Introduction
Addiction to opioid drugs such as morphine is a
universal social and public problem. The repeated administration of
opioid drugs may lead to the development of analgesic tolerance and
dependence, which limit the clinical use of opioid drugs in pain
treatment (1). Furthermore,
prolonged exposure to opioid drugs may result in pathological
changes in the liver in almost 100% of cases (2,3). A
previous study found that 44% of drug addicts suffered from acute
hepatitis, 34% from chronic hepatitis and 16% from liver damage
(4). Lately, clinical studies also
suggest that opiate addicts are at increased risk of progressive
renal failure (5–7). Renal diseases in opiate addicts are
associated with nephritic syndrome, acute glomerulonephritis and
interstitial nephritis (8,9). The acute or chronic administration of
opioid drugs may induce oxidative damage and cellular apoptosis in
the liver and kidney, and hence result in hepatic and renal damage
(10–13). Considering the role of the liver
and kidney in metabolism and detoxification, opioid drug-induced
liver and kidney toxicity has been a crucial issue in the therapy
for drug abuse.
Previous studies have shown that blocking oxidative
damage is a useful strategy for the treatment of opioid
drug-induced hepatic and renal damage (14). There are several molecules to
counteract oxidative stress in the body, such as thioredoxin-1
(Trx-1) and heat shock protein 70 (Hsp70). Trx-1 is a small
ubiquitous protein with redox-controlled cell functions (15,16).
Trx-1 has radical-scavenging activity and couples with
peroxiredoxin to scavenge hydrogen peroxide (17,18).
Trx-1 is able to protect cells from hydrogen peroxide, UV
irradiation and ischemic reperfusion (19,20).
Hsp70 is a stress-inducible protein that prevents protein
aggregation and facilitates refolding of dysfunctional proteins
(21). Hsp70 is able to enhance
the survival of cells and inhibits apoptosis induced by oxidative
damage during various stress conditions. Geranylgeranylacetone
(GGA) is an acyclic polyisoprenoid and widely used as an anti-ulcer
drug in the clinical setting. Previous studies have suggested that
GGA induced Trx-1 and Hsp70 expression in various cells to exert
cytoprotection (22–24). GGA has been widely reported to
exert cytoprotective effect against various stresses, such as
oxidative stress in the gastric mucosa, liver, heart and brain
(25–28). Our previous study also has
demonstrated that GGA protected against morphine-induced
hyperlocomotion, rewarding effect and withdrawal syndrome in mice
(29). However, there are no
studies of the role of GGA in the liver and kidney toxicity induced
by opioid drugs. In the present study, we postulated that GGA
induces Trx-1 and Hsp70 expression, which may in turn prevent
opiate-induced hepatic and renal injury. The present study was
designed to evaluate the protective effect of GGA against
morphine-induced hepatic and renal damage in mice.
Materials and methods
Reagents
GGA was purchased from Eisai (Tokyo, Japan).
Anti-mouse Trx-1 rabbit polyclonal antibody was obtained from Redox
Bioscience (Kyoto, Japan). Antibodies (pro-caspase-12 and -9,
caspase-3, β-actin and Hsp70) were purchased from Santa Cruz
Biotechnology, Inc. (Santa Cruz, CA, USA). Morphine hydrochloride
was purchased from the Shenyang First Pharmaceutical Factory,
Northeast Pharmaceutical Group Corporation (Shenyang, China). Mouse
malondialdehyde (MDA) enzyme-linked immunosorbent assay (ELISA) kit
was purchased from R&D Systems (Minneapolis, MN, USA).
Animals
Sixteen C57BL/6 mice (Chongqing Medical University,
China; age, 6–7 weeks) were used in the experiments. The mice were
housed in plastic cages and kept on a 12-h light-dark cycle and had
free access to food and water. The animals were cared for and used
in accordance with the National Institutes of Health Guide for the
Care and Use of Laboratory Animals. The experiment was approved by
the local Committee on Animal Use and Protection.
GGA and morphine treatment
Granulated GGA was suspended in saline immediately
before use. Mice were administered saline or GGA (800 mg/kg,
orally), using a micropipette 2 h prior to morphine treatment. The
mouse model of morphine dependence was created as described in our
previous study (29). The mice
were injected with escalating morphine doses twice daily (10, 20,
40, 60, 80 and 100 mg/kg) for 7 days. Two hours following the last
morphine injection, the mice were sacrificed using deep anesthesia,
and then heart perfusion was performed using saline. The liver and
kidney tissues were rapidly dissected, immediately frozen and
stored in a deep freezer at −80°C until use.
Western blot analysis
Protein lysates were prepared using a solubilizing
solution [20 mM Tris-HCl (pH 7.4), 150 mM NaCl, 1% NP-40, 1 mM
EDTA, 1 mM PMSF, 1 mM EGTA, 1% Triton X-100, 2.5 mM sodium
pyrophosphate, 1 mM Na3VO4, 1 mM
β-glycerolphosphate and 1 mg/ml leupeptin]. Protein concentration
was determined using the Bio-Rad protein assay reagent (Bio-Rad,
Hercules, CA, USA). An equal quantity of proteins was separated by
10% (for Hsp70), 12% (for pro-caspase-12) or 15% (for
pro-caspase-9, caspase-3 and Trx-1) SDS-PAGE and transferred to a
PVDF membrane (Millipore Corporation, Billerica, MA, USA). The
membrane was soaked in 10% skimmed milk (in PBS, pH 7.2, containing
0.1% Tween-20) overnight at 4°C, then incubated with primary
antibody followed by peroxidase-conjugated anti-mouse or
anti-rabbit IgG (KPL, Gaithersburg, MD, USA). The epitope was
visualized using an ECL Western Blot Detection kit (Millipore
Corporation). Densitometry analysis was performed using the ImageJ
software.
ELISA
The liver and kidney tissues were pooled and
homogenized in PBS. Samples were spun at 4,000 rpm for 15 min at
4°C. The supernatant was aliquoted and stored at −80°C for future
study. The concentration of MDA was measured using specific ELISA
kits (R&D, USA), according to the manufacturers’
instructions.
Statistical analysis
Data are expressed as the mean ± SD values.
Statistical analysis was performed using the SPSS software. The
one-way ANOVA followed by a post hoc multiple comparison test was
used to compare control and treated groups. P<0.05 was
considered to indicate a statistically significant difference.
Results
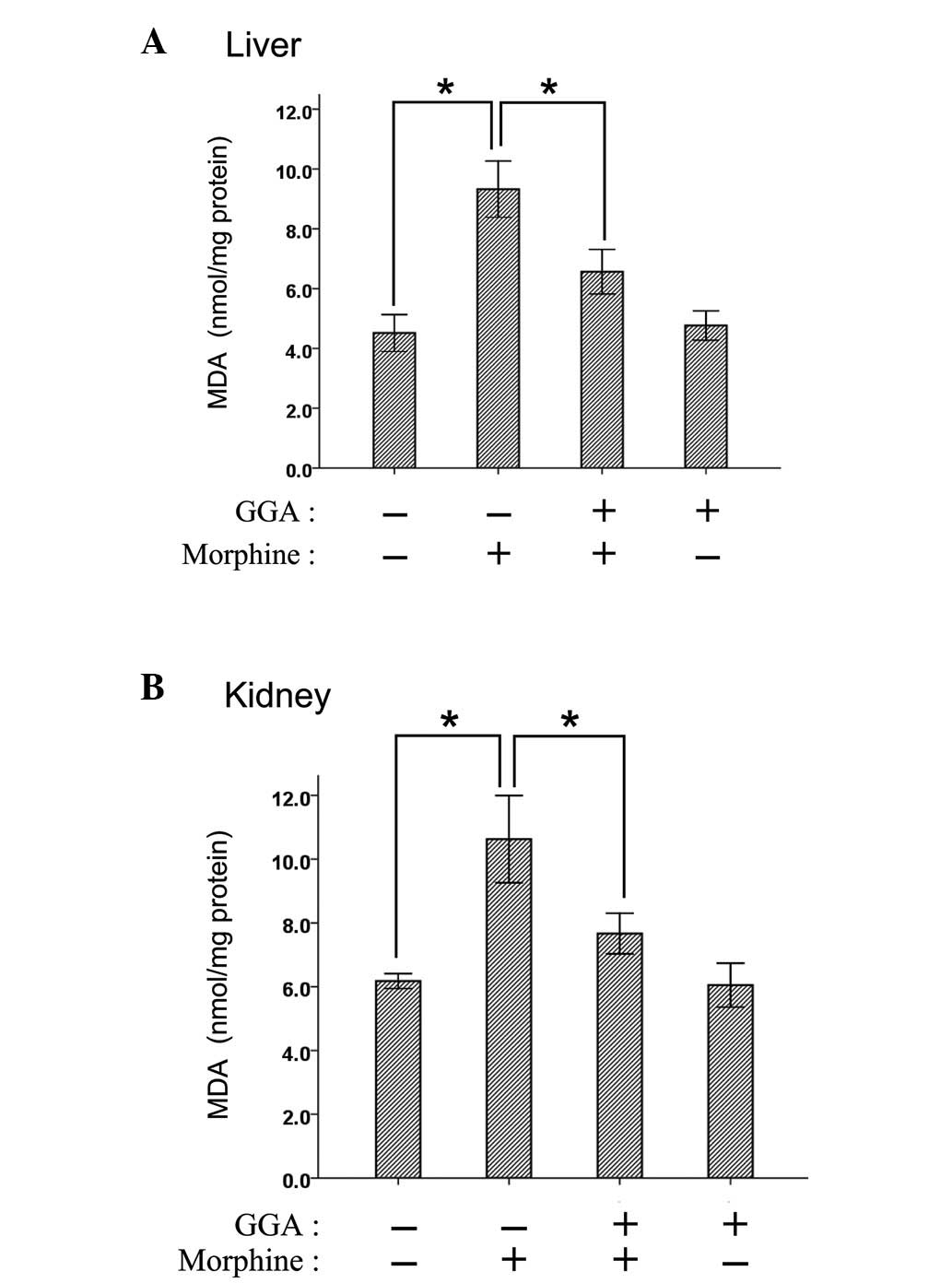
Effect of GGA on lipid peroxide formation
in the liver and kidney after chronic morphine treatment
As an important marker of oxidative lipid damage,
MDA was examined to estimate the extent of lipid peroxidation in
the present study. The levels of MDA in the liver and kidney were
significantly increased after chronic morphine treatment (Fig. 1). By contrast, the pre-treatment of
GGA significantly reduced lipid peroxide content in the liver and
kidney.
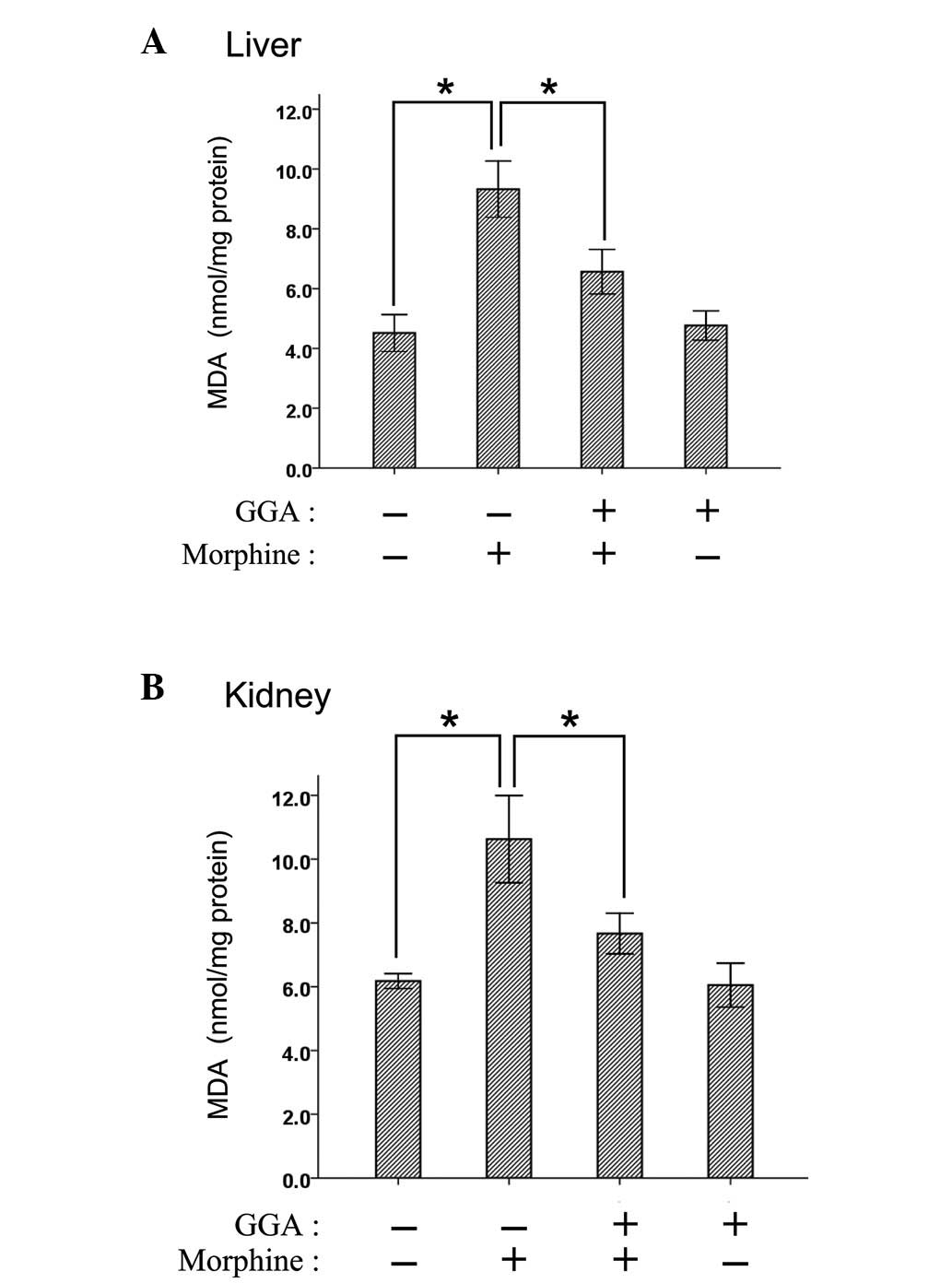 | Figure 1GGA suppressed morphine-induced lipid
peroxidation in the liver and kidney. Mice were injected with
escalating morphine doses twice daily (10, 20, 40, 60, 80 and 100
mg/kg), 2 h after GGA treatment (800 mg/kg, orally) for 7 days. Two
hours after the last morphine injection, the liver and kidney
tissues of mice were dissected. The MDA level in (A) the liver and
(B) kidney was measured using ELISA. Values are the mean ± SD; n=4.
Asterisks indicate a statistically significant difference
(*P<0.05). GGA, geranylgeranylacetone; MDA,
malondialdehyde; ELISA, enzyme-linked immunosorbent assay. |
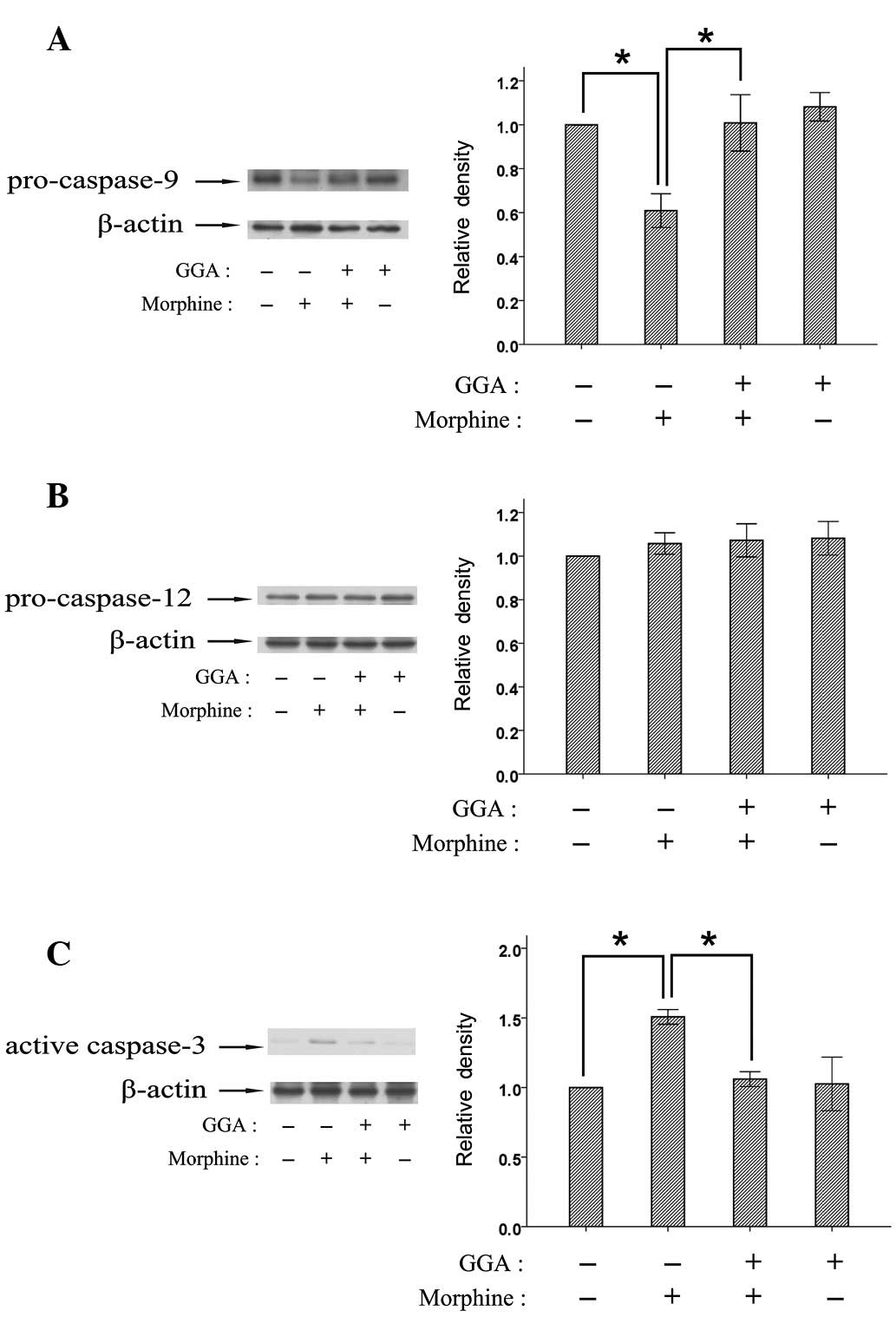
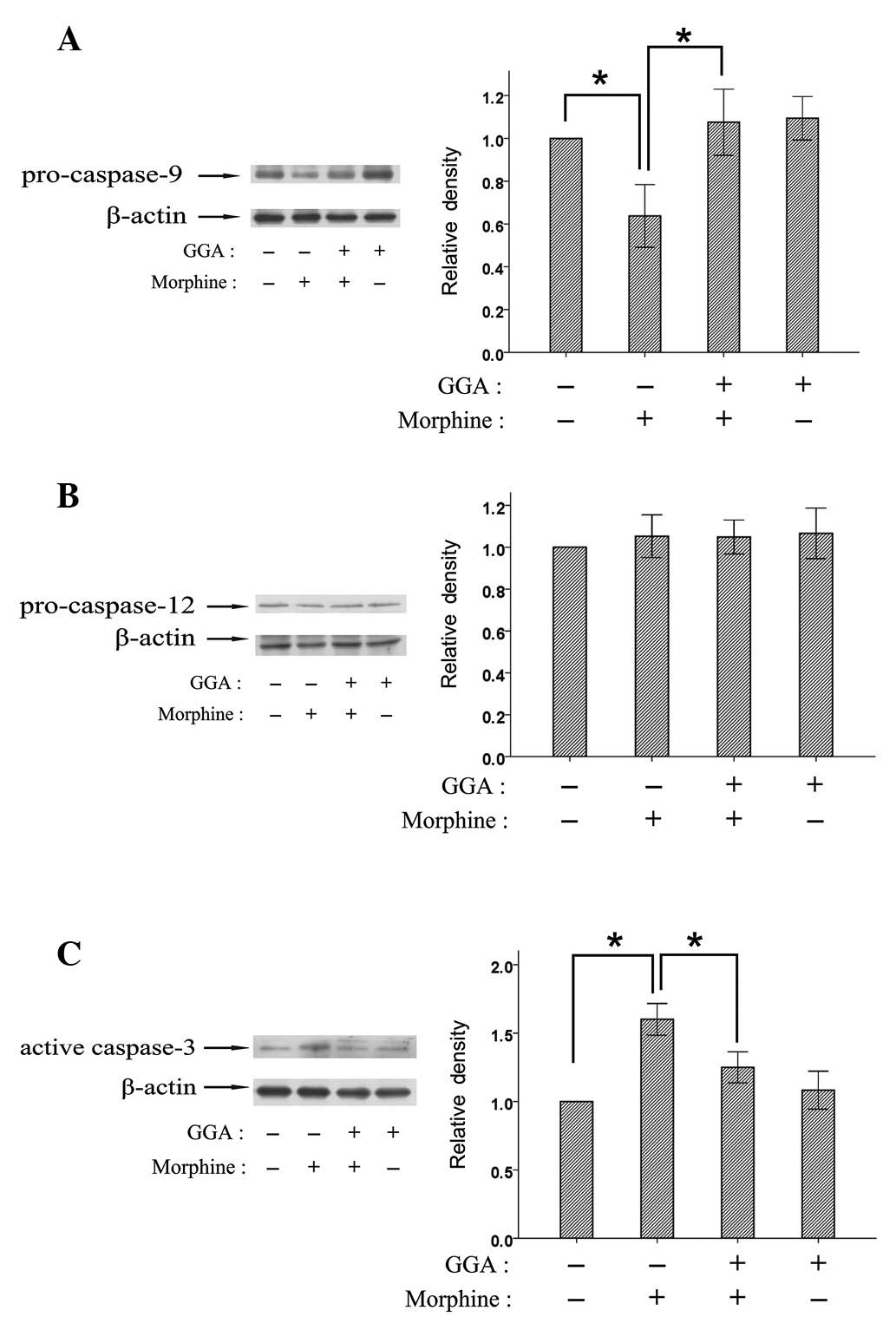
Effect of GGA on morphine-induced
apoptosis in the liver and kidney
To clarify the manner in which GGA affects cell
death pathways involved in the morphine-induced hepatic and renal
damage, the alterations of pro-caspases-9 and -12 and caspase-3
were examined following chronic morphine administration with or
without GGA pre-treatment using western blotting. Chronic morphine
administration led to the activation of caspases-9 and -3 in the
liver and kidney, while the level of pro-capase-12 was not affected
by morphine (Figs. 2 and 3). Furthermore, the pre-treatment with
GGA significantly inhibited the activation of caspases-9 and -3
induced by morphine in the liver and kidney.
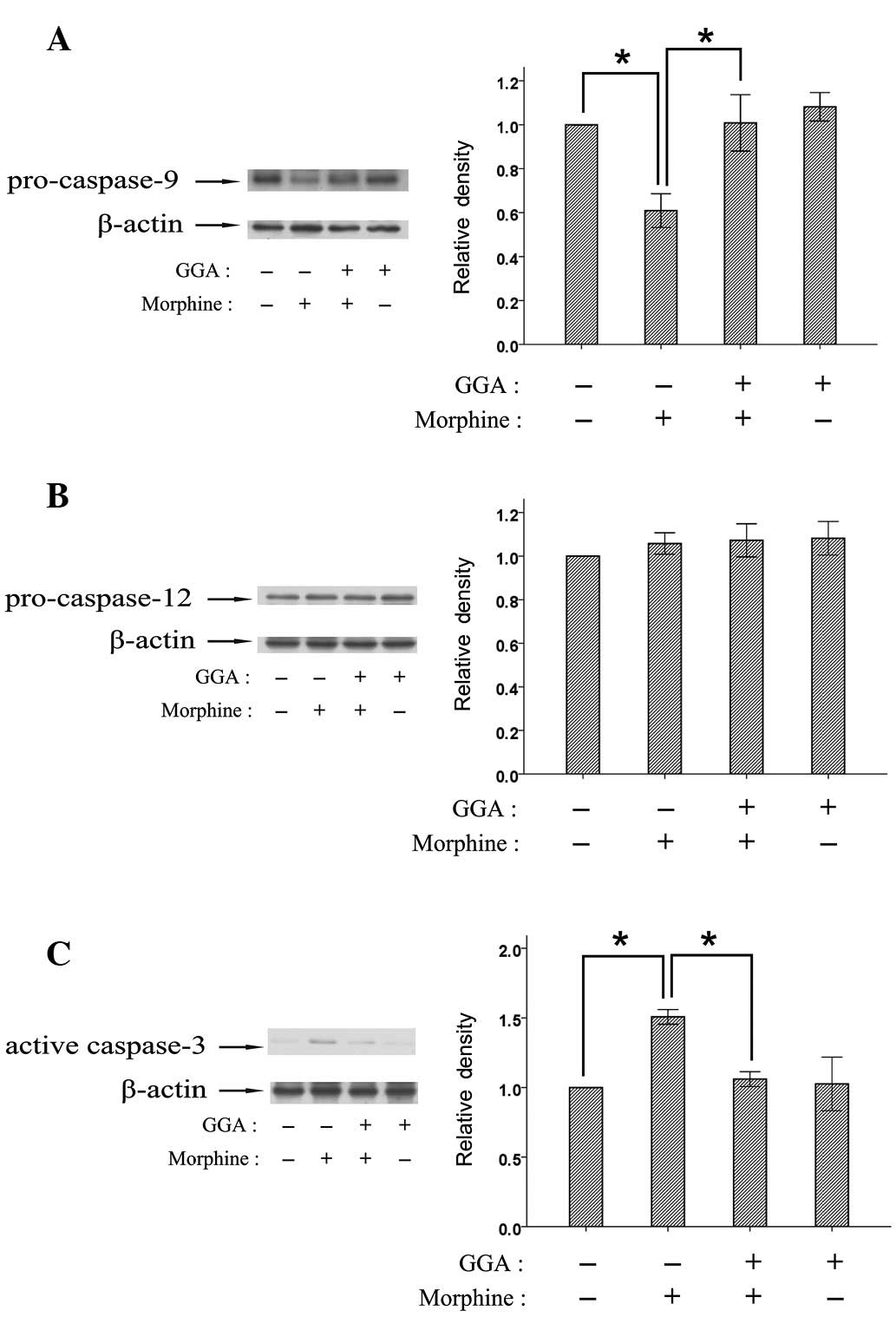 | Figure 2GGA regulated the activation of
caspases induced by morphine in the liver. Mice were injected with
escalating morphine doses twice daily (10, 20, 40, 60, 80 and 100
mg/kg), 2 h after GGA treatment (800 mg/kg, orally) for 7 days. Two
hours after the last morphine injection, the liver tissues of mice
were dissected, and the expression of (A) pro-caspase-9, (B) -12
and (C) caspase-3 was detected using western blotting.
Quantification is shown in the right panels (error bars represent
the mean± SD; n=4). Density values for each band were normalized
first to loading control and then to the control group. Asterisks
indicate a statistically significant difference
(*P<0.05). GGA, geranylgeranylacetone. |
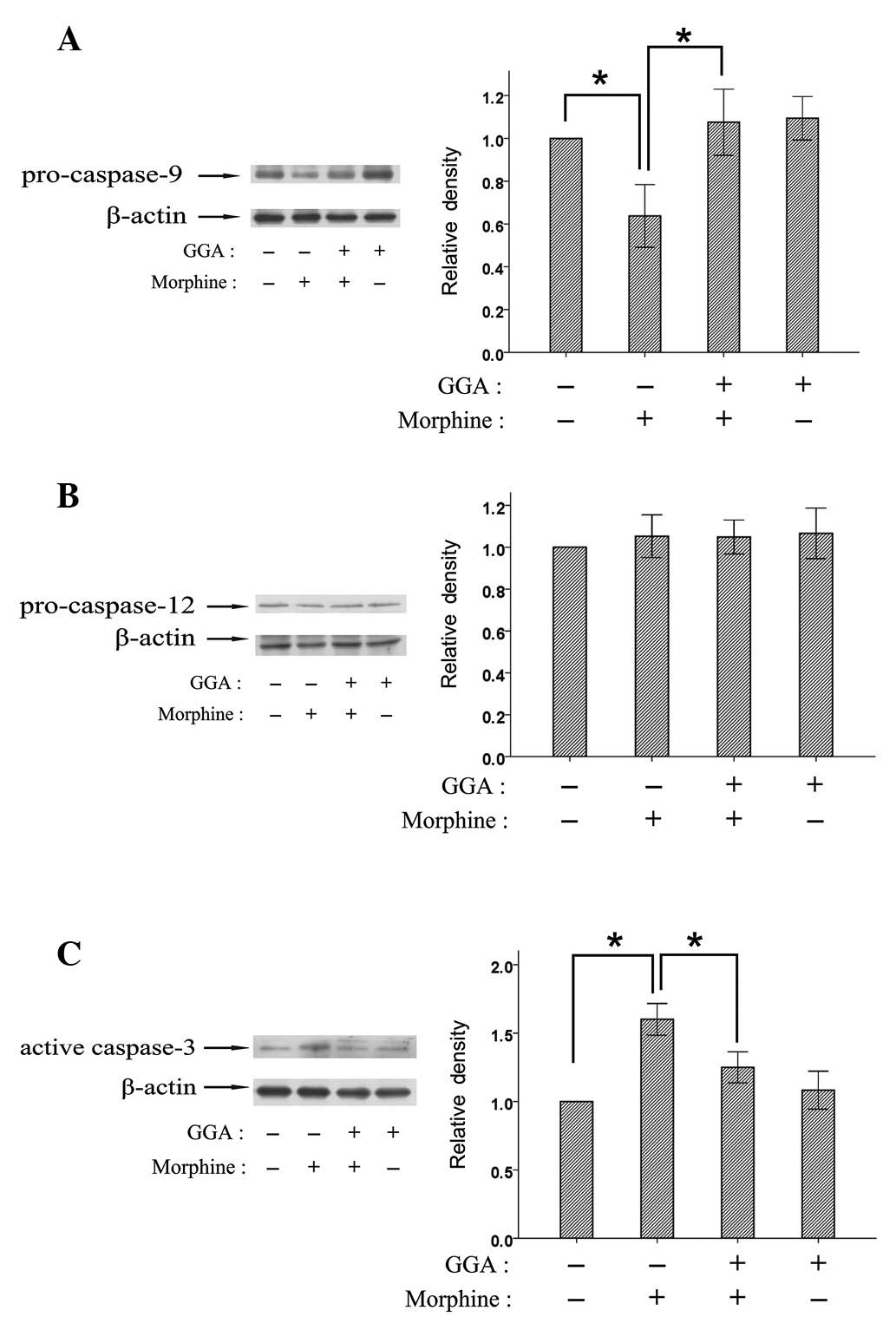 | Figure 3GGA regulated the activation of
caspases induced by morphine in the kidney. Mice were injected with
escalating morphine doses twice daily (10, 20, 40, 60, 80 and 100
mg/kg), 2 h after GGA treatment (800 mg/kg, orally) for 7 days. Two
hours after the last morphine injection, the kidney tissues of mice
were dissected, and the expression of (A) pro-caspase-9, (B) -12
and (C) caspase-3 was detected using western blotting.
Quantification is shown in the right panels (error bars represent
the mean ± SD; n=4). Density values for each band were normalized
first to loading control and then to the control group. Asterisks
indicate a statistically significant difference
(*P<0.05). GGA, geranylgeranylacetone. |
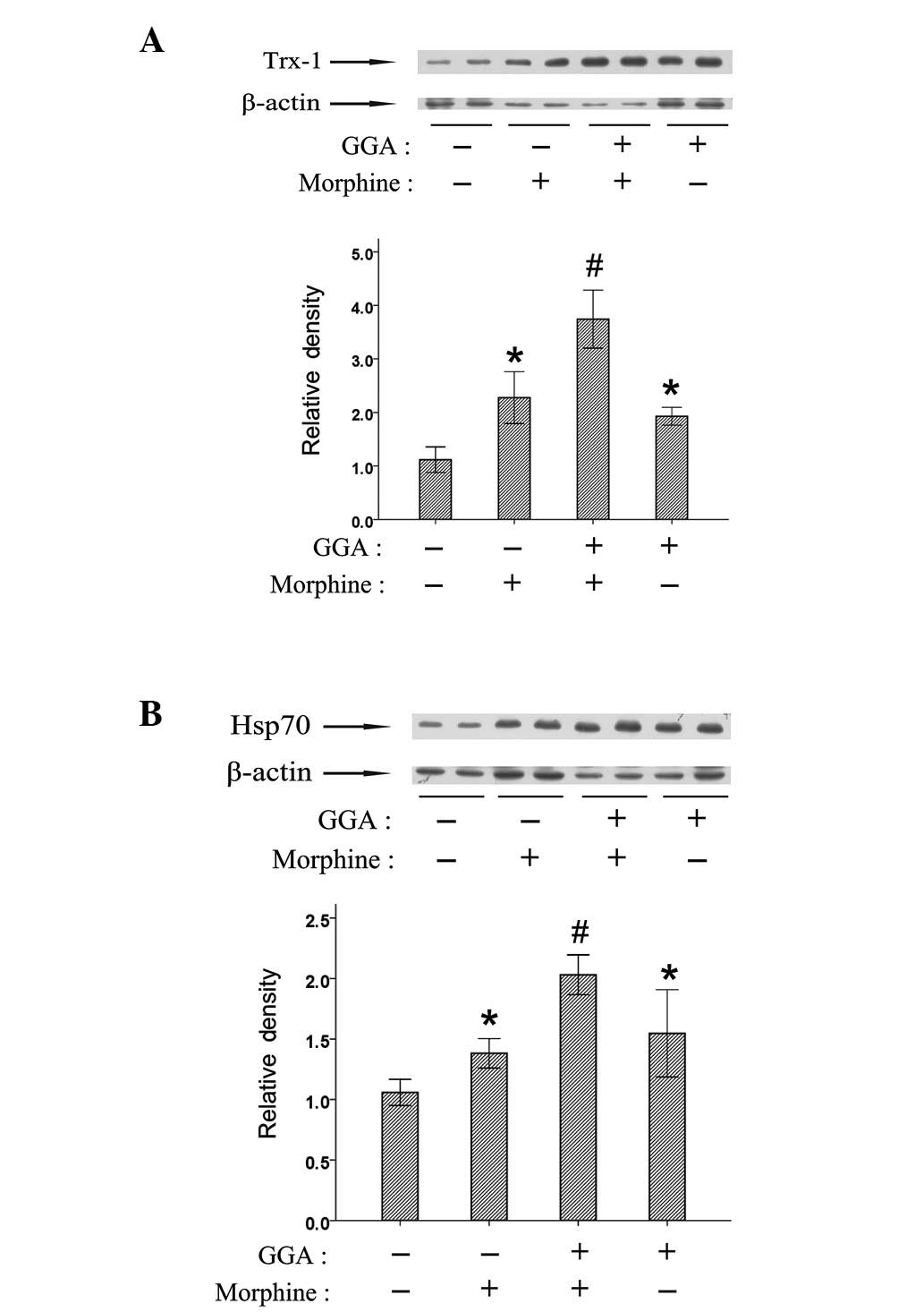
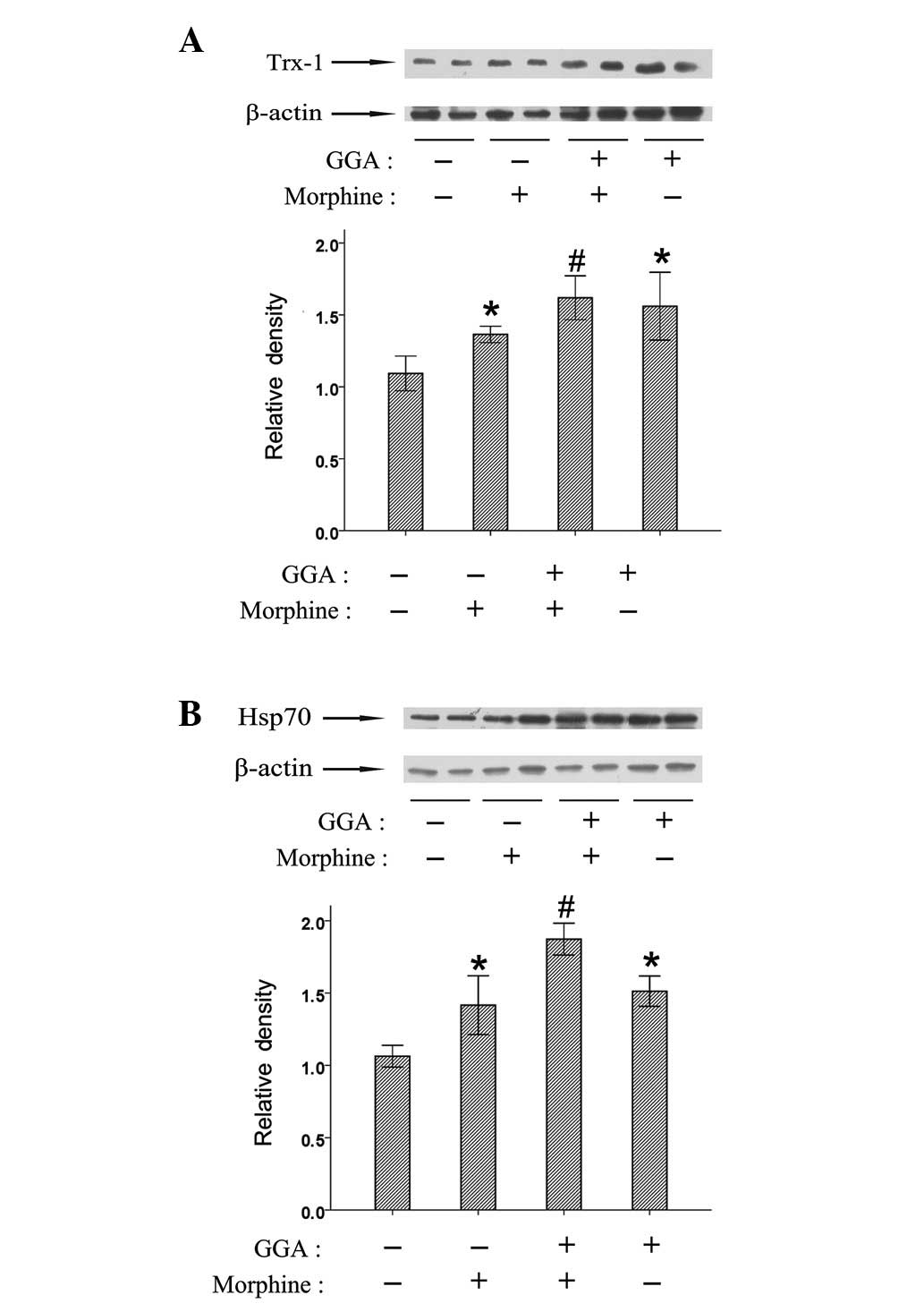
Effects of GGA on Trx-1 and Hsp70
expression in the liver and kidney following chronic morphine
treatment
To investigate the roles of Trx-1 and Hsp70
underlying the protective effect of GGA against morphine-induced
hepatic and renal damage, the levels of Trx-1 and Hsp70 were
examined following morphine treatment. Morphine significantly
increased the levels of Trx-1 and Hsp70 expression in the liver and
kidney (Figs. 4 and 5). GGA was also found to enhance
morphine-induced expression of Trx-1 and Hsp70 in the liver and
kidney. The above data indicated that GGA induced the expression of
Trx-1 and Hsp70, which may be involved in the protective roles of
GGA against morphine-induced hepatic and renal damage.
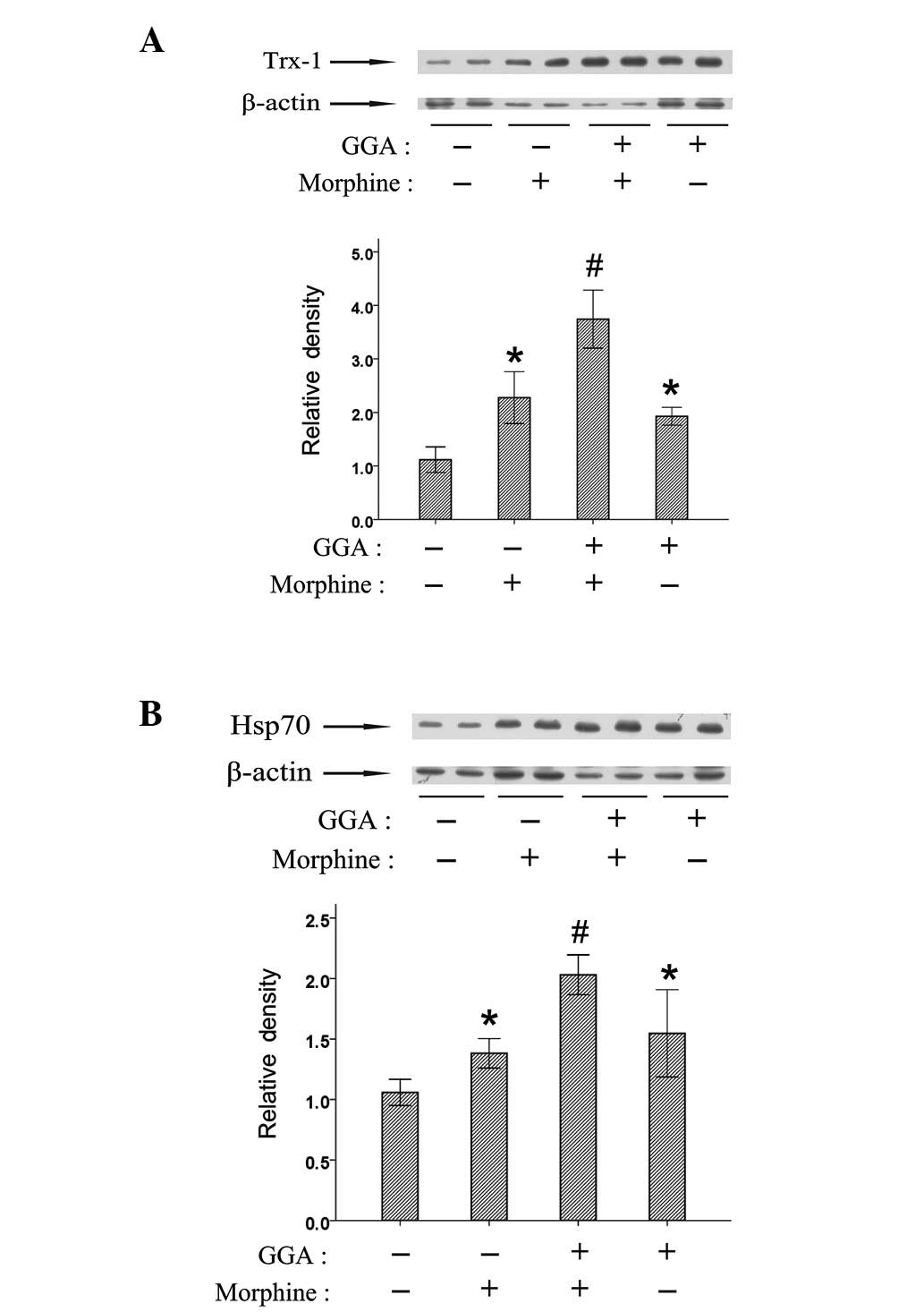 | Figure 4Changes in the expression of Trx-1
and Hsp70 after morphine treatment in the liver. Mice were injected
with escalating morphine doses twice daily (10, 20, 40, 60, 80 and
100 mg/kg), 2 h after GGA treatment (800 mg/kg, orally) for 7 days.
Two hours after the last morphine injection, the liver tissues of
mice were dissected, and the expression of (A) Trx-1 and (B) Hsp70
was detected using western blotting. Quantification is shown in the
right panels (error bars represent the mean ± SD; n=4). Density
values for each band were normalized first to loading control and
then to the control group. *P<0.05 vs. the control
group, and #P<0.05 vs. the chronic morphine-treated
group. GGA, geranylgeranylacetone; Hsp, heat shock protein. |
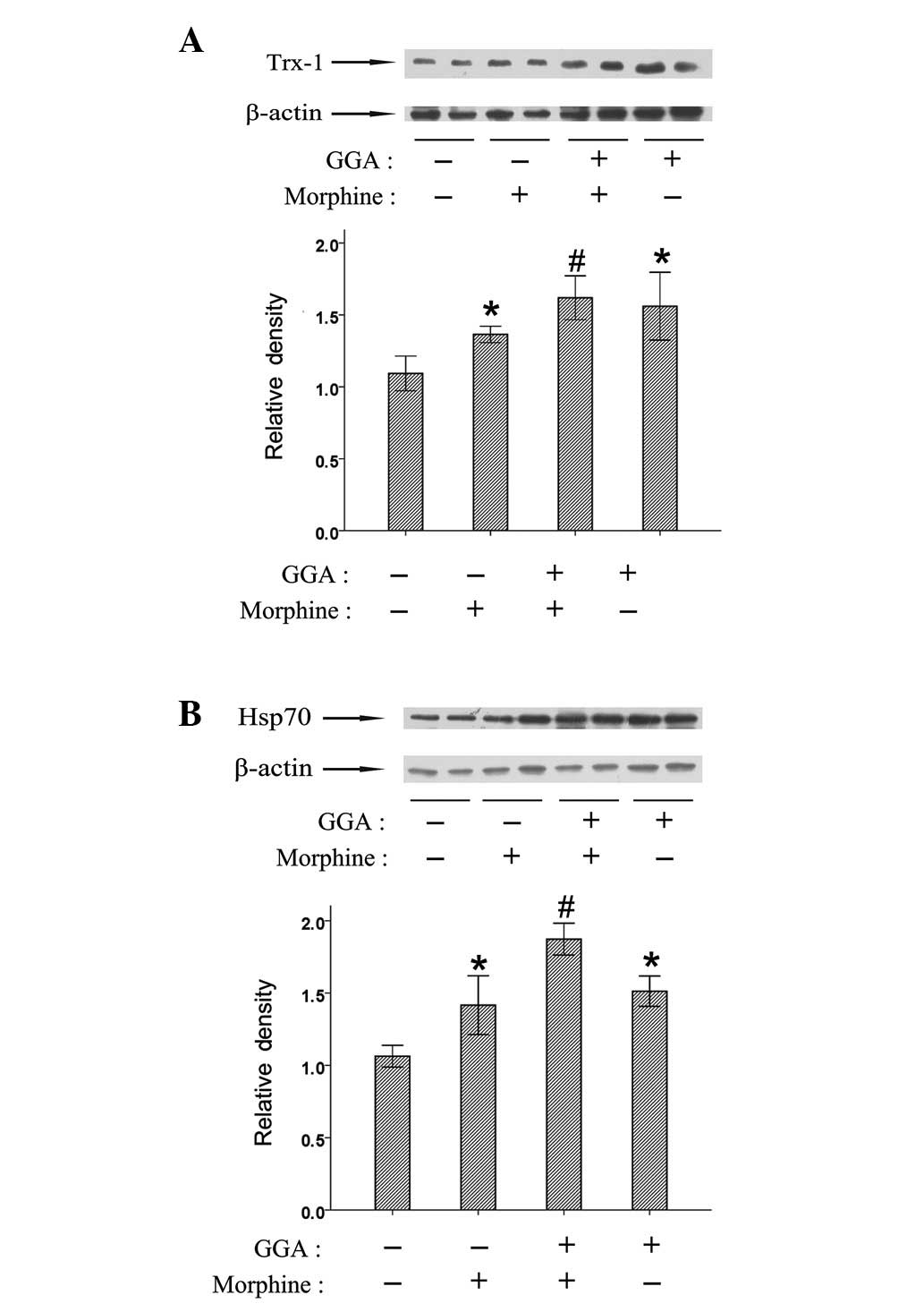 | Figure 5Changes in the expression of Trx-1
and Hsp70 after morphine treatment in the kidney. Mice were
injected with escalating morphine doses twice daily (10, 20, 40,
60, 80 and 100 mg/kg), 2 h after GGA treatment (800 mg/kg, orally)
for 7 days. Two hours after the last morphine injection, the kidney
tissues of mice were dissected, and the expression of (A) Trx-1 and
(B) Hsp70 was detected using western blotting. Quantification is
shown in the right panels (error bars represent the mean ± SD;
n=4). Density values for each band were normalized first to loading
control and then to the control group. *P<0.05 vs.
the control group, and #P<0.05 vs. the chronic
morphine-treated group. GGA, geranylgeranylacetone; Hsp, heat shock
protein. |
Discussion
GGA is an anti-ulcer drug developed in Japan and is
known to protect against organ and cell damage via inducing Hsp70
or Trx-1 expression. In the present study, we found that the
pre-treatment of GGA suppressed morphine-induced lipid peroxidation
and activation of caspases-9 and -3 in the liver and kidney. These
findings are consistent with those of previous studies, which
reported the protective effect of GGA against hepatic and renal
damage caused by other stimulations (30,31).
GGA suppressed the H2O2 and ethanol-induced
activation of JNK and caspases-9 and -3, leading to significant
inhibition of apoptosis in rat hepatocytes (32). Oral administration of GGA protects
liver damage following massive hepatectomy, warm
ischemic-reperfusion injury and exposure of acetaminophen in rats
(31,33,34).
In addition, GGA ameliorated ischemic acute renal failure via
inducing Hsp70 expression (35).
The dose of GGA used in this study is 800 mg/kg. However, it did
not show toxic effects in the present study. The results of our
previous animal experiment revealed that the pre-treatment of GGA
(800 mg/kg, 1 week) protected against morphine-induced
hyperlocomotion, rewarding effect and withdrawal syndrome (29). Oral GGA (600 and 1,200 mg/kg, 7
weeks) ameliorates symptomatic phenotypes of spinal and bulbar
muscular atrophy mice (36). There
is little information concerning any adverse drug effects of GGA.
These results suggest that GGA is a promising safe therapeutic
candidate for opioid drug-induced hepatic and renal damage. Besides
the cytoprotection in the liver and kidney, GGA also exerts
protective effects against various stresses in other organs,
including the heart and brain (37–39).
The toxicities of morphine in a number of tissues, including the
spinal cord and brain, have also been reported (40,41).
Whether or not GGA is able to protect against morphine-induced
toxicity in other organs remains to be elucidated.
Liver and kidney toxicities have been reported in
chronic use of morphine (10,42).
Serum aspartate aminotransferase and alanine aminotransferase
levels are increased following exposure to morphine in rats
(13). Animal studies have shown
that morphine may have a direct effect on the glomerulus, causing
oxidative stress, proliferation of fibroblasts and a decrease in
the degradation of type IV collagen (43–45).
Excessive free radical formation or antioxidant deficiency may
result in oxidative stress, a possible mechanism of the toxicity of
opioid drugs. Heroin abusers exhibited increased levels of
lipoperoxides and nitric oxide. The levels of various antioxidants,
including superoxide dismutase, glutathione and catalase, were
decreased following heroin or morphine exposure (46). It has also been reported that
morphine may result in lipid peroxidation in the liver and kidney
(13). In the present study, we
found that morphine increased MDA levels, demonstrating lipid
peroxidation in the liver and kidney following chronic morphine
treatment.
Extrinsic and intrinsic cell death pathways have
been shown to be involved in morphine-induced apoptosis. The
extrinsic cell death pathway has been reported to contribute to
morphine-induced macrophage apoptosis. Morphine enhanced Fas and
FasL expression in macrophages (47). The intrinsic cell death pathway
includes the mitochondria-mediated apoptosis pathway and
endoplasmic reticulum (ER)-mediated apoptosis pathway. Although
activation of several distinct upstream pathways may lead to
apoptosis, caspase-3 may be a common integration point (48). In the present study, we found that
caspase-3 was activated by morphine, suggesting that morphine leads
to apoptosis in the liver and kidney. Mitochondrial dysfunction
leads to the release of cytochrome c into the cytoplasm, and
initiates the activation of the caspase cascade by triggering the
activation of caspase-9, which elicits the activation of caspase-3,
leading to the morphological changes associated with apoptosis
(49). The results of in
vivo and in vitro studies indicate that caspases-9 and
-3 are activated following morphine treatment in macrophages, the
spinal cord or brain (41,50). In this study, we demonstrated that
morphine decreased the level of pro-caspase-9 expression,
indicating that morphine induces apoptosis through the
mitochondria-mediated pathway in the liver and kidney.
Pro-caspase-12 is localized on the cytoplasmic side of ER and is
proteolytically activated by excess ER stress. ER stress-induced
cell death has been reported to be mediated by the activation of
caspase-12 (51).
Caspase-12-deficient mice are resistant to ER stress-induced
apoptosis (52). However, in the
present study, the level of pro-caspase-12 expression was not
affected by morphine in the liver and kidney. These findings
suggest that the ER-mediated apoptosis pathway is not involved in
the morphine-induced apoptosis in the liver and kidney.
Eukaryotic cells have developed multiple mechanisms
to mount a response against environmental stressors. Cellular
stress responses require the activation of pro-survival pathways
and the production of molecules with antioxidant and anti-apoptotic
activities, allowing cells to effectively counteract diverse
stresses. Among the cellular pathways providing protection against
environmental stressors, a key role is played by vitagenes, such as
heat shock proteins and Trx-1 (53). Trx-1 expression is upregulated by
various stressors, including viral infection, mitogens, polycyclic
aromatic hydrocarbons, X-ray and UV irradiation, hydrogen peroxide
and ischemic reperfusion (54).
Hsp70 is also induced in response to a wide variety of stressors,
such as heat shock, ischemia, hydrogen peroxide and light damage
(26). The induction of Trx-1 and
Hsp70 contributes to cytoprotection against diverse stresses. It
has been reported that morphine increased Hsp70 expression in the
frontal cortex, amygdale and spinal cord (41,55,56).
Our previous study demonstrated that the levels of Trx-1 and Hsp70
expression in the nucleus accumbens of mice brain are increased
after chronic morphine treatment (29). In the present study, we found that
Trx-1 and Hsp70 were induced by morphine in the liver and kidney.
These results suggest that cellular defense mechanisms are
activated in the liver and kidney to resist the cellular damage
caused by morphine.
Modulation of endogenous cellular defense mechanisms
via the stress response signaling is becoming an innovative
approach to therapeutic intervention in diseases. Several studies
have used Trx-1 or Hsp70 inducers, including GGA, sulforaphane,
panaxatriol saponins and neurotropin, for therapeutic purposes
(57–60). In the present study, we found that
the increased level of MDA in the liver and kidney was suppressed
by the pre-treatment with GGA. The morphine-induced decrease of
pro-caspase-9 was suppressed by GGA. Furthermore, GGA inhibited the
morphine-induced activation of caspase-3 in the liver and kidney.
These results suggest that GGA treatment may be beneficial for
preventing morphine-induced hepatic and renal damage. In the
present study, we also demonstrated that GGA increased Trx-1 and
Hsp70 expression in the liver and kidney following morphine
treatment. A previous study has shown that morphine promotes p38
MAPK phosphorylation via opiate receptors through TGF-β and
iNOS-mediated downstream signaling (47). Trx-1 is known to have
radical-scavenging activity and scavenge hydrogen peroxide in
cooperation with peroxiredoxin. In addition, Trx-1 has been
reported to act as an endogenous inhibitor of apoptosis signaling
kinase 1 and p38 MAPK (61,62).
Hsp70 regulates the cellular redox status by modulating
glutathione-related enzyme activities (63). Hsp70 enhances the survival of cells
and prevents apoptosis against oxidative damage during various
stress conditions (21). The
antioxidant effects of GGA were previously reported in the ethanol-
and H2O2-induced cultured rat hepatocyte
injury and in light-induced photoreceptor cell damage through
inducing Trx-1 expression (58,64).
Thus, the protective effects of GGA against morphine-induced lipid
peroxidation and apoptosis in the liver and kidney might contribute
to the increased expression of Trx-1 and Hsp70.
In conclusion, the findings of the present study
indicate that morphine induces lipid peroxidation and
mitochondria-mediated apoptosis, and regulates Trx-1 and Hsp70
expression in the liver and kidney. GGA induced Trx-1 and Hsp70
expression and suppressed morphine-induced lipid peroxidation and
apoptosis in the liver and kidney. Our results suggest that GGA is
a promising therapeutic candidate for morphine-induced hepatic and
renal damage.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (no. 81160162, U1202227), a grant from
the Candidates of the Young and Middle Aged Academic Leaders of
Yunnan Province (no. 2006PY01-07), Application Basic Research Fund
of the Yunnan Province (no. 2009ZC165M), the foundation of
Excellent Doctor Degree Dissertation of the Kunming University of
Science and Technology and grant from the Key Laboratory of Medical
Neurobiology, Kunming University of Science and Technology,
China.
References
|
1
|
Christie MJ: Cellular neuroadaptations to
chronic opioids: tolerance, withdrawal and addiction. Br J
Pharmacol. 154:384–396. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Weller IV, Cohn D, Sierralta A, et al:
Clinical, biochemical, serological, histological and
ultrastructural features of liver disease in drug abusers. Gut.
25:417–423. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Colombo JP and Colombo J: Plasma
gamma-glutamyl transpeptidase in heroin addicts. Clin Chim Acta.
95:483–486. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
May B and Helmstaedt D: Liver disease in
drug addicts: clinical course-toxicological and clinical
pharmacological aspects. Int J Clin Pharmacol Biopharm. 12:50–56.
1975.PubMed/NCBI
|
|
5
|
Cunningham EE, Brentjens JR, Zielezny MA,
Andres GA and Venuto RC: Heroin nephropathy. A clinicopathologic
and epidemiologic study. Am J Med. 68:47–53. 1980.PubMed/NCBI
|
|
6
|
Connolly JO, Gillmore JD, Lachmann HJ,
Davenport A, Hawkins PN and Woolfson RG: Renal amyloidosis in
intravenous drug users. QJM. 99:737–742. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dettmeyer R, Wessling B and Madea B:
Heroin associated nephropathy - a post-mortem study. Forensic Sci
Int. 95:109–116. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bakir AA and Dunea G: Drugs of abuse and
renal disease. Curr Opin Nephrol Hypertens. 5:122–126. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jaffe JA and Kimmel PL: Chronic
nephropathies of cocaine and heroin abuse: a critical review. Clin
J Am Soc Nephrol. 1:655–667. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Payabvash S, Beheshtian A, Salmasi AH, et
al: Chronic morphine treatment induces oxidant and apoptotic damage
in the mice liver. Life Sci. 79:972–980. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Panchenko LF, Pirozhkov SV, Nadezhdin AV,
Baronets Vlu and Usmanova NN: Lipid peroxidation, peroxyl
radical-scavenging system of plasma and liver and heart pathology
in adolescence heroin users. Vopr Med Khim. 45:501–506. 1999.(In
Russian).
|
|
12
|
Sumathi T and Niranjali Devaraj S: Effect
of Bacopa monniera on liver and kidney toxicity in chronic
use of opioids. Phytomedicine. 16:897–903. 2009.
|
|
13
|
Atici S, Cinel I, Cinel L, Doruk N,
Eskandari G and Oral U: Liver and kidney toxicity in chronic use of
opioids: an experimental long term treatment model. J Biosci.
30:245–252. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang YT, Zheng QS, Pan J and Zheng RL:
Oxidative damage of biomolecules in mouse liver induced by morphine
and protected by antioxidants. Basic Clin Pharmacol Toxicol.
95:53–58. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Burke-Gaffney A, Callister ME and Nakamura
H: Thioredoxin: friend or foe in human disease? Trends Pharmacol
Sci. 26:398–404. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lillig CH and Holmgren A: Thioredoxin and
related molecules - from biology to health and disease. Antioxid
Redox Signal. 9:25–47. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chae HZ, Chung SJ and Rhee SG:
Thioredoxin-dependent peroxide reductase from yeast. J Biol Chem.
269:27670–27678. 1994.PubMed/NCBI
|
|
18
|
Das KC and Das CK: Thioredoxin, a singlet
oxygen quencher and hydroxyl radical scavenger: redox independent
functions. Biochem Biophys Res Commun. 277:443–447. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Nakamura H, Matsuda M, Furuke K, et al:
Adult T cell leukemia-derived factor/human thioredoxin protects
endothelial F-2 cell injury caused by activated neutrophils or
hydrogen peroxide. Immunol Lett. 42:75–80. 1994. View Article : Google Scholar
|
|
20
|
Takagi Y, Mitsui A, Nishiyama A, et al:
Overexpression of thioredoxin in transgenic mice attenuates focal
ischemic brain damage. Proc Natl Acad Sci USA. 96:4131–4136. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Evans CG, Chang L and Gestwicki JE: Heat
shock protein 70 (hsp70) as an emerging drug target. J Med Chem.
53:4585–4602. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bai J, Nakamura H, Hattori I, Tanito M and
Yodoi J: Thioredoxin suppresses 1-methyl-4-phenylpyridinium-induced
neurotoxicity in rat PC12 cells. Neurosci Lett. 321:81–84. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Dekigai H, Nakamura H, Bai J, et al:
Geranylgeranylacetone promotes induction and secretion of
thioredoxin in gastric mucosal cells and peripheral blood
lymphocytes. Free Radic Res. 35:23–30. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Fudaba Y, Ohdan H, Tashiro H, et al:
Geranylgeranylacetone, a heat shock protein inducer, prevents
primary graft nonfunction in rat liver transplantation.
Transplantation. 72:184–189. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yamagami K, Yamamoto Y, Ishikawa Y,
Yonezawa K, Toyokuni S and Yamaoka Y: Effects of
geranyl-geranyl-acetone administration before heat shock
preconditioning for conferring tolerance against
ischemia-reperfusion injury in rat livers. J Lab Clin Med.
135:465–475. 2000. View Article : Google Scholar
|
|
26
|
Ooie T, Takahashi N, Saikawa T, et al:
Single oral dose of geranylgeranylacetone induces heat-shock
protein 72 and renders protection against ischemia/reperfusion
injury in rat heart. Circulation. 104:1837–1843. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Fujiki M, Kobayashi H, Abe T and Ishii K:
Astroglial activation accompanies heat shock protein upregulation
in rat brain following single oral dose of geranylgeranylacetone.
Brain Res. 991:254–257. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yamanaka K, Takahashi N, Ooie T, Kaneda K,
Yoshimatsu H and Saikawa T: Role of protein kinase C in
geranylgeranylacetone-induced expression of heat-shock protein 72
and cardioprotection in the rat heart. J Mol Cell Cardiol.
35:785–794. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Luo FC, Qi L, Lv T, et al:
Geranylgeranylacetone protects mice against morphine-induced
hyperlocomotion, rewarding effect, and withdrawal syndrome. Free
Radic Biol Med. 52:1218–1227. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mao H, Li Z, Zhou Y, et al: HSP72
attenuates renal tubular cell apoptosis and interstitial fibrosis
in obstructive nephropathy. Am J Physiol Renal Physiol.
295:F202–F214. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fudaba Y, Tashiro H, Miyata Y, et al: Oral
administration of geranylgeranylacetone protects rat livers from
warm ischemic injury. Transplant Proc. 31:2918–2919. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ikeyama S, Kusumoto K, Miyake H, Rokutan K
and Tashiro S: A non-toxic heat shock protein 70 inducer,
geranylgeranylacetone, suppresses apoptosis of cultured rat
hepatocytes caused by hydrogen peroxide and ethanol. J Hepatol.
35:53–61. 2001. View Article : Google Scholar
|
|
33
|
Nishida T, Matsura T, Nakada J, et al:
Geranylgeranylacetone protects against acetaminophen-induced
hepatotoxicity by inducing heat shock protein 70. Toxicology.
219:187–196. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kanemura H, Kusumoto K, Miyake H, Tashiro
S, Rokutan K and Shimada M: Geranylgeranylacetone prevents acute
liver damage after massive hepatectomy in rats through suppression
of a CXC chemokine GRO1 and induction of heat shock proteins. J
Gastrointest Surg. 13:66–73. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Suzuki S, Maruyama S, Sato W, et al:
Geranylgeranylacetone ameliorates ischemic acute renal failure via
induction of Hsp70. Kidney Int. 67:2210–2220. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Katsuno M, Sang C, Adachi H, et al:
Pharmacological induction of heat-shock proteins alleviates
polyglutamine-mediated motor neuron disease. Proc Natl Acad Sci
USA. 102:16801–16806. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ooie T, Kajimoto M, Takahashi N, et al:
Effects of insulin resistance on geranylgeranylacetone-induced
expression of heat shock protein 72 and cardioprotection in
high-fat diet rats. Life Sci. 77:869–881. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Kim YH, Song JJ, Kim YC, et al:
Geranylgeranylacetone ameliorates acute cochlear damage caused by
3-nitropropionic acid. Neurotoxicology. 31:317–325. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhang K, Zhao T, Huang X, et al:
Preinduction of HSP70 promotes hypoxic tolerance and facilitates
acclimatization to acute hypobaric hypoxia in mouse brain. Cell
Stress Chaperones. 14:407–415. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hassanzadeh K, Roshangar L, Habibi-asl B,
et al: Riluzole prevents morphine-induced apoptosis in rat cerebral
cortex. Pharmacol Rep. 63:697–707. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hassanzadeh K, Habibi-asl B, Farajnia S
and Roshangar L: Minocycline prevents morphine-induced apoptosis in
rat cerebral cortex and lumbar spinal cord: a possible mechanism
for attenuating morphine tolerance. Neurotox Res. 19:649–659. 2011.
View Article : Google Scholar
|
|
42
|
Crowe AV, Howse M, Bell GM and Henry JA:
Substance abuse and the kidney. QJM. 93:147–152. 2000. View Article : Google Scholar
|
|
43
|
Singhal PC, Sharma P, Sanwal V, et al:
Morphine modulates proliferation of kidney fibroblasts. Kidney Int.
53:350–357. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Singhal PC, Gibbons N and Abramovici M:
Long term effects of morphine on mesangial cell proliferation and
matrix synthesis. Kidney Int. 41:1560–1570. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Patel J, Manjappa N, Bhat R, Mehrotra P,
Bhaskaran M and Singhal PC: Role of oxidative stress and heme
oxygenase activity in morphine-induced glomerular epithelial cell
growth. Am J Physiol Renal Physiol. 285:F861–F869. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Pan J, Zhang Q, Zhang Y, Ouyang Z, Zheng Q
and Zheng R: Oxidative stress in heroin administered mice and
natural antioxidants protection. Life Sci. 77:183–193. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Singhal PC, Bhaskaran M, Patel J, et al:
Role of p38 mitogen-activated protein kinase phosphorylation and
Fas-Fas ligand interaction in morphine-induced macrophage
apoptosis. J Immunol. 168:4025–4033. 2002. View Article : Google Scholar
|
|
48
|
Khanna N and Singh N: Role of caspases in
apoptosis and disease. Indian J Physiol Pharmacol. 43:151–159.
1999.
|
|
49
|
Friedlander RM: Apoptosis and caspases in
neurodegenerative diseases. N Engl J Med. 348:1365–1375. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Hassanzadeh K, Habibi-asl B, Roshangar L,
Nemati M, Ansarin M and Farajnia S: Intracerebroventricular
administration of riluzole prevents morphine-induced apoptosis in
the lumbar region of the rat spinal cord. Pharmacol Rep.
62:664–673. 2010. View Article : Google Scholar
|
|
51
|
Fujita E, Kouroku Y, Jimbo A, Isoai A,
Maruyama K and Momoi T: Caspase-12 processing and fragment
translocation into nuclei of tunicamycin-treated cells. Cell Death
Differ. 9:1108–1114. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Nakagawa T, Zhu H, Morishima N, et al:
Caspase-12 mediates endoplasmic-reticulum-specific apoptosis and
cytotoxicity by amyloid-beta. Nature. 403:98–103. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Calabrese V, Cornelius C, Mancuso C, et
al: Vitagenes, dietary antioxidants and neuroprotection in
neurodegenerative diseases. Front Biosci. 14:376–397. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Masutani H, Bai J, Kim YC and Yodoi J:
Thioredoxin as a neurotrophic cofactor and an important regulator
of neuroprotection. Mol Neurobiol. 29:229–242. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Ammon S, Mayer P, Riechert U, Tischmeyer H
and Hollt V: Microarray analysis of genes expressed in the frontal
cortex of rats chronically treated with morphine and after naloxone
precipitated withdrawal. Brain Res Mol Brain Res. 112:113–125.
2003. View Article : Google Scholar
|
|
56
|
Rodriguez Parkitna JM, Bilecki W,
Mierzejewski P, et al: Effects of morphine on gene expression in
the rat amygdala. J Neurochem. 91:38–48. 2004.PubMed/NCBI
|
|
57
|
Hoshino Y, Nakamura T, Sato A, Mishima M,
Yodoi J and Nakamura H: Neurotropin demonstrates cytoprotective
effects in lung cells through the induction of thioredoxin-1. Am J
Respir Cell Mol Biol. 37:438–446. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Tanito M, Kwon YW, Kondo N, et al:
Cytoprotective effects of geranylgeranylacetone against retinal
photooxidative damage. J Neurosci. 25:2396–2404. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tanito M, Masutani H, Kim YC, Nishikawa M,
Ohira A and Yodoi J: Sulforaphane induces thioredoxin through the
antioxidant-responsive element and attenuates retinal light damage
in mice. Invest Ophthalmol Vis Sci. 46:979–987. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Luo FC, Wang SD, Li K, Nakamura H, Yodoi J
and Bai J: Panaxatriol saponins extracted from Panax
notoginseng induces thioredoxin-1 and prevents
1-methyl-4-phenylpyridinium ion-induced neurotoxicity. J
Ethnopharmacol. 127:419–423. 2010.
|
|
61
|
Hashimoto S, Matsumoto K, Gon Y, et al:
Thioredoxin negatively regulates p38 MAP kinase activation and IL-6
production by tumor necrosis factor-alpha. Biochem Biophys Res
Commun. 258:443–447. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Saitoh M, Nishitoh H, Fujii M, et al:
Mammalian thioredoxin is a direct inhibitor of apoptosis
signal-regulating kinase (ASK) 1. EMBO J. 17:2596–2606. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Guo S, Wharton W, Moseley P and Shi H:
Heat shock protein 70 regulates cellular redox status by modulating
glutathione-related enzyme activities. Cell Stress Chaperones.
12:245–254. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Hirota K, Nakamura H, Arai T, et al:
Geranylgeranylacetone enhances expression of thioredoxin and
suppresses ethanol-induced cytotoxicity in cultured hepatocytes.
Biochem Biophys Res Commun. 275:825–830. 2000. View Article : Google Scholar : PubMed/NCBI
|