Introduction
Human colorectal cancer (CRC) is a type of cancer
that arises from uncontrolled cell growth in the colon or rectum,
sections of the large intestine or in the appendix (1). Genetic analysis shows that colon and
rectal tumors are essentially the same type of cancer (2). CRC is the third most commonly
diagnosed type of cancer in males and the second in females, and in
2008 there was an estimated 1.2 million novel CRC cases and 608,700
mortalities (3,4). Symptoms of CRC typically include
rectal bleeding and anemia, which may be associated with weight
loss and changes in bowel habits (5). The majority of CRC cases are a result
of lifestyle and increasing age, with a minority of cases
associated with underlying genetic disorders (6,7).
Cancers confined within the wall of the colon are often curable
with surgery, while cancers that have metastasized around the body
are usually incurable. At present, studies primarily focus on tumor
chemotherapy (8); however, the
pathogenesis of CRC remains unclear. Current management focuses on
extending patient lifespan via chemotherapy and improving quality
of life (9).
Tissue transglutaminase (tTG) is a matricellular
protein, which is expressed in multiple tissue and cell types
(10). It is unclear whether tTG
is important in CRC and if so, whether tTG may be inhibited by
certain of drugs. Fluorouracil is a standard chemotherapeutic agent
used in the treatment of CRC (11). Treatment options for CRC also
include additional chemotherapeutic agents and targeted therapies,
including cetuximab, panitumumab and bevacizumab (12). Correct use of these therapies may
result in a positive impact on patient prognosis (13).
Previously, data concerning cancer treatment using
traditional Chinese medicine has affected a number of cancer
treatments (14). It remains
unclear whether certain traditional Chinese medicines may be used
to inhibit tTG expression and improve the symptoms of CRC.
Cantharidin (also termed cantharidinate) has been used in
traditional Chinese medicine (15,16).
Cantharidinate induces cell cycle arrest and triggers apoptosis in
various types of tumor cells, including hepatoma, myeloma, oral
buccal carcinoma, leukemia, gastric cancer, human bladder carcinoma
TSGH-8301, colorectal cancer colo 205, A549 human lung cancer and
intestinal epithelial cells (17–20).
Therefore, the present study investigated the involvement of tTG in
human CRC and demonstrated that cantharidinate may be used to
inhibit the expression of tTG.
Materials and methods
Patients and tissue specimens
Twenty human CRC tissue specimens were obtained from
12 males and 8 females, (average age, 68.25 years; range, 21–87
years) by surgical resection between May 2011 and June 2012 in
Jilin University Second Hospital (Jilin, China). Written informed
patient consent was obtained and approval was acquired from the
Jilin University Second Hospital Ethics Committee (no. 2012–43).
Tissue microarrays (TMAs) were constructed. Histological tumor
grade of colon and sigmoid colon tissue were included in the
analysis. Expression of tTG was associated with patient
demographics, adjuvant treatment regimens and histological
parameters.
Histopathologic examination
Specimens and cells were examined using light
microscopy (Eclipse TE-2000-U equipped with an attached SXM1200F
digital camera; Nikon, Tokyo, Japan) following haematoxylin and
eosin (HE) staining.
Immunohistochemical staining
Paraffin-embedded slices (4-μm thick) were probed
with anti-human tTG monoclonal antibody (Sigma-Aldrich, St. Louis,
MO, USA; dilution, 1:300) at 4°C overnight. Sections were immersed
in 0.3% H2O2 in absolute methanol for 15 min
to block endogenous peroxidase. Color was developed using chromagen
3,3′-diaminobenzidine (DAB substrate kit and Immunohistochemistry
kit; Biosynthesis Biotechnology, Beijing, China). Slices were
counterstained with hematoxylin, mounted on glass coverslips and
sealed with neutral resin.
UCT-116 cell culture and treatment
UCT-116 human CRC cell lines were donated from Jilin
University Institute of Regenerative Medicine. UCT-116 cells were
routinely cultured in Dulbecco’s modified Eagle’s media (DMEM;
Gibco-BRL, Life Technologies, Carlsbad, CA, USA) supplemented with
20% fetal bovine serum (FBS; Gibco-BRL) and 50 U/ml antibiotics
under the conditions of 5% CO2 at 37°C. Following
trypsinization, cells were incubated in DMEM with 0.5% FBS for 24
h. Cells were treated with 2.5 μmol/l cantharidinate, provided by
Associate Professor Yang of the Second Hospital of Jilin University
and 2.5 μmol/l fluorouracil (Shanghai Hanhong Group, Shanghai,
China), with untreated cells used as a control, for 48 h.
Quantitative PCR (qPCR) analysis of
UCT-116 cells
Total RNA was extracted using TRIzol reagent
(Invitrogen Life Technologies, Carlsbad, CA, USA) according to the
manufacturer’s instructions. First strand cDNA was synthesized
using PrimeScript™RT enzyme mix I, oligo dT primers and random
hexamers (Takara Bio, Inc., Shiga, Japan). qPCR analysis was
performed using first strand cDNA, forward and reverse primers and
the SYBR premix Ex Taq™ Green II kit (Takara). Primers were
synthesized by Sangon Biotech Company (Shanghai, China) and the
sequences were as follows: Forward: 5′-GGCACAGTCAAGGCTGAGAATG-3′
and reverse: 5′-ATGGTGGTGAAGACGCCAGTA-3′ for glyceraldehyde
3-phosphate dehydrogenase (GAPDH) and forward:
5′-GACAAGCGCATCACACAGACA-3′ and reverse:
5′-TCTTTCGTTAGAGCCAAGGCC-3′ for tTG. Reaction and signal detection
were measured in triplicate independently by an iCyder iQ real-time
PCR Detection System (Bio-Rad, Hercules, CA, USA). mRNA levels were
calculated as the relative expression ratio compared with
GAPDH.
Statistical analysis
Statistical analysis of data was performed using
SPSS Version 11 for Windows (SPSS, Inc., Chicago, IL, USA). All
data are presented as the mean ± SEM. Statistical comparisons were
determined by Student’s t-test and P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinicopathological features and patient
outcome
The present study was performed on a TMA,
constructed from surgically resected samples of patients with
varying grades of differentiation of CRC. The demographics of the
patients are shown in Table I as
well as the clinicopathological features of the colon and the grade
of differentiation. The incidence of CRC of grades IIB, IIC, IIIB
and IIIA in males was 8.3, 8.3, 8.3 and 0%, respectively. The
incidence of CRC of grades IIB, IIC, IIIB and IIIA in females was
0, 0, 25 and 12.5%, respectively. The incidence of colon and
sigmoid colon cancer was 75 and 25% in males and 40 and 60% in
females, respectively.
 | Table IClinicopathological features of colon
cancer patient cohort (n=20). |
Table I
Clinicopathological features of colon
cancer patient cohort (n=20).
| Male (n=12) | Female (n=8) |
|---|
| Age (years) |
| Mean | 63.5 | 73.375 |
| Range | 21–80 | 63–87 |
| Minimum | 21 (12.5%) | 63 (25%) |
| Maximum | 80 (12.5%) | 87 (37.5%) |
| Grade of
differentiation |
| IIB | 1 (8.3%) | 0 |
| IIC | 1 (8.3%) | 0 |
| IIIB | 1 (8.3%) | 2 (25%) |
| IIIA | 0 | 1 (12.5%) |
| A moderately
differentiated adenocarcinoma | 9 (75%). | 5 (40%) |
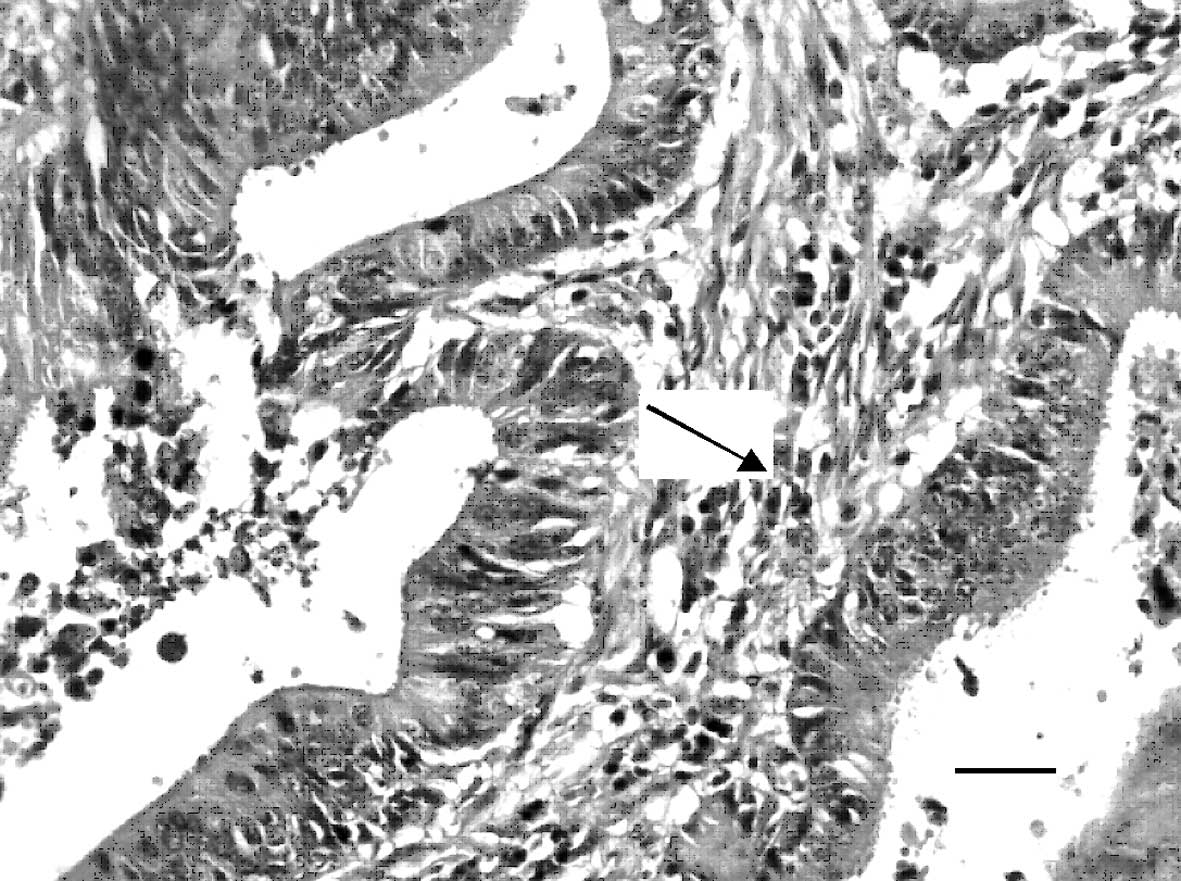
H&E of human CRC tissues
Following standard H&E staining, normal colon
tissue and the CRC TMAs were observed to have representative
histological structures by microscopy (Fig. 1). The immunohistochemical staining
of microarray samples was representative (Fig. 2A and B).
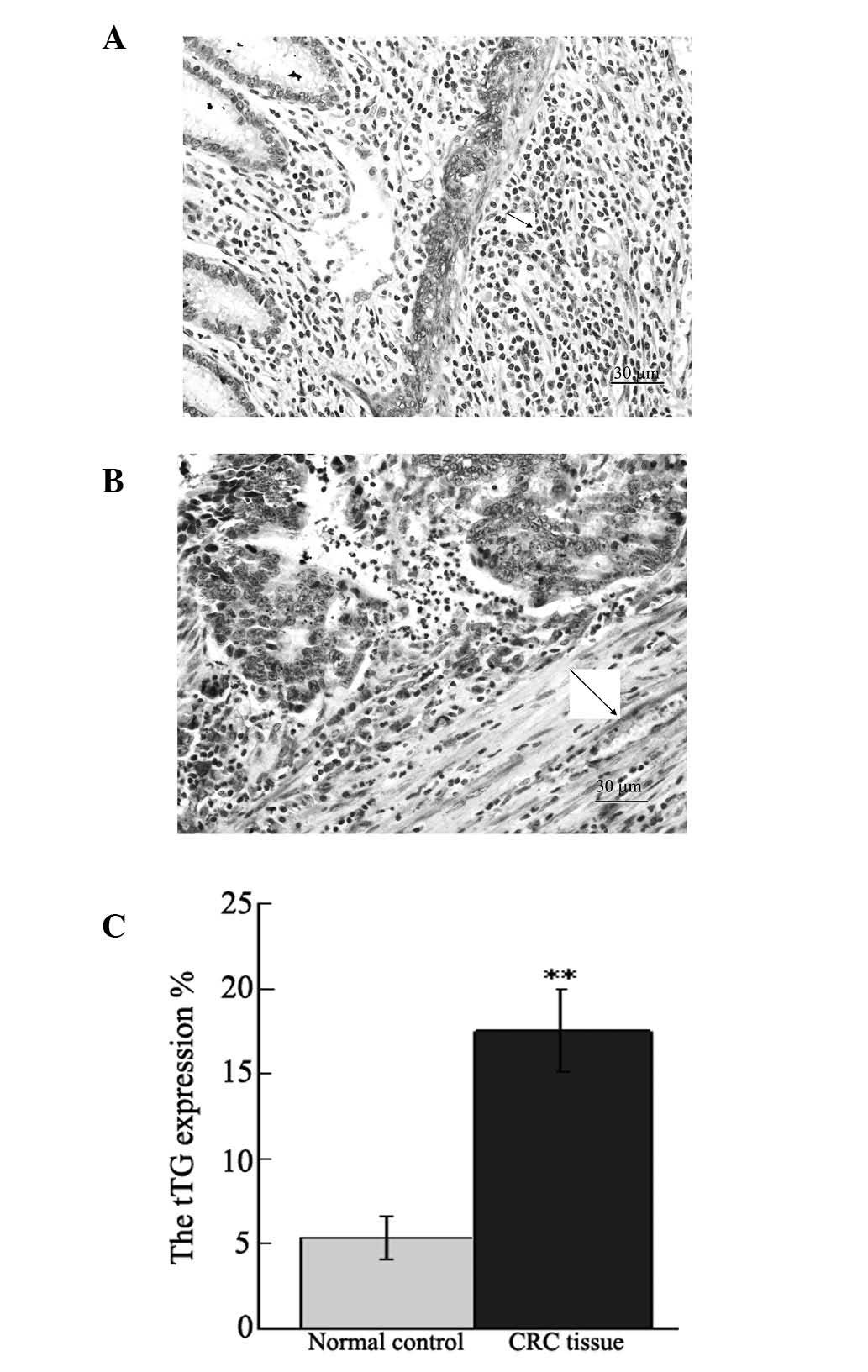
Immunohistochemical staining of tTG in
human CRC tissue
Immunohistochemical staining was used to determine
the expression of tTG protein in human CRC tissue. The results
showed that tTG was expressed in the membrane and cytoplasm of the
normal tissue of patients with CRC (Fig. 2A). The expression of tTG markedly
increased in CRC tissue. tTG was primarily expressed in the tumor
and interstitial regions (Fig.
2B). The expression of tTG exhibited a significant difference
between CRC and normal tissue (P<0.01; Fig 2C).
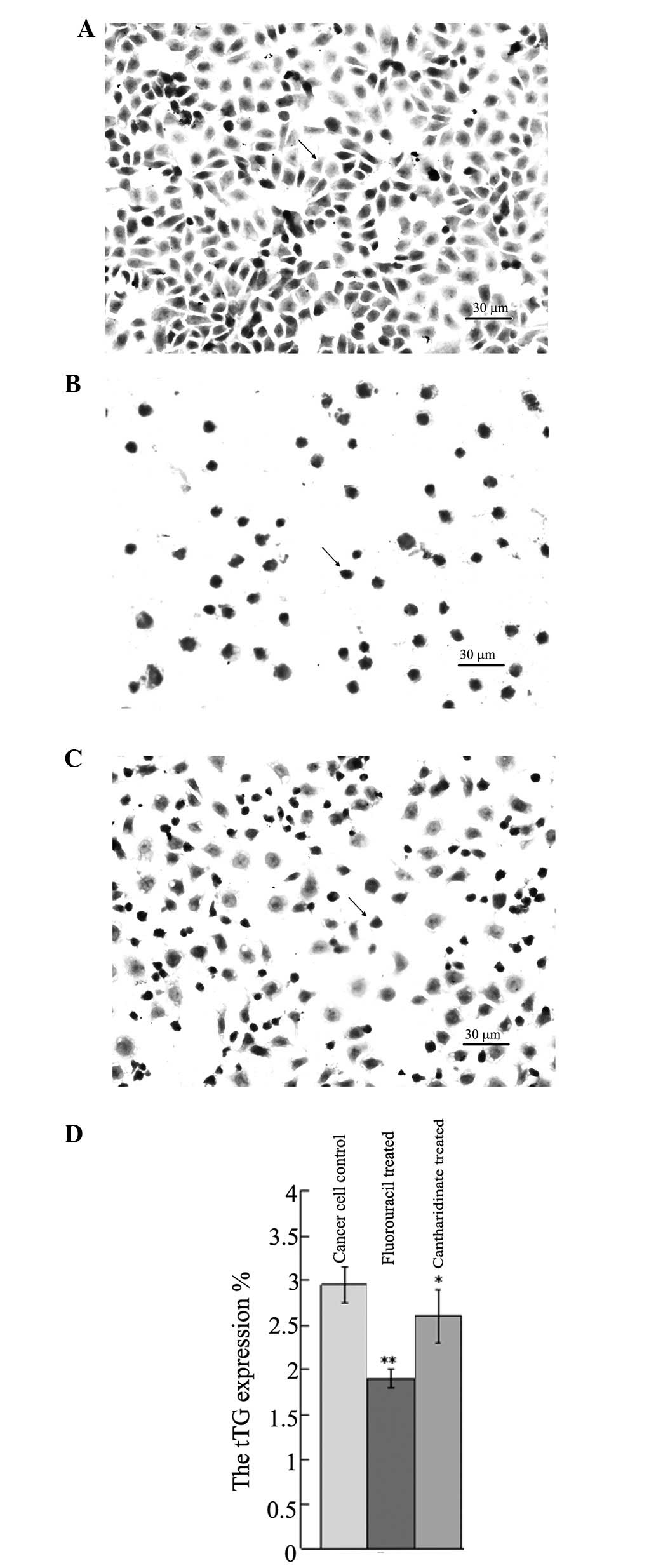
H&E staining of UCT-116 cells
Pathological changes of UCT-116 human CRC cells in
various groups are shown in Fig.
3A–C. The quantity of UCT-116 cells decreased 48 h following
the application of fluorouracil and cantharidinate (Fig. 3B and C). This result suggested that
cantharidinate may exert an accessorial effect and may reduce the
chemotherapeutic time, subsequently decreasing the side-effects of
the treatment of human CRC.
Immunohistochemical staining detects tTG
in UCT-116 cells
Fig. 4 shows tTG
immunohistochemical staining in UCT-116 cells. Immunohistochemical
staining detected a high level of tTG in the untreated UCT-116 cell
control (Fig. 4A and D).
Cantharidinate and fluorouracil treatment decreased the level of
tTG in UCT-116 cells significantly (P<0.05; Fig. 4B–D). This result suggested that
cantharidinate may inhibit the expression of tTG and block tumor
growth.
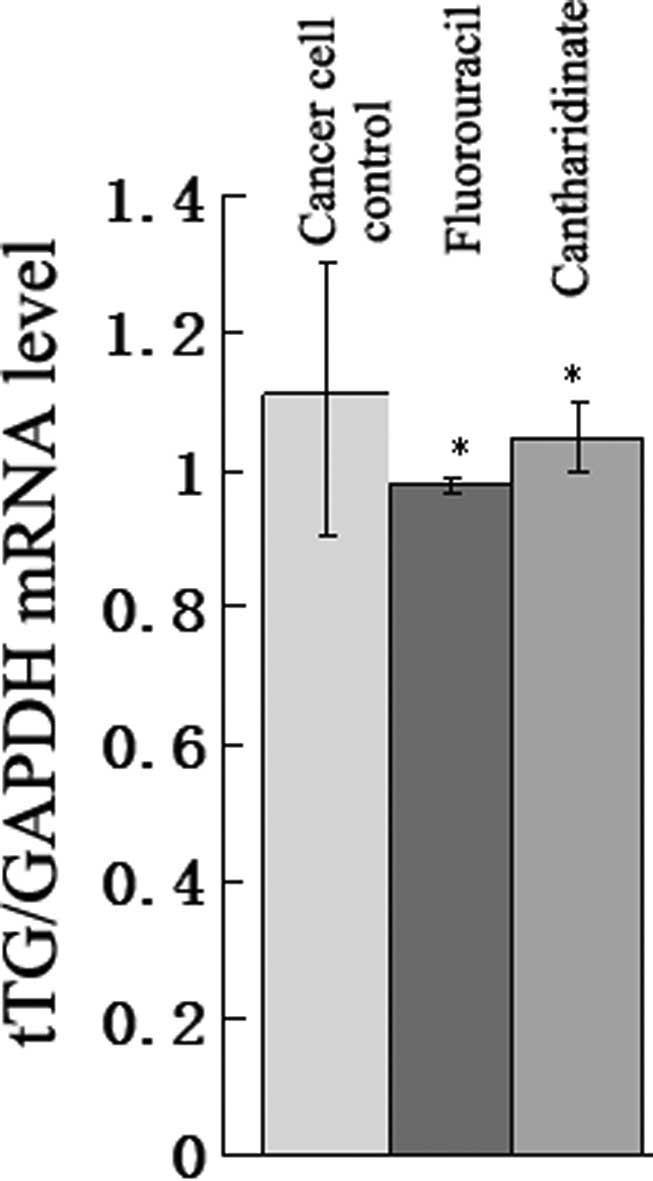
PCR analysis results
To determine whether the tTG mRNA level in UCT-116
cells altered following the application of cantharidinate, qPCR
analysis was performed. In Fig. 5,
the expression of tTG mRNA in the cantharidinate group decreased to
0.69-fold that of the untreated cancer cell control (P<0.05).
The level of tTG in the cantharidinate group was approximately the
same as that in the fluorouracil group. This result suggested that
cantharidinate may kill tumor cells by inhibiting tTG mRNA
expression.
Discussion
tTGs are a family of structurally and functionally
related proteins, which are widely distributed in all living
organisms (10). There has been an
increase in studies supporting the hypothesis that dysregulated
expression and function of tTG contributes to pathological
conditions, including cancer metastasis, tissue fibrosis, celiac
disease, neurodegenerative disorders and diseases associated with
the defective assembly of the stratum corneum of the skin (10). However, it remains unclear whether
tTG is significant in CRC.
The present study demonstrated that levels of tTG
were increased in the process of tumor occurrence and progression.
The roles of tTG upregulation in cancers may involve the following.
Agnihotri et al observed that tTG upregulation is associated
with the activation of nuclear transcription factor-κB (NF-κB),
Akt, focal adhesion kinase and hypoxia-inducible factor, thus tTG
may serve as a central mediator with a key role in the
inflammation-induced progression of mammary epithelial cancer cells
(21). Yakubov et al
reported that extracellular tTG promotes the metastasis of ovarian
cancer by noncanonical NF-κB activation (22). Furthermore, Caffarel et al
demonstrated that tTG is able to promote the progression of
cervical squamous cell carcinoma by enhancing the pro-malignant
effects of oncostatin M receptor overexpression (23). Wang et al suggested that
extracellular tTG has a crucial role in matrix-bound VEGF-mediated
angiogenesis (24).
A desirable property of an anticancer drug is to
induce the death of tumor cells with few side effects on normal
cells (12,13,15,16).
The present study demonstrated that canthardinate induced an
inhibitory effect on tTG, which is involved in human CRC. The
effects of cantharidinate are similar to that of fluorouracil.
Cantharidinate inhibits the proliferation of human CRC cells with
an IC50 of 2.5 μM and cantharidinate has marginal
cytotoxicity in normal cells (data not shown). The present study
demonstrated that cantharidinate reduced the expression of mRNA and
protein levels of tTG in human CRC cells. To the best of our
knowledge (15–20), the current study is the first to
show that the expression of tTG mRNA and protein are downregulated
by cantharidinate.
In conclusion, cantharidinate is significant in
human CRC as it inhibits the expression of tTG. Therefore,
cantharidinate may be considered to be a novel additional drug for
controlling the expression of tTG in human CRC and the growth of
human CRC.
References
|
1
|
Deng X, Cao Y, Liu Y, Li F, Sambandam K,
Rajaraman S, Perkins AS, Fields AP, Hellmich MR, Townsend CM Jr, et
al: Overexpression of Evi-1 oncoprotein represses TGF-β signaling
in colorectal cancer. Mol Carcinog. 52:255–264. 2013.PubMed/NCBI
|
|
2
|
Potter JD: Colorectal cancer: molecules
and populations. J Natl Cancer Inst. 91:916–932. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deschoolmeester V, Baay M, Specenier P,
Lardon F and Vermorken JB: A review of the most promising
biomarkers in colorectal cancer: one step closer to targeted
therapy. Oncologist. 15:699–731. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kotzev I, Mirchev M, Manevska B, Ivanova I
and Kaneva M: Risk and protective factors for development of
colorectal polyps and cancer (Bulgarian experience).
Hepatogastroenterology. 55:381–387. 2008.PubMed/NCBI
|
|
5
|
Domínguez-Ayala M, Díez-Vallejo J and
Comas-Fuentes A: Missed opportunities in early diagnosis of
symptomatic colorectal cancer. Rev Esp Enferm Dig. 104:343–349.
2012.PubMed/NCBI
|
|
6
|
Jass JR: Colorectal cancer: a multipathway
disease. Crit Rev Oncog. 12:273–287. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fearon ER: Molecular genetics of
colorectal cancer. Annu Rev Pathol. 6:479–507. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Posner MR: Paradigm shift in the treatment
of head and neck cancer: the role of neoadjuvant chemotherapy.
Oncologist. 10(Suppl 3): 11–19. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Simoglou C, Gymnopoulou E, Simoglou L,
Gymnopoulou M, Nikolaou K and Gymnopoulos D: Surgery for colorectal
cancer in the small town of Komotini. J Multidiscip Healthc.
5:273–276. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hu Y, Zhang H, Xiong X, Cao Y, Han Y and
Xi Z: Inhibitory effect of tissue transglutaminase (tTG) antisense
oligodeoxynucleotides on tTG expression in cultured bovine
trabecular meshwork cells. J Huazhong Univ Sci Technolog Med Sci.
25:729–731. 2005. View Article : Google Scholar
|
|
11
|
van Hazel GA, Pavlakis N, Goldstein D,
Olver IN, Tapner MJ, Price D, Bower GD, Briggs GM, Rossleigh MA,
Taylor DJ and George J: Treatment of fluorouracil-refractory
patients with liver metastases from colorectal cancer by using
yttrium-90 resin microspheres plus concomitant systemic irinotecan
chemotherapy. J Clin Oncol. 27:4089–4095. 2009.
|
|
12
|
Gerber DE: Targeted therapies: a new
generation of cancer treatments. Am Fam Physician. 77:311–319.
2008.PubMed/NCBI
|
|
13
|
Dehmer GJ, Douglas JS Jr, Abizaid A, et
al: SCAI/ACCF/HRS/ESC/SOLACI/APSIC statement on the use of live
case demonstrations at cardiology meetings: assessments of the past
and standards for the future. Heart Rhythm. 7:1522–1535. 2010.
View Article : Google Scholar
|
|
14
|
Liu HG and Huang HX: Overview
pharmacokinetic about traditional Chinese medicine in recent 10
years. Zhongguo Zhong Yao Za Zhi. 32:2346–2348. 2007.(In
Chinese).
|
|
15
|
Honkanen RE: Cantharidin, another natural
toxin that inhibits the activity of serine/threonine protein
phosphatases types 1 and 2A. FEBS Lett. 330:283–286. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Deng LP, Dong J, Cai H and Wang W:
Cantharidin as an antitumor agent: a retrospective review. Curr Med
Chem. 20:159–166. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Huang YP, Ni CH, Lu CC, et al:
Suppressions of migration and invasion by cantharidin in TSGH-8301
human bladder carcinoma cells through the inhibitions of matrix
metalloproteinase-2/-9 signaling. Evid Based Complement Alternat
Med. 2013:1902812013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhan YP, Huang XE, Cao J, et al: Clinical
study on safety and efficacy of Qinin® (cantharidin
sodium) injection combined with chemotherapy in treating patients
with gastric cancer. Asian Pac J Cancer Prev. 13:4773–4776.
2012.PubMed/NCBI
|
|
19
|
Kim YM, Ku MJ, Son YJ, Yun JM, Kim SH and
Lee SY: Anti-metastatic effect of cantharidin in A549 human lung
cancer cells. Arch Pharm Res. 36:479–484. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Yeh CH, Yang YY, Huang YF, Chow KC and
Chen MF: Induction of apoptosis in human Hep3B hepatoma cells by
norcantharidin through a p53 independent pathway via TRAIL/DR5
signal transduction. Chin J Integr Med. 18:676–682. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Agnihotri N, Kumar S and Mehta K: Tissue
transglutaminase as a central mediator in inflammation-induced
progression of breast cancer. Breast Cancer Res. 15:2022013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yakubov B, Chelladurai B, Schmitt J,
Emerson R, Turchi JJ and Matei D: Extracellular tissue
transglutaminase activates noncanonical NF-κB signaling and
promotes metastasis in ovarian cancer. Neoplasia. 15:609–619.
2013.PubMed/NCBI
|
|
23
|
Caffarel MM, Chattopadhyay A, Araujo AM,
Bauer J, Scarpini CG and Coleman N: Tissue transglutaminase
mediates the pro-malignant effects of oncostatin M receptor
over-expression in cervical squamous cell carcinoma. J Pathol.
231:168–179. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang Z, Perez M, Caja S, Melino G, Johnson
TS, Lindfors K and Griffin M: A novel extracellular role for tissue
transglutaminase in matrix-bound VEGF-mediated angiogenesis. Cell
Death Dis. 4:e8082013. View Article : Google Scholar : PubMed/NCBI
|