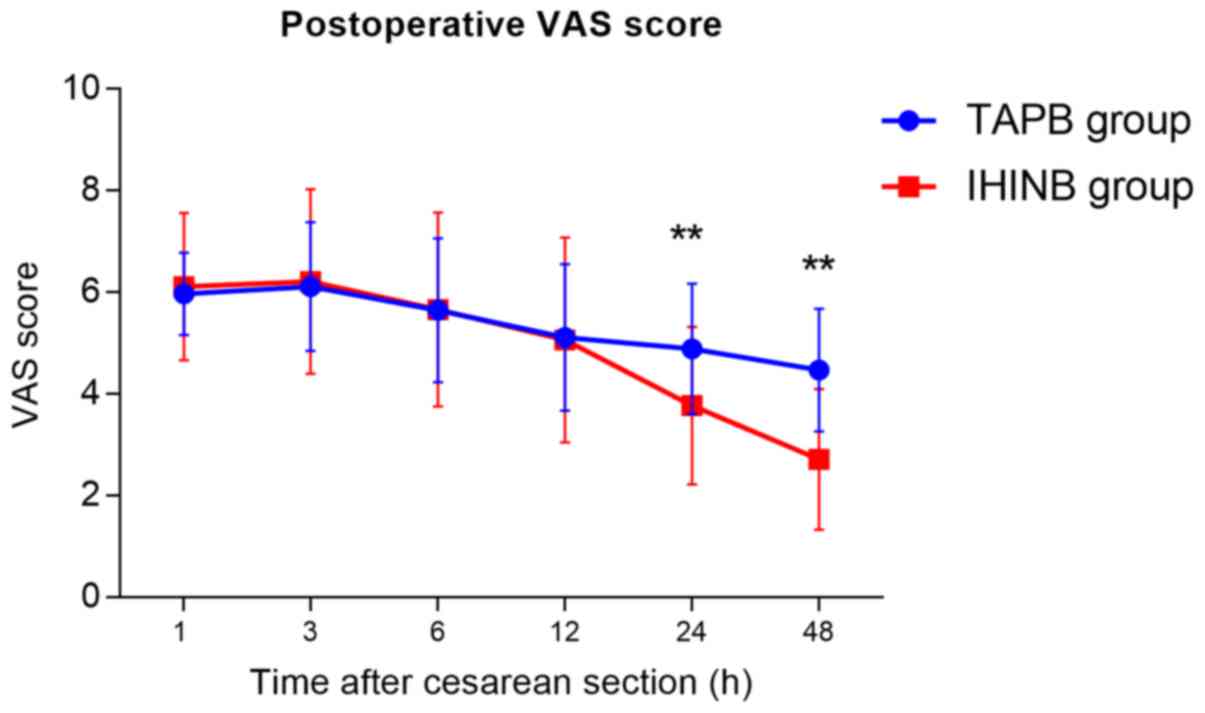
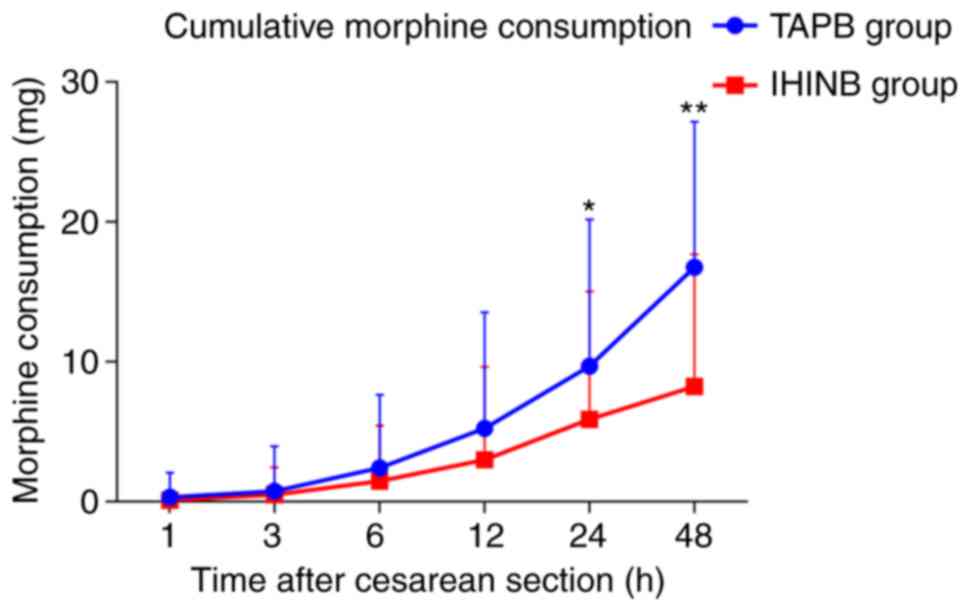
VAS score and cumulative morphine
consumption
The VAS score and cumulative morphine consumption
were compared between the two groups. As for the VAS score, there
was no significant difference between the two groups in the first
12 h (all P>0.05). However, the VAS score of the IHINB group was
significantly lower than that of the TAPB group at 24 and 48 h
after the surgery (P<0.001 for each; Fig. 3). Similar to the VAS score, the total
cumulative morphine consumption in the two groups was comparable at
12 h, while it was significantly lower for the IHINB group at 24
and 48 h after the surgery (P<0.05 and P<0.001 respectively;
Fig. 4).
Risk factors for post-operative
analgesia
A Cox regression analysis was performed to determine
the major risk factors for the analgesic effect in cesarean section
patients, (Table III). Uni- and
multivariate analysis demonstrated that the patient age and
education level were independent risk factors for the time to first
morphine request. However, the mode of post-operative analgesia
(TAPB or IHINB) was not a significant risk factor (P=0.628). In
addition, the type of local anesthetic was not an independent risk
factor (P=0.441).
 | Table III.Cox regression analysis of the
association of covariates with the time to first morphine
request. |
Table III.
Cox regression analysis of the
association of covariates with the time to first morphine
request.
|
| Univariate | Multivariate |
|---|
|
|
|
|
|---|
| Covariates | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age (years) | 0.914 | 0.866–0.965 |
0.001 | 0.927 | 0.876–0.980 | 0.008 |
| Weight (kg) | 1.007 | 0.990–1.023 |
0.429 | NA | NA | NA |
| Height (m) | 1.009 | 0.976–1.043 |
0.591 | NA | NA | NA |
| BMI
(kg/m2) | 1.009 | 0.972–1.047 |
0.654 | NA | NA | NA |
| Educationa |
|
Illiteracy | NA | NA | NA | NA | NA | NA |
|
Elementary school | 2.973 | 1.578–5.600 |
0.001 | 3.078 | 1.628–5.819 |
0.001 |
| High
school | 2.760 | 1.630–4.675 | <0.001 | 2.662 | 1.569–4.516 | <0.001 |
| College
or higher | 3.132 | 1.799–5.454 | <0.001 | 2.666 | 1.506–4.719 |
0.001 |
| ASA grade | 1.119 | 0.767–1.631 |
0.561 | NA | NA | NA |
| Local anesthetics
(levobupivacaine vs. ropivacaine) | 0.862 | 0.591–1.257 |
0.441 | NA | NA | NA |
| Gestational
week | 1.099 | 0.982–1.230 |
0.102 | 1.037 | 0.924–1.163 |
0.539 |
| Post-operative
analgesic (TAPB vs. IHINB) | 0.898 | 0.617–1.308 |
0.575 | 0.910 | 0.622–1.332 |
0.628 |
Side effects of post-operative
analgesia
Table IV presents
the prevalence of common adverse events of post-operative analgesia
in the groups, including hypotension, bradycardia, arrhythmia,
nausea, vomiting, pruritus and urinary retention. Statistical
analysis indicated that no significant difference in any of the
adverse events was present between the two groups (all
P>0.05).
 | Table IV.Adverse events of analgesia in the
two groups. |
Table IV.
Adverse events of analgesia in the
two groups.
| Complication | TAPB group
(n=62) | IHINB group
(n=62) | χ2 | P-value |
|---|
| Hypotension | 7
(11.3) | 10 (16.1) | 0.614 |
0.603 |
| Bradycardia | 3 (4.8) | 4 (6.5) | 0.151 | >0.999 |
| Arrhythmia | 0 (0.0) | 2 (3.2) | 2.033 |
0.496 |
| Nausea | 12 (19.4) | 7
(11.3) | 1.554 |
0.319 |
| Vomiting | 7
(11.3) | 8
(12.9) | 0.076 |
1.000 |
| Urinary
retention | 10 (16.1) | 18 (29.0) | 2.952 |
0.132 |
| Pruritus | 32 (51.6) | 35 (56.5) | 0.292 |
0.589 |
| Total | 47 (75.8) | 48 (77.4) | 0.045 |
0.832 |
Discussion
The present study retrospectively compared the
clinical data of cesarean section patients who received TAPB or
IHINB for post-operative analgesia. By using propensity score
matching, the differences in demographics and baseline
characteristics were eliminated, which made the results more
convincing. The results indicated that the analgesic effect of TAPB
and IHINB was similar, but IHINB had a stronger effect a 24 h after
the surgery.
The application of ultrasound in local nerve block
may significantly increase the accuracy of punctuation and decrease
the incidence of adverse events, which promotes the use of nerve
block in post-operative analgesia (13). In the present cohort, nerve block was
successfully performed in all cases without any complications. As
for the selection of local anesthetics, a randomized controlled
study indicated that levobupivacaine was more potent than
ropivacaine in peripheral nerve block to a certain extent (14). Either levobupivacaine or ropivacaine
was used in the present study, which depended on the
anesthesiologists' judgement. However, the proportions of patients
using either of the two different local anesthetics were similar
between the two groups, while the Cox regression analysis also
indicated that the type of local anesthetic had no significant
effect on the time to first request of morphine. A number of
studies have demonstrated that combination of local nerve block in
postoperative analgesia may significantly enhance the analgesic
effect and reduce the usage of morphine for patients undergoing
cesarean section (5,11,15,16).
TAPB, which was first described by McDonnell and
Laffey (17), blocks sensory nerves
that supply the anterior abdominal wall by deposition of local
anesthetics. When the needle is advanced across the neurofascial
planes of the anterior abdominal wall, the TAPB significantly
enhances the analgesic effect (18).
However, Lee et al (19)
indicated that the major targets of TAPB were T10-T12 nerves, while
the L1 nerve was merely blocked in half of the cases. The major
reasons for this unsatisfactory effect of TAPB on the L1 nerve may
be attributed to its varied anatomical pathways (20). However, the sensory nerve dominating
the pain stimulus of uterine incision for cesarean section is the
segment of the T12 and L1 nerves, while the
iliohypogastric/ilioinguinal nerve are major branches of the L1
nerve. Furthermore, TAP block is a field block while IHINB is a
truncal block. Hence, it was hypothesized that IHINB had a better
effect than TAPB. A prospective randomized controlled open-label
study led by Okur et al (21)
compared the postoperative analgesic effect of TAPB and IHINB in
patients undergoing inguinal herniorrhaphy with spinal anesthesia,
revealing that TAPB and IHINB have a better effect than the
controls using morphine only, and the time to first request of
morphine in patients with the IHINB was shorter than the other two
groups (21). However, TAPB and
IHINB as post-operative analgesia for cesarean section has been
rarely reported (5). Similar results
from the study by Okur et al (21) were obtained in the present study,
with the analgesic effect of TAPB and IHINB being comparable after
the first 12 h. However, better analgesia was achieved in the IHINB
group than that in the TAPB group after 24 h, with a lower VAS
score and morphine consumption. Of note, multiple modes of
analgesia in addition to local nerve block must be given for
patients undergoing cesarean section, since the pain is a
combination of somatic pain and visceral pain (22). TAPB and IHINB only block the somatic
pain, while the visceral pain should be relieved by other methods,
including intravenous morphine by PCIA. The common associated
adverse events of TAPB and IHINB were also compared in the present
study, with no statistical difference observed between the two
groups, which was in accordance with other studies (9,23,24).
Several limitations of the present study must be
noted. First, although a propensity score match was performed, the
present retrospective study inevitably had shortcomings of
non-randomization, incomplete clinical data and retrospective
analysis, which limited the power of evidence. Furthermore, the
sample size may have been insufficient to determine the difference
of major outcomes and potential adverse events, and future studies
with larger cohorts should be performed for further elucidation.
Finally, the dosage data of local anesthetics were missing, and it
was therefore impossible to compare them between the two groups,
while it was previously demonstrated that IHINB required less
anesthetics than TAPB (25).
In summary, TAPB and IHINB were comparable at
providing satisfactory post-operative analgesia and reducing
morphine consumption for maternal females after cesarean section;
however, IHINB had a better effect at 24 h after the surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed are available from
the corresponding author on reasonable request.
Authors' contributions
YJ and MY designed and led the current study. YL, SZ
and GZ collected and analyzed the general patient data. YJ and YL
wrote the manuscript and MY revised it. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Medical Ethics
Committee of Yueqing Third People's Hospital (Yueqing, China). The
patients provided written informed consent regarding the use of
their data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lumbiganon P, Laopaiboon M, Gülmezoglu AM,
Souza JP, Taneepanichskul S, Ruyan P, Attygalle DE, Shrestha N,
Mori R, Nguyen DH, et al World Health Organization Global Survey on
Maternal and Perinatal Health Research Group, : Method of delivery
and pregnancy outcomes in Asia: The WHO global survey on maternal
and perinatal health 2007–08. Lancet. 375:490–499. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wagner M: Epidural analgesia and risk of
caesarean section. Lancet. 353:5941999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hawkins JL: Epidural analgesia for labor
and delivery. N Engl J Med. 362:1503–1510. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
El Aish KA, Tafish R and Zourob H:
Morphine versus fentanyl for spinal post-caesarean analgesia: A
randomised controlled trial. Lancet. 391 (Suppl 2):S202018.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gucev G, Yasui GM, Chang TY and Lee J:
Bilateral ultrasound-guided continuous ilioinguinal-iliohypogastric
block for pain relief after cesarean delivery. Anesth Analg.
106:1220–1222, table of contents. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bell EA, Jones BP, Olufolabi AJ, Dexter F,
Phillips-Bute B, Greengrass RA, Penning DH and Reynolds JD; Duke
Women's Anesthesia Research Group, : Iliohypogastric-ilioinguinal
peripheral nerve block for post-Cesarean delivery analgesia
decreases morphine use but not opioid-related side effects. Can J
Anaesth. 49:694–700. 2002.(In English, French). View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kamal K, Jain P, Bansal T and Ahlawat G: A
comparative study to evaluate ultrasound-guided transversus
abdominis plane block versus ilioinguinal iliohypogastric nerve
block for post-operative analgesia in adult patients undergoing
inguinal hernia repair. Indian J Anaesth. 62:292–297. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bhatia N, Sen IM, Mandal B and Batra A:
Postoperative analgesic efficacy of ultrasound-guided
ilioinguinal-iliohypogastric nerve block compared with medial
transverse abdominis plane block in inguinal hernia repair: A
prospective, randomised trial. Anaesth Crit Care Pain Med.
38:41–45. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sujatha C, Zachariah M, Ranjan RV, George
SK, Ramachandran TR and Pillai AR: Transversus Abdominis Plane
Block versus Ilioinguinal/Iliohypogastric Nerve Block with Wound
Infiltration for Postoperative Analgesia in Inguinal Hernia
Surgery: A Randomized Clinical Trial. Anesth Essays Res.
11:976–980. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kiefer N, Krahe S, Gembruch U and Weber S:
Ultrasound anatomy of the transversus abdominis plane region in
pregnant women before and after cesarean delivery. BMC Anesthesiol.
16:1262016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tan TT, Teoh WH, Woo DC, Ocampo CE, Shah
MK and Sia AT: A randomised trial of the analgesic efficacy of
ultrasound-guided transversus abdominis plane block after caesarean
delivery under general anaesthesia. Eur J Anaesthesiol. 29:88–94.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sakalli M, Ceyhan A, Uysal HY, Yazici I
and Başar H: The efficacy of ilioinguinal and iliohypogastric nerve
block for postoperative pain after caesarean section. J Res Med
Sci. 15:6–13. 2010.PubMed/NCBI
|
|
13
|
Kagwa S, Hoeft MA, Firth PG, Ttendo S and
Modest VE: Ultrasound guided transversus abdominis plane versus
sham blocks after caesarean section in an Ugandan village hospital:
A prospective, randomised, double-blinded, single-centre study.
Lancet. 385 (Suppl 2):S362015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li A, Wei Z, Liu Y, Shi J, Ding H, Tang H,
Zheng P, Gao Y and Feng S: Ropivacaine versus levobupivacaine in
peripheral nerve block: A PRISMA-compliant meta-analysis of
randomized controlled trials. Medicine (Baltimore). 96:e65512017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Champaneria R, Shah L, Wilson MJ and
Daniels JP: Clinical effectiveness of transversus abdominis plane
(TAP) blocks for pain relief after caesarean section: A
meta-analysis. Int J Obstet Anesth. 28:45–60. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fusco P, Cofini V, Petrucci E, Scimia P,
Pozone T, Paladini G, Carta G, Necozione S, Borghi B and
Marinangeli F: Transversus Abdominis Plane Block in the Management
of Acute Postoperative Pain Syndrome after Caesarean Section: A
Randomized Controlled Clinical Trial. Pain Physician. 19:583–591.
2016.PubMed/NCBI
|
|
17
|
McDonnell JG and Laffey JG: Transversus
abdominis plane block. Anesth Analg. 105:8832007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Onishi Y, Kato R, Okutomi T, Tabata K,
Amano K and Unno N: Transversus abdominis plane block provides
postoperative analgesic effects after cesarean section: Additional
analgesia to epidural morphine alone. J Obstet Gynaecol Res.
39:1397–1405. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee TH, Barrington MJ, Tran TM, Wong D and
Hebbard PD: Comparison of extent of sensory block following
posterior and subcostal approaches to ultrasound-guided transversus
abdominis plane block. Anaesth Intensive Care. 38:452–460. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tran TM, Ivanusic JJ, Hebbard P and
Barrington MJ: Determination of spread of injectate after
ultrasound-guided transversus abdominis plane block: A cadaveric
study. Br J Anaesth. 102:123–127. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Okur O, Tekgul ZT and Erkan N: Comparison
of efficacy of transversus abdominis plane block and
iliohypogastric/ilioinguinal nerve block for postoperative pain
management in patients undergoing inguinal herniorrhaphy with
spinal anesthesia: A prospective randomized controlled open-label
study. J Anesth. 31:678–685. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zwissler B: Regional anesthesia and
analgesia for labor and delivery. N Engl J Med. 348:1818–1820;
author reply 1818–1820. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Mei W, Jin C, Feng L, Zhang Y, Luo A,
Zhang C and Tian Y: Bilateral ultrasound-guided transversus
abdominis plane block combined with ilioinguinal-iliohypogastric
nerve block for cesarean delivery anesthesia. Anesth Analg.
113:134–137. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Coffman JC, Fiorini K, Ristev G, Beeston W
and Small RH: Transversus abdominis plane and
ilioinguinal/iliohypogastric blocks for cesarean delivery in a
patient with type II spinal muscular atrophy. Int J Obstet Anesth.
25:79–81. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Eichenberger U, Greher M, Kirchmair L,
Curatolo M and Moriggl B: Ultrasound-guided blocks of the
ilioinguinal and iliohypogastric nerve: Accuracy of a selective new
technique confirmed by anatomical dissection. Br J Anaesth.
97:238–243. 2006. View Article : Google Scholar : PubMed/NCBI
|