Introduction
Hepatitis B virus (HBV) and hepatitis C virus (HCV)
infections are major risk factors for the development of human
hepatocellular carcinoma (HCC) (1–3). The
incidence of HCC in China is ~100/100,000 population, and a
principal component of the attributable risk is chronic HBV
infection (4), with >50% of the
global HCC burden attributed to HBV (5). In China, ~10% of patients with HCC
suffer from HCV infection, and certain patients have HBV and HCV
co-infections (6). In the USA, Europe
and Japan, >50% of current cases of HCC are attributable to HCV
infection, and the majority of these patients have cirrhosis
(7–9).
The time from initial diagnosis of chronic hepatitis to the
development of HCC may span several decades; once cirrhosis is
established, HCC develops at a yearly rate of 1–4% (10).
In China, the majority of patients with HCC present
with advanced-stage disease, and HCC has become the second leading
cause of mortality (11). Early
diagnosis relies on non-invasive biomarkers, imaging and clinical
parameters, with markers such as α-fetoprotein (AFP), the
proportion of the fucosylated isoform of AFP to total AFP, AFP-L3
and des-gamma-carboxy-prothrombin (DCP) being Food and Drug
Administration-approved for use in the surveillance of high-risk
populations (12,13). However, the clinical value of these
biomarkers is a subject of debate (14). In Japan, three biomarkers are combined
for surveillance (15,16), and this combined testing has a high
level of sensitivity and specificity (17,18). In
China, AFP is the only serum biomarker routinely used for HCC
diagnosis (19). Up to 50% of
patients with HCC have a serum AFP level of <20 ng/ml (20), and therefore are not correctly
diagnosed when AFP is the sole biomarker used to screen for HCC
(21).
In the current study, the efficacy of the
cancer-testis antigen (CTA) sperm-associated antigen 9 (SPAG9),
alone and combined with AFP, was evaluated for use in the diagnosis
of HCC caused by HBV or HCV infections.
CTAs include the melanoma antigen family, the
synovial sarcoma X family, cancer/testis antigen 2, G antigen 1,
cancer/testis associated protein CTp11 and cancer/testis antigen
1B. The expression of these antigens is normally restricted to the
testis, but these antigens are also expressed in tumor tissues
(22–24). Several studies have revealed that CTAs
are highly expressed in the tumor tissue of patients with HCC
(25–27). SPAG9 belongs to the
c-Jun-NH2 terminal kinase-interacting protein family
(28). Proteins from this family
function in cell growth, proliferation, apoptosis and tumor
development (29,30), and are expressed in renal cell
carcinoma, and ovarian, cervical, breast, thyroid and colorectal
cancer tissues, SPAG9 provokes a strong humoral immune response,
and its autoantibody can be detected in the peripheral blood of
patients with the aforementioned types of cancer (21–35). The
current study hypothesized that anti-SPAG9 antibody may be detected
in the peripheral blood of patients with HCC, and that, in
combination with serum AFP levels, it may provide a reliable
diagnostic test for HCC, particularly for AFP-negative
patients.
Materials and methods
Patients
A total of 31 cases of HCC caused by HBV or HCV
infections, 41 cases of hepatitis or cirrhosis caused by HBV or HCV
without HCC, and 37 normal healthy blood donors were enrolled at
Hunan Provincial Second People's Hospital (Changsha, China) from
March 2013 to May 2014. HCC was diagnosed as previously reported
(18). The inclusion criteria were no
prior anti-cancer treatment (therapeutic agents, radiotherapy or
chemotherapy) and positivity for HBV or HCV infection. The
exclusion criteria were as follows: Active liver disease
(non-cancerous hepatitis or cirrhosis), pregnancy, reproductive
system embryonic tumors or metastatic liver cancer. The cases with
hepatitis or cirrhosis without HCC included eight patients with
cirrhosis. Patient characteristics are summarized in Tables I and II. Peripheral blood samples were collected
from patients and controls. Serum was separated by centrifuging
blood at 1,000 × g for 10 min at 25°C. Serum samples were stored at
−80°C prior to analysis.
 | Table I.Characteristics of patients with HCC,
hepatitis or cirrhosis and healthy controls. |
Table I.
Characteristics of patients with HCC,
hepatitis or cirrhosis and healthy controls.
| Patient
characteristic | HCC (n=31) | Hepatitis/cirrhosis
(n=41) | Healthy controls
(n=35) |
|---|
| Age, years |
|
|
|
| Mean ±
SD (min, max) | 56±12 (36,76) | 41±16 (21,77) | 53±10 (26,71) |
| Sex |
|
|
|
| Male, %
(n/total) | 83.9 (26/31) | 82.9 (34/41) | 74.3 (26/35) |
| Female,
% (n/total) | 16.1 (5/31) | 17.1 (7/41) | 25.7 (9/35) |
| Cancer stage |
|
|
|
| II, %
(n/total) | 64.5 (20/31) |
|
|
| II +
IV, % (n/total) | 35.5 (11/31) |
|
|
| Hepatitis B
infection, n | 28 | 36 | 0 |
| Hepatitis C
infection, n | 3 | 5 | 0 |
 | Table II.Characteristics of patients with
hepatitis and cirrhosis and healthy controls. |
Table II.
Characteristics of patients with
hepatitis and cirrhosis and healthy controls.
| Patient
characteristic | Hepatitis
(n=33) | Cirrhosis
(n=8) | Healthy controls
(n=35) |
|---|
| Age, years |
|
|
|
| Mean ±
SD (min, max) | 41±13 (21,65) | 55±12 (32,77) | 53±10 (26,71) |
| Sex |
|
|
|
| Male, %
(n/total) | 81.8 (27/33) | 87.5 (7/8) | 74.3 (26/35) |
| Female,
% (n/total) | 18.2 (6/33) | 12.5 (1/8) | 25.7 (9/35) |
| Hepatitis B
infection, n | 28 | 8 | 0 |
| Hepatitis C
infection, n | 5 | 0 | 0 |
SPAG9 ELISA assay
Recombinant human SPAG9 protein (r-hSPAG9; Abnova,
Taipei, Taiwan) was used as antigen to establish an ELISA to detect
serum anti-SPAG9 immunoglobulin IgG antibody. Microtiter plates
were coated with r-hSPAG9 (100 ng/well) in 50 mM PBS (pH 7.4) at
4°C overnight. The plates were washed three times with PBS and
blocked with 5% bovine serum albumin (Zhejiang Tianhang
Biotechnology Co., Ltd, Huzhou, China) in PBS for 2 h at 37°C.
Post-blocking, the plates were incubated with a 1:10 dilution (0.05
M carbonate buffer, pH 9.6) of patient serum. Bound antibodies were
detected after incubation with a mouse anti-human antibody
conjugated to horseradish peroxidase (Beijing Beier Biological
Engineering Co., Ltd., Beijing, China; cat. no. 20141001) at an
optimized dilution of 1:5,000 in PBS for 2 h at 37°C. Enzyme
activation was performed with 0.05% orthophenylenediamine (Beijing
Beier Biological Engineering Co., Ltd.) in 50 mM citrate phosphate
buffer (pH 5.0) with 0.06% hydrogen peroxide as the substrate. The
reaction was terminated with 50 µl of 5 M
H2SO4, and the absorbance was read at a
wavelength of 450 nm using a microplate spectrophotometer with 630
nm as a reference filter. The intra- and inter-assay coefficients
of variation were 2.3 and 8.6%, respectively.
AFP chemiluminescence assay
Serum AFP levels were determined using the ADVIA
Centaur XP Immunoassay System (Siemens AG, Munich, Germany), and
the quality control materials were provided by Bio-Rad
Laboratories, Inc. (Hercules, CA, USA).
Statistical analysis
The Kruskal-Wallis, Mann-Whitney U,
independent-samples t and χ2 tests, as well as receiver
operator characteristic (ROC) curve analysis were performed using
SPSS version 16.0 (SPSS, Inc., Chicago, IL, USA). Results were
presented as the mean ± standard deviation. Anti-SPAG9 antibody
levels in patients with HCC, patients with hepatitis/cirrhosis and
healthy individuals were compared using the Mann-Whitney U test
with Bonferroni correction. α=0.0167 and P<0.0167 were
considered to indicate a statistically significant difference.
Positivity of anti-SPAG9 antibody in patients with HCC, patients
with hepatitis/cirrhosis and healthy individuals was compared using
the χ2 test and partitioned χ2 tests.
α=0.0125 and P<0.0125 were considered to indicate a
statistically significant difference. The percentages of patients
who were positive for a marker were compared using a χ2
test with an inspection level of 0.05 considered to indicate a
statistically significant difference. For multiple comparisons, the
χ2 test was used, with an inspection level corrected to
0.0125 considered to indicate a statistically significant
difference. For other comparisons performed with an
independent-samples t test, P<0.05 was considered to indicate a
statistically significant difference.
Results
Levels of serum anti-SPAG9 antibody in
patients with HCC and hepatitis/cirrhosis
The mean of the signal intensity in the SPAG9 ELISA
for patients with HCC (0.590±0.274) was significantly higher than
that for patients with hepatitis/cirrhosis (0.445±0.515) and
healthy individuals (0.189±0.115; P<0.001). Data from all
patients and individuals are plotted in Fig. 1A. Using a cut-off value of 0.42, 71.0%
of the patients with HCC were positive for the SPAG9 antigen,
whereas 26.8% of patients with hepatitis/cirrhosis and 8% of
healthy individuals were positive for the antigen based on this
cut-off (Fig. 1B). The mean
absorbance (0.89±0.810) of anti-SPAG9 immunoglobulin IgG antibody
in patients with cirrhosis was significantly higher compared with
that of patients with hepatitis (0.337±0.355) and healthy
individuals (P<0.001; Fig.
1C).
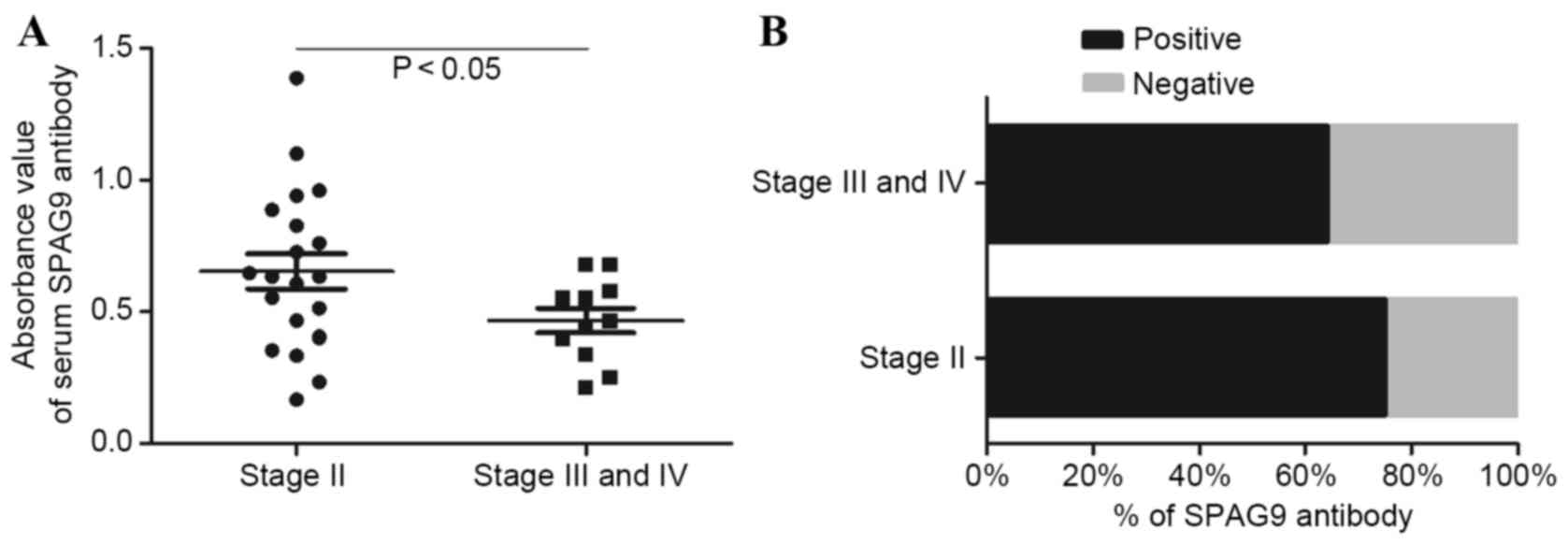
Levels of serum anti-SPAG9 antibody in
patients with various stages of HCC
The mean of the signal intensity in the SPAG9 ELISA
in patients with stage II HCC (0.647±0.310) was significantly
higher (P<0.01) compared with that in patients with stage III
and IV disease (0.468±0.153; Fig.
2A). Of the stage II patients with HCC, 75% were positive for
SPAG9, whereas 63.6% of stage III and IV patients were positive for
SPAG9 (Fig. 2B). This difference was
not significant.
Sensitivity and specificity of
anti-SPAG9 antibody alone and in combination with AFP for HCC
diagnosis
The sensitivity and specificity of anti-SPAG9
antibody alone for the diagnosis of HCC were 71.0 and 87.3%,
respectively. The sensitivity was higher compared with that of AFP
alone (64.5%), whereas the specificity was lower compared with that
of AFP alone (94.5%). When anti-SPAG9 and AFP were used in
parallel, the sensitivity and specificity were 90.3 and 83.6%,
respectively. In series, with the anti-SPAG9 antibody test
conducted first, the sensitivity and specificity were 45.2 and
98.2%, respectively (Table III).
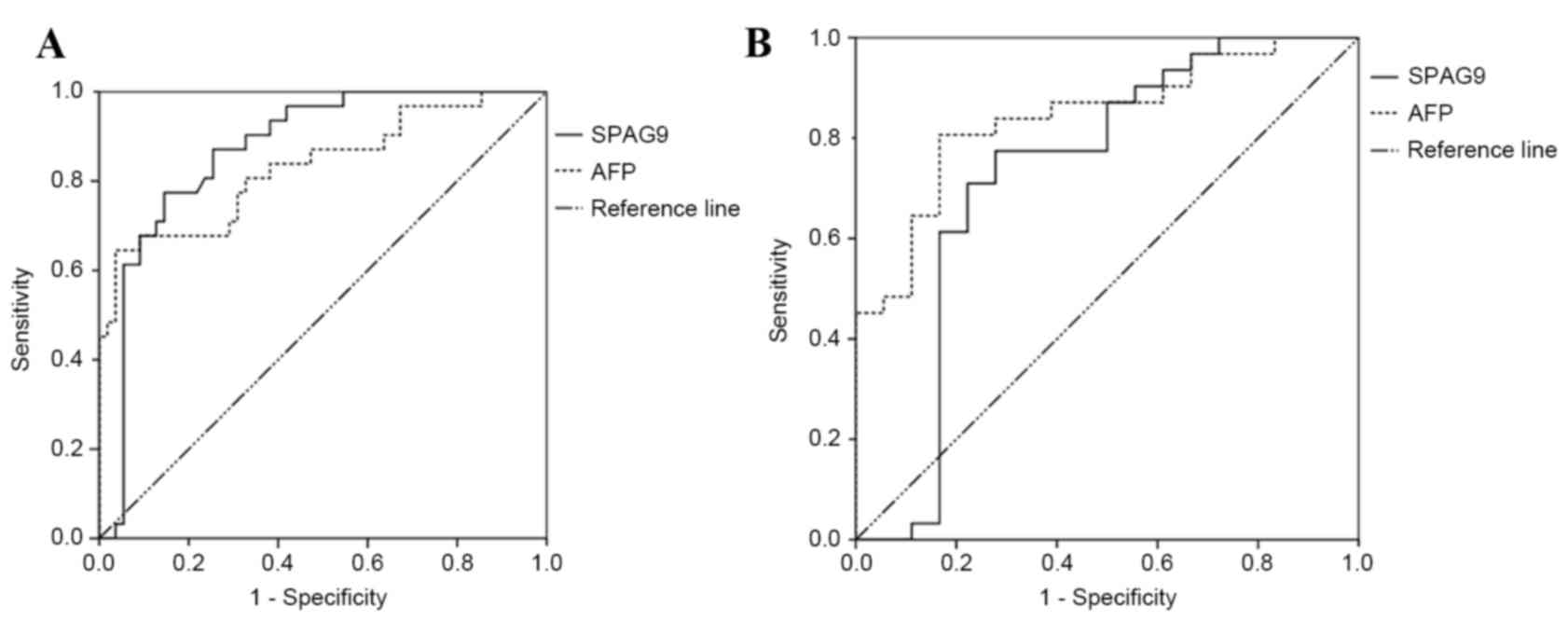
The ROC curve for serum anti-SPAG9 antibody had an AUC value of
0.870 [P<0.001; 95% confidence interval (CI), 0.793–0.947]. The
ROC curve for AFP had an AUC value of 0.832 (P<0.001; 95% CI,
0.736–0.928; Fig. 3A).
 | Table III.Diagnostic value of anti-SPAG9 alone
and in combination with AFP. |
Table III.
Diagnostic value of anti-SPAG9 alone
and in combination with AFP.
| Item | Sensitivity, % | Specificity, % | PPV, % | NPV, % | Positive likelihood
ratio | Negative likelihood
ratio | Youden index,
% |
|---|
| Anti-SPAG9
antibody | 71.0 | 87.3 | 75.9 | 84.2 | 5.58 | 0.33 | 58.2 |
| AFP | 64.5 | 94.5 | 87.0 | 82.5 | 11.83 | 0.38 | 59.1 |
| Parallel use | 90.3 | 83.6 | 75.7 | 93.9 | 5.52 | 0.12 | 74.0 |
| Series use
(anti-SPAG9, then AFP) | 45.2 | 98.2 | 93.3 | 76.1 | 24.84 | 0.56 | 43.3 |
The sensitivity and specificity of anti-SPAG9
antibody alone in the differential diagnosis of HCC were 71.0 and
77.8%, which was higher in sensitivity and lower in specificity
than the value obtained for AFP alone (64.5 and 83.3%,
respectively). A combination of anti-SPAG9 antibody with AFP in
parallel obtained a sensitivity and specificity of differential
diagnosis of 90.3 and 66.7%, respectively. When anti-SPAG9 antibody
and AFP were used in series, the sensitivity and specificity of
diagnosis were 45.2 and 94.4%, respectively (Table IV). ROC curves for serum anti-SPAG9
antibody had an AUC value of 0.729 (P<0.001; 95% CI,
0.559–0.899). The ROC curve for AFP had an AUC value of 0.842
(P<0.001; 95% CI, 0.732–0.953; Fig.
3B).
 | Table IV.Differential diagnostic value of
anti-SPAG9 alone and in combination with AFP. |
Table IV.
Differential diagnostic value of
anti-SPAG9 alone and in combination with AFP.
| Item | Sensitivity, % | Specificity, % | PPV, % | NPV, % | Positive likelihood
ratio | Negative likelihood
ratio | Youden index,
% |
|---|
| Anti-SPAG9
antibody | 71.0 | 77.8 | 84.6 | 60.9 | 3.19 | 0.37 | 48.7 |
| AFP | 64.5 | 83.3 | 87.0 | 57.7 | 3.87 | 0.43 | 47.8 |
| Parallel use | 90.3 | 66.7 | 82.4 | 80.0 | 2.71 | 0.15 | 57.0 |
| Series use
(anti-SPAG9, then AFP) | 45.2 | 94.4 | 93.3 | 50.0 | 8.13 | 0.58 | 39.6 |
Anti-SPAG9 antibody levels distinguish
between patients with HCC and with hepatitis/cirrhosis
Anti-SPAG9 antibodies were detected in 71.0% of
patients with HCC, whereas AFP was detected in 64.6% of patients;
this difference was not significant (P<0.05). Of patients with
hepatitis or cirrhosis, 26.8% tested positive for anti-SPAG9,
whereas 13% were positive for AFP, and this difference was
significant (P<0.01). In healthy controls, 8.0% had serum
antibodies against SPAG9 and 3.0% expressed AFP (Figs. 1B and 4). The proportion of male patients with HCC
that were positive for serum anti-SPAG9 antibody was significantly
lower than the proportion of female patients. By contrast, male
patients with HCC were more likely to test positive for serum AFP
compared with female patients (Fig.
5).
Discussion
China is a country with a high incidence of viral
hepatitis and high mortality rates due to HCC. In China, AFP is the
only serum biomarker included in the diagnostic criteria for HCC,
whereas other countries suggest the use of a combination of
non-invasive biomarkers for surveillance in high-risk populations.
At present, AFP is the most effective diagnostic indicator for HCC
(36). A recent meta-analysis of the
diagnostic value of AFP in HCC determined a pooled sensitivity of
66%, a specificity of 86% and an AUC value of 0.87 (37). The combination of AFP with DCP
produced a sensitivity of 55% for the detection of early-stage HCC
and 78% for the diagnosis of all stages of HCC, with cut-off values
of 10 ng/ml for AFP and 5 ng/ml for DCP (38). The addition of AFP-L3 led to a further
enhancement in sensitivity to 84% (39).
Anti-CTA antibodies are generally absent or present
at a low frequency in healthy individuals, but are highly expressed
by patients with cancer (40,41). The current study therefore
hypothesized that a CTA may serve as a biomarker for HCC. The
results revealed that the serum levels of anti-SPAG9 antibody had a
diagnostic sensitivity of 71.0%, a specificity of 87.3% and an AUC
value of 0.870 in patients with HCC. The combination of AFP with
anti-SPAG9 antibody in parallel had a sensitivity of 90.3%; in
series, the specificity was 98.2%. The level of serum anti-SPAG9
antibody was significantly higher in patients with HCC than in
patients with hepatitis or cirrhosis and healthy controls. In
addition, the serum anti-SPAG9 levels were significantly higher in
patients with stage II HCC compared with those in patients with
stage III or IV disease. These data indicate that anti-SPAG9 is a
potential early diagnostic marker for HCC. As the current study
evaluated a small cohort of patients, analyses of larger numbers of
patients are required.
The liver is a sexually dimorphic organ, with sex
variations in mitochondrial function, membrane lipid composition,
microsomal enzyme activity, gene expression and immune responses
(42). Sexual dimorphism of the liver
alters the metabolism of drugs and toxins in males and females
(43). This may at least partially
explain the observed sex differences in anti-SPAG9 antibody
expression in patients with HCC. In the current study, the
proportion of male patients with HCC that were positive for serum
anti-SPAG9 antibody was significantly lower compared with the
proportion of female patients. By contrast, male patients with HCC
were more likely to test positive for serum AFP compared with
female patients. However, the number of female patients included in
the present study was lower than the number of male patients, and
further research requires an expansion in the study population.
Chronic hepatitis and cirrhosis are common precursor
conditions of HCC. During the process of transition to malignancy,
certain patients may develop autoantibodies that were not present
during the precursory chronic liver disease phase (44). In the present study, the level of
anti-SPAG9 IgG antibody in patients with cirrhosis was
significantly higher compared with that in patients with hepatitis
and healthy controls. This suggests that the strong humoral immune
response triggered by SPAG9 in patients with cirrhosis may be an
early marker for carcinogenesis. A greater number of patients with
cirrhosis tested positive for SPAG9 compared with those who tested
positive for AFP, indicating that the humoral immune response to
SPAG9 may be an effective marker for early screening in populations
with a high risk for HCC.
In conclusion, anti-SPAG9 antibody levels in the
peripheral blood of patients with HCC were significantly higher
compared with those in patients with hepatitis or cirrhosis and
healthy controls. The potential value of SPAG9 as a diagnostic
marker for HCC requires further investigation. Combining serum
anti-SPAG9 antibody and AFP as disease markers may allow the early
diagnosis of HCC.
Acknowledgements
The present study was supported by a research grant
from the Health Department of Hunan Province Foundation (grant no.
B2011-099) and the Second People's Hospital of Hunan Province Key
Specialized Foundation (grant no. 2014-005).
Glossary
Abbreviations
Abbreviations:
|
SPAG9
|
sperm-associated antigen 9
|
|
HCC
|
hepatocellular carcinoma
|
|
AFP
|
α-fetoprotein
|
|
CTA
|
cancer-testis antigen
|
|
HBV
|
hepatitis B virus
|
|
HCV
|
hepatitis C virus
|
|
DCP
|
des-gamma-carboxy-prothrombin
|
|
ROC
|
receiver operator characteristic
|
References
|
1
|
Dhanasekaran R, Limaye A and Cabrera R:
Hepatocellular carcinoma: Current trends in worldwide epidemiology,
risk factors, diagnosis, and therapeutics. Hepat Med. 4:19–37.
2012.PubMed/NCBI
|
|
2
|
Raimondi S, Bruno S, Mondelli MU and
Maisonneuve P: Hepatitis C virus genotype 1b as a risk factor for
hepatocellular carcinoma development: A meta-analysis. J Hepatol.
50:1142–1154. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pollicino T, Squadrito G, Cerenzia G,
Cacciola I, Raffa G, Craxi A, Farinati F, Missale G, Smedile A,
Tiribelli C, et al: Hepatitis B virus maintains its pro-oncogenic
properties in the case of occult HBV infection. Gastroenterology.
126:102–110. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sherman M: Hepatocellular carcinoma:
Epidemiology, risk factors, and screening. Semin Liver Dis.
25:143–154. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Parkin DM: The global health burden of
infection-associated cancers in the year 2002. Int J Cancer.
118:3030–3044. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Song P, Feng X, Zhang K, Song T, Ma K,
Kokudo N, Dong J, Yao L and Tang W: Screening for and surveillance
of high-risk patients with HBV-related chronic liver disease:
Promoting the early detection of hepatocellular carcinoma in China.
Biosci Trends. 7:1–6. 2013.PubMed/NCBI
|
|
7
|
Kiyosawa K, Umemura T, Ichijo T, Matsumoto
A, Yoshizawa K, Gad A and Tanaka E: Hepatocellular carcinoma.
Recent trends in Japan. Gastroenterology. 127 5 Suppl 1:S17–S26.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Di Bisceglie AM, Lyra AC, Schwartz M,
Reddy RK, Martin P, Gores G, Lok AS, Hussain KB, Gish R, Van Thiel
DH, et al: Hepatitis C-related hepatocellular carcinoma in the
United States: Influence of ethnic status. Am J Gastroenterol.
98:2060–2063. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Donato F, Tagger A, Chiesa R, Ribero ML,
Tomasoni V, Fasola M, Gelatti U, Portera G, Boffetta P and Nardi G:
Hepatitis B and C virus infection, alcohol drinking, and
hepatocellular carcinoma: A case-control study in Italy. Brescia
HCC study. Hepatology. 26:579–584. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fattovich G, Giustina G, Degos F,
Tremolada F, Diodati G, Almasio P, Nevens F, Solinas A, Mura D,
Brouwer JT, et al: Morbidity and mortality in compensated cirrhosis
type C: A retrospective follow-up study of 384 patients.
Gastroenterology. 112:463–472. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kudo M, Han KH, Kokudo N, Cheng AL, Choi
BI, Furuse J, Izumi N, Park JW, Poon RT and Sakamoto M: Liver
cancer working group report. Jpn J Clin Oncol. 1 Suppl 40:i19–i27.
2010. View Article : Google Scholar
|
|
12
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
European Association for the Study of the
Liver, . European Organisation for Research and Treatment of
Cancer: EASL-EORTC clinical practice guidelines: Management of
hepatocellular carcinoma. J Hepatol. 56:908–943. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bruix J, Gores GJ and Mazzaferro V:
Hepatocellular carcinoma: Clinical frontiers and perspectives. Gut.
63:844–855. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Omata M, Lesmana LA, Tateishi R, Chen PJ,
Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT, et al: Asian
pacific association for the study of the liver consensus
recommendations on hepatocellular carcinoma. Hepatol Int.
4:439–474. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Makuuchi M, Kokudo N, Arii S, Futagawa S,
Kaneko S, Kawasaki S, Matsuyama Y, Okazaki M, Okita K, Omata M, et
al: Development of evidence-based clinical guidelines for the
diagnosis and treatment of hepatocellular carcinoma in Japan.
Hepatol Res. 38:37–51. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Song PP, Gao JJ, Kokudo N, Dong JH and
Tang W: ‘Knowledge into action’ exploration of an appropriate
approach for constructing evidence-based clinical practice
guidelines for hepatocellular carcinoma. Biosci Trends. 6:147–152.
2012.PubMed/NCBI
|
|
18
|
Song P, Gao J, Inagaki Y, Kokudo N,
Hasegawa K, Sugawara Y and Tang W: Biomarkers: Evaluation of
screening for and early diagnosis of hepatocellular carcinoma in
Japan and China. Liver Cancer. 2:31–39. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Song P, Tobe RG, Inagaki Y, Kokudo N,
Hasegawa K, Sugawara Y and Tang W: The management of
hepatocel-lular carcinoma around the world: A comparison of
guidelines from 2001 to 2011. Liver Int. 32:1053–1063. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Farinati F, Marino D, De Giorgio M, Baldan
A, Cantarini M, Cursaro C, Rapaccini G, Del Poggio P, Di Nolfo MA,
Benvegnù L, et al: Diagnostic and prognostic role of
alpha-fetoprotein in hepatocellular carcinoma: Both or neither? Am
J Gastroenterol. 101:524–532. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cui Z, Yu X, Guo L, Wei Y, Zheng S, Li W,
Chen P, Zhu J and Peng J: Combined analysis of serum
alpha-fetoprotein and MAGE-A3-specific cytotoxic T lymphocytes in
peripheral blood for diagnosis of hepatocellular carcinoma. Dis
Markers. 35:915–923. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Suri A: Cancer testis antigens-their
importance in immunotherapy and in the early detection of cancer.
Expert Opin Biol Ther. 6:379–389. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Grizzi F, Mirandola L, Qehajaj D, Cobos E,
Figueroa JA and Chiriva-Internati M: Cancer-testis antigens and
immunotherapy in the light of cancer complexity. Int Rev Immunol.
34:143–153. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Song MH, Choi KU, Shin DH, Lee CH and Lee
SY: Identification of the cancer/testis antigens AKAP3 and CTp11 by
SEREX in hepatocellular carcinoma. Oncol Rep. 28:1792–1798. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Peng JR, Chen HS, Mou DC, Cao J, Cong X,
Qin LL, Wei L, Leng XS, Wang Y and Chen WF: Expression of
cancer/testis (CT) antigens in Chinese hepatocellular carcinoma and
its correlation with clinical parameters. Cancer Lett. 219:223–232.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wang Y, Han KJ, Pang XW, Vaughan HA, Qu W,
Dong XY, Peng JR, Zhao HT, Rui JA, Leng XS, et al: Large scale
identification of human hepatocellular carcinoma-associated
antigens by autoantibodies. J Immunol. 169:1102–1109. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yang XA, Dong XY, Qiao H, Wang YD, Peng
JR, Li Y, Pang XW, Tian C and Chen WF: Immunohistochemical analysis
of the expression of FATE/BJ-HCC-2 antigen in normal and malignant
tissues. Lab Invest. 85:205–213. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Garg M, Chaurasiya D, Rana R, Jagadish N,
Kanojia D, Dudha N, Kamran N, Salhan S, Bhatnagar A, Suri S, et al:
Sperm-associated antigen 9, a novel cancer testis antigen, is a
potential target for immunotherapy in epithelial ovarian cancer.
Clin Cancer Res. 13:1421–1428. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jagadish N, Rana R, Mishra D, Kumar M and
Suri A: Sperm associated antigen 9 (SPAG9): A new member of c-Jun
NH2-terminal kinase (JNK) interacting protein exclusively expressed
in testis. Keio J Med. 54:66–71. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yi F, Ni W, Liu W, Pan X, Han X, Yang L,
Kong X, Ma R and Chang R: SPAG9 is overexpressed in human
astrocytoma and promotes cell proliferation and invasion. Tumour
Biol. 34:2849–2855. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Garg M, Kanojia D, Khosla A, Dudha N, Sati
S, Chaurasiya D, Jagadish N, Seth A, Kumar R, Gupta S, et al:
Sperm-associated antigen 9 is associated with tumor growth,
migration, and invasion in renal cell carcinoma. Cancer Res.
68:8240–8248. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Garg M, Kanojia D, Salhan S, Suri S, Gupta
A, Lohiya NK and Suri A: Sperm-associated antigen 9 is a biomarker
for early cervical carcinoma. Cancer. 115:2671–2683. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kanojia D, Garg M, Gupta S, Gupta A and
Suri A: Sperm-associated antigen 9, a novel biomarker for early
detection of breast cancer. Cancer Epidemiol Biomarkers Prev.
18:630–639. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Garg M, Kanojia D, Suri S, Gupta S, Gupta
A and Suri A: Sperm-associated antigen 9: A novel diagnostic marker
for thyroid cancer. J Clin Endocrinol Metab. 94:4613–4618. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kanojia D, Garg M, Gupta S, Gupta A and
Suri A: Sperm-associated antigen 9 is a novel biomarker for
colorectal cancer and is involved in tumor growth and
tumorigenicity. Am J Pathol. 178:1009–1020. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yao M, Zhao J and Lu F: Alpha-fetoprotein
still is a valuable diagnostic and prognosis predicting biomarker
in hepatitis B virus infection-related hepatocellular carcinoma.
Oncotarget. 7:3702–3708. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wan HG, Xu H, Gu YM, Wang H, Xu W and Zu
MH: Comparison osteopontin vs. AFP for the diagnosis of HCC: A
meta-analysis. Clin Res Hepatol Gastroenterol. 38:706–714. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ertle JM, Heider D, Wichert M, Keller B,
Kueper R, Hilgard P, Gerken G and Schlaak JF: A combination of
α-fetoprotein and des-γ-carboxy prothrombin is superior in
detection of hepatocellular carcinoma. Digestion. 87:pp. 121–131.
2013, View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hadziyannis E, Sialevris K, Georgiou A and
Koskinas J: Analysis of serum α-fetoprotein-L3% and des-γ
carboxyprothrombin markers in cases with misleading hepatocellular
carcinoma total α-fetoprotein levels. Oncol Rep. 29:835–839. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Tan EM: Autoantibodies as reporters
identifying aberrant cellular mechanisms in tumorigenesis. J Clin
Invest. 108:1411–1415. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Tan EM and Zhang J: Autoantibodies to
tumor-associated antigens: Reporters from the immune system.
Immunol Rev. 222:328–340. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Dhir RN, Dworakowski W, Thangavel C and
Shapiro BH: Sexually dimorphic regulation of hepatic isoforms of
human cytochrome p450 by growth hormone. J Pharmacol Exp Ther.
316:87–94. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Waxman DJ and Holloway MG: Sex differences
in the expression of hepatic drug metabolizing enzymes. Mol
Pharmacol. 76:215–228. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhang JY, Zhu W, Imai H, Kiyosawa K, Chan
EK and Tan EM: De-novo humoral immune responses to
cancer-associated autoantigens during transition from chronic liver
disease to hepatocellular carcinoma. Clin Exp Immunol. 125:3–9.
2001. View Article : Google Scholar : PubMed/NCBI
|