Introduction
Carbonic anhydrases (CA) are a family of zinc
metallo-enzymes that participate in the regulation of pH,
CO2 and HCO3− transport as well as
the water and electrolyte balance (1). The membrane associated glycoprotein
carbonic anhydrase 9 (CAIX) has the highest catalytic activity
among the members of the family (2) and catalyzes the reversible hydration
of carbon dioxide into carbonic acid. CAIX consists of four
domains, the N-terminal proteoglycan domain, the catalytic domain
exposed to the extracellular milieu, a transmembrane anchor, and a
short cytoplasmic tail (3).
Expression of CAIX is elicited under hypoxic conditions by hypoxia
inducible factor-1 (HIF-1α) (4).
Overexpression of CAIX is associated with tumor cell hypoxia in a
variety of human tumors (5),
including breast (6), bladder
(7), head and neck carcinomas
(8), esophageal and gastric
adenocarcinomas (9) and carcinomas
of the lung (10).
A number of clinical and preclinical studies
(11) have demonstrated a
correlation between CAIX expression in tumors and resistance to
chemotherapy and radiotherapy as well as increased potential for
metastasis and poor cancer prognosis (12,13).
Thus, identification of hypoxic regions within the tumors will aid
the stratification of patients that may benefit from alternative
treatment approaches for hypoxic tumors, such as use of
radiosensitizers (14),
hyperthermia (15), or
hypoxia-selective cytotoxins (16). This identification requires
availability of hypoxia detection assays.
Measurement of tumor hypoxia is feasible using both
traditional oxygenation measurements that are based on
oxygen-sensitive electrodes, and by imaging using positron emission
tomography (PET), and single photon emission computed tomography
(SPECT). The in vivo oxygenation measurement methodologies
are clinically less attractive due to their invasiveness and
accessibility limitations (17).
Therefore, development of non-invasive approaches for imaging of
regional tumor tissue hypoxia remains to be of interest. The
limited normal tissue expression of CAIX (epithelia of the stomach,
small intestine and gall bladder) (5) makes it an attractive target for
molecular imaging, which would allow both identification of hypoxic
tumors and predicting treatment outcome.
Currently, radiolabeled nitro-imidazole compounds
have found a clinical application for imaging of hypoxia (18). In hypoxic cells, nitro-imidazole
compounds are reduced by intracellular reductases into highly
reactive intermediates, which subsequently bind to thiol groups of
intracellular proteins, resulting in accumulation inside hypoxic
cells (19). Multiple studies have
been performed to improve in vivo stability of substrates
with nitro-groups against enzymatic cleavage for visualization of
tumor hypoxia using both SPECT (20) and PET (21). Among these hypoxia imaging agents
are the fluoromisonidazole (18F-FMISO) (22) and the recently designed
18FHX4 with improved pharmacokinetic and clearance
properties (23). A major
challenge in development of nitro-imidazole-based imaging agents
for hypoxia is the need to penetrate inside malignant cells, which
requires sufficiently high lipophilicity of a tracer. A high
lipophilicity slows down elimination of an unbound tracer from
normal tissues, which reduces tumor to normal tissue ratio of
radioactivity concentration (18).
Therefore, the use of an extracellular hypoxia-associated molecular
abnormality would be desirable.
Presence of the extracellular domain of CAIX makes
it a potential target for specific molecular detection approaches
using targeting proteins. Currently, CAIX is used clinically as a
diagnostic target for antibodies with implications for both therapy
and patient outcome (24).
Monoclonal antibodies with high affinity, such as chimeric G250 and
M75 have already been generated and tested for this purpose. Among
these, M75 is useful for western blotting, immunoprecipitation, and
immunohistochemistry (25) whereas
the anti-CAIX antibody cG250 was mostly studied for imaging of
renal clear cell carcinoma (RCC) (26). It has demonstrated also an obvious
potential for in vivo imaging of hypoxia with high tumor
specificity. A considerable effort has been made to explore its
potential for immunotherapy as well (27).
Hypoxic regions are, however, distant from blood
vessels (28), and an efficient
targeting agent must therefore have excellent tissue penetration
properties. Like any other monoclonal antibody, the cG250 has some
limitations due to its large size. In addition to the relatively
poor extravasation and tissue penetration, the long blood
circulation of cG250 necessitates several (4–7) days
interval between injection and imaging for obtaining optimal tumor
uptake and high contrast images (29). Recently, a number of studies for
development of targeting agents with smaller molecular weights,
e.g. engineered or enzymatically produced antibody fragments
(30–32) and peptides (33), have been performed to address this
problem. However, there is still room for improvement.
A new class of engineered small scaffold proteins,
Affibody molecules, may be an alternative tracer with favorable
properties for radionuclide molecular imaging (34). Affibody molecules are composed of a
3-helix cysteine-free bundle consisting of 58 amino acids (35). Randomization of 13 amino acids in
helices one and two displaces the native binding specificity and
creates a large library from which high affinity binders to
different proteinaceous targets are selected (35). Further affinity maturation permits
development of binders with picomolar affinity to different
cancer-associated molecular targets (36). The small size (7 kDa) of Affibody
molecules facilitates high rates of extravasation and tissue
penetration, and rapid blood clearance of unbound tracers, which
provides high contrast images a few hours after injection (37). Clinical data have demonstrated high
potential of Affibody molecules in molecular imaging (38,39).
The aim of the present study was to evaluate
feasibility of CAIX imaging in vivo using radiolabeled
Affibody molecules.
Materials and methods
General
Buffers, including 0.1 M phosphate-buffered saline
(PBS), pH 7.5, and 0.07 M sodium borate, pH 9.3, were prepared
using common methods from chemicals supplied by Merck (Darmstadt,
Germany). High-quality Milli-Q© water (resistance higher
than 18 MΩ/cm) was used for preparing solutions. IsoLink kits were
kindly provided by Covidien (Mansfield, MA, USA). 99mTc
was obtained as pertechnetate from an Ultra-TechneKow generator
(Covidien) by elution with sterile 0.9% NaCl.
125I-sodium iodide was purchased from Perkin-Elmer
(Waltham, MA, USA). Chloramine-T and sodium metabisulfite were from
Sigma-Aldrich (St. Louis, MO, USA). NAP-5 size exclusion columns
were purchased from GE Healthcare (Uppsala, Sweden). Cells used
during in vitro experiments were detached using trypsin-EDTA
solution (0.25% trypsin, 0.02% EDTA in buffer; Biochrom AG
Biotechnologie, Berlin, Germany). For in vivo experiments,
Ketalar (50 mg/ml; Pfizer, Inc., New York, NY, USA), Rompun (20
mg/ml; Bayer, Leverkusen, Germany) and heparin (5,000 IE/ml; Leo
Pharma, Copenhagen, Denmark) were used.
Radioactivity was measured using an automated
gamma-counter with a ~7.6-cm (3-in) NaI(Tl) detector (1480 Wizard;
Wallac Oy, Turku, Finland). The yield and purity of radiolabeled
Affibody molecules was determined by radio-instant thin layer
chromatography (radio-ITLC) 150–771 Dark Green, (Tec-Control
Chromatography strips from Biodex Medical Systems, Inc., Shirley,
NY, USA). Sodium dodecyl sulfate polyacrylamide gel electrophoresis
(SDS-PAGE), 200 V constant using NuPAGE 4–12% Bis-Tris Gel
(Invitrogen AB, Lidingö, Sweden) in MES buffer (Invitrogen AB) was
used for cross-validation of stability results. The distribution of
radioactivity along the thin layer chromatography strips and
SDS-PAGE gels was measured on a Cyclone™ Storage Phosphor system
and analyzed using OptiQuant™ image analysis software
(Perkin-Elmer).
Data on cellular processing and biodistribution were
assessed by an unpaired, two-tailed t-test using the GraphPad Prism
(version 6.00 for Windows; GraphPad Software, San Diego, CA, USA)
in order to determine any significant differences (P<0.05).
Details on selection of CAIX-targeting Affibody
molecule ZCAIX:1 will be reported elsewhere. A
histidine-glutamate-histidine-glutamate-histidine-glutamate
(HE)3-tag (40) was
introduced at N terminus of ZCAIX:1 for site-specific labelling
with 99mTc.
Labeling and stability test of Affibody
molecules with [99mTc (CO)3]+ and
125I
Radiolabelling of (HE)3-ZCAIX:1 with
[99mTc(CO)3]+ was performed as
described earlier (40). Briefly,
400–500 μl (~3GBq) of
99mTcO4−-containing generator
eluate was added to a lyophilized IsoLink kit. The mixture was
incubated at 100°C for 30 min. Thereafter, 40 μl of mixture was
transferred to a vial containing 100 μg of Affibody molecule in 40
μl of PBS, followed by incubation at 50°C. After incubation for 60
and 120 min, 1 μl samples were taken for analysis of the
radiochemical labeling yields using radio-ITLC. When the ITLC
strips were eluted with PBS, pertechnetate, as well as carbonyl and
histidine complexes of 99mTc, migrated with the eluent
front (Rf=1.0), while Affibody molecules did not move
under these conditions (Rf=0.0).
The radio-labeled Affibody molecules were purified
using NAP-5 columns pre-equilibrated and eluted with PBS. The
purity of each preparation was evaluated using radio-ITLC.
Stability of the 99mTc-(HE)3-ZCAIX:1 was
tested using histidine challenge method in which paired samples of
the radio-labeled conjugate were incubated at 37°C with 500-fold
and 5,000-fold excess of histidine for 4 h. Control samples were
treated in the same way but incubated in PBS. Thereafter, the
samples were analyzed using ITLC as described above.
Indirect radio-iodination of
(HE)3-ZCAIX:1 using
N-succinimidyl-para-(trimethylstannyl)-benzoate was performed as
previously described (41).
Stability of the 125I-iodinated Affibody molecule was
tested using three different challenge methods: incubation in
presence of 2 M non-radioactive NaI to disrupt non-covalent
adhesion of radio-iodide with the protein, in presence of 30%
ethanol to disrupt hydrophobic interaction of iodobenzoic acid with
the protein, and in presence of a mixture of 2 M cold NaI and 30%
ethanol. Paired samples of radiolabeled conjugate were incubated at
room temperature with the test solution for 4 h.
Affinity determination using
LigandTracer
The kinetics of binding of
99mTc-(HE)3-ZCAIX:1 to living CAIX-expressing
SK-RC-52 renal carcinoma cells was measured at 4°C using
LigandTracer Yellow (Ridgeview Instruments, Vänge, Sweden)
according to the established method (42). The LigandTracer device records in
real-time kinetics of binding to and dissociation of radiolabeled
tracers from living cells. TraceDrawer software (Ridgeview
Instruments) permits to calculate both the association and
dissociation rates and, based on that, the affinity of radiolabeled
conjugates is determined. In order to cover the concentration span
needed for proper affinity estimation, three increasing
concentrations of 99mTc-(HE)3-ZCAIX:1 (30, 90
and 150 nM) were used in each affinity assay.
In vitro binding specificity and cellular
processing assays
Binding specificity and cellular processing studies
were performed using the renal clear cell carcinoma SK-RC-52 cell
line by methodology validated earlier for anti-HER2 Affibody
molecules (43).
To evaluate specificity,
99mTc-(HE)3-ZCAIX:1 (13 nM) was added to two
sets of Petri dishes containing a monolayer cell (~1×106
cells/dish). To one set of the Petri dishes, a 100-fold molar
excess of the unlabeled (HE)3-ZCAIX:1 was added ~15 min
before addition of the radiolabeled conjugate to saturate binding
sites. The cells were incubated in a humidified incubator (5%
CO2, 37°C) for 1 h. Thereafter, the medium was
collected, the cells were washed with cold serum-free medium and
then trypsin-EDTA solution was added and incubated for 10 min.
Detached cells were collected. The radioactivity of cells and media
was measured and the percent of cell-bound radioactivity was
calculated.
To evaluate cellular processing, SK-RC-52 cells were
incubated with 13 nM 99mTc-(HE)3-ZCAIX:1 at
37°C and 5% CO2. At designated time-points (1, 2, 4, 8
and 24 h), a group of three dishes was removed from the incubator,
the media was collected and cells were washed with ice cold
serum-free medium. Thereafter, cells were treated with 0.5 ml 0.2 M
glycine buffer, pH 2.0, containing 4 M urea, for 5 min on ice. The
acidic solution was collected and cells were additionally washed
with 0.5 ml of glycine buffer. The acidic fractions were pooled.
The cells were then incubated with 0.5 ml of 1 M NaOH at 37°C for
at least 20 min. The cell debris was collected and the dishes were
additionally washed with 0.5 ml of NaOH solution. The alkaline
fractions were pooled. The radioactivity in the acidic solution was
considered as membrane bound, and in the alkaline fractions as
internalized.
In vivo evaluation of
99mTc-(HE)3-ZCAIX:1 and
125I-(HE)3-ZCAIX:1
Animal experiments have been performed according to
national legislation on laboratory animal protection and were
approved by the Ethics Committee for Animal Research of the Uppsala
University (Permit Number: 48/11). Euthanasia was performed under
Rompun/Ketalar anesthesia, and all efforts were made to minimize
suffering.
Biodistribution studies were performed in female
NMRI nu/nu mice. Two weeks before the study, 10×106
SK-RC-52 cells were implanted in right hind leg of NMRI nu/nu mice.
Average tumor weight was 0.30±0.14 g at the time of the experiment,
and the average animal weight was 17.1±1.3 g. For biodistribution
study of 99mTc-(HE)3-ZCAIX:1, mice were
randomized into groups of four. In order to determine the optimal
injected protein dose, 3 groups of animals were injected
intravenously (tail vein) with three different doses: 0.3 μg (80
kBq), 1 μg (80 kBq), and 5 μg (110 kBq) of
99mTc-(HE)3-ZCAIX:1 in 100 μl PBS and
sacrificed at 4 h p.i. To check the specificity of the xenograft
targeting of 99mTc-(HE)3-ZCAIX:1, a group of
four mice was subcutaneously pre-injected with 500 μg non-labeled
(His)6-ZCAIX:1 Affibody molecule 40 min before injection
of 1 μg (80 kBq) of 99mTc-(HE)3-ZCAIX:1 and
the mice were sacrificed at 4 h after injection of radioactive
tracer. Two additional groups of mice were injected with 1 μg (110
kBq) to measure biodistribution of
99mTc-(HE)3-ZCAIX:1 at 1 and 8 h p.i.
To study biodistribution of
125I-(HE)3-ZCAIX:1, 6 mice were randomized
into two groups of 3. Animals were injected intravenously with 1 μg
(27 kBq) 125I-(HE)3-ZCAIX:1 per animal in 100
μl PBS. The biodistribution was measured at 6 and 8 h after
injection.
Mice were sacrificed at predetermined time-points by
an intra-peritoneal injection of anesthesia (20 μl/g body weight;
Ketalar, 10 mg/ml; Rompun, 1 mg/ml). Organs and tissue samples were
excised and weighed, and their radioactivity was measured. The
tissue uptake values were calculated as percent of injected dose
per gram tissue (% ID/g).
In vivo imaging was performed to obtain a visual
confirmation of the biodistribution data. Two SK-RC-52 xenograft
bearing mice were injected with 11 MBq (3 μg) of
99mTc-(HE)3-ZCAIX:1. Mice were sacrificed by
cervical dislocation at 4 h after injection. The imaging experiment
was performed using an Infinia γ-camera (GE Healthcare) equipped
with a low energy high-resolution (LEHR) collimator. Static images
(30 min) were obtained with a zoom factor of 2 in a 256×256
matrix.
Results
Labeling of Affibody molecules with
[99mTc(CO)3]+ and
125I
99mTc-(HE)3-ZCAIX:1 Affibody
molecules were efficiently labeled with 99mTc. The yield
was 75±4%. After purification with disposable NAP-5 column, the
radiochemical purity of the conjugate was 99.6±0.2%. The
radioiodination yield was 14±1%, and the purity of
125I-(HE)3-ZCAIX:1 was of 98±1%.
99mTc-(HE)3-ZCAIX:1 was stable
under histidine challenge during 4 h, with no measurable release of
radionuclide after incubation with both 500 and 5000-fold molar
excess amounts of histidine. Similarly, no release of radioactivity
from 125I-(HE)3-ZCAIX:1 was detected after
incubation with NaI (2 M), 30% ethanol or a mixture of NaI (2 M)
and 30% ethanol. The amount of released 125I was minor
and within accuracy of the analytical method.
Affinity determination using
LigandTracer
The kinetic measurements of
99mTc-(HE)3-ZCAIX:1 binding to
CAIX-expressing SK-RC-52 cells in vitro using LigandTracer
Yellow confirmed that its high affinity to CAIX was preserved after
radiolabeling. The best fitting for 99mTc-labeled
(HE)3-ZCAIX:1 was obtained using a 1:2 interaction
model, which indicated that the binding of this radiolabeled
conjugate to living CAIX-expressing cells is mediated by two
binding site populations, one with strong and one with weaker
interaction. The dissociation constant at equilibrium (KD) for the
first interaction was 1.3 nM, and for the second one 130 nM.
In vitro binding specificity and cellular
processing
Addition of 100-fold excess of non-labeled Affibody
molecules caused a significant (P<0.005) decrease in
CAIX-binding of 99mTc-(HE)3-ZCAIX:1 to
CAIX-expressing SK-RC-52 cells, from 9.6±0.1 to 0.66±0.02% of added
radioactivity. This demonstrated saturable binding of
radioconjugates, indicating their specific interaction.
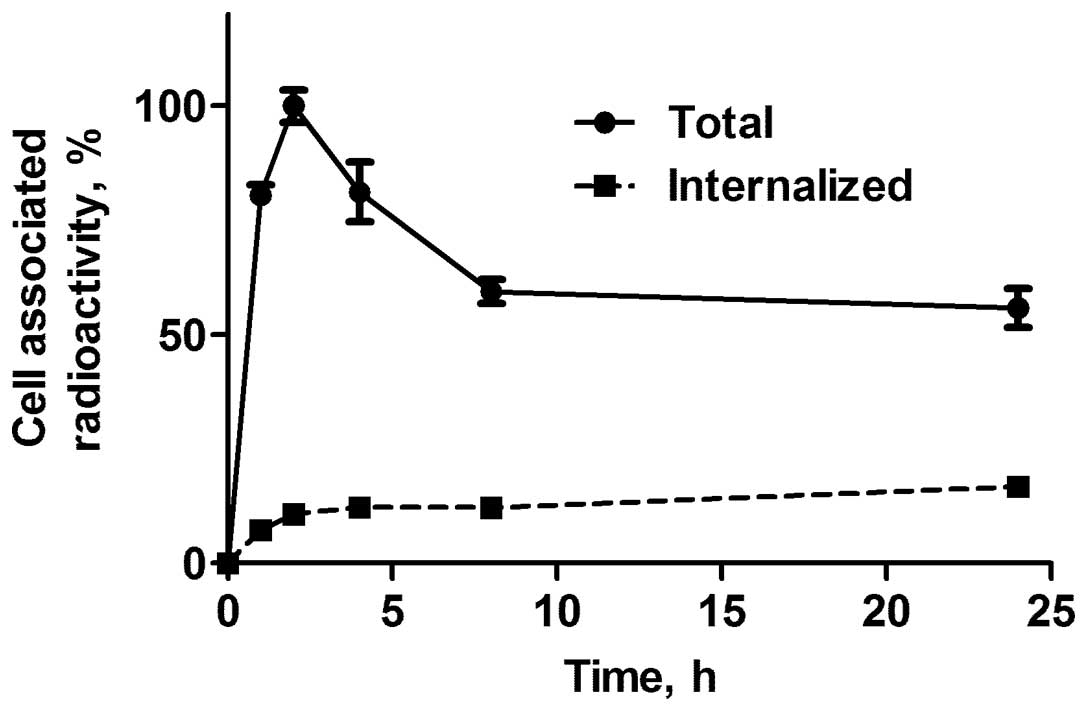
Cellular processing of
99mTc-(HE)3-ZCAIX:1 by CAIX-expressing
SK-RC-52 cells is presented in Fig.
1. The binding pattern of
99mTc-(HE)3-ZCAIX:1 showed a rapid increase
in total cell-associated radioactivity up to 2 h but decreased
considerably at 8 h (59±2% of maximum) and remained steady up to 24
h (55±4% of maximum). To exclude experimental artifacts, this
experiment was repeated twice, but demonstrated very concordant
results. The internalization of all radio-conjugates was slow and
increased slightly throughout the assay. The percentage of
internalized radioactivity by SK-RC-52 cells at 24 h after the
start of incubation was 16.7±0.1%.
In vivo studies of
99mTc-(HE)3-ZCAIX:1 and
125I-(HE)3-ZCAIX:1
The data concerning biodistribution of
99mTc-(HE)3-ZCAIX:1 female NMRI nu/nu mice
bearing SK-RC-52 xenografts at 4 h after injection of different
protein doses are presented in Tables
I and II. There was no
significant difference in tumor-to-organ ratios, except that
tumor-to-spleen ration was significantly lower at the injected
protein dose of 0.3 μg than 5 μg. An injected dose of 1 μg was
selected for further animal studies.
 | Table IBiodistribution of
99mTc-(HE)3-ZCAIX:1 at 4 h after injection in
NMRI nu/nu mice bearing SK-RC-52 xenografts. |
Table I
Biodistribution of
99mTc-(HE)3-ZCAIX:1 at 4 h after injection in
NMRI nu/nu mice bearing SK-RC-52 xenografts.
| Total injected dose
(μg) |
|---|
|
|
|---|
| Organ | 0.3 | 1 | 5 |
|---|
| Blood | 0.2±0.0 | 0.2±0.0 | 0.2±0.0 |
| Lung | 0.4±0.1 | 0.3±0.1 | 0.4±0.1 |
| Salivary gland | 0.4±0.1 | 0.4±0.1 | 0.5±0.1 |
| Liver | 1.2±0.4 | 1.0±0.4 | 0.1±0.1 |
| Spleen | 0.5±0.1 | 0.3±0.1 | 0.4±0.0 |
| Stomach | 0.4±0.0 | 0.5±0.1 | 0.4±0.1 |
| Duodenum | 0.4±0.1 | 0.5±0.2 | 0.4±0.1 |
| Colon | 0.6±0.3 | 1.2±0.5 | 0.9±0.4 |
| Kidney | 143±17 | 141±45 | 154±2 |
| Tumor | 11.0±3.0 | 10.0±1.0 | 11.0±2.0 |
| Muscle | 0.1±0.0 | 0.1±0.1 | 0.1±0.0 |
| Bone | 0.2±0.1 | 0.1±0.0 | 0.2±0.0 |
 | Table IITumor-to-organ ratios of
99mTc-(HE)3-ZCAIX:1 at 4 h after injection in
NMRI nu/nu mice bearing SK-RC-52 xenografts. |
Table II
Tumor-to-organ ratios of
99mTc-(HE)3-ZCAIX:1 at 4 h after injection in
NMRI nu/nu mice bearing SK-RC-52 xenografts.
| Dose (μg) |
|---|
|
|
|---|
| Organ | 0.3 | 1 | 5 |
|---|
| Blood | 62±14 | 53±10 | 65±5 |
| Lung | 26±6 | 35±11 | 24±7 |
| Salivary gland | 27±5 | 25±6 | 23±2 |
| Liver | 9±2 | 11±4 | 11±1 |
| Spleen | 23±1a | 36±14 | 29±4 |
| Stomach | 29±5 | 20±6 | 29±4 |
| Duodenum | 30±5 | 22±8 | 26±1 |
| Colon | 19±8 | 9±3 | 14±5 |
| Kidney | 0.1±0.0 | 0.1±0.0 | 0.1±0.0 |
| Muscle | 95±15 | 104±52 | 102±30 |
| Bone | 47±9 | 80±32 | 59±23 |
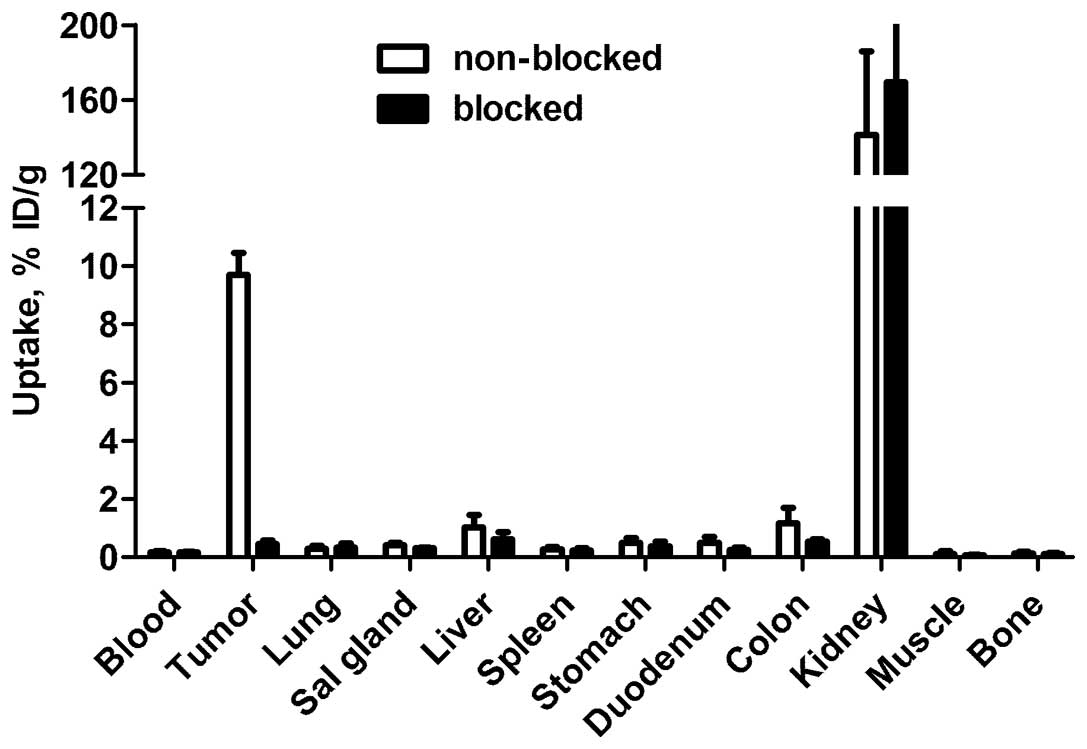
The results of in vivo specificity test are
presented in Fig. 2.
Pre-saturation of CAIX with non-labeled Affibody molecule caused
decrease of uptake from 9.7±0.7 to 0.5±0.1% ID/g
(P<5×10−7). The reduction of tumor uptake
demonstrated saturability of the
99mTc-(HE)3-ZCAIX:1 tumor accumulation and
suggested its specific targeting. There was no significant
difference in 99mTc-(HE)3-ZCAIX:1 uptake in
any other organ after injection of excess amount of non-labeled
Affibody molecules.
The data concerning biodistribution of
99mTc-(HE)3-ZCAIX:1 (injected dose of 1 μg)
in SK-RC-52 xenograft bearing female NMRI nu/nu mice at 1, 4 and 8
h p.i. are shown in Tables III
and IV.
99mTc-(HE)3-ZCAIX:1 showed a rapid blood
clearance already at 1 h p.i. The blood-associated radioactivity
reduced ~4 times between 1 and 4 h, but did not change at 8 h after
injection in comparison with 4 h. A low level of radioactivity
(2.8±1.4% ID at 1 h, 4.5±1.2% ID at 4 h and 1.20±0.30% ID at 8 h
p.i.) in the gastrointestinal tract (with its content) suggested
that hepatobiliary excretion played a minor role in clearance of
99mTc-(HE)3-ZCAIX:1. Most likely, the
clearance of the radio-conjugate from body was via glomerular
filtration with subsequent re-absorption in kidneys. The tumor
uptake of radioactivity was highest at 1 h (22±3% ID/g), which
decreased about two times (9.7±0.7% ID/g) at 4 h and remained at
the same level at 8 h after injection. There was significant
decrease of radioactivity uptake of
99mTc-(HE)3-ZCAIX:1 in lung and salivary
glands between 1 and 4 h with further decrease between 4 and 8 h
after injection. The concentration of radioactivity in all other
organs was low at 1 h and decreased significantly by 4 h
(P<0.05), but there was no significant difference between 4 and
8 h p.i. On the other hand, there was a significant difference
between 1 and 8 h p.i. (P<0.05). Overall, tumor-to-blood and
tumor-to-organ (except for tumor-to-colon) ratios of
99mTc-(HE)3-ZCAIX:1 were the highest at 4 h
(P<0.05), and decreased slightly at 8 h after injection
(Table IV).
 | Table IIIBiodistribution of
99mTc-(HE)3-ZCAIX:1 (injected dose 1 μg) at
1, 4 and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts. |
Table III
Biodistribution of
99mTc-(HE)3-ZCAIX:1 (injected dose 1 μg) at
1, 4 and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts.
|
99mTc-(HE)3-ZCAIX:1 |
|---|
|
|
|---|
| 1 h | 4 h | 8 h |
|---|
| Blood | 0.9±0.2a | 0.2±0.0 | 0.2±0.0c |
| Lung | 1.4±0.3a | 0.3±0.1b | 0.6±0.2c |
| Salivary gland | 1.0±0.2a | 0.4±0.1b | 0.85±0.2 |
| Liver | 4.0±0.7a | 1±0.4 | 0.9±0.3c |
| Spleen | 0.7±0.1a | 0.3±0.1 | 0.6±0.2 |
| Stomach | 1.4±0.4a | 0.5±0.1 | 0.5±0.3 |
| Duodenum | 2.6±0.5a | 0.5±0.2 | 0.5±0.2c |
| Colon | 0.7±0.1 | 1.2±0.5 | 0.5±0.1 |
| Kidney | 226±20a | 141±45 | 170±52 |
| Tumor | 22.3±3.2a | 9.7±0.7 | 7.3±3.0c |
| Muscle | 0.4±0.1a | 0.1±0.1 | 0.2±0.1 |
| Bone | 0.5±0.1a | 0.1±0.0 | 0.3±0.2 |
 | Table IVTumor-to-organ ratios of
99mTc-(HE)3-ZCAIX:1 (injected dose 1 μg) at
1, 4 and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts. |
Table IV
Tumor-to-organ ratios of
99mTc-(HE)3-ZCAIX:1 (injected dose 1 μg) at
1, 4 and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts.
|
99mTc-(HE)3-ZCAIX:1 |
|---|
|
|
|---|
| 1 h | 4 h | 8 h |
|---|
| Blood | 26±4a | 53±1 | 42±7c |
| Lung | 15±3a | 35±11b | 13±1c |
| Salivary gland | 23±6 | 25±6b | 10±5c |
| Liver | 6±1a | 11±4 | 9±0.3c |
| Spleen | 29±1 | 36±14b | 14±4c |
| Stomach | 17±5 | 20±6 | 19±10c |
| Duodenum | 9±3a | 22±8 | 15±3c |
| Colon | 32±5a | 9±3 | 14±3c |
| Kidney | 0.1±0.0 | 0.1±0.0 | 0.0±0.0c |
| Muscle | 61±14 | 104±52 | 45±8c |
| Bone | 47±7 | 80±32b | 30±10c |
The data concerning biodistribution study of
125I-(HE)3-ZCAIX:1 in SK-RC-52 xenograft
bearing mice (6 and 8 h p.i.) are presented in Tables V and VI. There was no significant difference
between biodistribution and tumor uptake or tumor-to-blood and
tumor-to-organ ratio of 125I-(HE)3-ZCAIX:1 at
6 and 8 h p.i. The tumor and kidney uptake of this radio-conjugate
was equal at both 6 h (2.3±0.5% ID/g and 2.7±1.4% ID/g) and 8 h
(1.6±0.3% ID/g and 1.6±0.1% ID/g) after injection.
 | Table VBiodistribution of
125I-(HE)3-ZCAIX:1 (injected dose 1 μg) at 6
and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts. |
Table V
Biodistribution of
125I-(HE)3-ZCAIX:1 (injected dose 1 μg) at 6
and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts.
|
125I-(HE)3-ZCAIX:1 |
|---|
|
|
|---|
| 6 h | 8 h |
|---|
| Blood | 0.09±0.02 | 0.07±0.02 |
| Lung | 0.09±0.04 | 0.05±0.01 |
| Salivary gland | 0.10±0.04 | 0.11±0.05 |
| Liver | 0.20±0.01 | 0.18±0.01 |
| Spleen | 0.08±0.02 | 0.08±0.01 |
| Stomach | 0.08±0.03 | 0.08±0.06 |
| Duodenum | 0.07±0.01 | 0.05±0.03 |
| Colon | 0.04±0.01 | 0.03±0.01 |
| Kidney | 2.7±1.4 | 1.6±0.1 |
| Tumor | 2.2±0.5 | 1.6±0.3 |
| Muscle | 0.03±0.01 | 0.022±0.04 |
| Bone | 0.04±0.01 | 0.04±0.03 |
 | Table VITumor-to-organ ratios of
125I-(HE)3-ZCAIX:1 (injected dose 1 μg) at 6
and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts. |
Table VI
Tumor-to-organ ratios of
125I-(HE)3-ZCAIX:1 (injected dose 1 μg) at 6
and 8 h after injection in NMRI nu/nu mice bearing SK-RC-52
xenografts.
|
125I-(HE)3-ZCAIX:1 |
|---|
|
|
|---|
| 6 h | 8 h |
|---|
| Blood | 26±2 | 24±5 |
| Lung | 30±13 | 31±5 |
| Salivary gland | 22±1 | 18±11 |
| Liver | 11±2 | 9±1 |
| Spleen | 31±12 | 20±6 |
| Stomach | 30±11 | 28±14 |
| Duodenum | 33±6 | 35±16 |
| Kidney | 0.9±0.2 | 1.0±0.1 |
| Muscle | 84±18 | 77±18 |
| Bone | 53±11 | 56±37 |
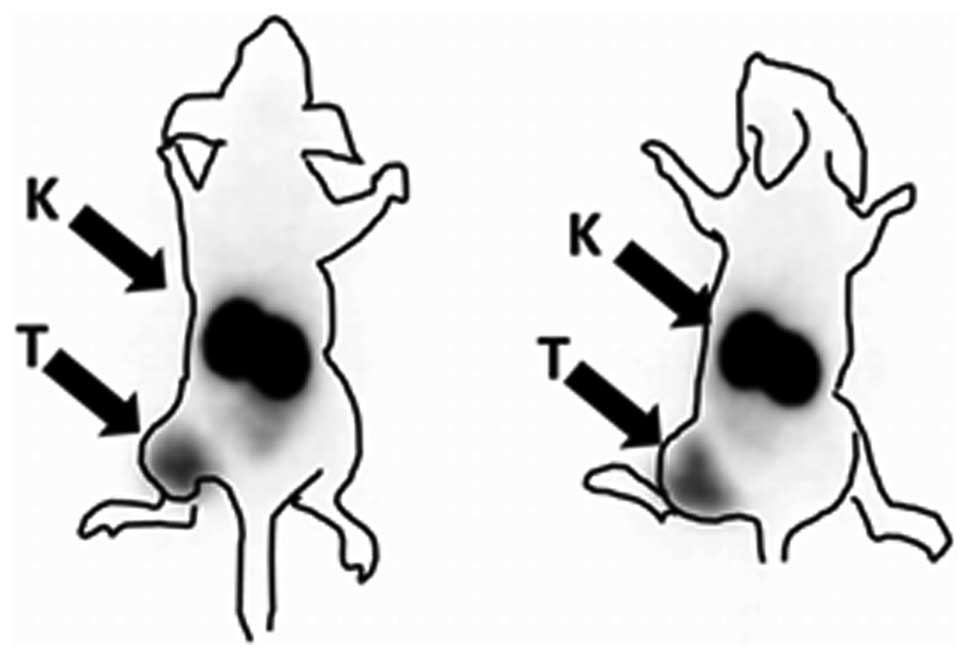
The obtained high contrast images of
99mTc-(HE)3-ZCAIX:1 confirmed the
biodistribution results (Fig. 3).
Images obtained at 4 h p.i. showed no visible uptake in any organ
except kidneys. Tumors were clearly visualized. The
tumor-to-contralateral site ratio was 16.2±0.6.
Discussion
Imaging contrast is an important factor determining
sensitivity and therefore, accuracy of molecular imaging. Data
concerning CAIX-targeting antibodies (31) demonstrated that the use of smaller
fragments enables better contrast in comparison with intact IgG,
and provides shorter time between injection and peak contrast.
Affibody molecules are 4-fold smaller than the smallest antibody
fragments. An excellent imaging contrast has been demonstrated for
a number of molecular targets using Affibody molecules (37). Therefore, we have generated an
Affibody molecule with low nanomolar affinity to CAIX. For
biodistribution studies, a negatively charged
histidine-glutamate-histidine-glutamate-histidine-glutamate
[HEHEHE, (HE)3]-tag was engineered at N-terminus of the
selected Affibody molecules. Previous studies have demonstrated
that (HE)3-tags enables stable site-specific labeling of
Affibody molecules with
[99mTc(CO)3]+, and provide much
lower hepatic accumulation of radioactivity than with hexahistidine
tags (40). In addition, the use
of (HE)3-tag provides favorable modification of
biodistribution profile even if different labels (e.g.
111In or radioidine) are used (41). In the case of anti-CAIX, the use of
(HE)3-tag enabled efficient and stable labeling using
commercially available labeling IsoLink kit. Binding of
99mTc-(HE)3-ZCAIX:1 to CAIX-expressing cells
was saturable, which indicates its binding specificity. The binding
of 99mTc-(HE)3-ZCAIX:1 showed a maximum
uptake at 2 h after incubation start. An important feature of
99mTc-(HE)3-ZCAIX:1 was relatively slow
internalization. Only 16.7% of cell-associated radioactivity was
internalized at 24 h after incubation start. Interaction of
99mTc-(HE)3-ZCAIX:1 with living SK-RC-52
cells showed the presence of two binding sites, one strong (1.3 nM)
and another much weaker.
In vivo,
99mTc-(HE)3-ZCAIX:1 showed efficient and
specific targeting of CAIX-expressing SK-RC-52 xenografts, since
the tumor uptake was reduced from 9.7±0.7 to 0.4±0.1% ID/g
(P<5×10−7) by pre-saturation of CAIX in vivo
(Fig. 2). There was no significant
difference in uptake of 99mTc-(HE)3-ZCAIX:1
in other organs, suggesting no on-target interaction of
99mTc-(HE)3-ZCAIX:1 in vivo. This was
also confirmed by absence of significant difference in
biodistribution after injection of 0.3, 1 or 5 μg
99mTc-(HE)3-ZCAIX:1 (Tables I and II). The pattern of
99mTc-(HE)3-ZCAIX:1 (Tables III and IV) biodistribution at different
time-points was similar to biodistribution of anti-HER2
99mTc-(HE)3-ZHER2:342 Affibody
molecule (41), which also has no
or low target expression in normal tissues. In both cases, there
was rapid clearance of radioactivity from blood and normal tissues.
At the same time, there was high and non-saturable uptake of
radioactivity in kidneys, which is typical for Affibody molecules
with residualizing labels. The pattern of tumor uptake in
vivo resembled binding to the cells in vitro: a high
uptake at 1 h after injection (23±3% ID/g) was significantly
reduced to 9.7±0.7% ID/g at 4 h after injection, but further
reduction of tumor uptake to 7.3±3% ID/g at 8 h after injection was
not significant. The highest tumor-to-organ ratios for
99mTc-(HE)3-ZCAIX:1 were obtained at 4 h
after injection. Experimental imaging demonstrated that
CAIX-expressing SK-RC-52 xenografts could be visualized with high
contrast in mice (Fig. 3). In
agreement with biodistribution data, the only organ with higher
radioactivity accumulation than in tumor was the kidneys.
One possible clinical application of CAIX imaging
is discrimination between benign and malignant primary kidney
tumors. This requires higher level of radionuclide accumulation in
tumors than in kidneys. Apparently, this is not possible when
residualizing labels are used. However, the Affibody molecules
showed slow internalization by the tumor cells. Therefore,
residualizing properties of a label are not absolutely necessary
for a good retention of radionuclides in tumors. On the contrary,
internalization of Affibody in kidneys is rapid, and the use of
non-residualizing radiohalogen labels results in a rapid washout of
radioactivity from kidneys (36,44,41).
This created a precondition to obtain a higher radioactivity uptake
in tumor than in kidney a few hours after injection for
high-affinity anti-HER2 ZHER2:342 Affibody molecule or
its derivatives (36,44,41).
We tested if this is also correct for (HE)3-ZCAIX:1
using non-residualizing 125I-para-iodobenzoate label. To
allow for clearance of radionuclide from kidneys, biodistribution
of 125I-(HE)3-ZCAIX:1 was measured at 6 and 8
h after injection (Table V). As
expected, renal accumulation of radioactivity was much lower in the
case of radioiodine label than in the case of 99mTc
(1.6±0.1 vs. 170±52% ID/g at 8 h p.i., respectively). However,
there was also an appreciable release of
125I-(HE)3-ZCAIX:1 radioactivity from tumors
as well. As a result, tumor-to-kidney ratios were 0.90±0.2 at 6 h
p.i. and 0.99±0.09 at 8 h p.i., i.e. a positive contrast was not
achieved. It has to be noted that anti-HER2 ZHER2:342
Affibody molecule has low picomolar affinity (36). It is likely that further affinity
maturation of anti-CAIX Affibody molecules might provide variants
enabling higher uptake in tumors than in kidneys. With the existing
affinities, imaging of primary renal cell carcinoma using Affibody
molecules is not feasible. Besides lower renal uptake, the use of
radioiodine label did not provide any advantage over
99mTc. The tumor-to-blood ratio was higher for the
99mTc. At 8 h p.i.,
125I-(HE)3-ZCAIX:1 provided higher
tumor-to-lung and tumor-to-duodenum ratios than
99mTc-(HE)3-ZCAIX:1 at the same time-point.
However, these values were not higher than values provided by
99mTc-(HE)3-ZCAIX:1 at 4 h after
injection.
Earlier, several approaches to develop probes for
imaging of CAIX-expression have been evaluated in mice. The use of
intact chimeric G250 antibody resulted in a tumor uptake in the
range of 20 to 110% ID/g and tumor-to-blood ratio in the range of 4
to 9, depending on xenograft model and labeling chemistry (31,45–46).
An optimal imaging time was between 2 and 4 days after injection.
The use of Fab and (Fab′)2 fragments enabled reduction
of imaging time to 24 h p.i., still tumor-to-blood ratio did not
exceed 17 (31,32). Attempts to use radiolabeled
sulfonamide derivatives did not yet result in development of an
imaging agent with tumor uptake of >0.5% ID/g and tumor-to-blood
ratios of more than 1 in murine models (47). Current data suggest that the use of
99mTc-(HE)3-ZCAIX:1 permits appreciably
higher tumor-to-blood ratio than any existing agent for imaging of
CAIX in vivo. In addition, the optimal imaging time is only
a few hours after injection which would facilitate potential
clinical use. It opens also an opportunity to use short-lived
labels, such as 68Ga and 18F, for imaging of
hypoxia using Affibody molecules in the future.
In conclusion, we show the utility of radiolabeled
Affibody molecules as a very promising format for probes for
imaging of CAIX-expression in vivo. The use of
99mTc-(HE)3-ZCAIX:1 permits obtaining the
highest tumor-to-blood ratio so far reported in the literature.
However, further affinity maturation might be required to provide
an Affibody-based agent suitable for imaging of primary renal cell
carcinoma.
Acknowledgements
The present research was financially supported by
grants from the Swedish Cancer Society (Cancerfonden) and the
Swedish Research Council (Vetenskapsrådet).
References
|
1
|
Parkkila S: An overview of the
distribution and function of carbonic anhydrases in mammals. The
Carbonic Anhydrases: New Horizons. Chegwidden WR, Carter N and
Edwards Y: Birkhauser Verlag; Basel: pp. 76–93. 2000
|
|
2
|
Wingo T, Tu C, Laipis PJ and Silverman DN:
The catalytic properties of human carbonic anhydrase IX. Biochem
Biophys Res Commun. 288:666–669. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Opavsky R, Pastorekova S, Zelnik V, et al:
Human MN/CA9 gene, a novel member of the carbonic anhydrase family:
structure and exon to protein domain relationships. Genomics.
33:480–487. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harris AL: Hypoxia - a key regulatory
factor in tumour growth. Nat Rev Cancer. 2:38–47. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Potter C and Harris AL: Hypoxia inducible
carbonic anhydrase IX, marker of tumour hypoxia, survival pathway
and therapy target. Cell Cycle. 3:164–167. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hussain SA, Ganesan R, Reynolds G, et al:
Hypoxia-regulated carbonic anhydrase IX expression is associated
with poor survival in patients with invasive breast cancer. Br J
Cancer. 96:104–109. 2008. View Article : Google Scholar
|
|
7
|
Ord JJ, Agrawal S, Thamboo TP, et al: An
investigation into the prognostic significance of necrosis and
hypoxia in high grade and invasive bladder cancer. J Urology.
178:677–682. 2007. View Article : Google Scholar
|
|
8
|
Le QT, Kong C, Lavori PW, et al:
Expression and prognostic significance of a panel of tissue hypoxia
markers in head-and-neck squamous cell carcinomas. Int J Radiat
Oncol Biol Phys. 69:167–175. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Driessen A, Landuyt W, Pastorekova S, et
al: Expression of carbonic anhydrase IX (CAIX), a hypoxia-related
protein, rather than vascular-endothelial growth factor (VEGF), a
pro-angiogenic factor, correlates with an extremely poor prognosis
in esophageal and gastric adenocarcinomas. Ann Surg. 243:334–340.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Swinson DE, Jones JL, Richardson D, et al:
Carbonic anhydrase IX expression, a novel surrogate marker of tumor
hypoxia, is associated with a poor prognosis in non-small-cell lung
cancer. J Clin Oncol. 21:473–482. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Robertson N, Potter C and Harris AL: Role
of carbonic anhydrase IX in human tumor cell growth, survival, and
invasion. Cancer Res. 64:6160–6165. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Brizel DM, Dodge RK, Clough RW and
Dewhirst MW: Oxygenation of head and neck cancer: changes during
radiotherapy and impact on treatment outcome. Radiother Oncol.
53:113–117. 1999. View Article : Google Scholar
|
|
13
|
Hockel M, Schlenger K, Aral B, et al:
Association between tumor hypoxia and malignant progression in
advanced cancer of the uterine cervix. Cancer Res. 56:4509–4515.
1996.PubMed/NCBI
|
|
14
|
Zeng L, Ou G, Itasaka S, et al: TS-1
enhances the effect of radiotherapy by suppressing
radiation-induced hypoxia-inducible factor-1 activation and
inducing endothelial cell apoptosis. Cancer Sci. 99:2327–2335.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zaffaroni N, Fiorentini G and De Giorgi U:
Hyperthermia and hypoxia: new developments in anticancer
chemotherapy. Eur J Surg Oncol. 27:340–342. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yamazaki Y, Kunimoto S and Ikeda D:
Rakicidin A: a hypoxia-selective cytotoxin. Biol Pharm Bull.
30:261–265. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Raleigh JA, Dewhirst MW and Thrall DE:
Measuring tumor hypoxia. Semin Radiat Oncol. 6:37–45. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mees G, Dierckx R, Vangestel C and Van de
Wiele C: Molecular imaging of hypoxia with radiolabelled agents.
Eur J Nucl Med Mol Imaging. 36:1674–1686. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Machulla HJ: Imaging of Hypoxia-Tracer
Developments. Kluwer Academic Publishers; Dordrecht: pp. 1–18.
1999
|
|
20
|
Wiebe LI and McEwan AJB: Scintigraphic
imaging of focal hypoxic tissue: development and clinical
applications of 123I-IAZA. Braz Arch Biol Technol.
45:89–102. 2002. View Article : Google Scholar
|
|
21
|
Wiebe LI: PET radiopharmaceuticals for
metabolic imaging in oncology. PET and Molecular Imaging: State of
the Art and Future Perspectives. Tamaki Y and Kuge Y:
(International Congress Series 1264C). Elsevier; Amsterdam: pp.
53–76. 2003
|
|
22
|
Graham MM, Peterson LM, Link JM, et al:
Fluorine-18-fluoromisonidazole radiation dosimetry in imaging
studies. J Nucl Med. 38:1631–1636. 1997.PubMed/NCBI
|
|
23
|
Doss M, Zhang JJ, Bélanger MJ, et al:
Biodistribution and radiation dosimetry of the hypoxia marker
18F-HX4 in monkeys and humans determined by using
whole-body PET/CT. Nucl Med Commun. 31:1016–1024. 2010.PubMed/NCBI
|
|
24
|
Brouwers AH, Buijs WC, Mulders PF, et al:
Radioimmunotherapy with [131I]cG250 in patients with
metastasized renal cell cancer: dosimetric analysis and immunologic
response. Clin Cancer Res. 11:7178–7186. 2005. View Article : Google Scholar
|
|
25
|
Li Y, Wang H, Oosterwijk E, et al:
Antibody-specific detection of CAIX in breast and prostate cancers.
Biochem Biophys Res Commun. 28:488–492. 2009. View Article : Google Scholar
|
|
26
|
Oosterwijk-Wakka JC, Boerman OC, Peter FA,
Oosterwijk M and Oosterwijk E: Application of monoclonal antibody
G250 recognizing carbonic anhydrase IX in renal cell carcinoma. Int
J Mol Sci. 14:11402–11423. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Steffens MG, Boerman OC, Oyen WJG, et al:
MN/CA IX/G250 as a potential target for immunotherapy of renal cell
carcinomas. Br J Cancer. 81:741–746. 1999. View Article : Google Scholar
|
|
28
|
Kerbel R and Folkman J: Clinical
translation of angiogenesis inhibitors. Nat Rev Cancer. 2:727–739.
2002. View
Article : Google Scholar : PubMed/NCBI
|
|
29
|
Povoski SP, Hall NC, Murrey DA Jr, et al:
Multimodal imaging and detection strategy with 124 I-Labeled
chimeric monoclonal antibody cG250 for accurate localization and
confirmation of extent of disease during laparoscopic and open
surgical resection of clear cell renal cell carcinoma. Surg Innov.
20:59–69. 2013. View Article : Google Scholar :
|
|
30
|
Ahlskog JK, Schliemann C, Mårlind J, et
al: Human monoclonal antibodies targeting carbonic anhydrase IX for
the molecular imaging of hypoxic regions in solid tumours. Br J
Cancer. 101:645–657. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Carlin S, Khan N, Ku T, et al: Molecular
targeting of carbonic anhydrase IX in mice with hypoxic HT29
colorectal tumor xenografts. PLoS One. 5:e108572010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hoeben BA, Kaanders JH, Franssen GM, et
al: PET of hypoxia with 89Zr-labeled
cG250-F(ab′)2 in head and neck tumors. J Nucl Med.
51:1076–1083. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Askoxylakis V, Garcia-Boy R, Rana S, et
al: A new peptide ligand for targeting human carbonic anhydrase IX,
identified through the phage display technology. PLoS One.
5:e159622010. View Article : Google Scholar
|
|
34
|
Löfblom J, Feldwisch J, Tolmachev V, et
al: Affibody molecules: engineered proteins for therapeutic,
diagnostic and biotechnological applications. FEBS Lett.
584:2670–2680. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nygren PÅ: Alternative binding proteins:
affibody binding proteins developed from a small three-helix bundle
scaffold. FEBS J. 275:2668–2676. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Orlova A, Magnusson M, Eriksson TL, et al:
Tumor imaging using a picomolar affinity HER2 binding affibody
molecule. Cancer Res. 66:4339–4348. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ahlgren S and Tolmachev V: Radionuclide
molecular imaging using Affibody molecules. Curr Pharm Biotechnol.
11:581–589. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Baum RP, Prasad V, Muller D, et al:
Molecular imaging of HER2-expressing malignant tumors in breast
cancer patients using synthetic 111In- or
68Ga-labeled affibody molecules. J Nucl Med. 51:892–897.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sörensen J, Sandberg D, Sandström M, et
al: First-in-human molecular imaging of HER2 expression in breast
cancer metastases using the 111In-ABY-025 affibody
molecule. J Nucl Med. 55:730–735. 2014. View Article : Google Scholar
|
|
40
|
Tolmachev V, Hofstrom C, Malmberg J, et
al: HEHEHE-tagged affibody molecules may be purified by IMAC, are
conveniently labeled with
[99mTc(CO)3]+ and show improved
biodistribution. Bioconjug Chem. 21:2013–2022. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Orlova A, Wållberg H, Stone-Elander S and
Tolmachev V: On the selection of a tracer for PET imaging of
HER2-expressing tumors: direct comparison of a
124I-labeled Affibody molecule and trastuzumab in a
murine xenograft model. J Nucl Med. 50:417–425. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Björkelund H, Gedda L, Barta P, Malmqvist
M and Andersson K: Gefitinib induces epidermal growth factor
receptor dimers which alters the interaction characteristics with
125I-EGF. PLoS One. 6:e247392011. View Article : Google Scholar
|
|
43
|
Wållberg H and Orlova A: Slow
internalization of anti-HER2 synthetic affibody monomer
111In-DOTA-ZHER2:342-pep2: implications for
development of labeled tracers. Cancer Biother Radiopharm.
23:435–442. 2008. View Article : Google Scholar
|
|
44
|
Kramer-Marek G, Kiesewetter DO, Martiniova
L, Jagoda E, Lee SB and Capala J:
[18F]FBEM-ZHER2:342-Affibody molecule-a new
molecular tracer for in vivo monitoring of HER2 expression by
positron emission tomography. Eur J Nucl Med Mol Imaging.
35:1008–1018. 2008. View Article : Google Scholar
|
|
45
|
Brouwers AH, van Eerd JE, Frielink C,
Oosterwijk E, Oyen WJ, Corstens FH and Boerman OC: Optimization of
radioimmunotherapy of renal cell carcinoma: labeling of monoclonal
antibody cG250 with 131I, 90Y,
177Lu, or 186Re. J Nucl Med. 45:327–337.
2004.PubMed/NCBI
|
|
46
|
Lawrentschuk N, Lee FT, Jones G,
Rigopoulos A, Mountain A, et al: Investigation of hypoxia and
carbonic anhydrase IX expression in a renal cell carcinoma
xenograft model with oxygen tension measurements and
124I-cG250 PET/CT. Urol Oncol. 29:411–420. 2011.
View Article : Google Scholar
|
|
47
|
Akurathi V, Dubois L, Celen S, et al:
Development and biological evaluation of
99mTc-sulfonamide derivatives for in vivo visualization
of CA IX as surrogate tumor hypoxia markers. Eur J Med Chem.
71:374–384. 2014. View Article : Google Scholar : PubMed/NCBI
|