Introduction
Tumors that occur in the uterine corpus include
epithelial, mesenchymal, mixed epithelial and mesenchymal,
miscellaneous, lymphoid and myeloid and secondary tumors, as well
as trophoblastic disease (1).
Endometrial cancer is the third most common cause of death among
gynecological cancers, following ovarian and cervical cancer, with
increasing incidence rates in several countries (2). This may be attributed to the increasing
number of elderly individuals and increasing rates of obesity
(2). Endometrial cancer includes
several carcinomas, which are divided into type I and II cancers
and include endometrioid adenocarcinomas, mucinous adenocarcinomas,
serous carcinomas, clear-cell carcinomas and several other rare
forms, such as neuroendocrine tumors, including small-cell, mixed,
undifferentiated and dedifferentiated carcinomas (3).
In addition, choriocarcinoma is a malignant
trophoblastic tumor, usually of the placenta, that may also occur
in the uterine corpus. choriocarcinoma belongs to the malignant end
of the spectrum of gestational trophoblastic disease, with 20% of
this disease occurring after normal pregnancy (4). However, it is rare for trophoblastic
disease to present in the uterus of postmenopausal women (5). Furthermore, non-gestational
choriocarcinomas occur in the absence of a preceding gestation, and
often tend to occur as a component of an ovarian germ cell tumor
(6). Almost all primary
non-gestational choriocarcinomas of the female genital tract have
been described in the ovaries (7,8).
The number of reports in the literature regarding
endometrial cancer in which choriocarcinoma differentiation occurs
in the uterine corpus is limited (9),
with only a single report of coexistence of a mixed adenocarcinoma
and a choriocarcinoma (10). we
herein report the first case of a collision tumor in the uterine
corpus composed of three histologically distinct cancers, namely an
endometrioid carcinoma, an undifferentiated carcinoma and a
choriocarcinoma.
Case report
Our patient was a 52-year-old woman with a history
of two pregnancies and two deliveries; the last delivery was when
she was 28 years old. The patient was 156 cm in height, weighed 51
kg, and had a body mass index of 20.95 kg/m2. The history of
menstrual cycles was regular and she had gone through menopause at
the age of 51 years. The surgical history included an appendectomy
at the age of 19 years, but there was no family history of cancer.
The patient consulted a gynecologist with a main complaint of
moderate genital bleeding. A 35×30-mm mass lesion, which bled
easily, was detected in the cervix.
The patient was referred to our hospital and, after
undergoing a detailed examination, received further treatment due
to the suspicion of cervical cancer. During the first visit to our
hospital, a pelvic examination revealed an enlarged cervix, while
the digital examination revealed extension to the parametrium on
either side of the uterus. The colposcopic examination revealed
that the invasive carcinoma was a large polypoid mass in the
cervical canal. The cytological diagnosis of the cervical lesion
was a high-grade squamous intraepithelial lesion and the
pathological diagnosis, using a punch biopsy, indicated a squamous
cell carcinoma (SCC). Transvaginal ultrasonography revealed a mixed
echogenic mass in the cervix, sized 49×49×57 mm (Fig. 1A). Magnetic resonance imaging (MRI)
revealed a hyperintense cervical mass sized 55×51×52 mm, invading
the lower uterine segment (Fig. 1B).
Positron emission tomography-computed tomography (CT) revealed
intense fludeoxyglucose activity correlating with a cervical and
endometrial mass, without signs of metastasis to other organs or to
the pelvic and paraaortic lymph nodes (Fig. 1C). The tumor marker carbohydrate
antigen (CA)-125 was elevated (91.8 U/ml), but other markers,
including carcinoembryonic antigen, CA19-9 and SCC antigen, were
within the normal range.
With an initial diagnosis of stage Ib2 cervical
cancer, the patient underwent radical hysterectomy, bilateral
adnexectomy and pelvic lymph node dissection. the abdominal cavity
was free of ascites, disseminated lesions and adhesions to adjacent
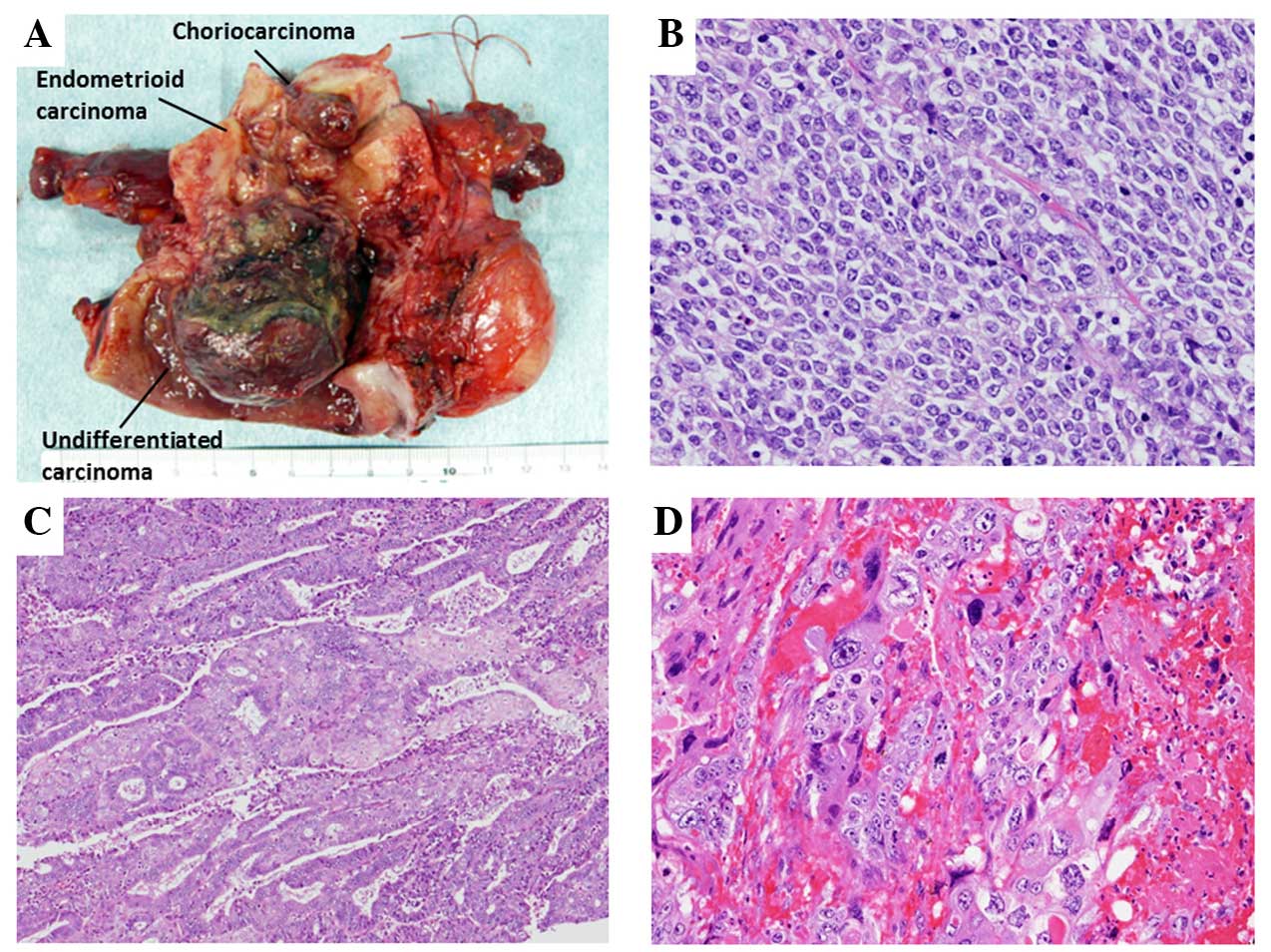
organs. Three distinct tumors were identified in the resected
specimen, one in the lower segment, one in the middle segment and
one in the fundus of the uterine corpus (Fig. 2A). The histopathological examination
of the masses revealed that they were three histologically distinct
cancers: an undifferentiated carcinoma of the lower segment,
invading half the thickness of the myometrium (Fig. 2B); an endometrioid adenocarcinoma with
squamous differentiation, grade 2, confined to the endometrium in
the middle segment (Fig. 2C); and a
choriocarcinoma with lymphovascular space invasion, but without an
endometrioid adenocarcinoma component, in the fundus of the uterine
corpus (Fig. 2D), metastasizing to
the lymph nodes of the left external iliac artery. There was no
communication between the three lesions in the uterine corpus.
The clinical diagnosis was stage IIIC1 endometrial
cancer [International Federation of Gynecology and Obstetrics 2008
(1)]and choriocarcinoma. the patient
was diagnosed with three histologically distinct neoplasms in the
uterine corpus. After the operation, chemotherapy with paclitaxel
175 mg/m2 plus carboplatin area under the curve = 6 (TC
regimen) was administered, due to the high risk of endometrial
cancer. Six treatment cycles were completed without dose reduction
or suspension of treatment. The β-human chorionic gonadotropin
(hCG) level was 19.5 mIU/ml when the pathological results of the
coexistence with a choriocarcinoma were obtained, and the β-hCG
level (1.0 mIU/ml) after six cycles of TC was above the normal
range (0–0.5 mIU/ml), although other tumor markers were within
normal limits, and CT revealed no cancer recurrence or metastasis.
Five additional cycles using methotrexate (20 mg/m2 body surface ×5
days) were administered and completed without dose reduction or
suspension of treatment. After the five cycles, the tumor markers,
including the β-hCG level, were within normal limits, without
cancer relapse during 1 year of follow-up.
Discussion
We reported a case with three histologically
distinct cancers in the uterine corpus: an endometrioid carcinoma,
an undifferentiated carcinoma and a choriocarcinoma. There are
several reports in the literature on endometrial cancer with
choriocarcinoma differentiation, with two distinct components in
the primary tumor, and the prognosis of this tumor type is reported
to be poor (9). However, only a
single case of a histologically distinct coexistence of a mixed
adenocarcinoma and a choriocarcinoma in the uterine corpus has been
reported to date (10).
Collision tumors are an uncommon phenomenon
characterized by the coexistence of two completely distinct and
independent tumors at the same site. The two morphologically
separate tumors are sharply demarcated from each other. This entity
is distinct from neoplasms demonstrating heterologous or mixed
elements (11). collision tumors have
been reported in various organs, such as the ovary and uterus, as
well as in the esophagus, stomach, colon, lung, skin, thyroid gland
and breast (12,13).
In patients with collision tumors of the uterine
corpus, the median age is 64.9 years (range, 47–85 years); the
histological diagnoses in previously reported collision tumors of
the uterine corpus are summarized in Table I (10,13–20).
Several reports determined that collision tumors of the uterine
corpus were mainly composed of two distinct tumors, an endometrial
carcinoma (endometrioid or serous adenocarcinoma) and a mesenchymal
tumor (leiomyosarcoma or endometrial stromal sarcoma). However, in
a recent report, three distinct endometrial cancers were found in
the uterine corpus, a malignant mixed Müllerian tumor, a serous
adenocarcinoma and an endometrioid adenocarcinoma (20). In the present case report, we
identified three histologically distinct lesions in the uterine
corpus, including an endometrioid carcinoma, an undifferentiated
carcinoma and a choriocarcinoma.
 | Table I.Summary of histological diagnosis of
collision tumors of the uterine corpus reported in the
literature. |
Table I.
Summary of histological diagnosis of
collision tumors of the uterine corpus reported in the
literature.
| Histological
diagnosis | No. | (Refs.) |
|---|
| Two distinct
tumors |
|
|
|
Endometrioid carcinoma/serous
carcinoma/leiomyosarcoma or endometrial stromal sarcoma | 7 | (13–17) |
|
Endometrioid
carcinoma/carcinosarcoma | 1 | (18) |
| Serous
carcinoma/small cell carcinoma | 1 | (19) |
| Mixed
cell carcinoma/choriocarcinoma | 1 | (10) |
| Three distinct
tumors |
|
|
| Serous
carcinoma/endometrioid carcinoma/carcinosarcoma | 1 | (20) |
|
Undifferentiated
carcinoma/endometrioid carcinoma/choriocarcinoma | 1 | Present case |
| Total | 12 |
|
Choriocarcinomas of the uterine corpus are rare,
particularly after menopause (21).
Choriocarcinomas of gestational and non-gestational origin have a
distinct prognosis, but cannot be distinguished by routine
histological examination (22).
Molecular genetic analysis may reliably identify the genetic origin
of a pure ovarian choriocarcinoma (23–25);
however, as this is an unestablished and costly technique with
limited availability, it was not used it in this case. However, our
patient was in the high-risk group of endometrial cancer due to the
lymph node metastasis and the histological type, i.e.,
undifferentiated carcinoma (26).
Thus, the patient received six cycles of TC as adjuvant
chemotherapy for high-risk endometrial cancer and an additional
five cycles of chemotherapy with MTX, as the β-hCG level after six
cycles of TC remained above the normal range.
Collision tumors of the uterine corpus are rare,
with only 10 cases of two distinct tumors and 1 case of three
distinct tumors reported thus far. Moreover, there was only 1 case
of a collision tumor composed of a choriocarcinoma with a
histologically distinct endometrial carcinoma. To the best of our
knowledge, this is the first report of a collision tumor composed
of three histologically distinct neoplasms, including a
choriocarcinoma, an endometrioid adenocarcinoma and an
undifferentiated carcinoma. The diagnosis of a collision tumor
prior to surgery is difficult if the neoplasms are located in close
proximity, or one tumor predominates compared with the others, as
in the present case. Careful pathological examination is crucial
for accurately diagnosing the neoplasms constituting the collision
tumor in order to prescribe the necessary treatment for a favorable
prognosis.
References
|
1
|
Kurman RJ, Carcangiu ML, Herrington CS and
Young RH: WHO classification of tumours OF female reprOduCTive
organs. WHO CLASSIFICATION OF TUMOURS. 6:(4TH). (Lyon). IARC Press.
122–167. 2014.
|
|
2
|
Stewart BW and Wild CP: World Cancer
Report 2014. Chapter 5.12. LYON: IARC PRESS. 2014.
|
|
3
|
Hoffman BL, Schorge JO, Schaffer JI,
Halvorson LM, Bradshaw KD and Cunningham FG: Endometrial cancer.
Williams Gynecology. Hoffman BL, Schorge JO, Schaffer JI, Halvorson
LM, Bradshaw KD and Cunningham FG: (2ND). (New York). McGraw-Hill.
817–838. 2012.
|
|
4
|
Lurain JR: Gestational trophoblastic
disease II: Classification and management of gestational
trophoblastic neoplasia. Am J Obstet Gynecol. 204:11–18. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chittenden B, Ahamed E and Maheshwari A:
Choriocarcinoma in a postmenopausal woman. Obstet Gynecol.
114:462–465. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Russell P and Farnsworth A:
Non-gestational choriocarcinomas. Surgical Pathology of the
Ovaries. Russell P and Farnsworth A: (2ND). (Edinburgh). Churchill
Livingstone. 263–264. 1997.
|
|
7
|
Jiao LZ, Xiang Y, Feng FZ, Wan XR, Zhao J,
Cui QC and Yang XY: Clinical analysis of 21 cases of nongestational
ovarian choriocarcinoma. Int J Gynecol Cancer. 20:299–302. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Haruma T, Ogawa C, Nishida T, Kusumoto T,
Nakamura K, Seki N, Katayama T and Hiramatsu Y: Pure
choriocarcinoma of the ovary in Silver-Russell syndrome. Acta Med
Okayama. 69:183–188. 2015.PubMed/NCBI
|
|
9
|
Ishida M and Okabe H: Endometrioid
adenocarcinoma with choriocarcinomatous differentiation: A case
report and review of the literature. Oncol Lett. 6:655–658.
2013.PubMed/NCBI
|
|
10
|
Gao HJ, Zhou W, Zhang XF, Zhou CY and Qian
JH: Coexistent gestational choriocarcinoma and mixed adenocarcinoma
of the uterus. Eur J Gynaecol Oncol. 34:362–367. 2013.PubMed/NCBI
|
|
11
|
Van Eeden S, Nederlof PM, Taal BG,
Offerhaus GJ and Van Velthuysen ML: A tumour with a neuroendocrine
and papillary serous component: Two or a pair? J Clin Pathol.
55:710–714. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Singh AK and Singh M: Collision tumours of
ovary: A very rare case series. J Clin Diagn Res. 8:FD14–FD16.
2014.PubMed/NCBI
|
|
13
|
Patwardhan JR and Gadgil RK: Collision
tumour of the uterus. Indian J Cancer. 6:194–197. 1969.PubMed/NCBI
|
|
14
|
Lifschitz-Mercer B, Czernobilsky B, Dgani
R, Dallenbach-Hellweg G, Moll R and Franke WW: Immunocytochemical
study of an endometrial diffuse clear cell stromal sarcoma and
other endometrial stromal sarcomas. Cancer. 59:1494–1499. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sreenan JJ and Hart WR: Carcinosarcomas of
the female genital tract. A pathologic study of 29 metastatic
tumors: Further evidence for the dominant role of the epithelial
component and the conversion theory of histogenesis. Am J Surg
Pathol. 19:666–674. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lam KY, Khoo US and Cheung A: Collision of
endometrioid carcinoma and stromal sarcoma of the uterus: A report
of two cases. Int J Gynecol Pathol. 18:77–81. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gaertner EM, Farley JH, Taylor RR and
Silver SA: Collision of uterine rhabdoid tumor and endometrioid
adenocarcinoma: A case report and review of the literature. Int J
Gynecol Pathol. 18:396–401. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Takahashi Y and Inoue T: Hepatoid
carcinoma of the uterus that collided with carcinosarcoma. Pathol
Int. 53:323–326. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shaco-Levy R, Manor E, Piura B and Ariel
I: An unusual composite endometrial tumor combining papillary
serous carcinoma and small cell carcinoma. Am J Surg Pathol.
28:1103–1106. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jang KS, Lee WM, Kim YJ and Cho SH:
Collision of three histologically distinct endometrial cancers of
the uterus. J Korean Med Sci. 27:89–92. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhao J, Xiang Y, Wan XR, Feng FZ, Cui QC
and Yang XY: Molecular genetic analyses of choriocarcinoma.
Placenta. 30:816–820. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wang Y, Yang Y, Teng F, Zhang H and Xue F:
Pure nongestational uterine choriocarcinoma in a postmenopausal
Chinese woman confirmed with short tandem repeat analysis. Am J
Obstet Gynecol. 211:e1–e3. 2014. View Article : Google Scholar
|
|
23
|
Hirata Y, Yanaihara N, Yanagida S, Fukui
K, Iwadate K, Kiyokawa T and Tanaka T: Molecular genetic analysis
of nongestational choriocarcinoma in a postmenopausal woman: A case
report and literature review. Int J Gynecol Pathol. 31:364–368.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fisher RA, Newlands ES, Jeffreys AJ, Boxer
GM, Begent RH, Rustin GJ and Bagshawe KD: Gestational and
nongestational trophoblastic tumors distinguished by DNA analysis.
Cancer. 69:839–845. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fisher RA, Savage PM, MacDermott C, Hook
J, Sebire NJ, Lindsay I and Seckl MJ: The impact of molecular
genetic diagnosis on the management of women with hCG-producing
malignancies. Gynecol Oncol. 107:413–419. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Johnson N, Bryant A, Miles T, Hogberg T
and Cornes P: Adjuvant chemotherapy for endometrial cancer after
hysterectomy. Cochrane Database Syst Rev: CD003175. 2011.
View Article : Google Scholar
|