Introduction
Gorham-Stout syndrome (GSS), also named disappearing
bone disease, phantom bone disease or massive osteolysis, is a rare
osteolytic disease resulting from benign lymphovascular
proliferation (1). It was first
described as ‘the boneless arm’ in 1838(2). Since then, only 300 cases have been
reported worldwide. GSS may involve any bone of the body and most
commonly affects the shoulder girdle, pelvis, ribs and skull. Owing
to its rarity and non-specific clinical manifestation, accurate
diagnosis is difficult and usually delayed. The conditions of
certain patients can progress to complete bone destruction, while
those of other patients are self-limiting. Patients with GSS
complicated with spinal involvement or chylothorax usually have
poor prognosis (3). The treatment
options, including surgery, radiotherapy and medical therapy,
remain controversial. Stable spinal lesions may be treated with
conservative treatments, including braces, halo tractions,
radiotherapy and medical therapy (4). To maintain stability and prevent
neurological injury, surgical management is required for unstable
spinal lesions (5). The present
study reports on a case of GSS in a 22-year-old male involving the
C1-T1 vertebrae with bilateral pleural effusion and discusses the
diagnostic characteristics and therapeutic management.
Case report
In July 2017, a 22-year-old male was admitted to a
local hospital with neck pain and limited movement of the neck for
1 month. The relevant medical history of the patient's family was
uneventful and the patient had no history of trauma. A CT scan
revealed multiple osteolysis of the occipital bone and several
cervical vertebrae and thoracic vertebrae with a mildly increased
fluorodeoxyglucose uptake accompanied by an adjacent soft tissue
mass. A needle biopsy of the cervical vertebrae was performed and
the results revealed hyperplasia of the fibrous tissues in the bone
lesions without evidence of malignancy. No definite diagnosis was
made at that time. Considering the complexity and high risk
associated with surgery, the patient underwent irradiation
treatment of the cervical vertebrae once at the local hospital.
At 1 week following radiation treatment, the patient
developed shortness of breath and chest tightness. Chest ultrasound
demonstrated large bilateral pleural effusion. The patient then
presented at the Department of Respiratory and Critical Care
Medicine, Changzheng Hospital (Shanghai, China). On examination,
the patient was conscious but distressed and his neck was
immobilized using a cervical gear. The patient had percussion
dullness, decreased vocal resonance and diminished breath sounds
bilaterally, but no palpable lymph nodes, edema of the lower
extremities or neurological deficits. Laboratory examination,
including routine blood tests, biochemical tests and serum tumor
markers, were normal, except for albumin levels of 25 g/l (normal
range based on observations at Changzheng Hospital, 40-55 g/l).
Radiography revealed marked osteolysis in the occipital bone, as
well as C2-7 and T2 vertebrae (Fig.
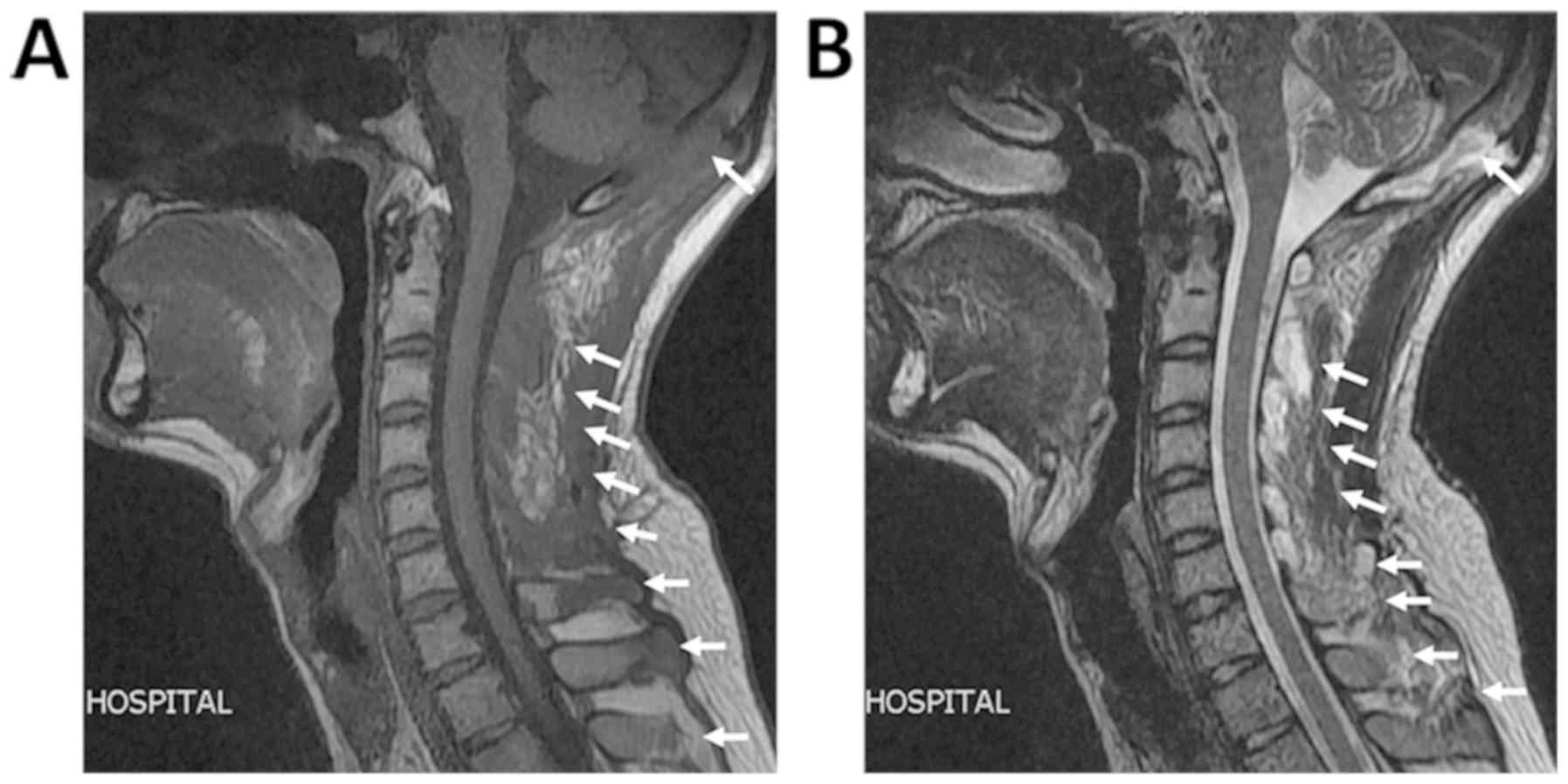
1). On MRI, low signal intensity in the occipital bone and
C1-T1 vertebrae was observed in the T1-weighted images (Fig. 2). The corresponding T2-weighted MRI
revealed an inhomogeneous high signal intensity within the lesions
(Fig. 2). The chest CT scan revealed
a large amount of bilateral pleural effusion (Fig. 3). A chest catheter was inserted to
the right pleural cavity for daily drainage and bloody pleural
fluid was collected for further analysis. To determine the cause of
the bloody pleural effusion, left-sided thoracoscopy was performed,
but no abnormalities were identified. Approximately 1 l of bloody
pleural fluid was drained from the left pleural cavity during
surgery. Pleural effusion samples were gathered from the patient on
the 1st, 2nd and 3rd day
post-surgery. Cytological analysis of the pleural fluid was
performed and the results were negative regarding malignancies. The
patient exhibited a rapid accumulation of pleural fluid within 5
days after thoracoscopy and pleural aspiration yielded a milky
white fluid, which was proven to be chyle via laboratory analysis.
The patient was provided with a low-fat diet and received
intravenous albumin infusion.
Considering the spinal instability caused by
extensive vertebral involvement and the possibility of pathological
fracture, the patient was then transferred to the Department of
Osseous Oncology at Changzheng Hospital for surgical intervention.
The surgery was performed via a posterior approach. During the
surgery, it was observed that the spinous processes of the C2-7
vertebrae had almost disappeared and had manifested as malacia, the
blood supply was highly abundant, multiple vertebral plates and
occipital protuberances were destroyed and chyle outflowed from the
bone lesions. Pedicle screws were then inserted into the pedicles
of the bilateral T3, T1 and C2 vertebrae, left-side T2 and C5
vertebrae and right-side T3 and T7 vertebrae. The remaining pedicle
bones could not be treated in the same way, as they were almost
destroyed. The occipital protuberance was largely destroyed and the
cerebral dura mater was visible; therefore, the damaged bone and
soft tissues were resected and a screw and an internal fixator were
installed in the undamaged occipital cortex. A connecting rod was
fixed to the occipital and bilateral pedicle screws. To relieve the
pressure at the dural sac, the soft tissues behind the C2-7
vertebrae was carefully separated and removed. The spinous
processes and vertebral plates of the T1-3 vertebrae were resected,
the damaged bone was scraped off and a gelatin sponge was inserted
into the site of damage of the T1-3 vertebrae. Histopathological
examination of the excised tissues revealed proliferative fibrous
tissues and numerous thin-walled blood vessels in the affected bone
cavity, without evidence of cellular atypia and osteogenesis
reactions (Fig. 4).
Based on the clinical, radiological and pathological
results, the patient was eventually diagnosed with GSS. The surgery
was effective and no surgery-associated complications were observed
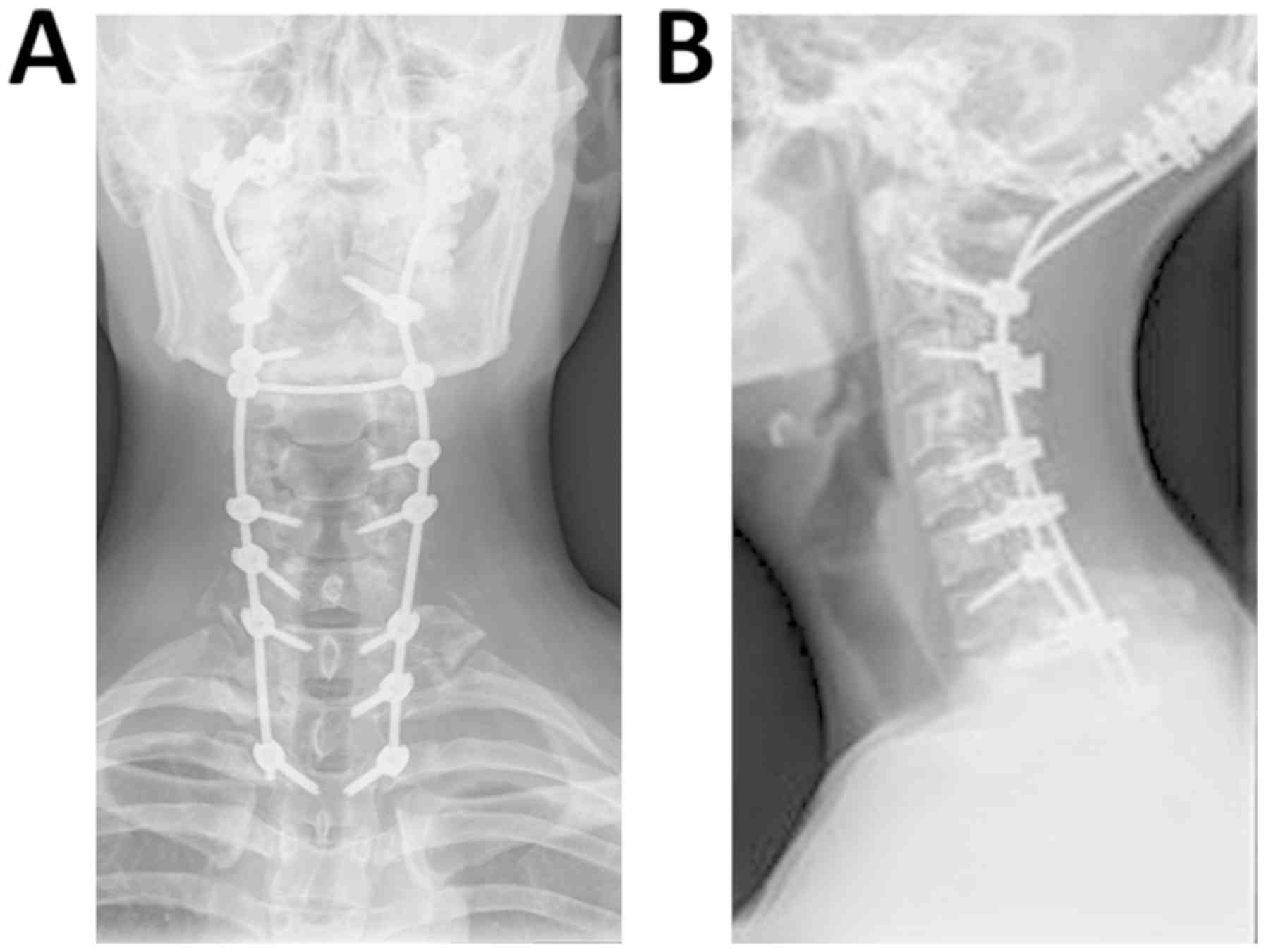
(Fig. 5). Thereafter, the patient
received 4 mg of zoledronic acid by intravenous administration
every 2 months. He was also provided with calcium and vitamin D
supplementation. The pleural effusions gradually decreased after
surgery and the patient was discharged from our hospital at 10 days
post-surgery without any neurological complications. At the
18-month follow-up visit, there was no evidence of new bone
resorption.
Discussion
GSS is a rare osteolytic disease, which has received
substantial attention since it was first described in 1838(6). This disease has no features of
inheritance and may occur at any age, but frequently affects
children or young individuals (7).
The etiology and pathogenesis of GSS remain poorly
understood. Gorham and Stout (6)
speculated that abnormal hyperplasia of vascular tissues in the
bone marrow cavity results in mechanical pressure, local hypoxia
and acidosis, thus leading to bone resorption. Osteolysis was also
thought to correlate with the increased number or enhanced activity
of osteoclasts in bone lesions (8).
Various studies have suggested that perivascular monocytes are
involved in bone resorption (9,10).
Furthermore, the serum levels of basic fibroblast growth factor,
vascular endothelial growth factor (VEGF)-A, VEGF-C and
interleukin-8 were found to be markedly elevated in certain
patients, indicating their potential roles in GSS (11,12).
In 1983, Heffez et al (13) put forward 8 diagnostic criteria for
GSS: i) Positive biopsy for angiomatous tissue; ii) absence of
cellular atypia; iii) minimal or no osteoblastic response and
absence of dystrophic calcification; iv) evidence of local and
progressive osseous resorption; v) non-expansile and non-ulcerative
lesion; vi) absence of visceral involvement; vi) osteolytic
radiographic pattern; viii) negative hereditary, metabolic,
neoplastic, immunologic or infectious etiology. In the present
case, the radiographical and CT images indicated multiple sites of
osteolysis of the occipital bone and multiple cervical vertebrae,
and the patient was initially suspected to have primary malignant
or metastatic bone tumors. However, extensive workup, including
laboratory examination, systemic CT scan, thoracoscopy and needle
biopsy of the cervical vertebra did not provide any evidence of
neoplastic, endocrinological or infectious diseases. To obtain an
accurate diagnosis and receive further treatment, the patient was
transferred to the Department of Osseous Oncology at Changzheng
Hospital for surgical intervention. Post-operative
histopathological examination of the excised occipital and cervical
lesions revealed that the bone cavity was infiltrated with numerous
dilated blood vessels and fibrous tissues without cellular atypia;
thus, the patient was eventually diagnosed with GSS.
Owing to its rarity, no standard treatment is
available for GSS. The treatment options include surgery, radiation
therapy and medical therapy, depending on the location and size.
The morbidity and mortality are high when the cervical spine is
involved, as cervical spinal cord injury or cerebrovascular
accident may occur. Between 1997 and 2019, only 17 cases affecting
the cervical spine (including the present case) have been reported
in the English literature. Details of such cases are summarized in
Table I (14-25).
Surgical treatment was performed in 9 patients (52%), of whom 2
patients also received radiotherapy. The most common surgical
method is spinal fusion using an internal fixator, e.g. a screw and
a plate, or bone graft reconstruction. The anterior or posterior
approach may be selected according to the specific condition. Of
these 9 reported cases, 2 had no description of the disease
progression during follow-up. Osteolysis stopped progressing in 6
of the other 7 cases. Only 1 case developed more severe osteolysis
during follow-up. The majority of cases have favorable outcomes
when adequate spinal fusion is performed. Radiotherapy on its own
or combined with medication was administered to 8 patients (47.2%).
The outcomes of patients who receive radiotherapy may be different.
Among these previous cases, 2 patients had new bone formation, 1
patient exhibited no further bone resorption, 3 patients had
progressive osteolysis and 2 patients died.
 | Table IReview of treatment of cervical
vertebral osteolysis in patients with GSS. |
Table I
Review of treatment of cervical
vertebral osteolysis in patients with GSS.
| First author
(year) | Age
(years)/gender | Location | Follow-up
duration | Treatment | Outcomes | (Refs.) |
|---|
| Kim (2019) | 22/male | C3-T4 | 1 year | Anterior and
posterior fixation with screw and plate system | No progression | (14) |
| Tena-Sanabria
(2019) | 6/male | C1-C3 | Not specified | Radiotherapy (45
Gy/25f) | Spinal cord
compression and death | (15) |
| Tateda (2017) | 15/male | C1-C5 | 5 years | Anterior spinal
fusion with iliac bone graft and screw and plate system | No recurrence | (16) |
| Schell (2016) | 31/female | C1-C4 | 6 years | Anterior and
posterior spinal fusion with rib and iliac crest graft and
rhBMP2 | No recurrence | (5) |
| Noda (2013) | 15/male | C1-C8 | Not specified | Anterior cervical
fusion | Not described | (17) |
| Heyd (2011) | 38/male | Upper cervical
spine | 24 months | Radiotherapy (18x2
Gy) | Progression | (18) |
| Heyd (2011) | 24/female | Cervical spine | 46 months | Radiotherapy (18x2
Gy) | Progression | (18) |
| Heyd (2011) | 44/male | Cervical spine | 54 months | Radiotherapy (20x2
Gy) | No progression | (18) |
| Kai (2006) | 35/female | C7 | Not specified | Vertebrectomy with
bone grafting | Not described | (19) |
| Lekovic (2006) | 10/male | C1-C2 | 6 years | Posterior spinal
fusion with placement of wires, radiotherapy (5x2 Gy) | Progression | (20) |
| Chong (2003) | 49/male | C2-C5 | 1.5 years | Anterior and
posterior fixation with iliac graft and screw and plate system | No progression | (21) |
| Bode-Lesniewska
(2002) | 65/female | Cervico-thoracic
spine | 15 months | Radiotherapy (20x2
Gy) | Post-radiation
esophagitis and death | (22) |
| Mawk (1997) | 6/male | C1-C3 | 3 months | Radiotherapy | Remineralization | (4) |
| Chung (1997) | 48/female | C3-T5 | Not specified | Radiotherapy | Progression | (23) |
| Hagberg (1997) | 19/male | C7-T2 | 19 months | Stabilisation
surgery, radiotherapy (15x2 Gy), interferon | No progression | (24) |
| Khosrovi (1997) | 62/male | C1-C2 | 2 years | Radiotherapy (20x2
Gy) | Remineralization | (25) |
In the case of the present study, remediation of
dangerous cervical vertebral instability and prevention of spinal
cord injury were accomplished via posterior resection of the
occipital and cervical vertebral lesions and spinal reconstruction
using an internal fixator. As the C1-T1 vertebrae were involved,
the surgery was fairly difficult but successful and no
post-operative complications occurred. Biphosphonates are a potent
inhibitor of osteoclasts and may suppress bone resorption in GSS
(26). Therefore, the patient was
administered 4 mg zoledronic acid every 2 months and vitamin D
supplements post-surgery. At the time of conclusion of the study,
the patient had no procedure-associated complications and
osteolysis had not progressed.
Chylous effusions usually occur in patients with GSS
with rib, clavicular, sternal, scapular or vertebral involvement
(7). Chylothorax may result from
direct pleural involvement or obstruction of the thoracic duct by
lymphovascular tissues (27).
Bilateral chylothorax is a clinically challenging condition and has
a high mortality rate of 53% (28).
Common interventions include thoracic duct ligation, pleurodesis,
pleurectomy, resection of lymphangiomatous lesions, radiotherapy
and medical therapy (28). In the
present case, the patient was provided with a low-fat diet and
received intravenous albumin infusion and chest catheter drainage.
Chyle outflowing from the bone lesions was observed during surgery
and the lymphangiomatous tissues were surgically resected from the
affected bones. The pleural effusion gradually decreased after
surgery.
In conclusion, the present study reported on a case
of GSS extensively invading the C1-T1 vertebrae accompanied by a
large amount of bilateral pleural effusion. This case exemplifies
that when osteolysis of unknown causes occurs, GSS, although rare,
should be taken into consideration. Bloody or chylous pleural
effusions may occur in patients with GSS with pleural involvement
or thoracic duct obstruction. For patients with cervical spinal
involvement, rapid surgical interventions are recommended to
achieve spinal stability and prevent neurological complications. In
the present case, the clinical outcome was favorable after surgical
intervention and bisphosphonate treatment.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural
Science Foundation of China (grant nos. 81602618 and 81672929).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KJC interpreted the data and prepared the
manuscript. MHY prepared the discussion section including the
literature search and analyzed the data of previously reported
cases. HH and BL performed the data acquisition and revised the
final draft. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Written informed consent was acquired from the
patient prior to participation in this study. The present study was
approved by the Ethics Committee of Shanghai Changzheng
Hospital.
Patient consent for publication
Written consent was provided by the patient for the
publication of his data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dickson GR, Hamilton A, Hayes D, Carr KE,
Davis R and Mollan RA: An investigation of vanishing bone disease.
Bone. 11:205–210. 1990.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Vinée P, Tanyü MO, Hauenstein KH, Sigmund
G, Stöver B and Adler CP: CT and MRI of Gorham syndrome. J Comput
Assist Tomogr. 18:985–989. 1994.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tie ML, Poland GA and Rosenow EC III:
Chylothorax in Gorham's syndrome. A common complication of a rare
disease. Chest. 105:208–213. 1994.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mawk JR, Obukhov SK, Nichols WD, Wynne TD,
Odell JM and Urman SM: Successful conservative management of Gorham
disease of the skull base and cervical spine. Childs Nerv Syst.
13:622–625. 1997.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Schell A, Rhee JM, Allen A, Andras L and
Zhou F: Surgical management of Gorham disease involving the upper
cervical spine with occipito-cervical-thoracic fusion: A case
report. Spine J. 16:e467–e472. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gorham LW and Stout AP: Massive osteolysis
(acute spontaneous absorption of bone, phantom bone, disappearing
bone); its relation to hemangiomatosis. J Bone Joint Surg Am.
37-A:985–1004. 1955.PubMed/NCBI
|
|
7
|
Hellyer J, Oliver-Allen H, Shafiq M,
Tolani A, Druzin M, Jeng M, Rockson S and Lowsky R: Pregnancy
complicated by gorham-stout disease and refractory chylothorax. AJP
Rep. 6:e355–e358. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Möller G, Priemel M, Amling M, Werner M,
Kuhlmey AS and Delling G: The Gorham-Stout syndrome (Gorham's
massive osteolysis). A report of six cases with histopathological
findings. J Bone Joint Surg Br. 81:501–506. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Heyden G, Kindblom LG and Nielsen JM:
Disappearing bone disease. A clinical and histological study. J
Bone Joint Surg Am. 59:57–61. 1977.PubMed/NCBI
|
|
10
|
Hammer F, Kenn W, Wesselmann U, Hofbauer
LC, Delling G, Allolio B and Arlt W: Gorham-Stout disease:
Stabilization during bisphosphonate treatment. J Bone Miner Res.
20:350–353. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hominick D, Silva A, Khurana N, Liu Y,
Dechow PC, Feng JQ, Pytowski B, Rutkowski JM, Alitalo K and
Dellinger MT: VEGF-C promotes the development of lymphatics in bone
and bone loss. Elife. 7(e34323)2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Baud J, Lomri A, Graber D and Bikfalvi A:
The therapeutic response in Gorham's syndrome to the beta-blocking
agent propranolol is correlated to VEGF-A, but not to VEGF-C or
FLT1 expression. BMC Res Notes. 8(333)2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Heffez L, Doku HC, Carter BL and Feeney
JE: Perspectives on massive osteolysis. Report of a case and review
of the literature. Oral Surg Oral Med Oral Pathol. 55:331–343.
1983.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Kim JH, Yoon DH, Kim KN, Shin DA, Yi S,
Kang J and Ha Y: Surgical management of gorham-stout disease in
cervical compression fracture with cervicothoracic fusion: Case
report and review of literature. World Neurosurg. 129:227–281.
2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tena-Sanabria ME, Jesús-Mejenes LY,
Fuentes-Herrera G, Álvarez-Martínez FA, Victorio-García NP and
Núñez-Enríquez JC: A report of two children with Gorham-Stout
disease. BMC Pediatr. 19(206)2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tateda S, Aizawa T, Hashimoto K, Kanno H,
Ohtsu S, Itoi E and Ozawa H: Successful management of gorham-stout
disease in the cervical spine bycombined conservative and surgical
treatments: A Case Report. Tohoku J Exp Med. 241:249–254.
2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Noda M, Endo C, Hoshikawa Y, Ishibashi N,
Suzuki T, Okada Y and Kondo T: Successful management of intractable
chylothorax in Gorham-Stout disease by awake thoracoscopic surgery.
Gen Thorac Cardiovasc Surg. 61:356–358. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Heyd R, Micke O, Surholt C, Berger B,
Martini C, Füller J, Schimpke T and Seegenschmiedt MH: German
Cooperative Group on Radiotherapy for Benign Diseases (GCG-BD).
Radiation therapy for Gorham-Stout syndrome: Results of a national
patterns-of-care study and literature review. Int J Radiat Oncol
Biol Phys. 81:e179–e185. 2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kai B, Ryan A, Munk PL and Dunlop P:
Gorham disease of bone: Three cases and review of radiological
features. Clin Radiol. 61:1058–1064. 2006.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lekovic GP, Mariwalla NR, Horn EM, Chang
S, Rekate HL and Theodore N: Skeletal dysplasia involving the
subaxial cervical spine. Report of two cases and review of the
literature. Neurosurg Focus. 20(E8)2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chong Ng L and Sell P: Gorham disease of
the cervical spine-a case report and review of the literature.
Spine. 28:E355–E358. 2003.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bode-Lesniewska B, von Hochstetter A,
Exner GU and Hodler J: Gorham-Stout disease of the shoulder girdle
and cervico-thoracic spine: Fatal course in a 65-year-old woman.
Skeletal Radiol. 31:724–729. 2002.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chung C, Yu JS, Resnick D, Vaughan LM and
Haghighi P: Gorham syndrome of the thorax and cervical spine: CT
and MRI findings. Skeletal Radiol. 26:55–59. 1997.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Hagberg H, Lamberg K and Aström G:
Alpha-2b interferon and oral clodronate for Gorham's disease.
Lancet. 350:1822–1823. 1997.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Khosrovi H, Ortiz O, Kaufman HH, Schochet
SS Jr, Reddy GN and Simmons D: Massive osteolysis of the skull and
upper cervical spine. Case report and review of the literature. J
Neurosurg. 87:773–780. 1997.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Liu Y, Zhong DR, Zhou PR, Lv F, Ma DD, Xia
WB, Jiang Y, Wang O, Xing XP and Li M: Gorham-Stout disease:
Radiological, histological, and clinical features of 12 cases and
review of literature. Clin Rheumatol. 35:813–823. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Chavanis N, Chaffanjon P, Frey G, Vottero
G and Brichon PY: Chylothorax complicating Gorham's disease. Ann
Thorac Surg. 72:937–939. 2001.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Brodszki N, Länsberg JK, Dictor M,
Gyllstedt E, Ewers SB, Larsson MK and Eklund EA: A novel treatment
approach for paediatric Gorham-Stout syndrome with chylothorax.
Acta Paediatr. 100:1448–1453. 2011.PubMed/NCBI View Article : Google Scholar
|