Introduction
Although endobronchial metastasis is rare, colon,
kidney and breast cancer are three of the malignancies that can
develop endobronchial metastasis (1,2). A
range of conditions, including non-malignant tumors, primary lung
carcinoma and endobronchial metastasis of carcinoma from
extra-pulmonary organs, may form part of the differential diagnosis
of endobronchial lesions in the clinic (3–8).
Superficial-type endobronchial metastasis arising from
extrathoracic tumors is extremely rare and thus, the incidence
remains unknown. To prevent bleeding and airway obstruction caused
by endobronchial metastasis, irradiation and photodynamic therapy
have been proposed, however, a standard therapy has not yet been
established due to its rarity and the outcome of this type of
endobronchial metastasis from colorectal cancer has not been
previously reported. The present study reports the case of a
patient with superficial-type endobronchial metastases in the
bronchi, which were unexpectedly found by bronchoscopic
examination. Written informed consent was obtained from the
patient.
Case report
A 76-year-old male was referred to the Mito Medical
Center (Mito, Japan) due to a two-month history of vomiting and a
loss of body weight. Eight years previously, the patient had
undergone a surgical resection for colon cancer. Upon admission,
the laboratory examination revealed a hemoglobin level of 12.4 g/dl
(normal range, 13–16 g/dl), a hematocrit level of 36.2% (normal
range, 40–52%) and a C-reactive protein count of 1.11 g/dl (normal
range, ≤0.5 m/dl). The serum level of carcinoembryonic antigen was
elevated to 35.1 ng/ml (normal range, ≤5.0 ng/ml). A physical
examination revealed right subclavian lymph node swelling, which
was pathologically proven to be lymph node metastasis from colon
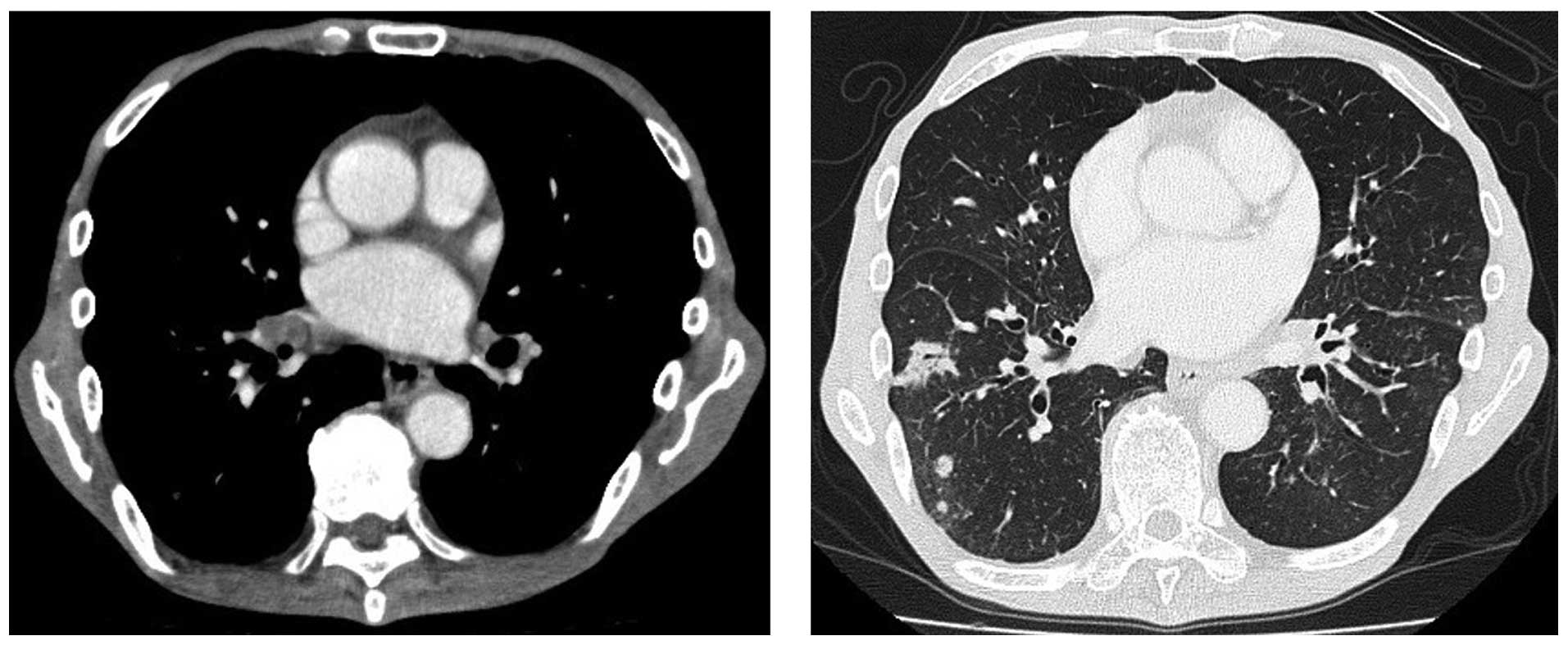
cancer. Computed tomography (CT) of the abdomen revealed multiple
metastatic tumors in the liver. X-ray and CT of the chest revealed
small masses in the lungs, with bilateral hilar lymph node swelling
(Fig. 1). As these pulmonary
lesions were observed, bronchoscopy was performed to obtain
pathological specimens and to confirm that these lesions were
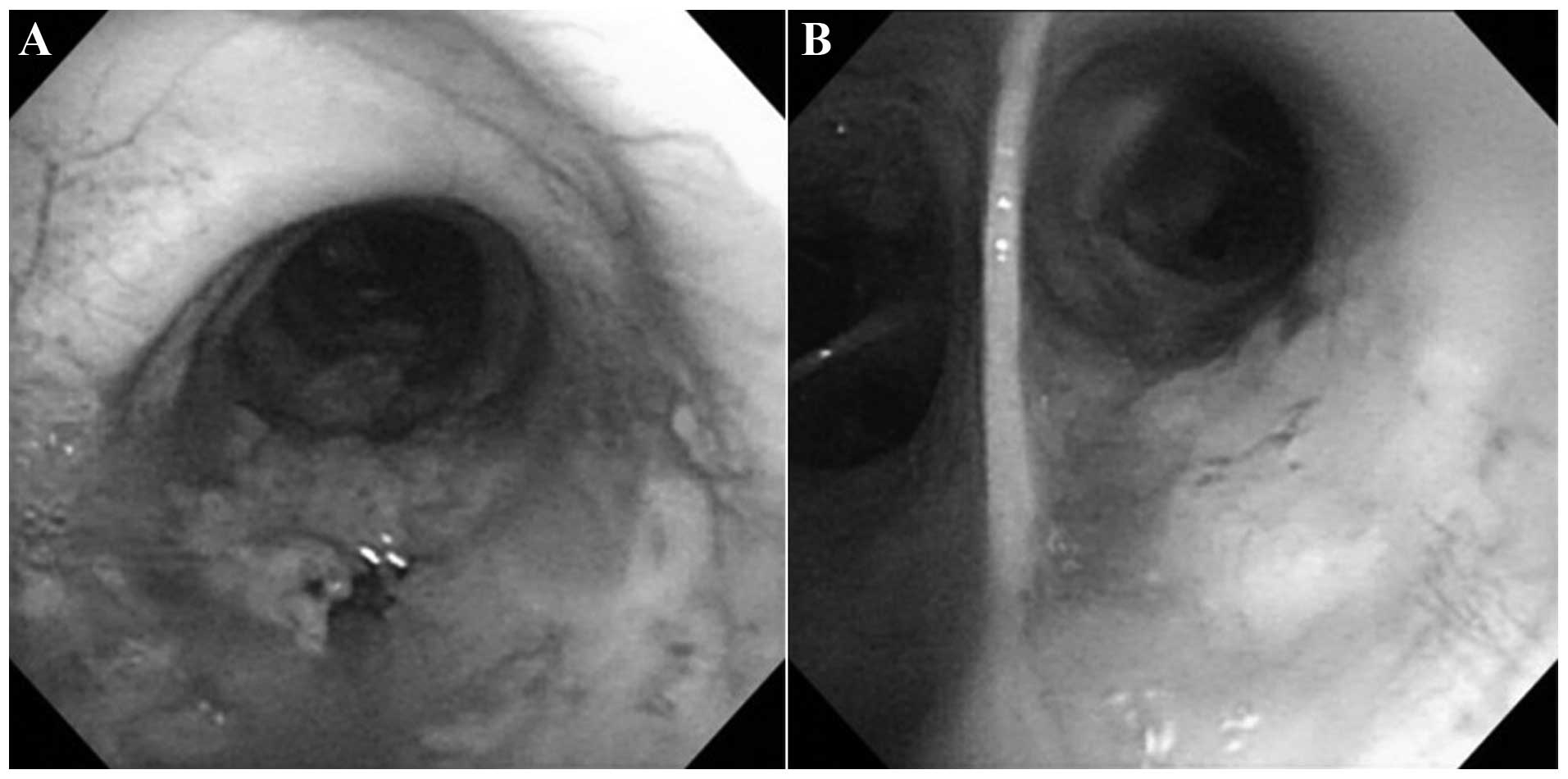
metastatic tumors from colon cancer. Bronchoscopy revealed
unexpected superficial endobronchial tumors in the two bronchi
(Fig. 2), which were white and
marginally elevated flat lesions with irregular margins. No
necrotic tissue was identified, however, the development of small
blood vessels surrounding the lesions was observed.
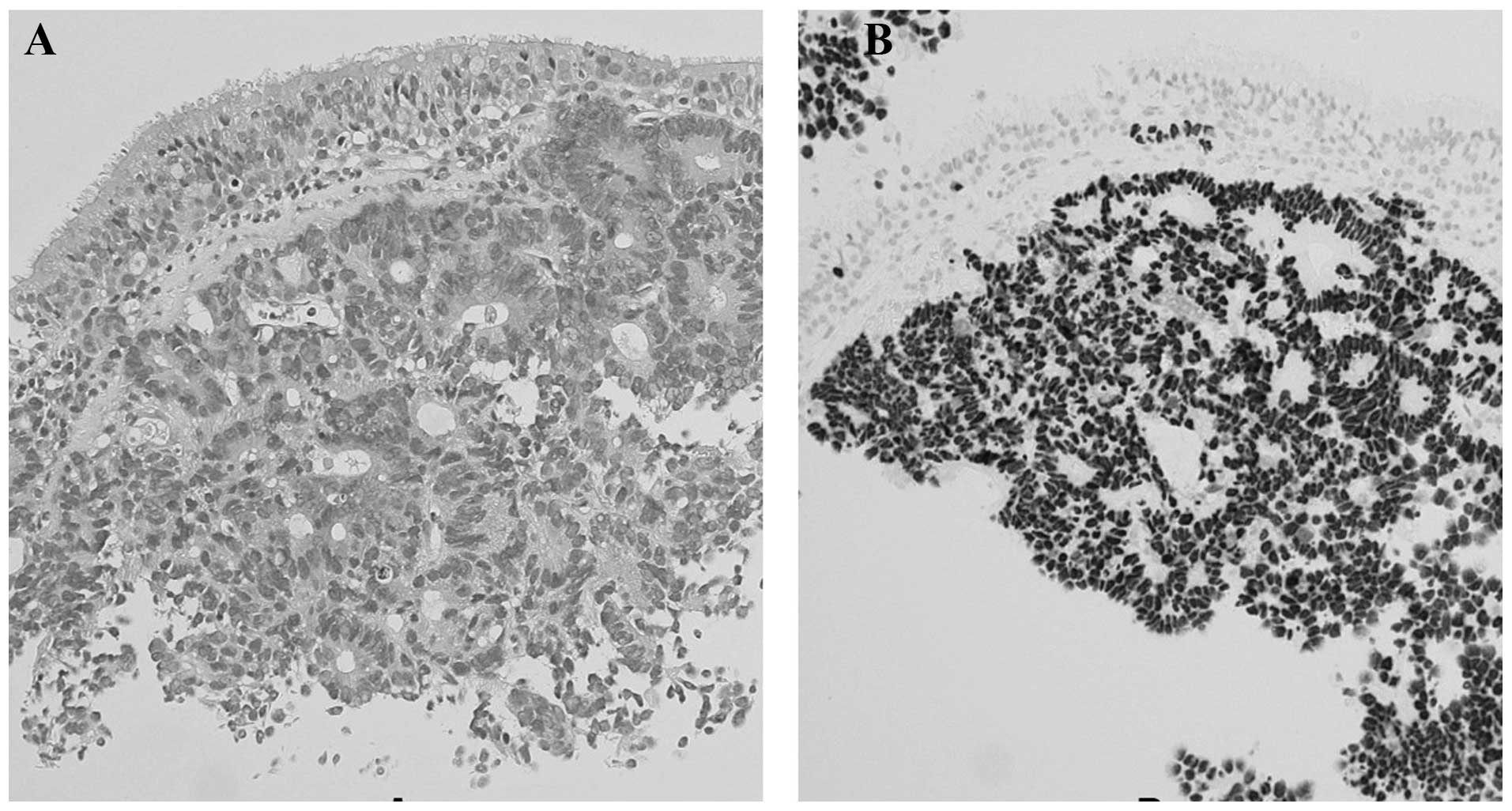
Pathological examination of the tumors obtained from
the left main bronchus revealed well-differentiated adenocarcinoma
with a cribriform pattern, which was consistent with the findings
of a resected adrenocortical carcinoma (Fig. 3A). Positive immunochemical staining
with caudal-type homeobox transcription factor 2 was confirmed
(Fig. 3B). The patient was treated
with two courses of TS-1 (80 mg/day for two weeks), but developed
multiple brain metastases. One month subsequent to the initiation
of the chemotherapy, the patient succumbed to colon cancer. An
autopsy was not permitted.
Discussion
The lung is one of the most common metastatic sites
of extra-thoracic tumors, the majority of which are found in the
pulmonary parenchyma. Although extremely rare, patients with
endobronchial metastasis do occur. The most common symptoms of
endobronchial metastasis are coughing and hemoptysis, followed by
dyspnea and wheezing. If one or more of these symptoms are present
in patients with extra-thoracic tumors, it is possible that such
symptoms may be being caused by endobronchial metastasis. However,
endobronchial metastasis can also be found in asymptomatic
patients. Three of the most common tumors that develop
endobronchial metastases are breast, colon and renal tumors
(1,2,5–7).
The differential diagnosis of an endobronchial mass
lesion includes non-malignant tumors, endobronchial metastasis of
carcinoma from extrapulmonary organs and primary lung carcinoma
(3–8). Endobronchial lesions can be examined
by fiberoptic bronchoscopy, since the majority of lesions are
within the view and grasp of the bronchoscopic field. Non-malignant
endobronchial tumors usually possess a smooth surface with a
uniform color (9). Endoscopic
manifestations of an endobronchial metastatic lesion are
considerably variable, but polypoid tumors with necrotic material
and nodular tumors are commonly observed. Among the primary lung
cancer types, squamous cell carcinoma is the most prevalent
histological type that is centrally located and exhibits
endobronchial extension (4).
Polypoid lesions with a necrotic material-covered rough surface are
the most frequently occurring tumors in squamous cell carcinoma
(10,11). Certain patients with squamous cell
or mucoepidermoid lung cancer exhibit superficial or nodular
endobronchial tumors (12,13). In addition, although extremely rare,
multifocal primary squamous cell carcinomas can develop in each of
the bronchi, as observed in the present case (12). The mass-like endobronchial plug
(14), which possibly represents an
endobronchial infectious process, including mucus plugs distal to a
centrally obstructing lesion due to fungus or tuberculosis, also
simulates an endobronchial mass on endobronchial examination. In
general, it is accepted that without pathological confirmation, the
bronchoscopic findings of endobronchial metastasis are not clearly
distinct from those of primary lung carcinoma and non-malignant
tumors (15,16). In certain cases, the benefits of
bronchoscopic examination may be diminished due to the presence of
necrotic material interfering with the opportunity to obtain a
proper diagnostic specimen (17–19).
Therefore, in order to form a proper diagnosis, it is essential to
combine the pathological diagnosis with immunohistochemical
examination using appropriate specimens obtained by bronchoscopic
biopsy.
In primary lung cancer, the endobronchial types have
been defined as superficial, nodular and submucosal (20). By contrast, however, there has been
no such classification for endobronchial metastatic lesions. If the
primary lung cancer classification was to be applied to the present
case, the tumor may be classed as of superficial or submucosal
type. The endobronchial lesions in the present patient may be the
early stage of endobronchial metastasis. These lesions may become
enlarged to form nodular lesions, which are usually classified as
nodular-type lung cancer.
Endobronchial lesions may form either by invasion
from the surrounding tissues, including the lung parenchyma or
hilar and/or mediastinal lymph nodes, or by direct seeding within
the bronchial wall (1,2). The endobronchial metastasis type in
the present patient may be due to direct metastasis to the bronchus
or endobronchial invasion of mediastinal or hilar lymphadenopathy.
Although endobronchial metastasis is an extremely rare tumor
presentation, the possibility that colon cancer can develop
superficial endobronchial tumors in each of the bronchi should be
considered.
References
|
1
|
Akoglu S, Uçan ES, Celik G, et al:
Endobronchial metastases from extrathoracic malignancies. Clin Exp
Metastasis. 22:587–591. 2005.
|
|
2
|
Kiryu T, Hoshi H, Matsui E, et al:
Endotracheal/endobronchial metastases: clinicopathologic study with
special reference to developmental modes. Chest. 119:768–775.
2001.
|
|
3
|
Unger M: Endobronchial therapy of
neoplasms. Chest Surg Clin N Am. 13:129–147. 2003.
|
|
4
|
Koss MN, Hochholzer L and Frommelt RA:
Carcinosarcomas of the lung: a clinicopathologic study of 66
patients. Am J Surg Pathol. 23:1514–1526. 1999.
|
|
5
|
Katsimbri PP, Bamias AT, Froudarakis ME,
et al: Endobronchial metastases secondary to solid tumors: report
cases and review of the literature. Lung Cancer. 28:163–170.
2000.
|
|
6
|
Braman SS and Whitcomb ME: Endobronchial
metastasis. Arch Intern Med. 135:543–547. 1975.
|
|
7
|
Seo JB, Im JG, Goo JM, et al: Atypical
pulmonary metastases: spectrum of radiologic findings.
Radiographics. 21:403–417. 2001.
|
|
8
|
Shah H, Garbe L, Nussbaum E, et al: Benign
tumors of the tracheobronchial tree. Endoscopic characteristics and
role of laser resection. Chest. 107:1744–1751. 1995.
|
|
9
|
Oshikawa K, Ohno S, Ishii Y and Kitamura
S: Evaluation of bronchoscopic findings in patients with metastatic
pulmonary tumor. Intern Med. 37:349–353. 1998.
|
|
10
|
Lam B, Wong MP, Fung SL, et al: The
clinical value of autofluorescence bronchoscopy for the diagnosis
of lung cancer. Eur Respir J. 28:915–919. 2006.
|
|
11
|
Shulman L and Ost D: Advances in
bronchoscopic diagnosis of lung cancer. Curr Opin Pulm Med.
13:271–277. 2007.
|
|
12
|
Yasufuku K: Early diagnosis of lung
cancer. Clin Chest Med. 31:39–47. 2010.
|
|
13
|
Wildbrett P, Horras N, Lode H, Warzok R,
Heidecke CD and Barthlen W: Mucoepidermoid carcinoma of the lung in
a 6-year-old boy. Afr J Paediatr Surg. 9:159–162. 2012.
|
|
14
|
Itoi S, Ohara G, Kagohashi K, Kawaguchi M,
Kurishima K and Satoh H: Tracheobronchial mucoid pseudotumor. Cent
Eur J Med. 7:385–387. 2012.
|
|
15
|
Murakami S, Watanabe Y, Saitoh H, et al:
Treatment of multiple primary squamous cell carcinomas of the lung.
Ann Thorac Surg. 60:964–969. 1995.
|
|
16
|
Saida Y, Kujiraoka Y, Akaogi E, et al:
Early squamous cell carcinoma of the lung: CT and pathologic
correlation. Radiology. 201:61–65. 1996.
|
|
17
|
Lau KY: Endobronchial actinomycosis
mimicking pulmonary neoplasm. Thorax. 47:664–665. 1992.
|
|
18
|
Kim JS, Rhee Y, Kang SM, et al: A case of
endobronchial aspergilloma. Yonsei Med J. 41:422–425. 2000.
|
|
19
|
Van den Brande P, Lambrechts M, Tack J and
Demedts M: Endobronchial tuberculosis mimicking lung cancer in
elderly patients. Respir Med. 85:107–109. 1991.
|
|
20
|
The Japan Lung Cancer Society. General
Rule for Clinical and Pathological Record of Lung Cancer. 7th
edition. Kanehara Shuppan; Tokyo, Japan: 2010
|