|
1
|
Chi AC, Day TA and Neville BW: Oral cavity
and oropharyngeal squamous cell carcinoma-an update. CA Cancer J
Clin. 65:401–421. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2013. CA: A Cancer J Clin. 63:11–30. 2013.
|
|
3
|
Li P, Cao Q, Shao P, Cai H, Zhou H, Chen
J, Qin C, Zhang Z, Ju X and Yin C: Genetic polymorphisms in HIF1A
are associated with prostate cancer risk in a Chinese population.
Asian J Androl. 14:864–869. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kim SS, Ruiz VE, Carroll JD and Moss SF:
Helicobacter pylori in the pathogenesis of gastric cancer
and gastric lymphoma. Cancer Lett. 305:228–238. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Whitmore SE and Lamont RJ: Oral bacteria
and cancer. PLos Pathog. 10:e10039332014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gershkovitz M, Fainsod-Levi T, Zelter T,
Sionov RV and Granot Z: TRPM2 modulates neutrophil attraction to
murine tumor cells by regulating CXCL2 expression. Cancer Immunol
Immunother. 68:33–43. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Song JM, Woo BH, Lee JH, Yoon S, Cho Y,
Kim YD and Park HR: Oral Administration of Porphyromonas
gingivalis, a major pathogen of chronic periodontitis, promotes
resistance to paclitaxel in mouse xenografts of oral squamous cell
carcinoma. Int J Mol Sci. 20:24942019. View Article : Google Scholar
|
|
8
|
Gao JL, Kwan AH, Yammine A, Zhou X,
Trewhella J, Hugrass BM, Collins D, Horne J, Ye P, Harty D, et al:
Structural properties of a haemophore facilitate targeted
elimination of the pathogen Porphyromonas gingivalis. Nat
Commun. 9:40972018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Inaba H, Sugita H, Kuboniwa M, Iwai S,
Hamada M, Noda T, Morisaki I, Lamont RJ and Amano A:
Porphyromonas gingivalis promotes invasion of oral squamous
cell carcinoma through induction of proMMP9 and its activation.
Cell Microbiol. 16:131–145. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lanzós I, Herrera D, Santos S, O'Connor A,
Peña C, Lanzós E and Sanz M: Microbiological effects of an
antiseptic mouth rinse in irradiated cancer patients. Med Oral
Patol Oral Cir Bucal. 16:e1036–e1042. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
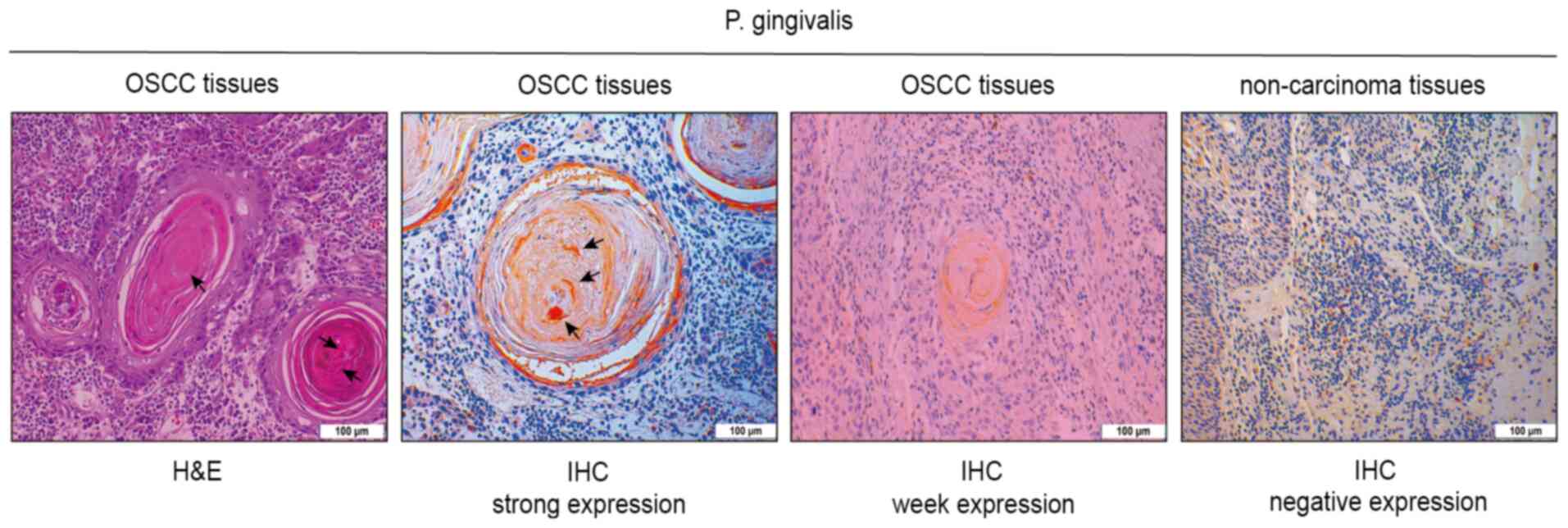
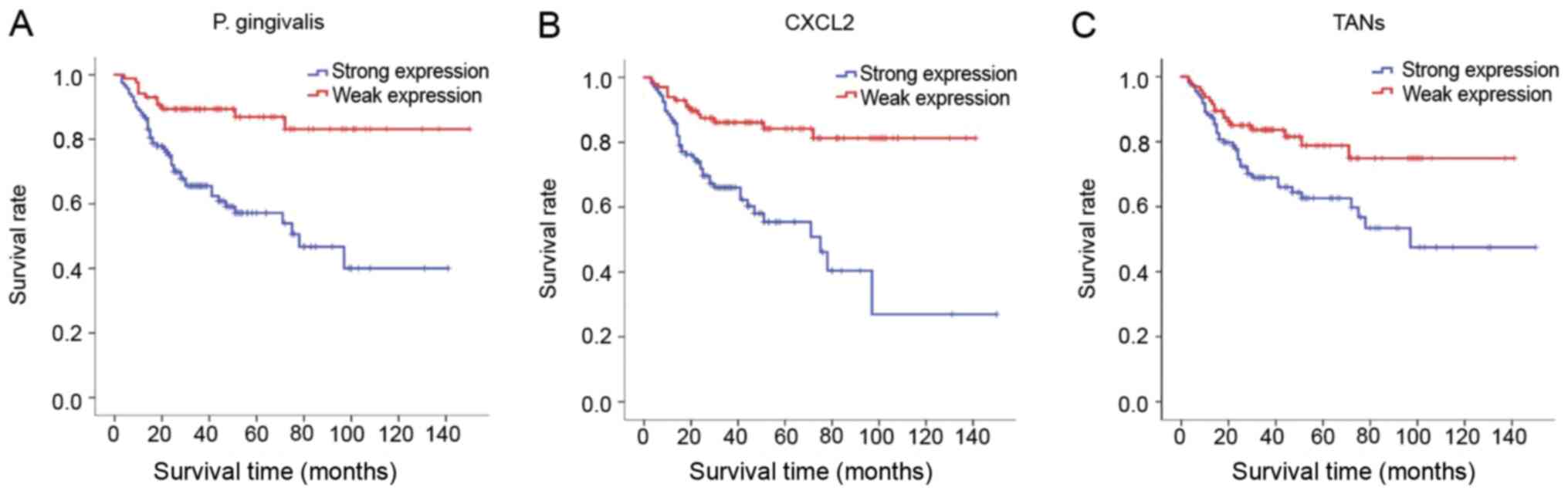
Wen L, Mu W, Lu H, Wang X, Fang J, Jia Y,
Li Q, Wang D, Wen S, Guo J, et al: Porphyromonas gingivalis
Promotes oral squamous cell carcinoma progression in an immune
microenvironment. J Dent Res. 99:666–675. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
da Silva JM, Soave DF, Moreira Dos Santos
TP, Batista AC, Russo RC, Teixeira MM and da Silva TA: Significance
of chemokine and chemokine receptors in head and neck squamous cell
carcinoma: A critical review. Oral Oncol. 56:8–16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vashishta A, Jimenez-Flores E, Klaes CK,
Tian S, Miralda I, Lamont RJ and Uriarte SM: Putative periodontal
pathogens, Filifactor alocis and Peptoanaerobacter
Stomatis, induce differential cytokine and chemokine production
by human neutrophils. Pathogens. 8:592019. View Article : Google Scholar
|
|
14
|
Hardaway AL, Herroon MK, Rajagurubandara E
and Podgorski I: Marrow adipocyte-derived CXCL1 and CXCL2
contribute to osteolysis in metastatic prostate cancer. Clin Exp
Metastasis. 32:353–368. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
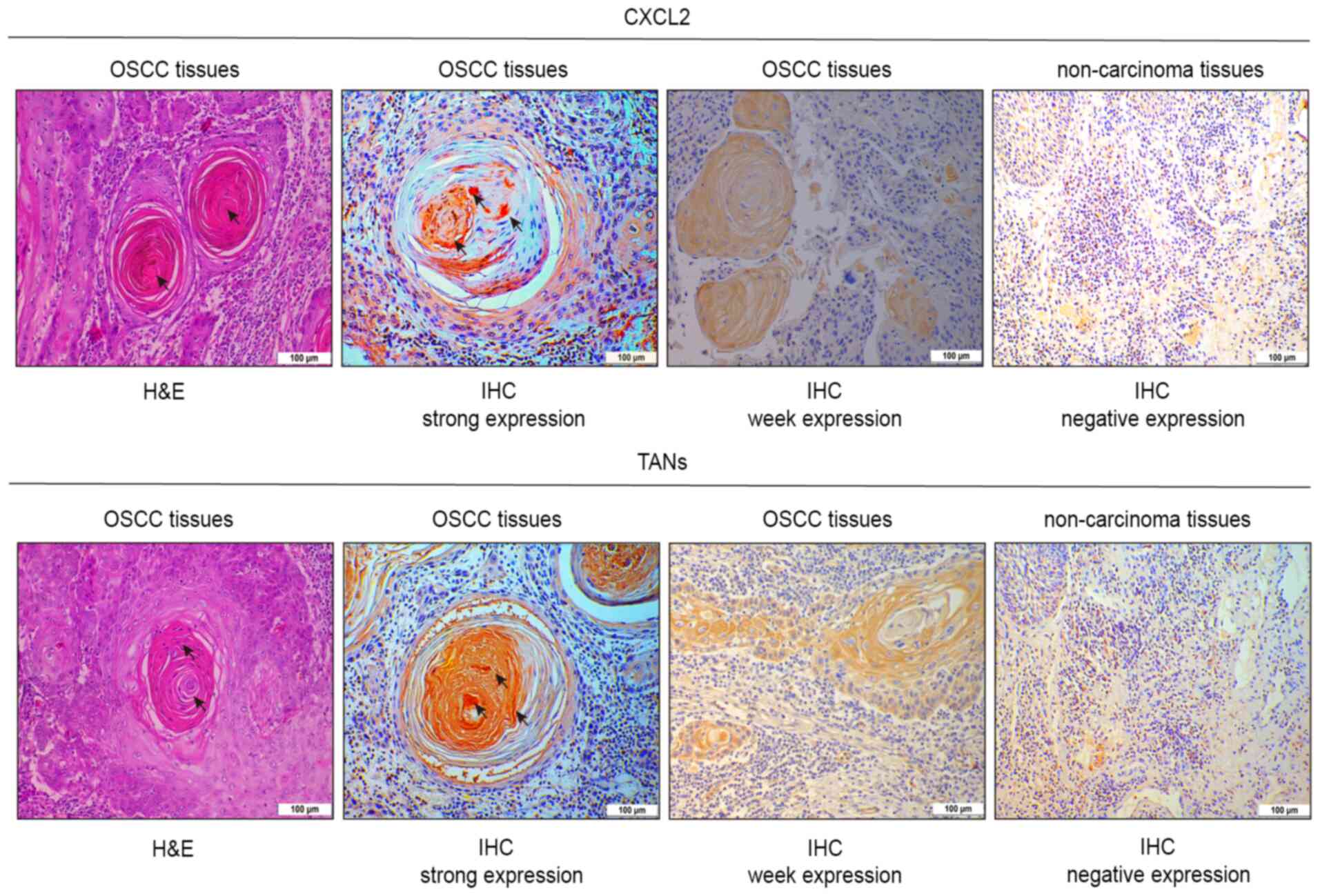
Zhang H, Ye YL, Li MX, Ye SB, Huang WR,
Cai TT, He J, Peng JY, Duan TH, Cui J, et al: CXCL2/MIF-CXCR2
signaling promotes the recruitment of myeloid-derived suppressor
cells and is correlated with prognosis in bladder cancer. Oncogene.
36:2095–2104. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fridlender ZG, Sun J, Mishalian I, Singhal
S, Cheng G, Kapoor V, Horng W, Fridlender G, Bayuh R, Worthen GS
and Albelda SM: Transcriptomic analysis comparing tumor-associated
neutrophils with granulocytic myeloid-derived suppressor cells and
normal neutrophils. PLoS One. 7:e315242012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hagerling C and Werb Z: Neutrophils:
Critical components in experimental animal models of cancer. Semin
Immunol. 28:197–204. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Powell DR and Huttenlocher A: Neutrophils
in the tumor microenvironment. Trends Immunol. 37:41–52. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li S, Cong X, Gao H, Lan X, Li Z, Wang W,
Song S, Wang Y, Li C, Zhang H, et al: Tumor-associated neutrophils
induce EMT by IL-17a to promote migration and invasion in gastric
cancer cells. J Exp Clin Cancer Res. 38:62019. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sahingur SE and Yeudall WA: Chemokine
function in periodontal disease and oral cavity cancer. Front
Immunol. 6:2142015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Carey LA, Metzger R, Dees EC, Collichio F,
Sartor CI, Ollila DW, Klauber-DeMore N, Halle J, Sawyer L, Moore DT
and Graham ML: American Joint Committee on cancer
tumor-node-metastasis stage after neoadjuvant chemotherapy and
breast cancer outcome. J Natl Cancer Inst. 97:1137–1142. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Geng F, Liu J, Guo Y, Li C, Wang H, Wang
H, Zhao H and Pan Y: Persistent exposure to Porphyromonas
gingivalis promotes proliferative and invasion capabilities,
and tumorigenic properties of human immortalized oral epithelial
cells. Front Cell Infect Microbiol. 7:57–61. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Qiu X, Lei Z, Wang Z, Xu Y, Liu C, Li P,
Wu H and Gong Z: Knockdown of LncRNARHPN1-AS1 inhibits cell
migration, invasion and proliferation in head and neck squamous
cell carcinoma. J Cancer. 10:4000–4008. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li L, Lei Q, Zhang S, Kong L and Qin B:
Screening and identification of key biomarkers in hepatocellular
carcinoma: Evidence from bioinformatic analysis. Oncol Rep.
38:2607–2618. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bryne M, Koppang HS, Lilleng R, Stene T,
Bang G and Dabelsteen E: New malignancy grading is a better
prognostic indicator than Broders' grading in oral squamous cell
carcinomas. J Oral Pathol Med. 18:432–437. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Carus A, Ladekarl M, Hager H, Nedergaard
BS and Donskov F: Tumour-associated CD66b+ neutrophil count is an
independent prognostic factor for recurrence in localised cervical
cancer. Br J Cancer. 108:2116–2122. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Akinkugbe AA, Garcia DT, Brickhouse TH and
Mosavel M: Lifestyle risk factor related disparities in oral cancer
examination in the U.S: A population-based cross-sectional study.
BMC Public Health. 20:153–163. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Danaei G: Global burden of
infection-related cancer revisited. Lancet Oncol. 13:564–565. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Iqbal J, McRae S, Banaudha K, Mai T and
Waris G: Mechanism of hepatitis C virus (HCV)-induced osteopontin
and its role in epithelial to mesenchymal transition of
hepatocytes. J Biol Chem. 293:200102018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Horikawa T, Yang J, Kondo S, Yoshizaki T,
Joab I, Furukawa M and Pagano JS: Twist and epithelial-mesenchymal
transition are induced by the EBV oncoprotein latent membrane
protein 1 and are associated with metastatic nasopharyngeal
carcinoma. Cancer Res. 67:1970–1978. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chandrakesan P, Roy B, Jakkula LU, Ahmed
I, Ramamoorthy P, Tawfik O, Papineni R, Houchen C, Anant S and Umar
S: Utility of a bacterial infection model to study
epithelial-mesenchymal transition, mesenchymal-epithelial
transition or tumorigenesis. Oncogene. 33:2639–2654. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Parkin DM: The global health burden of
infection-associated cancers in the year 2002. Int J Cancer.
118:3030–3044. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lee J, Roberts JS, Atanasova KR, Chowdhury
N, Han K and Yilmaz Ö: Human primary epithelial cells acquire an
epithelial-mesenchymal-transition phenotype during long-term
infection by the oral opportunistic pathogen, Porphyromonas
gingivalis. Front Cell Infect Microbiol. 7:4932017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Woo BH, Kim DJ, Choi JI, Kim SJ, Park BS,
Song JM, Lee JH and Park HR: Oral cancer cells sustainedly infected
with Porphyromonas gingivalis exhibit resistance to Taxol
and have higher metastatic potential. Oncotarget. 8:46981–46992.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wen L, Mu W, Lu H, Wang X, Fang J, Jia Y,
Li Q, Wang D, Wen S, Guo J, et al: Porphyromonas gingivalis
Promotes oral squamous cell carcinoma progression in an immune
microenvironment. J Dent Res. 99:666–675. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Peres MA, Macpherson LMD, Weyant RJ, Daly
B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño
CC, Kearns C, et al: Oral diseases: A global public health
challenge. Lancet. 394:249–260. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yee M, Kim S, Sethi P, Duzgunes N and
Konopka K: Porphyromonas gingivalis stimulates IL-6 and IL-8
secretion in GMSM-K, HSC-3 and H413 oral epithelial cells.
Anaerobe. 28:62–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
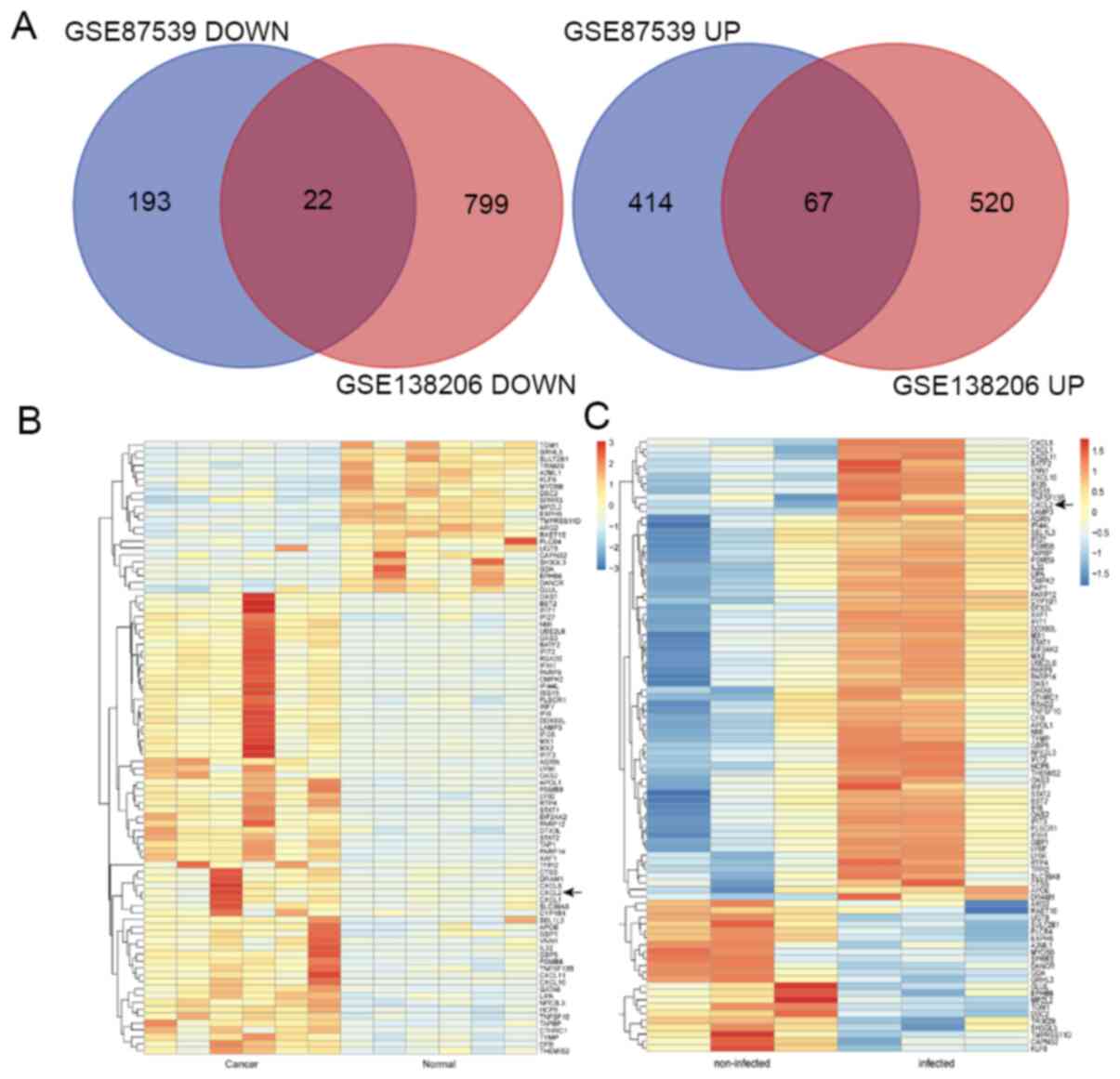
Geng F, Wang Q, Li C, Liu J, Zhang D,
Zhang S and Pan Y: Identification of potential candidate genes of
oral cancer in response to chronic infection with Porphyromonas
gingivalis using bioinformatical analyses. Front Oncol.
9:912019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Bunt SK, Yang L, Sinha P, Clements VK,
Leips J and Ostrand-Rosenberg S: Reduced inflammation in the tumor
microenvironment delays the accumulation of myeloid-derived
suppressor cells and limits tumor progression. Cancer Res.
67:10019–10026. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zenobia C and Hajishengallis G:
Porphyromonas gingivalis virulence factors involved in
subversion of leukocytes and microbial dysbiosis. Virulence.
6:236–243. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhang Y and Li X:
Lipopolysaccharide-regulated production of bone sialoprotein and
interleukin-8 in human periodontal ligament fibroblasts: The role
of toll-like receptors 2 and 4 and the MAPK pathway. J Periodontal
Res. 50:141–151. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Shi H, Han X, Sun Y, Shang C, Wei M, Ba X
and Zeng X: Chemokine (C-X-C motif) ligand 1 and CXCL2 produced by
tumor promote the generation of monocytic myeloid-derived
suppressor cells. Cancer Sci. 109:3826–3839. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ban Y, Mai J, Li X, Mitchell-Flack M,
Zhang T, Zhang L, Chouchane L, Ferrari M, Shen H and Ma X:
Targeting autocrine CCL5-CCR5 axis reprograms immunosuppressive
myeloid cells and reinvigorates antitumor immunity. Cancer Res.
77:2857–2868. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Lafuente Ibáñez de Mendoza I, Maritxalar
Mendia X, García de la Fuente AM, Quindós Andrés G and Aguirre
Urizar JM: Role of Porphyromonas gingivalis in oral squamous
cell carcinoma development: A systematic review. J Periodontal Res.
55:13–22. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ohms M, Moller S and Laskay T: An attempt
to polarize human neutrophils toward N1 and N2 phenotypes in vitro.
Front Immunol. 11:5322020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Feliciano P: CXCL1 and CXCL2 link
metastasis and chemoresistance. Nat Genet. 44:8402012. View Article : Google Scholar
|
|
47
|
Eckert AW, Wickenhauser C, Salins PC,
Kappler M, Bukur J and Seliger B: Correction to: Clinical relevance
of the tumor microenvironment and immune escape of oral squamous
cell carcinoma. J Transl Med. 16:402018. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Eruslanov EB, Bhojnagarwala PS, Quatromoni
JG, Stephen TL, Ranganathan A, Deshpande C, Akimova T, Vachani A,
Litzky L, Hancock WW, et al: Tumor-associated neutrophils stimulate
T cell responses in early-stage human lung cancer. J Clin Invest.
124:5466–5480. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wu P, Wu D, Ni C, Ye J, Chen W, Hu G, Wang
Z, Wang C, Zhang Z, Xia W, et al: γδT17 cells promote the
accumulation and expansion of myeloid-derived suppressor cells in
human colorectal cancer. Immunity. 40:785–800. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Peltanova B, Raudenska M and Masarik M:
Effect of tumor microenvironment on pathogenesis of the head and
neck squamous cell carcinoma: A systematic review. Mol Cancer.
18:632019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Yasunaga JI and Matsuoka M: Oncogenic
spiral by infectious pathogens: Cooperation of multiple factors in
cancer development. Cancer Sci. 109:24–32. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wen J, Wang Y, Gao C, Zhang G, You Q,
Zhang W, Zhang Z, Wang S, Peng G and Shen L: Helicobacter pylori
infection promotes Aquaporin 3 expression via the
ROS-HIF-1α-AQP3-ROS loop in stomach mucosa: A potential novel
mechanism for cancer pathogenesis. Oncogene. 37:3549–3561. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Nagarsheth N, Wicha MS and Zou W:
Chemokines in the cancer microenvironment and their relevance in
cancer immunotherapy. Nat Rev Immunol. 17:559–572. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Damgaard C, Kantarci A, Holmstrup P,
Hasturk H, Nielsen CH and Van Dyke TE: Porphyromonas
gingivalis-induced production of reactive oxygen species, tumor
necrosis factor-α, interleukin-6, CXCL8 and CCL2 by neutrophils
from localized aggressive periodontitis and healthy donors:
Modulating actions of red blood cells and resolvin E1. J
Periodontal Res. 52:246–254. 2017. View Article : Google Scholar : PubMed/NCBI
|