Introduction
Rhabdomyosarcoma (RMS) is a rare yet highly
malignant cancer type in the adult population, with an estimated
incidence of 0.9 per million per year (1). It may affect numerous structures and
organs, including the head and neck, genitourinary tract,
extremities and trunk (1,2). Adults with spinal RMS have a
significantly poor prognosis. Wang et al (3) reported that the median overall
survival (OS) period was merely 10 months, in a retrospective study
of 11 cases and review of 22 cases from the previous literature.
They indicated that the cases with radical resection had a longer
median OS period (3). Treatment
guidelines and recommendations for adult spinal RMS were
established in reference to those for children and experts'
experience, rather than studies of high quality (3–6).
In the present study, the case of a middle-aged
female with isolated spinal RMS involving T11 to L2 vertebrae was
reported. The patient was scheduled to receive a multimodality
treatment regimen of total resection with 3D-print reconstruction,
early start of stereotactic body radiotherapy (SBRT) and
chemotherapy. Consequently, the patient enjoyed a long survival
period and the outcome was encouraging. Furthermore, the literature
regarding spinal RMS was reviewed and an overview of the evidence
of the efficacy of treatment modalities currently available was
presented. The case described herein provides useful information
that will be of value to the clinical community.
Case report
Case presentation
A 46-year-old female patient visited Peking
University Third Hospital (Beijing, China) in November 2017 due to
progressive back pain. However, the patient had no symptoms or
signs of neurological impairment as determined by physical
examination. The patient was practically afebrile and in an overall
good condition. The patient had no history of malignancies, known
history of tuberculosis infection or invasive interventions on the
spine. The results of laboratory tests were generally normal and
serological examination for tumor markers of breast, lung,
gastrointestinal and liver neoplasms was negative.
Imaging work-ups
Computed tomography (CT) scans revealed large
expansile, osteolytic lesions mainly dwelling in the right halves
of the T12 and L1 vertebral bodies (Fig. 1). The lesion on magnetic resonance
imaging scans revealed homogeneously T1-weighted hypointense and
T2-weighted hyperintense signals. On axial images, possible
involvement of the right crus of the diaphragm was noted. The
images of positron emission tomography-CT revealed significantly
elevated uptake of 18-fluorodeoxyglucose in the T11-L2 region.
 | Figure 1.Presentation of the imaging prior to
the operation. (A-F) Computed tomography sagittal (A) and coronal
(B) reconstruction films revealed an osteolytic, expansile lesion
in the spine, with (C) T11, (D) T12, (E) L1 and (F) L2 being
invaded. (G-I) On magnetic resonance imaging scans, the lesion was
(G) T1-weighted hypointensive and (I) T2-weighted hyperintensive,
with edema signals in the normal parts of the vertebrae. (H) The
lesion displayed homogeneous enhancement on T1-enhanced films. The
lesion invaded the (C and H) anterior, lower corner of T11 (red
arrow in H) and (F and H) anterior superior corner of L2 (green
arrow in H). (H) A long-flank soft tissue mass was revealed along
the anterior T11 to the superior corner of the L2 vertebra. From
the images of (J) T12 and (K) L1 planes, the right crus of the
diaphragm had a possible involvement with the tumor, whilst the
periaortic space stayed uninvaded (scale bars, 2 cm). |
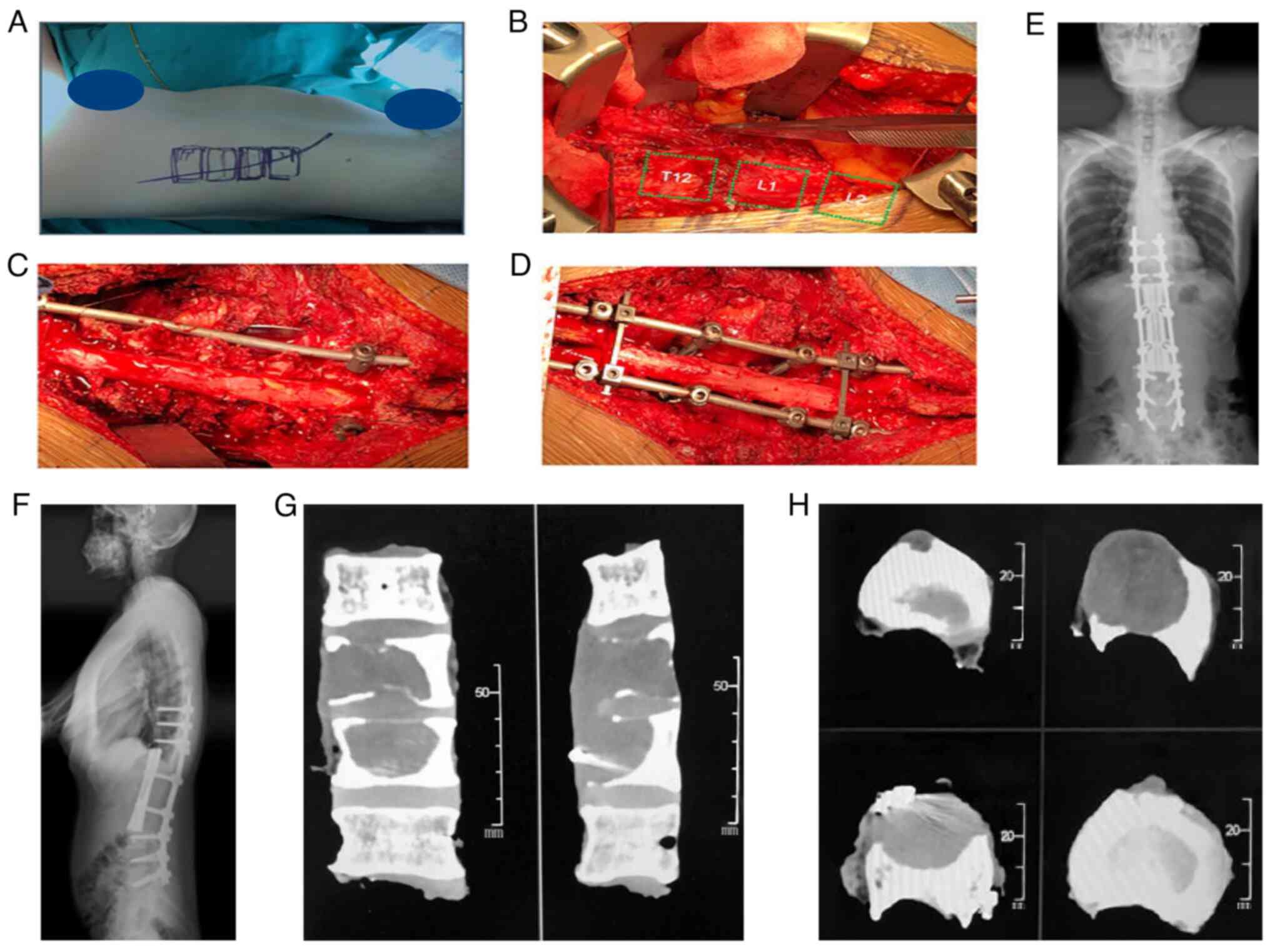
Surgical strategies and
techniques
The patient of the current study presented with an
isolated spinal lesion, without any distant metastasis or visceral
organs involved. Furthermore, the involvement of paraspinal tissues
was relatively limited (Fig. 1G-K),
which remained the possibility of total en-bloc resection.
Thus, it was decided to surgically resect the tumor lesion.
Prior to the operation, the feeding vessels of the
tumor and Adamkiewicz artery were evaluated by digital subtraction
angiography. Just the feeding vessels were embolized while keeping
the Adamkiewicz artery untouched. According to the extent of the
tumor invading the vertebral body, anterior dissection was
performed via a retroperitoneal approach with the patient in the
left decubitus position (Fig. 2).
The margins of the tumor were ill-defined and no intact capsule was
detected. The attaching segment of iliopsoas and suspicious portion
of the right diaphragm crus were cut off. The anterior exposure was
practically fulfilled by blunt dissection with fingers. During the
procedure, the anterior one-third of the intervertebral disc was
removed.
The patient was then placed in the prone position
and sufficient exposure from T8 to L5 was established. The
bilateral nerves of T11, T12 and L1 were ligated and cut, while the
L2 nerves were preserved. Dissection along the vertebral bodies was
then performed in a forward direction to conjoin with the anterior
dissection. The remaining posterior intervertebral disc was
removed. The specimen was rotated out, entirely and uneventfully.
The reconstruction was then made with a patient-tailored 3D-printed
prosthesis and the fixation levels were at T8, T9 and T10, and L3,
L4 and L5. The 3D-printed implant had two lateral holes, which were
connected with the posterior rods by the screws. The implant was
fabricated with titanium alloy and contained a porous
microstructure mimicking cancellous bone, so no additional bone
graft was required to achieve the final fusion.
The postoperative pathological examinations were
conducted according to standard procedures and the results were
consistent with embryonal RMS. The margin of the specimen was clear
of tumor infiltration.
Rehabilitation and pain
management
At one week after the operation, the patient was
transferred to the rehabilitation center of Peking University Third
Hospital (Beijing, China), to facilitate the recovery of the
patient's physical functions. During the postoperative hospital
stay, the patient reported slight to moderate pain and was
prescribed oral non-steroidal anti-inflammatory drugs to control
her pain.
RT and chemotherapy
The patient started SBRT 40 days after the
operation. The radioactive dose was 35 Gy in five fractions. After
another 40 days, the patient was administered six cycles of
chemotherapy and the regimen was six cycles of ifosfamide +
adriamycin (Fig. 3).
Post-treatment course and events
During the chemotherapy period, a subcutaneous
nodule was detected, which was inferred to be the colonization of
disseminated tumor cells in the procedure of CT-guided biopsy. The
patient underwent extensive skin and subcutaneous removal to
radically resect the lesion (Fig.
4). Pulmonary metastasis was detected 10 months after the
operation. A video-assisted thoracoscopic surgery was arranged to
resect the metastatic lesion, which was followed by three cycles of
ifosfamide + etoposide + vincristine.
Local recurrence appeared 19 months after the
operation in the right crus of the diaphragm (Fig. 5). At the same time, pulmonary
metastasis exhibited slight progress. Therefore, SBRT was
implemented at these two sites.
Latest follow-up
At the latest follow-up, which was 40 months after
the index operation, it was indicated that the local recurrence was
stable, but that pulmonary metastasis progressed with new nodules
emerging. Therefore, the patient was prepared for another cycle of
SBRT for progressing pulmonary metastasis.
Discussion
Among adults with RMS, patients with spinal
involvement have a much poorer prognosis (3). The 5-year survival rate of adult RMS
was reported to be 27% (7), but
there were no such data for the subgroup of spinal RMS. In the
series of Wang et al (3),
the longest survival period was 18 months. By contrast, the patient
of the present study has survived for >40 months since the index
surgery in December 2017. Considering the patient is of moderate
health and tolerant to another cycle of SBRT, she may presumably
have a long life expectancy.
A multi-modalities regimen is common practice for
the treatment of spinal RMS and total en-bloc resection
remains a first choice, particularly for an isolated lesion
(3–6). This malignancy is of an aggressive
nature. Invasion to multiple vertebrae and juxtaposing soft tissues
may have occurred by the time of diagnosis (3). The challenges of surgery include how
to radically resect the tumor and reconstruct the spine at the same
time. The former challenge is the surgeons' experience and surgical
skills concerned; the latter has been mitigated with the
application of a customized 3D-printed vertebral body (8).
The patient of the current study presented with a
long-flank soft tissue mass anterior to the vertebral bodies and
suspicious involvement of the right crus of the diaphragm. An
anterior dissection and exposure would be indicated in this
setting. The suspicious segment of the right diaphragm crus was cut
off to secure a clear margin. The posterior manipulations were
technically challenging. To facilitate the removal, certain nerve
roots were required to be sacrificed, which, however, left no
persistent sequelae. During the procedure, caution was taken to
avoid tear of the dural sac and the pleura/peritoneum on the
ventral side. The surgeon should be alert to the dissemination of
tumor cells in the surgical bed, which should be avoided. In the
present case, distilled water and cisplatinum irrigation were used
to avoid the colonization of tumor cells in situ.
Radiotherapy has demonstrated its efficacy for local
control after surgery (4–6,9,10). In
the previous literature, numerous advanced and effective delivery
techniques, including intensity-modulated RT, brachytherapy, proton
beam RT and SBRT, have been described (4,10).
SBRT is an image-guided modality and may be planned well according
to the postoperative and re-irradiation settings, allowing accurate
delivery of the local ablative dose (9). This technique has a prominent
advantage for the tumors around the cord; thus, this delivery
technique was applied to the patient of the present study. Usually,
RT is performed between 6 and 12 weeks after the operation, but an
earlier start forebodes a better local control for parameningeal
RMS (4,10). Considering the relatively quick
healing of the wound and timely restoration of the patient's
general condition, SBRT on the operative area, particularly the
right diaphragm crus, was started 40 days after the operation,
which led to local recurrence occurring later than previously
reported (3). In previous studies,
a wide range of RT doses, from 20 to 70 Gy, is used (3,10). The
final dose administered to the patient of the present study was
decided based on the studies and treatment experience of low-risk
pediatric patients (4). The patient
literally had a period of local control for 19 months until a
relapse occurred in the right diaphragm crus. The relapse in this
area was preoperatively expected, considering the existence of
tumor invasion. However, it would be too invasive to remove the
entire diaphragm and paraspinal muscle, as this may cause severe
respiratory dysfunction and visceral complications. In the present
study, SBRT was administered as 5 fractions, which was rather like
intensity-modulated RT, as SBRT in single- and multi-fractions may
provide satisfactory efficacy for spinal tumors (11). The combination of total
en-bloc tumor resection and earlier start of adjuvant SBRT
may provide satisfying local control for isolated spinal RMS
(11).
Due to the small number of adult patients and lack
of centralization of care for them, there is currently no
standardized recommended chemotherapy regimen for adults with RMS.
The general practice is to refer to regimens for pediatric
patients. The mainstay regimen for pediatric patients is
vincristine, actinomycin D and cyclophosphamide (VAC) (2–4). The
combination and dose of these agents are required to be balanced
over the efficacy and cytotoxicity. Previous studies emphasized the
incorporation of cyclophosphamide into the regimen (3,12–16).
However, the cumulative toxicity must be heeded for pediatric
patients, which usually impedes the administration of a sufficient
dose. Therefore, in the adult patient of the present study, the
dose of cyclophosphamide was intensified with caution (nine cycles
in total). The efficacy of doxorubicin did not stand firmly in the
reexamination in a multicenter, randomized controlled trial, in
spite of numerous studies stating it as the standard of care
(1,17). In addition, the use of other
traditional agents was sporadically reported and their efficacy
requires further examination (4,12,13,18).
Certain on-going prospective trials continue to examine and develop
new chemotherapy agents and molecular therapies (19). Furthermore, another modality is
rising and has gained substantial interest. Targeted therapy was
revealed to have encouraging potential in various
clinical/preclinical studies and is likely to provide a big advance
in the care of RMS (3,19–21).
In a national study including 449 adults with RMS,
Bompas et al (1) reported
that non-alveolar RMS, younger age (<25 years), R0 resection, RT
and VAC-based chemotherapy regimens were relevant with a better OS
in patients with localized RMS. In the patient of the present
study, the employment of a 3D-printed vertebral body enabled an
invasive yet complete resection of multiple vertebrae, yielding an
R0 resection. The earlier start of SBRT after the operation further
facilitated local control. These made a remarkable contribution to
the long locoregional control period for the patient of the present
study. The treatment schedule of this patient was individualized by
our institutional multidisciplinary treatment team. Considering
that the tumor mostly dwelled within the vertebral space and had
limited involvement of surrounding soft tissue, the resection
surgery was undertaken as the first step. Preoperative SBRT may
reduce tumor load and remain an alternative option. However, it
frequently causes severe adhesion of tumor capsule to the
surrounding tissues. Regrettably, the patient of the present study
developed colonization of tumor cells in the path of biopsy, which
was an indication for extensive skin and subcutaneous removal. This
event raises awareness of the necessity of a holistic and
coordinated strategy when planning the path of biopsy and surgical
incision. However, the outcome for the present patient was
encouraging, suggesting that proactive treatment strategies and
advances in surgical techniques and instruments still have an
essential role in primary tumors of high malignancy.
Currently, there is no well-established treatment
guideline for adult RM, and physicians used to refer to the
treatment strategy for pediatric patients (3–6).
Numerous lessons may be learned from the patient of the present
study. As adult RMS is highly malignant, total en-bloc
resection of the tumor is so far the best choice. Different from
the condition in children, adult RMS is less sensitive to
conventional RT and CT (1,4,12,13,18).
Thus, adjuvant SBRT was performed after the operation. Furthermore,
the puncture biopsy channels were planned to be removed together
when designing the operation plan prior to surgery. If the tumor
has invaded the diaphragm and paraspinal muscles, it is technically
impossible to remove the entire diaphragm and iliopsoas muscle.
However, it may be recommended that the invaded part of muscles
shall be dissected in an extracapsular way, leaving the tumor
untouched intraoperatively, and then remove the whole specimen.
Acknowledgements
The authors would like to thank Dr Baoshan Cao and
Dr Li Liang (Department of Medical Oncology and Radiation Sickness,
Peking University Third Hospital, Beijing, China) for their support
in the preparation of this article.
Funding
This study was supported by the institutional research fund
(Peking University Third Hospital; grant no. Y73504-03). The fund
had no influence on the design of the study, the collection,
analysis or interpretation of data or the preparation of the
manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SD and PH designed the report, reviewed the patient
information, collected and processed the clinical data and drafted
the manuscript. SY performed the pathological diagnosis. HZ
performed RT and chemotherapy. FW designed the study, selected the
patient, processed the data and supervised the study. SD and PH
confirm the authenticity of all the raw data. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The preparation of this retrospective study was
approved by the Ethics Committee Board of Peking University Third
Hospital (Beijing, China). Written informed consent was obtained
from the patient.
Patient consent for publication
Written consent to publication of clinical data and
images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bompas E, Campion L, Italiano A, Le Cesne
A, Chevreau C, Isambert N, Toulmonde M, Mir O, Ray-Coquard I,
Piperno-Neumann S, et al: Outcome of 449 adult patients with
rhabdomyosarcoma: An observational ambispective nationwide study.
Cancer Med. 7:4023–4035. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kaseb H, Kuhn J and Babiker HM:
Rhabdomyosarcoma. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing. 2022.
|
|
3
|
Wang T, Gao X, Yang J, Guo W, Wu Z, Tang
L, Cao S, Cai X, Liu T, Jia Q and Xiao J: Treatment strategies and
outcomes for spinal rhabdomyosarcoma: A series of 11 cases in a
single center and review of the literature. Clin Neurol Neurosurg.
192:1057292020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gurria JP and Dasgupta R: Rhabdomyosarcoma
and extraosseous ewing sarcoma. Children (Basel).
5:1652018.PubMed/NCBI
|
|
5
|
Raney RB, Maurer HM, Anderson JR, Andrassy
RJ, Donaldson SS, Qualman SJ, Wharam MD, Wiener ES and Crist WM:
The intergroup rhabdomyosarcoma study group (IRSG): Major lessons
from the IRS-I through IRS-IV studies as background for the current
IRS-V treatment protocols. Sarcoma. 5:9–15. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Spreafico F, Ferrari A, Mascarin M,
Collini P, Morosi C, Biasoni D, Biassoni V, Schiavello E, Gandola
L, Gattuso G, et al: Wilms tumor, medulloblastoma, and
rhabdomyosarcoma in adult patients: lessons learned from the
pediatric experience. Cancer Metastasis Rev. 38:683–694. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sultan I, Qaddoumi I, Yaser S,
Rodriguez-Galindo C and Ferrari A: Comparing adult and pediatric
rhabdomyosarcoma in the surveillance, epidemiology and end results
program, 1973 to 2005: An analysis of 2,600 patients. J Clin Oncol.
27:3391–3397. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wei F, Li Z, Liu Z, Liu X, Jiang L, Yu M,
Xu N, Wu F, Dang L, Zhou H, et al: Upper cervical spine
reconstruction using customized 3D-printed vertebral body in 9
patients with primary tumors involving C2. Ann Transl Med.
8:3322020. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Osborn VW, Lee A and Yamada Y:
Stereotactic body radiation therapy for spinal malignancies.
Technol Cancer Res Treat. 17:15330338188023042018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ladra MM, Szymonifka JD, Mahajan A,
Friedmann AM, Yong Yeap B, Goebel CP, MacDonald SM, Grosshans DR,
Rodriguez-Galindo C, Marcus KJ, et al: Preliminary results of a
phase II trial of proton radiotherapy for pediatric
rhabdomyosarcoma. J Clin Oncol. 32:3762–3770. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gong Y, Xu L, Zhuang H, Jiang L, Wei F,
Liu Z, Li Y, Yu M, Ni K and Liu X: Efficacy and safety of different
fractions in stereotactic body radiotherapy for spinal metastases:
A systematic review. Cancer Med. 8:6176–6184. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Arndt CA, Stoner JA, Hawkins DS, Rodeberg
DA, Hayes-Jordan AA, Paidas CN, Parham DM, Teot LA, Wharam MD,
Breneman JC, et al: Vincristine, actinomycin, and cyclophosphamide
compared with vincristine, actinomycin, and cyclophosphamide
alternating with vincristine, topotecan, and cyclophosphamide for
intermediate-risk rhabdomyosarcoma: Children's oncology group study
D9803. J Clin Oncol. 27:5182–5188. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Arndt CA, Hawkins DS, Meyer WH, Sencer SF,
Neglia JP and Anderson JR: Comparison of results of a pilot study
of alternating vincristine/doxorubicin/cyclophosphamide and
etoposide/ifosfamide with IRS-IV in intermediate risk
rhabdomyosarcoma: A report from the children's oncology group.
Pediatr Blood Cancer. 50:33–36. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Walterhouse DO, Pappo AS, Meza JL,
Breneman JC, Hayes-Jordan A, Parham DM, Cripe TP, Anderson JR,
Meyer WH and Hawkins DS: Reduction of cyclophosphamide dose for
patients with subset 2 low-risk rhabdomyosarcoma is associated with
an increased risk of recurrence: A report from the soft tissue
sarcoma committee of the children's oncology group. Cancer.
123:2368–2375. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dumont SN, Araujo DM, Munsell MF,
Salganick JA, Dumont AG, Raymond KA, Linassier C, Patel S, Benjamin
RS and Trent JC: Management and outcome of 239 adolescent and adult
rhabdomyosarcoma patients. Cancer Med. 2:553–563. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gupta AA, Anderson JR, Pappo AS, Spunt SL,
Dasgupta R, Indelicato DJ and Hawkins DS: Patterns of
chemotherapy-induced toxicities in younger children and adolescents
with rhabdomyosarcoma: A report from the children's oncology group
soft tissue sarcoma committee. Cancer. 118:1130–1137. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bisogno G, Jenney M, Bergeron C,
GallegoMelcón S, Ferrari A, Oberlin O, Carli M, Stevens M, Kelsey
A, De Paoli A, et al: Addition of dose-intensified doxorubicin to
standard chemotherapy for rhabdomyosarcoma (EpSSG RMS 2005): A
multicentre, open-label, randomised controlled, phase 3 trial.
Lancet Oncol. 19:1061–1071. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hawkins DS, Chi YY, Anderson JR, Tian J,
Arndt CAS, Bomgaars L, Donaldson SS, Hayes-Jordan A, Mascarenhas L,
McCarville MB, et al: Addition of vincristine and irinotecan to
vincristine, dactinomycin, and cyclophosphamide does not improve
outcome for intermediate-risk rhabdomyosarcoma: A report from the
children's oncology group. J Clin Oncol. 36:2770–2777. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hawkins DS, Gupta AA and Rudzinski ER:
What is new in the biology and treatment of pediatric
rhabdomyosarcoma? Curr Opin Pediatr. 26:50–56. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Weitao Y, Fangxing W, Qiqing C and
Jiaqiang W: Efficacy and safety of apatinib in advanced sarcoma: An
open-label, nonrandomized, single-center study of 45 patients.
Anticancer Drugs. 30:e07782019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van Erp AEM, Versleijen-Jonkers YMH, van
der Graaf WTA and Fleuren EDG: Targeted therapy-based combination
treatment in rhabdomyosarcoma. Mol Cancer Ther. 17:1365–1380. 2018.
View Article : Google Scholar : PubMed/NCBI
|