|
1
|
Pluta RM, Hansen-Schwartz J, Dreier J,
Vajkoczy P, Macdonald RL, Nishizawa S, Kasuya H, Wellman G, Keller
E, Zauner A, et al: Cerebral vasospasm following subarachnoid
hemorrhage: Time for a new world of thought. Neurol Res.
31:151–158. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen S, Feng H, Sherchan P, Klebe D, Zhao
G, Sun X, Zhang J, Tang J and Zhang JH: Controversies and evolving
new mechanisms in subarachnoid hemorrhage. Prog Neurobiol.
115:64–91. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rothoerl RD and Ringel F: Molecular
mechanisms of cerebral vasospasm following aneurysmal SAH. Neurol
Res. 29:636–642. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ciurea AV, Palade C, Voinescu D and Nica
DA: Subarachnoid hemorrhage and cerebral vasospasm-literature
review. J Med Life. 6:120–125. 2013.PubMed/NCBI
|
|
5
|
Crowley RW, Medel R, Kassell NF and Dumont
AS: New insights into the causes and therapy of cerebral vasospasm
following subarachnoid hemorrhage. Drug Discov Today. 13:254–260.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fassbender K, Hodapp B, Rossol S, Bertsch
T, Schmeck J, Schütt S, Fritzinger M, Horn P, Vajkoczy P, Kreisel
S, et al: Inflammatory cytokines in subarachnoid hemorrhage:
Association with abnormal blood flow velocities in basal cerebral
arteries. J Neurol Neurosurg Psychiatry. 70:534–537. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Osuka K, Watanabe Y, Yamauchi K, Nakazawa
A, Usuda N, Tokuda M and Yoshida J: Activation of the JAK-STAT
signaling pathway in the rat basilar artery after subarachnoid
hemorrhage. Brain Res. 1072:1–7. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dumont AS, Dumont RJ, Chow MM, Lin CL,
Calisaneller T, Ley KF, Kassell NF and Lee KS: Cerebral vasospasm
after subarachnoid hemorrhage: Putative role of inflammation.
Neurosurgery. 53:123–135. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cheng MF, Song JN, Li DD, Zhao YL, An JY,
Sun P and Luo XH: The role of rosiglitazone in the proliferation of
vascular smooth muscle cells after experimental subarachnoid
hemorrhage. Acta Neurochir (Wien). 156:2103–2109. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kolias AG, Sen J and Belli A: Pathogenesis
of cerebral vasospasm following aneurysmal subarachnoid hemorrhage:
Putative mechanisms and novel approaches. J Neurosci Res. 87:1–11.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ohkuma H, Tsurutani H and Suzuki S:
Changes of beta-actin mRNA expression in canine vasospastic basilar
artery after experimental subarachnoid hemorrhage. Neurosci Lett.
311:9–12. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Davis-Dusenbery BN, Wu C and Hata A:
Micromanaging vascular smooth muscle cell differentiation and
phenotypic modulation. Arterioscler Thromb Vasc Biol. 31:2370–2377.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Rensen SS, Doevendans PA and van Eys GJ:
Regulation and characteristics of vascular smooth muscle cell
phenotypic diversity. Neth Heart J. 15:100–108. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Beamish JA, He P, Kottke-Marchant K and
Marchant RE: Molecular regulation of contractile smooth muscle cell
phenotype: Implications for vascular tissue engineering. Tissue Eng
Part B Rev. 16:467–491. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shimamura N and Ohkuma H: Phenotypic
transformation of smooth muscle in vasospasm after aneurysmal
subarachnoid hemorrhage. Transl Stroke Res. 5:357–364. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang JH, Badaut J, Tang J, Obenaus A,
Hartman R and Pearce WJ: The vascular neural network-a new paradigm
in stroke pathophysiology. Nat Rev Neurol. 8:711–716. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang J, Wang L, Fu W, Wang C, Guo D,
Jiang J and Wang Y: Smooth muscle cell phenotypic diversity between
dissected and unaffected thoracic aortic media. J Cardiovasc Surg
(Torino). 54:511–521. 2013.PubMed/NCBI
|
|
18
|
Lim HJ, Lee S, Park JH, Lee KS, Choi HE,
Chung KS, Lee HH and Park HY: PPAR delta agonist L-165041 inhibits
rat vascular smooth muscle cell proliferation and migration via
inhibition of cell cycle. Atherosclerosis. 202:446–454. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Moreno S, Farioli-Vecchioli S and Cerù MP:
Immunolocalization of peroxisome proliferator-activated receptors
and retinoid X receptors in the adult rat CNS. Neuroscience.
123:131–145. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ehrenborg E and Krook A: Regulation of
skeletal muscle physiology and metabolism by peroxisome
proliferator-activated receptor delta. Pharmacol Rev. 61:373–393.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim HJ, Ham SA, Kim SU, Hwang JY, Kim JH,
Chang KC, Yabe-Nishimura C, Kim JH and Seo HG: Transforming growth
factor-beta1 is a molecular target for the peroxisome
proliferator-activated receptor delta. Circ Res. 102:193–200. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Blenis J: Signal transduction via the MAP
kinases: Proceed at your own RSK. Proc Natl Acad Sci USA.
90:5889–5892. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Seger R and Krebs EG: The MAPK signaling
cascade. FASEB J. 9:726–735. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Frödin M and Gammeltoft S: Role and
regulation of 90 kDa ribosomal S6 kinase (RSK) in signal
transduction. Mol Cell Endocrinol. 151:65–77. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kawai-Kowase K and Owens GK: Multiple
repressor pathways contribute to phenotypic switching of vascular
smooth muscle cells. Am J Physiol Cell Physiol. 292:C59–C69. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kang YH, Yang IJ and Shin HM: Herbal
formula HMC05 prevents human aortic smooth muscle cell migration
and proliferation by inhibiting the ERK1/2 MAPK signaling cascade.
J Nat Med. 66:177–184. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
MacArthur Clark JA and Sun D: Guidelines
for the ethical review of laboratory animal welfare People's
Republic of China national standard GB/T 35892-2018 (issued 6
February 2018 effective from 1 September 2018). Animal Model Exp
Med. 3:103–113. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Muroi C, Fujioka M, Okuchi K, Fandino J,
Keller E, Sakamoto Y, Mishima K, Iwasaki K and Fujiwara M: Filament
perforation model for mouse subarachnoid hemorrhage:
Surgical-technical considerations. Br J Neurosurg. 28:722–732.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Sugawara T, Ayer R, Jadhav V and Zhang JH:
A new grading system evaluating bleeding scale in filament
perforation subarachnoid hemorrhage rat model. J Neurosci Methods.
167:327–334. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Suzuki H, Hasegawa Y, Chen W, Kanamaru K
and Zhang JH: Recombinant osteopontin in cerebral vasospasm after
subarachnoid hemorrhage. Ann Neurol. 68:650–660. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen Y, Zhang Y, Tang J, Liu F, Hu Q, Luo
C, Tang J, Feng H and Zhang JH: Norrin protected blood-brain
barrier via frizzled-4/β-catenin pathway after subarachnoid
hemorrhage in rats. Stroke. 46:529–536. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Teng Z, Jiang L, Hu Q, He Y and Guo Z, Wu
Y, Huang Z, Cao F, Cheng C, Sun X and Guo Z: Peroxisome
proliferator-activated receptor β/δ alleviates early brain injury
after subarachnoid hemorrhage in rats. Stroke. 47:196–205. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ostrowski RP, Colohan AR and Zhang JH:
Mechanisms of hyperbaric oxygen-induced neuroprotection in a rat
model of subarachnoid hemorrhage. J Cereb Blood Flow Metab.
25:554–571. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Choudhri TF, Hoh BL, Solomon RA, Connolly
ES Jr and Pinsky DJ: Use of a spectrophotometric hemoglobin assay
to objectively quantify intracerebral hemorrhage in mice. Stroke.
28:2296–2302. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Carpenter RC, Miao L, Miyagi Y, Bengten E
and Zhang JH: Altered expression of P(2) receptor mRNAs in the
basilar artery in a rat double hemorrhage model. Stroke.
32:516–522. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Chen D, Tang J, Khatibi NH, Zhu M, Li Y,
Wang C, Jiang R, Tu L and Wang S: Treatment with Z-ligustilide, a
component of Angelica sinensis, reduces brain injury after a
subarachnoid hemorrhage in rats. J Pharmacol Exp Ther. 337:663–672.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Fan R, Enkhjargal B, Camara R, Yan F, Gong
L, Shengtao Yao, Tang J, Chen Y and Zhang JH: Critical role of
EphA4 in early brain injury after subarachnoid hemorrhage in rat.
Exp Neurol. 296:41–48. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
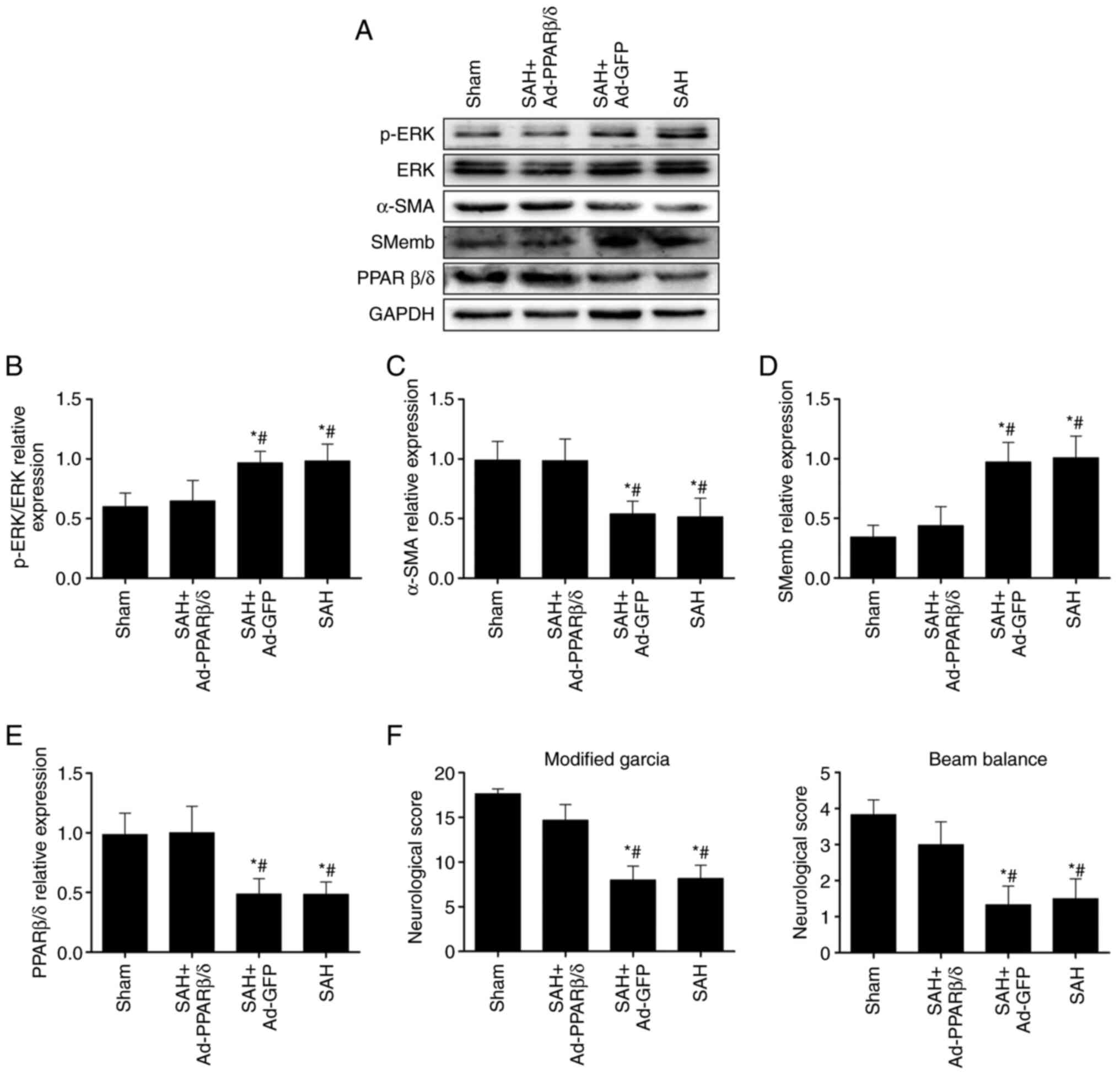
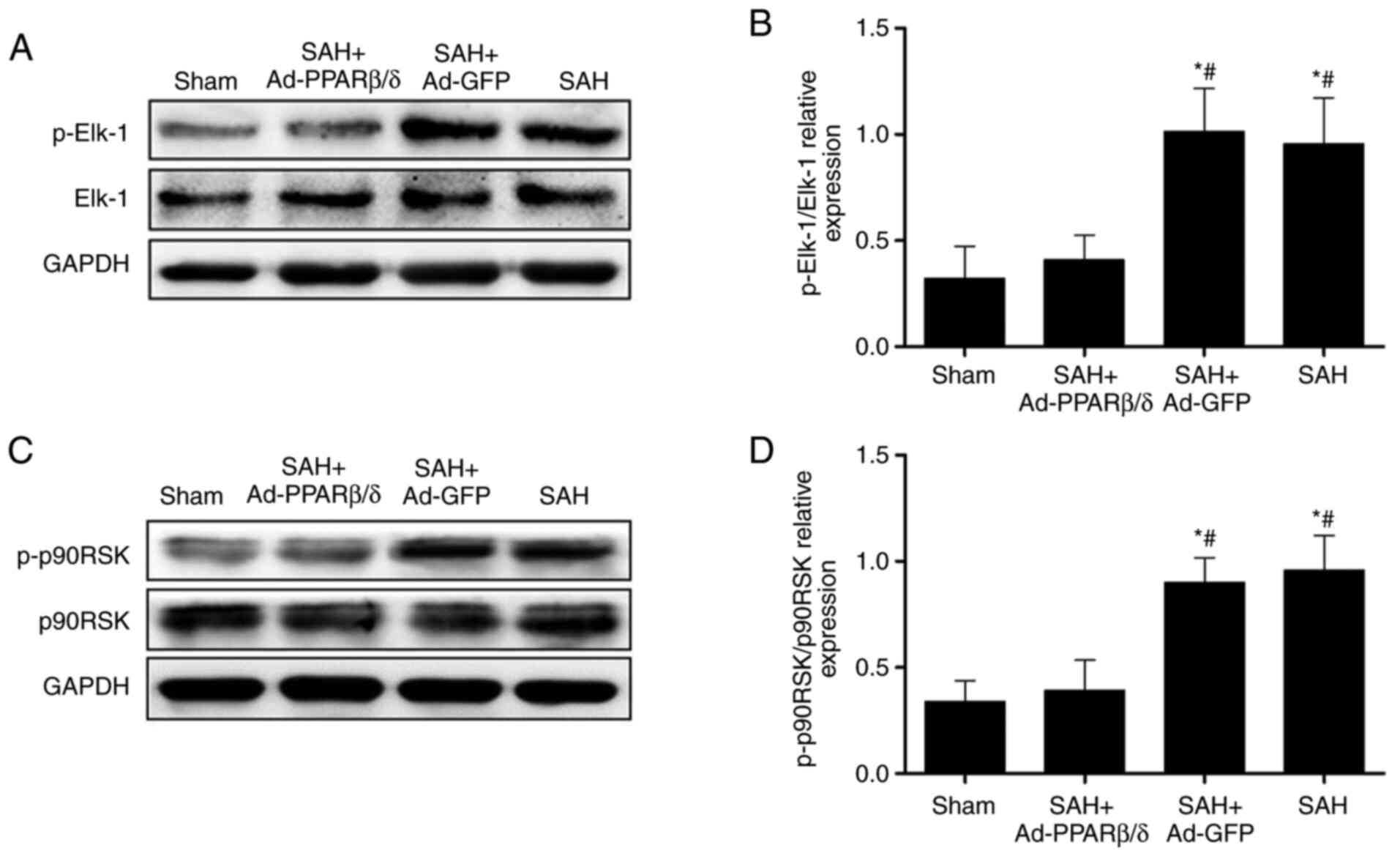
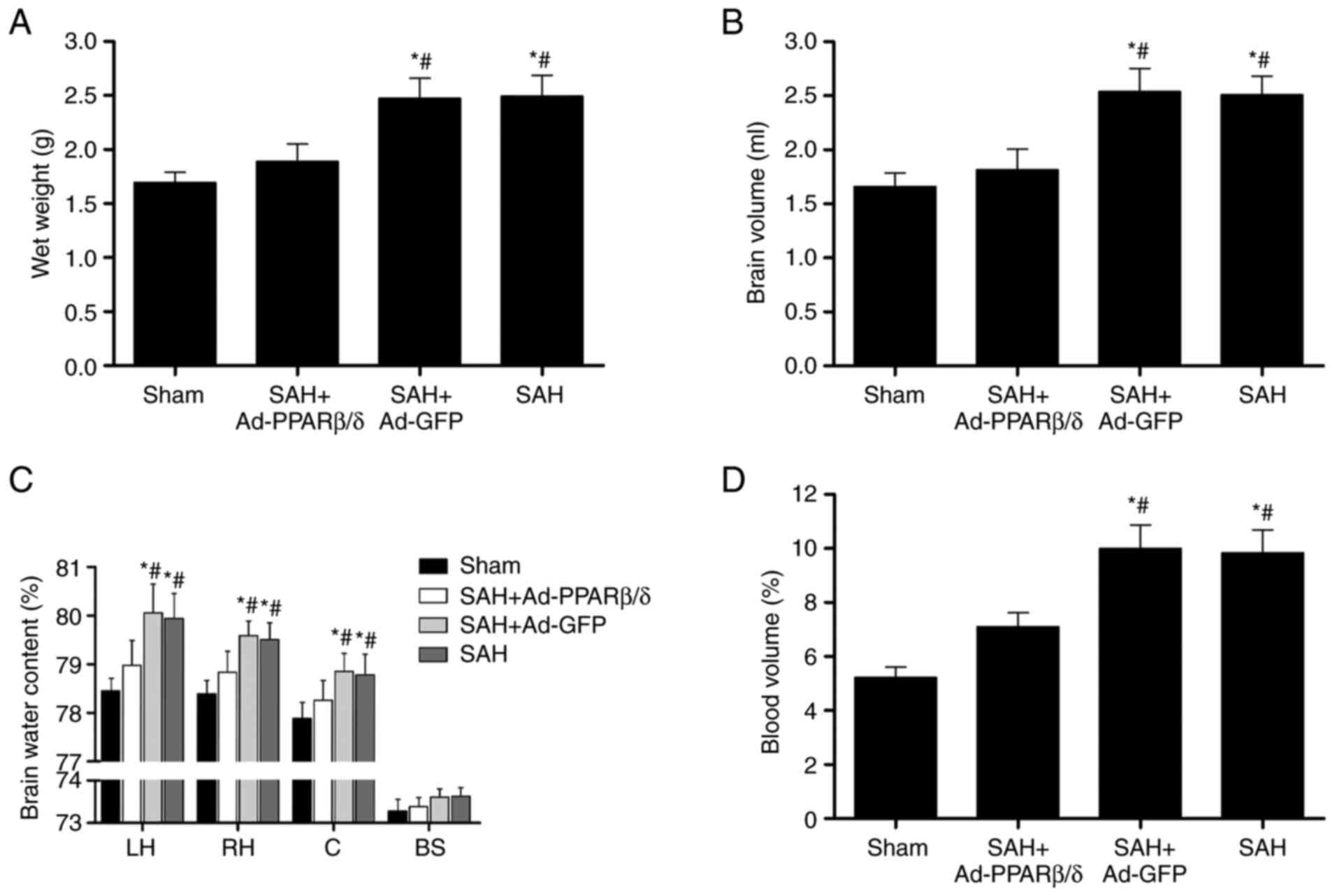
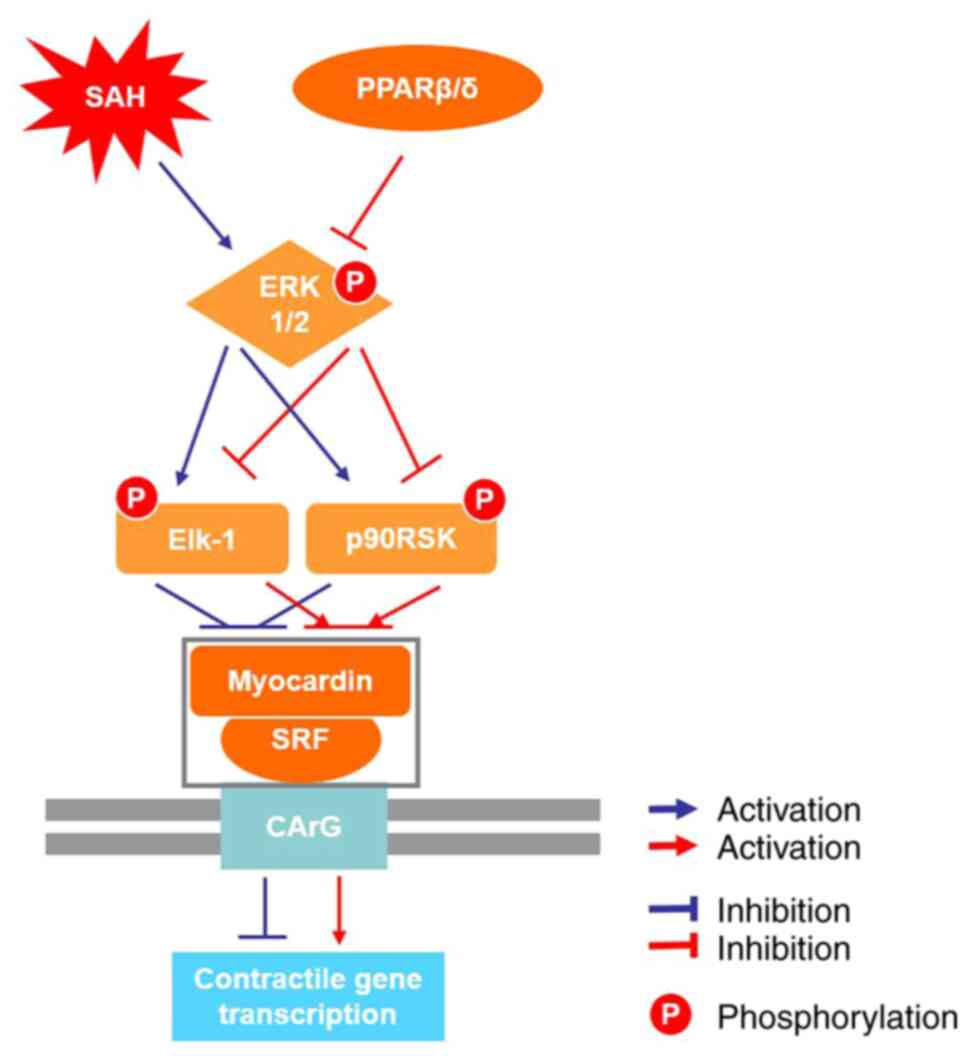
Zhang H, Jiang L, Guo Z, Zhong J, Wu J, He
J, Liu H, He Z, Wu H, Cheng C and Sun X: PPARβ/δ, a novel regulator
for vascular smooth muscle cells phenotypic modulation and vascular
remodeling after subarachnoid hemorrhage in rats. Sci Rep.
7:452342017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Maddahi A, Povlsen GK and Edvinsson L:
Regulation of enhanced cerebrovascular expression of
proinflammatory mediators in experimental subarachnoid hemorrhage
via the mitogen-activated protein kinase kinase/extracellular
signal-regulated kinase pathway. J Neuroinflammation. 9:2742012.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Danura H, Schatlo B, Marbacher S, Kerkeni
H, Diepers M, Remonda L, Fathi AR and Fandino J: Acute angiographic
vasospasm and the incidence of delayed cerebral vasospasm:
Preliminary results. Acta Neurochir Suppl. 120:187–190.
2015.PubMed/NCBI
|
|
41
|
Shimamura N, Munakata A and Ohkuma H:
Current management of subarachnoid hemorrhage in advanced age. Acta
Neurochir Suppl. 110:151–155. 2011.PubMed/NCBI
|
|
42
|
Chou SH, Smith EE, Badjatia N, Nogueira
RG, Sims JR II, Ogilvy CS, Rordorf GA and Ayata C: A randomized,
double-blind, placebo-controlled pilot study of simvastatin in
aneurysmal subarachnoid hemorrhage. Stroke. 39:2891–2893. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Edvinsson LI and Povlsen GK: Vascular
plasticity in cerebrovascular disorders. J Cereb Blood Flow Metab.
31:1554–1571. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ohkuma H, Suzuki S and Ogane K: Phenotypic
modulation of smooth muscle cells and vascular remodeling in
intraparenchymal small cerebral arteries after canine experimental
subarachnoid hemorrhage. Neurosci Lett. 344:193–196. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wu J, Zhang Y, Yang P, Enkhjargal B,
Manaenko A, Tang J, Pearce WJ, Hartman R, Obenaus A, Chen G and
Zhang JH: Recombinant osteopontin stabilizes smooth muscle cell
phenotype via integrin receptor/integrin-linked kinase/rac-1
pathway after subarachnoid hemorrhage in rats. Stroke.
47:1319–1327. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Smyth LCD, Rustenhoven J, Scotter EL,
Schweder P, Faull RL, Park TI and Dragunow M: Markers for human
brain pericytes and smooth muscle cells. J Chem Neuroanat.
92:48–60. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Piqueras L, Reynolds AR, Hodivala-Dilke
KM, Alfranca A, Redondo JM, Hatae T, Tanabe T, Warner TD and
Bishop-Bailey D: Activation of PPARbeta/delta induces endothelial
cell proliferation and angiogenesis. Arterioscler Thromb Vasc Biol.
27:63–69. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Lee CH, Chawla A, Urbiztondo N, Liao D,
Boisvert WA, Evans RM and Curtiss LK: Transcriptional repression of
atherogenic inflammation: Modulation by PPARdelta. Science.
302:453–457. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chang CZ, Wu SC and Kwan AL: Glycyrrhizin
attenuates proinflammatory cytokines through a peroxisome
proliferator-activated receptor-γ-dependent mechanism and
experimental vasospasm in a rat model. J Vasc Res. 52:12–21. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Hamaya R, Ogawa M, Suzuki J, Kobayashi N,
Hirata Y, Nagai R, Komuro I and Isobe M: A selective peroxisome
proliferator-activated receptor-β/δ agonist attenuates neointimal
hyperplasia after wire-mediated arterial injury. Expert Opin.
Investig. Drugs. 22:1095–1106. 2013.PubMed/NCBI
|
|
51
|
Pipes GC, Creemers EE and Olson EN: The
myocardin family of transcriptional coactivators: Versatile
regulators of cell growth, migration, and myogenesis. Genes Dev.
20:1545–1556. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Parmacek MS: Myocardin-related
transcription factors: Critical coactivators regulating
cardiovascular development and adaptation. Circ Res. 100:633–644.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Takata Y, Liu J, Yin F, Collins AR, Lyon
CJ, Lee CH, Atkins AR, Downes M, Barish GD, Evans RM, et al:
PPARdelta-mediated antiinflammatory mechanisms inhibit angiotensin
II-accelerated atherosclerosis. Proc Natl Acad Sci USA.
105:4277–4282. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Salvadó L, Barroso E, Gómez-Foix AM,
Palomer X, Michalik L, Wahli W and Vázquez-Carrera M: PPARβ/δ
prevents endoplasmic reticulum stress-associated inflammation and
insulin resistance in skeletal muscle cells through an
AMPK-dependent mechanism. Diabetologia. 57:2126–2135. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hsieh HL, Wu CY and Yang CM: Bradykinin
induces matrix metalloproteinase-9 expression and cell migration
through a PKC-delta-dependent ERK/Elk-1 pathway in astrocytes.
Glia. 56:619–632. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Wang Z, Wang DZ, Hockemeyer D, McAnally J,
Nordheim A and Olson EN: Myocardin and ternary complex factors
compete for SRF to control smooth muscle gene expression. Nature.
428:185–189. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Toral M, Romero M, Pérez-Vizcaíno F,
Duarte J and Jiménez R: Antihypertensive effects of peroxisome
proliferator-activated receptor-β/δ activation. Am J Physiol Heart
Circ Physiol. 312:H189–H200. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Barroso E, Eyre E, Palomer X and
Vázquez-Carrera M: The peroxisome proliferator-activated receptor
β/δ (PPARβ/δ) agonist GW501516 prevents TNF-α-induced NF-κB
activation in human HaCaT cells by reducing p65 acetylation through
AMPK and SIRT1. Biochem Pharmacol. 81:534–543. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Zarzuelo MJ, Jiménez R, Galindo P, Sánchez
M, Nieto A, Romero M, Quintela AM, López-Sepúlveda R, Gómez-Guzmán
M, Bailón E, et al: Antihypertensive effects of peroxisome
proliferator-activated receptor-β activation in spontaneously
hypertensive rats. Hypertension. 58:733–743. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Law RE, Goetze S, Xi XP, Jackson S, Kawano
Y, Demer L, Fishbein MC, Meehan WP and Hsueh WA: Expression and
function of PPARgamma in rat and human vascular smooth muscle
cells. Circulation. 101:1311–1318. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Dorhout Mees SM, Rinkel GJE, Feigin VL,
Algra A, van den Bergh WM, Vermeulen M and van Gijn J: Calcium
antagonists for aneurysmal subarachnoid hemorrhage. Stroke.
39:514–515. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Pandey AS, Elias AE, Chaudhary N, Thompson
BG and Gemmete JJ: Endovascular treatment of cerebral vasospasm:
Vasodilators and angioplasty. Neuroimaging Clin N Am. 23:593–604.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Hansen-Schwartz J: Cerebral vasospasm: A
consideration of the various cellular mechanisms involved in the
pathophysiology. Neurocrit Care. 1:235–246. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Edvinsson L, Larsen SS, Maddahi A and
Nielsen J: Plasticity of cerebrovascular smooth muscle cells after
subarachnoid hemorrhage. Transl Stroke Res. 5:365–376. 2014.
View Article : Google Scholar : PubMed/NCBI
|