Introduction
Myelodysplastic syndrome (MDS) is a bone marrow (BM)
failure syndrome of hematopoietic stem cell disorder characterized
by ineffective hematopoiesis, blood cell dysplasia, and a high risk
of progression to acute myeloid leukemia (AML), especially in high
risk (HR) patients defined by the International Prognostic Scoring
System (IPSS) or the revised IPSS (IPSS-R) (1–4).
Although allogeneic stem cell transplantation (ASCT) is the only
curative treatment option for HR-MDS, most patients are ineligible
for ASCT because of their high age and comorbidities (1–5). A
hypomethylating agent azacitidine (AZA) has been one of the
standards of care for patients with ASCT-ineligible HR-MDS
(6) since the AZA-001 trial
demonstrated its superior efficacy to conventional care regimens of
physicians' choice in improving overall survival (OS) reaching 24.5
months as the median period (7).
With this regard, AZA showed the potential to induce hematological
improvement and delay leukemic evolution. However, the median OS in
patients with MDS treated with AZA seemed shorted in real-world
daily (RWD) practice around 10–17 months (8–10).
Moreover, patients received a median of 9 cycles of AZA in the
AZA-001 trial (7), while only 4–6
cycles in real-world practice (8–10).
Therefore, it is critically important to predict the treatment
outcome of patients with HR-MDS by AZA treatment in RWD practice
for treatment decision-making, i.e., who will and will not be
expected to benefit from AZA monotherapy.
The IPSS-R consisting of pre-treatment variables,
including blood cell counts, BM blast ratio, and cytogenetics, has
been widely utilized as the prognosis prediction model in various
treatment situations in MDS (11).
Many studies have also reported the adverse prognostic impact of
cytopenia before treatment initiation in MDS (11–15).
Moreover, AZA treatment potentially causes various types of adverse
events that hamper treatment continuation (10,16–17),
and, especially, hematologic toxicities frequently necessitate the
increase of blood transfusion, trigger severe infection, and even
result in the treatment cessation in the early phase of treatment
(18). Although several previous
studies have reported the influence of blood cell transition after
the initiation of hypomethylating agents (HMA) on response and
prognosis in patients with MDS (19–21),
the prognostic impact of hematologic toxicities in the early
clinical phase of AZA monotherapy has not been evaluated in
conjunction with pre-treatment prognostic factors commonly utilized
in the classical prognostic indices, such as IPSS-R.
To answer this question, we conducted a
multi-institutional retrospective analysis to investigate the
prognostic impact of cytopenia during the first cycle of AZA
monotherapy in conjunction with other classical prognostic factors.
In addition to the evaluation of neutropenia after the first cycle
of AZA monotherapy for 28 days, we evaluated the degree of anemia
and thrombocytopenia by the dose of blood transfusion required
during the first cycle as the surrogates of anemia and
thrombocytopenia, because the minimum levels of hemoglobin (Hb)
level and platelet counts are masked by blood transfusion, and,
therefore, are not considered to be suitable as biomarkers.
Materials and methods
Study design and patients
We retrospectively collected clinical and survival
data of 212 patients with MDS who started AZA monotherapy between
January 2012 and December 2021 and survived more than 29 days after
the start of AZA at seven institutes belonging to the Kyoto
Clinical Hematology Study Group (KOTOSG), i.e., Kyoto Prefectural
University of Medicine (Kyoto, Japan), Aiseikai Yamashina Hospital
(Kyoto, Japan), Japan Community Health Care Organization Kyoto
Kuramaguchi Medical Center (Kyoto, Japan), Fukuchiyama City
Hospital (Fukuchiyama, Japan), Japanese Red Cross Kyoto Daiichi
Hospital (Kyoto, Japan), Japanese Red Cross Kyoto Daini Hospital
(Kyoto, Japan) and Matsushita Memorial Hospital (Moriguchi, Japan).
Diagnosis of MDS and MDS subtypes were re-evaluated based on the
2016 World Health Organization (WHO) classification (22). This study included patients with
intermediate, high, or very high risk MDS according to the IPSS-R
(11), while excluded patients who
underwent ASCT. We evaluated the factors included in the IPSS-R,
i.e., karyotype, rate of BM blasts, Hb level, platelet counts,
absolute neutrophil counts (ANC), age at diagnosis, gender, ANC on
the 29th day after the initiation of AZA (ANC29), and the
transfusion units required within 28 days from the start of AZA
with red cell concentrates, designated here as RCC28, and platelet
concentrate (PC28). This study was conducted following the
Declaration of Helsinki and the ethical guidelines and approved by
The Ethics Committee of each institute that participated in the
study.
Treatment with AZA and blood
transfusion
All patients were treated with AZA monotherapy as
standard clinical treatment, administered subcutaneously or
intravenously at 75 mg/m2/day for seven days every 28
days. Dose reduction of AZA based on the patient's condition was
allowed at the discretion of each treating physician. RCC and PC
transfusions were performed at each treating physician's
discretion, along with the transfusion guidelines defined by the
Japanese Society of Transfusion Medicine and Cell Therapy, which
recommend that the trigger Hb level for RCC transfusion is 6–7 g/dl
and the trigger platelet counts for PC transfusion is
10×109/l (23,24). G-CSF was allowed at the discretion
of the attending physician.
Survival and statistical analysis
The conditional survival period after the first
cycle of AZA treatment (CS-AZA1) was defined as the time from the
29th day after the start of AZA to the date of death from any
cause. The conditional leukemia-free survival period after the
first cycle of AZA treatment (CLFS-AZA1) was defined as the time
from the 29th day after the start of AZA to the date of progression
to AML or death from any cause, whichever came first. CS-AZA1 and
CLFS-AZA1 were analyzed using the Kaplan-Meier method and compared
by log-rank test.
We randomly selected 70% of all patients as a
training set and the remaining 30% as a validation set. Severe
neutropenia was defined as ANC29 less than the first quartile. As
described, severe anemia and thrombocytopenia were surrogated by
the degree of transfusion dependency in this study, and severe
anemia and severe thrombocytopenia were defined by RCC28 and PC28
more than the third quartile. The relative dose intensity in the
first cycle of AZA treatment (RDI-AZA1) was defined by the ratio of
the dose administered in the first cycle of AZA divided by the
amount determined in the AZA-001 trial, i.e., 75 mg/m2
for seven days (7). Fisher's exact
test was used to compare categorical variables, and Mann-Whitney U
test or Kruskal-Wallis test was used to compare continuous
variables between two and more than two groups, respectively.
Steel-Dwass test was used as post hoc analysis after the
Kruskal-Wallis test. Because all continuous variables analyzed in
this study, i.e., BM blast ratio, Hb level, platelet counts, white
blood cell counts (WBC), ANC, age at diagnosis, RCC28, PC28, ANC29,
and RDI-AZA1 were not found to follow a normal distribution by the
Shapiro-Wilk test in the training set patients, the correlation
between the two variables was analyzed using Spearman's rank
correlation coefficient (25). The
univariate and multivariate analyses were performed by Cox
proportional hazards regression to identify significant independent
prognostic factors for CS-AZA1 and CLFS-AZA1. Elements with
P<0.1 in the univariate analysis were selected for evaluation in
the multivariate analysis. In addition, we tried to create a new
predictive model by combining independent prognostic factors
extracted in the training cohort and verified it in the validation
cohort. To evaluate the prognostic discriminatory ability of the
new prognostic prediction score, we evaluated Harrell's c-index,
which estimates the probability that out of two randomly selected
patients, the patient with a lower (better) prognostic score will
live longer than the patient with a higher (worse) prognostic score
(26,27). The P-values of <0.05 were
considered statistically significant. All statistical analyses were
performed with EZR version 1.61 (28).
Results
Patient characteristics
The training and the validation sets comprised 143
and 69 patients, respectively. There were no significant
differences in patients' characteristics between the training and
the validation sets (Table I). In
the training set, the median age of patients was 76 years old
(range 52–94), and 98 (68.5%) patients were male. According to the
IPSS-R, 75 patients (52.4%) were classified as very high-risk, 39
(27.3%) as high-risk, and 29 (20.3%) as intermediate-risk. Precise
data about RCC28, PC28, and ANC29 in the training set are shown in
Table II. As a result, the median
numbers of RCC28 and PC28 were four units and 0 units,
respectively, and the median number of ANC29 was
0.43×109/l. Severe anemia and severe thrombocytopenia
were determined to be more than six and 30 units, respectively.
Severe neutropenia was determined to be less than
0.18×109/l. G-CSF was administered in 10 patients,
including those with severe neutropenic patients with
infection.
 | Table I.Baseline characteristics, RCC and PC
units within 28 days from the start of AZA, and ANC on the 29th day
after the start of AZA of patients in the training and the
validation set. |
Table I.
Baseline characteristics, RCC and PC
units within 28 days from the start of AZA, and ANC on the 29th day
after the start of AZA of patients in the training and the
validation set.
|
Characteristics | Training set
(n=143) | Validation set
(n=69) | P-value |
|---|
| Age, years | 76 (52–94) | 73 (31–93) | 0.192 |
| Male/female, n
(%) | 98 (68.5)/45
(31.5) | 54 (78.3)/15
(21.7) | 0.148 |
| WHO 2016
classification, n (%) |
|
| 0.388 |
|
MDS-SLD | 2 (1.4) | 1 (1.4) |
|
|
MDS-MLD | 22 (15.4) | 17 (24.6) |
|
|
MDS-RS-SLD | 1 (0.7) | 1 (1.4) |
|
|
MDS-RS-MLD | 6 (4.2) | 2 (2.9) |
|
|
MDS-EB1 | 54 (37.8) | 17 (24.6) |
|
|
MDS-EB2 | 55 (38.5) | 28 (40.6) |
|
|
MDS-U | 3 (2.0) | 3 (4.3) |
|
| Hemoglobin level,
g/dl | 7.8 (3.5–13.0) | 7.5 (3.2–11.4) | 0.242 |
| Platelet counts,
×109/l | 68.0
(2.0–1139.0) | 50.0
(10.0–685.0) | 0.216 |
| WBC,
×109/l | 2.5 (0.8–24.4) | 2.4 (0.2–42.4) | 0.442 |
| ANC,
×109/l | 1.1 (0.0–19.6) | 1.2 (0.0–23.3) | 0.887 |
| Blast in bone
marrow, % | 7.4 (0.0–19.8) | 6.0 (0.0–18.8) | 0.700 |
| Cytogenetic risk
defined by IPSS-R, n (%) |
|
| 0.515 |
| Very
good | 2 (1.4) | 0 (0.0) |
|
|
Good | 34 (23.8) | 16 (23.2) |
|
|
Intermediate | 33 (23.1) | 16 (23.2) |
|
|
Poor | 15 (10.5) | 3 (4.3) |
|
| Very
poor | 59 (41.3) | 34 (49.3) |
|
| IPSS-R risk group,
n (%) |
|
| 0.107 |
|
Intermediate | 29 (20.3) | 7 (10.1) |
|
|
High | 39 (27.3) | 26 (37.7) |
|
| Very
high | 75 (52.4) | 36 (52.2) |
|
| RCC transfusion
units within 28 days from the start of AZA, days | 4 (0–30) | 4 (0–12) | 0.153 |
| PC transfusion
units within 28 days from the start of AZA, days | 0 (0–170) | 0 (0–120) | 0.682 |
| ANC on the 29th day
after the start of AZA, ×109/l | 0.4 (0.0–9.3) | 0.5 (0.0–9.8) | 0.793 |
 | Table II.RCC28, PC28, and ANC29 in the
training set. |
Table II.
RCC28, PC28, and ANC29 in the
training set.
| Variable | Minimum | 1st quartile | Median | 3rd quartile | Maximum |
|---|
| RCC28, unit | 0 | 0 | 4 | 6a | 30 |
| PC28, unit | 0 | 0 | 0 | 30a | 170 |
| ANC29,
×109/l | 0.02 | 0.18a | 0.43 | 1.32 | 9.31 |
Survival data and prognostic factors
for CS-AZA1 and CLFS-AZA1 in the training set
In the training set, with the median follow-up
period calculated from the 29th day after the start of the
first-cycle AZA was 11.7 months (range, 0.1–60.8), the median
CS-AZA1 was 13.9 months (95% confidence interval (CI), 11.5–17.1)
(Fig. 1A), and the median CLFS-AZA1
was 11.4 months (95% CI, 9.0–14.3) (Fig. 1B). Both CS-AZA1 and CLFS-AZA1 showed
significant differences in the stratification with IPSS-R-defined
groups. Namely, the median CS-AZA1 was 11.8 (95% CI, 9.5–15.4),
15.1 (95% CI, 7.7–23.6), and 21.9 (95% CI, 10.7–36.8) months
(P=0.003), in the very high-, high-, and intermediate-risk groups,
respectively (Fig. 1C), whereas the
median CLFS-AZA1 was 10.4 (95% CI, 7.9–11.9), 14.0 (95% CI,
7.5–18.7), and 16.0 (95% CI, 7.7–27.1) (P=0.007) (Fig. 1D), respectively. The median RDI-AZA1
in the training set was 90% (interquartile range (IQR), 66–97), and
we determined the cutoff of RDI-AZA1 was set to 90%. RDI-AZA1 had
no prognostic impact on either CS-AZA1 or CLFS-AZA1 (Fig. 1E, F).
The univariate analysis for CS-AZA1 found that the
male gender, the very poor cytogenetic risk, the low Hb level of
<8.0 g/dl at diagnosis, the low platelet counts of
<50×109/l at diagnosis, the low ANC of
<0.8×109/l at diagnosis, severe anemia defined by
RCC28, and severe thrombocytopenia defined by PC28, and severe
neutropenia defined by ANC29 were associated with short CS-AZA1
(Table III). Then, the
multivariate analysis for CS-AZA1 identified that the very poor
risk cytogenetics (HR, 2.18; 95% CI, 1.42–3.33; P<0.001) and
severe thrombocytopenia defined by the more than 30 units of PC28
(HR, 2.90; 95% CI, 1.56–5.37; P<0.001) were independent poor
prognostic factors (Table III).
The multivariate analysis for CLFS-AZA1 also showed that the very
poor risk cytogenetics (HR, 1.80; 95% CI, 1.20–2.71; P=0.004) and
severe thrombocytopenia defined by the more than 30 units of PC28
(HR, 2.05; 95% CI, 1.13–3.73; P=0.018) were independent poor
prognostic factors (Table
III).
 | Table III.Uni- and multivariate analyses for
CS-AZA1 and CLFS-AZA1. |
Table III.
Uni- and multivariate analyses for
CS-AZA1 and CLFS-AZA1.
|
|
| CS-AZA1 | CLFS-AZA1 |
|---|
|
|
|
|
|
|---|
|
|
| Univariate
analysis | Multivariate
analysis | Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|
|
|---|
| Factors | Variables | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| Age | <75 | Reference |
|
|
|
|
| Reference |
|
|
|
|
|
|
| ≥75 | 1.10 | 0.76–1.62 | 0.609 |
|
|
| 1.26 | 0.87–1.83 | 0.214 |
|
|
|
| Sex | Female | Reference |
|
| Reference |
|
| Reference |
|
|
|
|
|
|
| Male | 1.42 | 0.94–2.13 | 0.095 | 1.45 | 0.98–2.29 | 0.062 | 1.26 | 0.85–1.86 | 0.255 |
|
|
|
| Cytogenetic | Very good,
good, | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
| risk according | intermediate, |
|
|
|
|
|
|
|
|
|
|
|
|
| to IPSS-R | and poor |
|
|
|
|
|
|
|
|
|
|
|
|
| classification | Very poor | 2.12 | 1.44–3.13 | <0.001 | 2.18 | 1.42–3.33 | <0.001 | 1.80 | 1.24–2.61 | 0.002 | 1.80 | 1.20–2.71 | 0.004 |
| Blast in bone | <10% | Reference |
|
|
|
|
| Reference |
|
|
|
|
|
| marrow | ≥10% | 0.94 | 0.63–1.41 | 0.782 |
|
|
| 1.06 | 0.72–1.56 | 0.764 |
|
|
|
| Hemoglobin | ≥8 g/dl | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
| level | <8 g/dl | 1.42 | 0.97–2.08 | 0.070 | 1.33 | 0.88–1.99 | 0.175 | 1.49 | 1.03–2.15 | 0.034 | 1.39 | 0.94–2.06 | 0.098 |
| Platelet
counts |
≥50×109/l | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
|
|
<50×109/l | 1.60 | 1.08–2.36 | 0.018 | 0.73 | 0.44–1.22 | 0.227 | 1.47 | 1.01–2.15 | 0.047 | 0.89 | 0.56–1.43 | 0.639 |
| ANC |
≥0.8×109/l | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
|
|
<0.8×109/l | 1.55 | 1.05–2.29 | 0.028 | 1.40 | 0.89–2.22 | 0.146 | 1,40 | 0.95–2.05 | 0.088 | 1.23 | 0.78–1.91 | 0.372 |
| RCC28 | ≤6 units | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
|
| >6 units | 2.98 | 1.89–4.70 | <0.001 | 1.57 | 0.90–2.73 | 0.114 | 2.60 | 1.66–4.09 | <0.001 | 1.50 | 0.87–2.61 | 0.148 |
| PC28 | ≤30
units/month | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
|
| >30
units/month | 2.74 | 1.68–4.47 | <0.001 | 2.90 | 1.56–5.37 | <0.001 | 2.36 | 1.45–3.83 | 0.001 | 2.05 | 1.13–3.73 | 0.018 |
| ANC29 |
≥0.18×109/l | Reference |
|
| Reference |
|
| Reference |
|
| Reference |
|
|
|
|
<0.18×109/l | 1.71 | 1.11–2.64 | 0.016 | 1.09 | 0.65–1.83 | 0.739 | 1.58 | 1.04–2.46 | 0.032 | 1.13 | 0.68–1.87 | 0.643 |
Characteristics and outcomes of
patients with severe thrombocytopenia defined by PC28
We next analyzed the correlation between PC28 and
other variables, characteristics, and treatment outcomes of
patients with severe thrombocytopenia defined by more than 30 units
of PC28 in the training set. We investigated whether PC28
correlated with age, gender, Hb level, platelet counts, WBC, ANC,
blast ratio in bone marrow, cytogenetic risk, RCC28, ANC29, and
RDI-AZA1 by Spearman's rank correlation coefficient. Hb level
(r=−0.258, P=0.002), platelet counts (r=−0.623, P<0.001), RCC28
(r=0.583, P<0.001), and ANC29 (r=−0.281, P=0.001) had a
correlation with PC28, and other variables did not have a
correlation with PC28 (Table SI).
The baseline characteristics, RCC28, PC28, ANC29, and RDI-AZA1 of
patients with severe thrombocytopenia and those without severe
thrombocytopenia were summarized in Table IV. Patients with severe
thrombocytopenia had lower baseline Hb levels, lower baseline
platelet counts, higher RCC28, and lower ANC29. RDI-AZA1 in
patients with severe thrombocytopenia tended to be lower, although
not statistically significant. The median CS-AZA1 was 5.8 months
(95% CI, 2.5–13.1) in patients with severe thrombocytopenia and
15.4 months (95% CI, 11.8–18.1) in patients without severe
thrombocytopenia (P<0.001) (Fig.
2A). The median CLFS-AZA1 was 4.5 months (95% CI, 2.5–11.9) in
patients with severe thrombocytopenia and 12.3 months (95% CI,
10.4–15.1) in patients without severe thrombocytopenia (P<0.001)
(Fig. 2B). The cumulative incidence
of progression to AML was similar between patients with and without
severe thrombocytopenia (P=0.752) (Fig.
2C).
 | Table IV.Baseline clinical characteristics,
RCC28, PC28 and ANC29 of patients with/without severe
thrombocytopenia defined by >30 units of PC28. |
Table IV.
Baseline clinical characteristics,
RCC28, PC28 and ANC29 of patients with/without severe
thrombocytopenia defined by >30 units of PC28.
| Variable | No severe
thrombocytopenia (n=115) | Severe
thrombocytopenia (n=28) | P-value |
|---|
| Age, years | 76 (52–94) | 74 (52–90) | 0.178 |
| Male/Female, n
(%) | 79 (68.7)/36
(31.3) | 19 (67.9)/9
(32.1) | 1.000 |
| Hemoglobin level,
g/dl | 8.1 (3.5–13.0) | 7.0 (5.5–10.2) | 0.004 |
| Platelet counts,
×109/l | 76.0
(14.0–1139.0) | 24.5
(2.0–270.0) | <0.001 |
| WBC,
×109/l | 2.5 (0.8–19.0) | 2.2 (0.8–24.4) | 0.344 |
| ANC,
×109/l | 1.1 (0.0–13.1) | 0.9 (0.1–19.6) | 0.692 |
| Blast in bone
marrow, % | 6.8 (0.4–19.8) | 8.3 (0.3–18.4) | 0.557 |
| Cytogenetic risk
according to IPSS-R, n (%) |
|
| 0.598 |
| Very
good | 2 (1.7) | 0 (0.0) |
|
|
Good | 25 (21.7) | 9 (32.1) |
|
|
Intermediate | 27 (23.5) | 6 (21.4) |
|
|
Poor | 14 (12.2) | 1 (3.6) |
|
| Very
poor | 47 (40.9) | 12 (42.9) |
|
| RCC28,
units/month | 2 (0–14) | 8 (0–30) | <0.001 |
| PC28,
units/month | 0 (0–30) | 60 (35–170) | <0.001 |
| ANC29,
×109/l | 0.5 (0.0–9.0) | 0.3 (0.0–9.3) | 0.039 |
| RDI-AZA1, % | 91 (68–97) | 81 (62–95) | 0.059 |
Since severe thrombocytopenia defined by PC28 was
significantly worse in the CS-AZA1 but was not linked to the
cumulative incidence of progression to AML, we compared the causes
of death. In twenty-two patients with severe thrombocytopenia died
within the follow-up period, the causatives of death were AML in 10
(45.5%), infection in 5 (22.7%), hemorrhagic event in 1 (4.5%), and
other disease in 1 (4.5%), and unknown in 5 patients (22.7%)
(Fig. 2D). In eighty-seven patients
without severe thrombocytopenia died within the follow-up period,
the causatives of death were AML in 46 (52.9%), infection in 19
(21.8%), hemorrhagic event in 3 (3.4%), other malignancy in 1
(1.1%), other diseases in 2 (2.3%), and unknown in 16 patients
(18.4%) (Fig. 2E). Thus, the
causatives of death were not significantly different between
patients with severe thrombocytopenia and those without
(P=0.862).
Establishment of a new prognostic
model for CS-AZA1 and CLFS-AZA1
Because most of the variables utilized in IPSS-R,
except cytogenetics, were not shown to have prognostic impacts on
CS-AZA1 and CLFS-AZA1 in our cohort, we next tried to develop a new
prognostic model, here designated as the Kyoto Conditional Survival
Scoring System (KCSS), for patients with MDS treated by AZA
monotherapy, by incorporating the very poor risk cytogenetics
according to the IPSS-R and severe thrombocytopenia defined by more
than 30 units of PC28 as prognostic variables. We classified
patients into three risk groups by the number of risk factors,
i.e., the good-risk group without any risk factor, the
intermediate-risk group with one risk factor, and the poor-risk
group with two risk factors.
The baseline characteristics, RCC28, PC28, ANC29,
and RDI-AZA1 of patients in the training set according to the risk
groups by the KCSS were summarized in Table V. There were significant differences
in platelet counts at diagnosis, RCC28, and ANC29, in addition to
IPSS-R-defined cytogenetic features and PC28, among different risk
groups. When analyzing the relationship between the disease risks
evaluated by IPSS-R and KCSS, the good-risk group by KCSS consisted
of 36.8, 41.2, and 22.1% of the intermediate-, high-, and very
high-risk patients according to the IPSS-R, respectively. The
KCSS-defined intermediate-risk group consisted of 6.3, 15.9, and
77.8% of intermediate-, high-, and very high-risk patients,
according to the IPSS-R. The poor-risk group defined by KCSS
consisted of 8.3 and 91.7% of high- and very high-risk patients,
according to the IPSS-R (Fig.
3A).
 | Table V.Baseline characteristics, RCC28,
PC28, ANC29 and RDI-AZA1 according to the risk group defined by
KCSS in the training set. |
Table V.
Baseline characteristics, RCC28,
PC28, ANC29 and RDI-AZA1 according to the risk group defined by
KCSS in the training set.
| Parameter | Good-risk group
(n=68) | Intermediate-risk
group (n=63) | Poor-risk group
(n=12) | P-value |
|---|
| Age, years | 76 (56–94) | 76 (52–90) | 68 (52–84) | 0.079 |
| Male/Female, n
(%) | 45 (66.2)/23
(33.8) | 47 (74.6)/16
(25.4) | 6 (50.0)/6
(50.0) | 0.206 |
| Hemoglobin level,
g/dl | 8.1 (5.7–13.0) | 7.7 (3.5–11.2) | 7.3 (6.1–10.0) | 0.174 |
| Platelet counts,
×109/l | 88.5
(17.0–1139.0) | 46.0
(3.0–470.0) | 23.5
(2.0–270.0) | <0.001 |
| WBC,
×109/l | 2.6 (0.8–19.0) | 2.4 (1.0–24.4) | 2.4 (0.8–22.1) | 0.888 |
| ANC,
×109/l | 1.1 (0.0–13.1) | 1.0 (0.1–10.6) | 0.8 (0.1–19.6) | 0.703 |
| Blast in bone
marrow, % | 7.8 (0.4–19.4) | 6.8 (0.0–19.8) | 8.0 (0.3–18.4) | 0.959 |
| Cytogenetic risk
according to IPSS-R, n (%) |
|
|
| <0.001 |
| Very good | 2 (2.9) | 0 (0.0) | 0 (0.0) |
|
| Good | 25 (36.8) | 9 (14.3) | 0 (0.0) |
|
| Intermediate | 27 (39.7) | 6 (9.5) | 0 (0.0) |
|
| Poor | 14 (20.6) | 1 (1.6) | 0 (0.0) |
|
| Very poor | 0 (0.0) | 47 (74.6) | 12 (100.0) |
|
| RCC28, unit | 2 (0–10) | 4 (0–24) | 8 (2–30) | <0.001 |
| PC28, unit | 0 (0–30) | 10 (0–170) | 60 (40–120) | <0.001 |
| ANC29,
×109/l | 0.7 (0.0–9.0) | 0.4 (0.0–9.3) | 0.2 (0.1–5.6) | 0.003 |
| RDI-AZA1, %, median
(IQR) | 90 (69–98) | 89 (63–96) | 92 (66–96) | 0.553 |
The CS-AZA1 and CLFS-AZA1 of the three risk groups
defined by KCCS were significantly different in the training set.
The median CS-AZA1 was 3.8 (95% CI, 0.9–9.3), 12.2 (95% CI,
9.5–15.4), 20.4 (95% CI, 15.1–25.9) months in patients with the
poor-risk group, intermediate-risk group, and good-risk group
defined by KCSS, respectively (P<0.001) (Fig. 3B), while the median CLFS-AZA1 were
3.6 (95% CI, 0.9–5.7), 11.2 (95% CI, 8.5–14.0), and 15.1 (95% CI,
10.5–20.4) months in patients with poor-risk group,
intermediate-risk group, and good-risk group defined by KCSS,
respectively (P<0.001) (Fig.
3C).
KCSS also successfully stratified the patients'
risks in CS-AZA1 and CLFS-AZA1 in the validation set. The median
CS-AZA1 was 3.2 (95% CI, 0.9–9.7), 10.0 (95% CI, 5.6–14.7), and
26.2 (95% CI, 13.7–37.7) months in patients with poor-risk group,
intermediate-risk group, and good-risk group defined by KCSS,
respectively (P<0.001) (Fig.
3D), and the median CLFS-AZA-1 was 2.8 (95% CI, 0.9–9.7), 7.9
(95% CI, 5.3–11.9), 16.5 (95% CI, 8.0–21.2) months in patients with
poor-risk group, intermediate-risk group, and good-risk group
defined by KCSS, respectively (P<0.001) (Fig. 3E).
Assessing the predictive value and
treatment cycles of KCSS
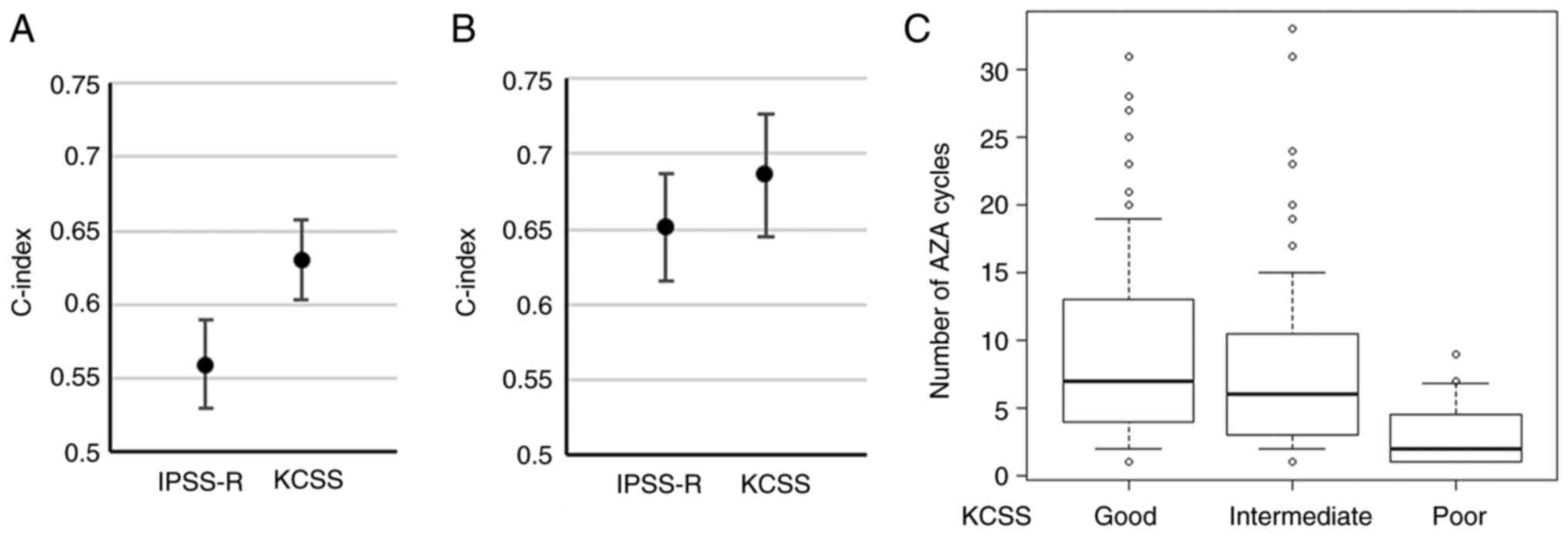
To evaluate the predictive value of KCSS, we
evaluated the c-index of KCSS and the treatment cycles of each risk
group concerning the comparison with IPSS-R. In the training set,
c-indices for CS-AZA1 of IPSS-R and KCSS were 0.559 (standard error
(SE), 0.030) and 0.630 (SE, 0.027), respectively (Fig. 4A). In the validation set, c-indices
for CS-AZA1 of IPSS-R and KCSS were 0.651 (SE, 0.036) and 0.686
(SE, 0.041), respectively (Fig.
4B). Finally, we analyzed the cycle numbers of AZA treatment in
the entire cohort. The median cycle number of AZA in the whole
cohort was 6 (interquartile range (IQR), 3–11) cycles. According to
IPSS-R, the median cycle numbers of AZA were 6 (IQR, 3–10), 6 (IQR,
4–11), and 6 (IQR, 3–11) in the very high-, high-,
intermediate-risk groups, respectively (P=0.372). According to
KCSS, the median cycle numbers of AZA were 2 (IQR, 1–5), 6 (IQR,
3–11), and 7 (IQR, 4–13) in patients with the poor-risk group,
intermediate-risk group, and good-risk group, respectively
(P<0.001), thus, were significantly different among risk groups
(Fig. 4C). In post hoc analysis,
the number of AZA cycles of poor-risk patients was lower than that
of intermediate-(P<0.001) and good-risk (P<0.001)
patients.
Discussion
Many studies have supported the adverse prognostic
impact of cytopenia before treatment initiation in MDS (11–15).
Although AZA improved the prognosis of patients with HR-MDS,
cytopenia after starting AZA often hampers treatment continuation,
resulting in severe infection and intolerance (10,16–17).
Moreover, it has been reported that cytopenia after starting AZA is
particularly severe in the first cycle (18). Although several previous studies
have reported the influence of blood cell transition after
initiating HMA on response and prognosis in patients with MDS
(19–21), the prognostic impact of severe
cytopenia in the early phase of treatment has not been evaluated.
Therefore, we in this study retrospectively investigated the
prognostic significance of severe cytopenia occurring during the
first cycle of AZA monotherapy in the setting of real-world
practice.
This study showed that the very poor risk
cytogenetics according to the IPSS-R and the higher requirements of
PLT transfusion units during the first AZA cycle (PC28) had
independent adverse prognostic impacts in patients with MDS treated
by AZA monotherapy. In contrast, the IPSS-R factors other than
cytogenetics, i.e., blast ratio in BM, Hb level, platelet counts,
and ANC before AZA treatment, were not significantly associated
with CS-AZA1 and CLFS-AZA1. This provoked us to develop a new
prognostic model of KCSS consisting of two independent prognostic
factors described above, and, importantly, KCSS successfully
discriminated risk groups in CS-AZA1 and CLFS-AZA1 in our cohort.
Considering that the pre-treatment findings define IPSS-R, while
KCSS utilizes the post-treatment information, comparing the
predictive values of IPSS-R and KCSS is unreasonable. However, our
study highlighted the prognostic significance of hematologic status
during the first cycle of AZA in MDS.
In previous studies, hematologic recovery after
starting HMA in MDS patients has been reported to be associated
with treatment outcomes. Lieke et al. and Ping et al showed
that platelet count changes after HMA initiation correlate with
prognosis (19,20). Nathan et al. created a machine
learning model to predict favorable treatment responses in 424 MDS
patients treated with AZA for over four months. They found that the
post-treatment response of Hb level and platelet counts was crucial
in predicting treatment outcomes (21). Our study demonstrated that the
number of transfusions representing platelet changes was related to
prognosis, which validates these previous findings. Unlike previous
studies that predicted a favorable prognosis in patients whose
platelet counts increased after starting HMA (19,20) or
predicted the response rate based on blood cell changes after
starting HMA (21), our study has a
notable strength in identifying patients with a very inferior
prognosis as evidenced by the median survival of approximately four
months in the poor-risk group according to KCSS, which was not
included in previous studies.
It has been reported that 91% of the first responses
by AZA were achieved within six cycles in the AZA-001 trial
(29) and that responders obtained
a better prognosis (30,31). It has also been recommended to
continue AZA monotherapy for at least 4–6 cycles to assess
response, even in cases with progressive cytopenia after starting
AZA (32,33). However, this has not been easily
reproduced in real-world practice (8–10).
With this regard, it was intriguing that the treatment cycle was
more closely associated with KCSS than IPSS-R in our cohort.
Indeed, the median cycle of AZA was only two cycles in patients
judged as poor-risk by KCSS in our cohort, again reflecting the
difficulty of treatment continuation in this particular population.
Most of the poor-risk patients defined by KCSS had severe anemia
and neutropenia in addition to severe thrombocytopenia after the
initiation of AZA, and these might collectively make treatment
continuation difficult by causing various kinds of adverse
events.
KCSS showed superior abilities in discriminating
risk groups in CS-AZA1 and CLFS-AZA1 to IPSS-R in our cohort and
identified patients who did not benefit from AZA treatment and
could not continue AZA for a sufficient period. Approximately 50%
of patients had less than 90% of RDI-AZA1, and the RDI-AZA1 of the
oldest patient, a 93-year-old, was 75%. Patients with severe
thrombocytopenia defined by PC28 were found to have higher RCC28
and lower ANC29 despite a lower tendency in RDI-AZA1, which
suggested the difficulty of administrating full doses of AZA to
some patients, especially those with severe thrombocytopenia, in
clinical practice. Although a previous study showed that reducing
the dosage of AZA before achieving the objective response was
associated with poor prognosis and that dose reduction of AZA
should be decided with caution (34), based on the results of this study,
the dose reduction of AZA in consideration of hematologic toxicity
is unavoidable in actual clinical practice. Considering the severe
hematologic toxicity of AZA in some patients, new therapeutic
agents may be needed to improve the prognosis of this group of
patients. For example, magrolimab, an anti-CD47 antibody (35), and sabatolimab, which inhibits
T-cell immunoglobulin and mucin domain 3 (36), are expected to be new therapeutic
agents for MDS.
This study had several limitations. First, there was
the possibility that the threshold for transfusion varied among
attending physicians. However, most researchers belonging to KOTOSG
adhered to the established guidelines for RCC and PC transfusions
(23,24), and, therefore, we consider that the
bias was minimal. Second, genetic information about the patients
was not obtained. It is well recognized that genetic and epigenetic
mutations are closely linked to therapeutic response and prognosis
(37–43). Future studies should, therefore,
integrate the genetic information to establish a more accurate
predictive model. Third, due to the retrospective observational
design of this study, information regarding the cause of death was
often unknown. Therefore, we could not thoroughly analyze the
etiology underlying the poor prognosis of patients with severe
thrombocytopenia defined by PC28. Additionally, the prognostic
significance of performance status (PS) was not assessed in this
study due to the limited number of patients with a PS of >2
because most patients analyzed had a PS of 0 or 1 based on the
Eastern Cooperative Oncology Group criteria (44).
In conclusion, severe PC transfusion dependency
during the first cycle of AZA and very poor risk cytogenetics are
the critically important prognostic indicators in AZA monotherapy
for MDS, and KCSS may be a useful predictive prediction model of
CS-AZA1 and CLFS-AZA1.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YI, HO and JK designed the study. AM, YKK, SC, TF,
TT, YS, SM, HK, SKO, SF, DN, KH, HU, EK, NU and JK acquired and
provided data. YI and HO confirm the authenticity of all the raw
data and performed statistical analyses. YI, HO and JK wrote the
manuscript. JK supervised the study. All authors interpreted data
and read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by The Ethics Committee of
each institute that participated in the study. The Ethics Committee
of each institute waived the need to obtain documented informed
consent from the study subjects under the setting of an opt-out,
and we disclosed information about the study to the patients. The
name, location, and approval number of each institute participating
in this study are: Division of Hematology and Oncology, Department
of Medicine, Kyoto Prefectural University of Medicine (Kyoto,
Japan), approval no ERB-C-1335-1; Department of Hematology,
Aiseikai Yamashina Hospital (Kyoto, Japan), approval no. FY2016 No.
8.; Department of Hematology, Japan Community Health Care
Organization Kyoto Kuramaguchi Medical Center (Kyoto, Japan),
approval no. 2023022101; Department of Hematology, Fukuchiyama City
Hospital (Kyoto, Japan), approval no. 4-18; Department of
Hematology, Japanese Red Cross Kyoto Daiichi Hospital (Kyoto,
Japan), approval no. 1490; Department of Hematology, Japanese Red
Cross Kyoto Daini Hospital (Kyoto, Japan), approval no. S2022-19;
Department of Hematology, Matsushita Memorial Hospital (Osaka,
Japan), approval no. 22014.
Patient consent for publication
The Ethics Committee of each institute waived the
need to obtain documented informed consent from the study subjects
under the setting of an opt-out, and we disclosed information about
the study to the patients.
Competing interests
TF has received honoraria from Takeda
Pharmaceutical; TT has received honoraria from Bristol Myers Squibb
(BMS), Janssen Pharmaceutical, Sanofi, Kyowa Kirin and Chugai
Pharmaceutical; YS has received honoraria from Ono Pharmaceutical,
BMS, Janssen Pharmaceutical, Sanofi, Kyowa Kirin, Takeda
Pharmaceutical and Chugai Pharmaceutical; SM has received honoraria
from Sanofi and Ono Pharmaceutical; and NU has received honoraria
from BMS and Takeda. JK is a consultant for Janssen Pharmaceutical,
Abbvie and BMS; has received research funding from Kyowa Kirin,
Chugai Pharmaceutical, Ono Pharmaceutical, Shionogi and BMS; and
has received honoraria from Janssen Pharmaceutical, Kyowa Kirin,
Chugai Pharmaceutical, Ono Pharmaceutical, Sanofi and BMS. None of
the pharmaceutical companies aforementioned benefited from the
present research or played any role in our study. All other authors
declare that they have no competing interests.
References
|
1
|
Fenaux P, Haase D, Santini V, Sanz GF,
Platzbecker U and Mey U: Myelodysplastic syndromes: ESMO clinical
practice guidelines for diagnosis, treatment, and follow-up. Ann
Oncol. 32:142–156. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sekeres MA and Cutler C: How we treat
higher-risk myelodysplastic syndromes. Blood. 123:829–836. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Aubrey BJ and Brunner AM: SOHO state of
the art and next questions: Treatment of higher-risk
myelodysplastic syndromes. Clin Lymphoma Myeloma Leuk. 22:869–877.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Adès L, Itzykson R and Fenaux P:
Myelodysplastic syndromes. Lancet. 383:2239–2252. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Neukirchen J, Schoonen WM, Strupp C,
Gattermann N, Aul C, Haas R and Germing U: Incidence and prevalence
of myelodysplastic syndromes: Data from the Düsseldorf
MDS-registry. Leuk Res. 35:1591–1596. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bewersdorf JP, Carraway H and Prebet T:
Emerging treatment options for patients with high-risk
myelodysplastic syndrome. Ther Adv Hematol.
11:20406207209550062020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fenaux P, Mufti GJ, Hellstrom-Lindberg E,
Santini V, Finelli C, Giagounidis A, Schoch R, Gattermann N, Sanz
G, List A, et al: Efficacy of azacitidine compared with that of
conventional care regimens in the treatment of higher-risk
myelodysplastic syndromes: A randomised, open-label, phase III
study. Lancet Oncol. 10:223–232. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zeidan AM, Sekeres MA, Garcia-Manero G,
Steensma DP, Zell K, Barnard J, Ali NA, Zimmerman C, Roboz G,
DeZern A, et al: Comparison of risk stratification tools in
predicting outcomes of patients with higher-risk myelodysplastic
syndromes treated with azanucleosides. Leukemia. 30:649–657. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bernal T, Martínez-Camblor P,
Sánchez-García J, de Paz R, Luño E, Nomdedeu B, Ardanaz MT, Pedro
C, Amigo ML, Xicoy B, et al: Effectiveness of azacitidine in
unselected high-risk myelodysplastic syndromes: Results from the
Spanish registry. Leukemia. 29:1875–1881. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zeidan AM, Hu X, Zhu W, Stahl M, Wang R,
Huntington SF, Giri S, Bewersdorf JP, Podoltsev NA, Gore SD, et al:
Association of provider experience and clinical outcomes in
patients with myelodysplastic syndromes receiving hypomethylating
agents. Leuk Lymphoma. 61:397–408. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Greenberg PL, Tuechler H, Schanz J, Sanz
G, Garcia-Manero G, Solé F, Bennett JM, Bowen D, Fenaux P, Dreyfus
F, et al: Revised international prognostic scoring system for
myelodysplastic syndromes. Blood. 120:2454–2465. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Greenberg P, Cox C, LeBeau MM, Fenaux P,
Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, et al:
International scoring system for evaluating prognosis in
myelodysplastic syndromes. Blood. 89:2079–2088. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kantarjian H, O'Brien S, Ravandi F, Cortes
J, Shan J, Bennett JM, List A, Fenaux P, Sanz G, Issa JP, et al:
Proposal for a new risk model in myelodysplastic syndrome that
accounts for events not considered in the original international
prognostic scoring system. Cancer. 113:1351–1361. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mozessohn L, Cheung MC, Fallahpour S, Gill
T, Maloul A, Zhang L, Lau O and Buckstein R: Azacitidine in the
‘real-world’: An evaluation of 1101 higher-risk myelodysplastic
syndrome/low blast count acute myeloid leukaemia patients in
Ontario, Canada. Br J Haematol. 181:803–815. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Diamantopoulos PT and Viniou NA: Factors
affecting response to 5-azacytidine and prognosis of
myelodysplastic syndrome. Is long-term survival a realistic goal?
Leuk Res. 103:1065432021.PubMed/NCBI
|
|
16
|
Diamantopoulos PT, Symeonidis A, Pappa V,
Kotsianidis I, Galanopoulos A, Pontikoglou C, Anagnostopoulos A,
Vassilopoulos G, Zikos P, Hatzimichael E, et al: The effect of
5-azacytidine treatment delays and dose reductions on the prognosis
of patients with myelodysplastic syndrome: How to optimize
treatment results and outcomes. Br J Haematol. 192:978–987. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Derissen EJB, Beijnen JH and Schellens
JHM: Concise drug review: Azacitidine and decitabine. Oncologist.
18:619–624. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Uchida T, Ogawa Y, Kobayashi Y, Ishikawa
T, Ohashi H, Hata T, Usui N, Taniwaki M, Ohnishi K, Akiyama H, et
al: Phase I and II study of azacitidine in Japanese patients with
myelodysplastic syndromes. Cancer Sci. 102:1680–1686. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
van der Helm LH, Alhan C, Wijermans PW,
van Marwijk Kooy M, Schaafsma R, Biemond BJ, Beeker A, Hoogendoorn
M, van Rees BP, de Weerdt O, et al: Platelet doubling after the
first azacitidine cycle is a promising predictor for response in
myelodysplastic syndromes (MDS), chronic myelomonocytic leukaemia
(CMML) and acute myeloid leukaemia (AML) patients in the Dutch
azacitidine compassionate named patient programme. Br J Haematol.
155:599–606. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lu PF, Deng LN, Meng FK, Wang Y, Xiao M
and Li DJ: platelet doubling after first decitabine cycle predicts
response and survival of myelodysplastic syndrome patients. Curr
Med Sci. 42:77–84. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Radakovich N, Sallman DA, Buckstein R,
Brunner A, Dezern A, Mukerjee S, Komrokji R, Al-Ali N, Shreve J,
Rouphail Y, et al: A machine learning model of response to
hypomethylating agents in myelodysplastic syndromes. IScience.
25:1049312022. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Arber DA, Orazi A, Hasserjian R, Thiele J,
Borowitz MJ, Beau MM, Bloomfield CD, Cazzola M and Vardiman JW: The
2016 revision to the World Health Organization classification of
myeloid neoplasms and acute leukemia. Blood. 127:2391–2405. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yonemura Y, Matsumoto M, Inada E, Ueda Y,
Ohishi K, Kubo T, Kumakawa M, Sueoka E, Sonoki T, Nagai K, et al:
Guideline for the use of red blood cell products based on
scientific evidence (Revision 2nd edition). Jpn J Transf Cell Ther.
64:688–699. 2018.(In Japanese).
|
|
24
|
Takami A, Matsushita T, Ogata M, Fujii N,
Kubuki Y, Fujiwara S, Matsumoto M and Tomiyama Y: Guideline for the
use of platelet transfusion concentrates based on scientific
evidence: Update 2019. Jpn J Transf Cell Ther. 65:544–561. 2019.(In
Japanese).
|
|
25
|
Schober P, Boer C and Schwarte LA:
Correlation coefficients: Appropriate use and interpretation.
Anesth Analg. 126:1763–1768. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Harrell FE Jr, Califf RM, Pryor DB, Lee KL
and Rosati RA: Evaluating the yield of medical tests. JAMA.
247:2543–2546. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Harrell FE Jr, Lee KL and Mark DB:
Multivariable prognostic models: Issues in developing models,
evaluating assumptions and adequacy, and measuring and reducing
errors. Stat Med. 15:361–387. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kanda Y: Investigation of the freely
available easy-to-use software ‘EZR’ for medical statistics. Bone
Marrow Transplant. 48:452–458. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Silverman LR, Fenaux P, Mufti GJ, Santini
V, Hellström-Lindberg E, Gattermann N, Sanz G, List AF, Gore SD and
Seymour JF: Continued azacitidine therapy beyond time of first
response improves quality of response in patients with higher-risk
myelodysplastic syndromes. Cancer. 117:2697–2702. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Gore SD, Fenaux P, Santini V, Bennett JM,
Silverman LR, Seymour JF, Hellström-Lindberg E, Swern AS, Beach CL
and List AF: A multivariate analysis of the relationship between
response and survival among patients with higher-risk
myelodysplastic syndromes treated within azacitidine or
conventional care regimens in the randomized AZA-001 trial.
Haematologica. 98:1067–1072. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Diamantopoulos PT, Pappa V, Symeonidis A,
Kotsianidis I, Galanopoulos A, Papadaki H, Anagnostopoulos A,
Vassilopoulos G, Zikos P, Hatzimichael E, et al: Characteristics of
Long-term survival in patients with myelodysplastic syndrome
treated with 5-Azacyditine: Results From the Hellenic 5-Azacytidine
registry. Clin Lymphoma Myeloma Leuk. 20:114–121. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Greenberg PL, Stone RM, Al-Kali A, Bennett
JM, Borate U, Brunner AM, Chai-Ho W, Curtin P, de Castro CM, Deeg
HJ and DeZem AE: NCCN Guidelines® Insights:
Myelodysplastic Syndromes, Version 3.2022. Featured Updates to the
NCCN Guidelines. J Natl Compr Canc Netw. 20:106–117. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Palacios-Berraquero ML and Alfonso-Piérola
A: Current therapy of the patients with MDS: Walking towards
personalized therapy. J Clin Med. 10:21072021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Laribi K, Bolle D, Alani M, Ghnaya H,
Besançon A, Farhi J, Mheidly K, Denizon N and de Materre AB: Impact
of the relative dose intensity on survival of patients with
high-risk myelodysplastic syndromes treated with Azacitidine.
Cancer Med. 8:2188–2195. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Eladl E, Tremblay-LeMay R, Rastgoo N,
Musani R, Chen W, Liu A and Chang H: Role of CD47 in hematological
malignancies. J Hematol Oncol. 13:962020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zeidan AM, Komrokji RS and Brunner AM:
TIM-3 pathway dysregulation and targeting in cancer. Expert Rev
Anticancer Ther. 21:523–534. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Bersanelli M, Travaglino E, Meggendorfer
M, Matteuzzi T, Sala C, Mosca E, Chiereghin C, Nanni ND, Gnocchi M,
Zampini M, et al: Classification and Personalized prognostic
assessment on the basis of clinical and genomic features in
Myelodysplastic Syndromes. J Clin Oncol. 39:1223–1233. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Nazha A, Komrokji R, Meggendorfer M, Jia
X, Radakovich N, Shreve J, Hilton CB, Nagata Y, Hamilton BK,
Mukherjee S, et al: Personalized prediction model to risk stratify
patients with Myelodysplastic Syndromes. J Clin Oncol.
39:3737–3746. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Liu YC, Kwon J, Fabiani E, Xiao Z, Liu YV,
Follo MY, Liu J, Huang H, Gao C, Liu J, et al: Demethylation and
up-regulation of an oncogene after Hypomethylating therapy. N Engl
J Med. 386:1998–2010. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Papaemmanuil E, Gerstung M, Malcovati L,
Tauro S, Gundem G, Van Loo P, Yoon CJ, Ellis P, Wedge DC,
Pellagatti A, et al: Clinical and biological implications of driver
mutations in myelodysplastic syndromes. Blood. 122:3616–3627. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Haferlach T, Nagata Y, Grossmann V, Okuno
Y, Bacher U, Nagae G, Schnittger S, Sanada M, Kon A, Alpermann T,
et al: Landscape of genetic lesions in 944 patients with
myelodysplastic syndromes. Leukemia. 28:241–247. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bejar R, Stevenson K, Abdel-Wahab O,
Galili N, Nilsson B, Garcia-Manero G, Kantarjian H, Raza A, Levine
RL, Neuberg D and Ebert BL: Clinical effect of point mutations in
myelodysplastic syndromes. N Engl J Med. 364:2496–2506. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yoshida K, Sanada M, Shiraishi Y, Nowak D,
Nagata Y, Yamamoto R, Sato Y, Sato-Otsubo A, Kon A, Nagasaki M, et
al: Frequent pathway mutations of splicing machinery in
myelodysplasia. Nature. 478:64–69. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern cooperative oncology group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|