Introduction
Diabetes involves the state of chronic hyperglycemia
caused by a range of genetic and environmental factors, and it is
widely considered as one of the risk factors for periodontal
disease (1). Previous studies have
suggested that advanced glycosylation ends (AGEs) triggered by
long-term hyperglycemia can stimulate phagocytes to release
inflammatory cytokines, including tumor necrosis factor (TNF)-α,
interleukin (IL)-1β and IL-6 (2),
which may activate osteoclasts and matrix metalloproteinases
(MMPs), and lead to the destruction of bone and periodontal tissue
(3). TNF-α is one of the most
important inflammatory factors and exerts a variety of biological
effects. It can promote the degradation of connective tissue matrix
and is the leading cytokine of local alveolar bone absorption,
induced by inflammation (4). MMPs
are tightly associated with periodontal tissue destruction and
reconstruction, and are important in the development of
periodontitis (5). MMP-3 is a
member of the MMP family. It leads to the direct degradation of the
extracellular matrix and also induces the expression levels of
MMP-1, MMP-8 and MMP-9, and consequently causes more extensive
damage in periodontal tissue (6).
Therefore, the upregulation of the expression of MMP-3 is more
significant compared with the upregulation of other MMPs. The
alterations of TNF-α and MMP-3 in periodontal tissue may lead to
changes and disorders in the periodontal tissue, promoting the
development of periodontitis (7).
The present study established a rat model of
diabetes and observed histological changes of the periodontal
tissues under the microscope following tissue staining with
hematoxylin and eosin. The expression levels of TNF-α and MMP-3
were observed by immunohistochemistry. The periodontitis induced by
diabetes is closely associated with oxidative stress. Urate is an
antioxidant, which is able to bind to ONOO- in normal conditions.
It is considered to be a specific scavenger of ONOO- (8,9).
Oxidative stress is an imbalance between the production of reactive
oxygen species and antioxidant function, leading to tissue injury.
The produced reactive oxygen species, such as superoxide and
hydroxyl radicals, are able to damage numerous biological
molecules, including DNA and lipid. It has been suggested that
there is a causal association between insulin resistance, oxidative
stress and periodontitis, and that hyperglycemia is a major cause
of oxidative stress (10,11). The present study aimed to
investigate the effect of β-anhydroicaritin on the changes in the
expression levels of TNF-α and MMP-3, and pathological changes in
the periodontal tissue of diabetic rats, providing a theoretical
basis for the prevention of diabetic periodontitis.
Materials and methods
Reagents and animals
Wistar rats (n=40; three months old; body weight,
200–220 g) were purchased from Shanghai Slaccas experimental animal
Co., Ltd. (Shanghai, China; certificate no. SCXK 2013-0012).
β-Anhydroicaritin was purchased from the National
Institute for the Control of Pharmaceutical and Biological Products
(Beijing, China). Urate was purchased from Shanghai Jimei
Biotechnology Co. Ltd. (Shanghai, China). Streptozocin (STZ) was
purchased from Hangzhou Baitong Biological Technology Co. Ltd.
(Hangzhou, China). Rabbit anti-TNF-α polyclonal antibody (cat. no.
ab6671) and rabbit anti-MMP-3 polyclonal antibody (cat. no.
ab137659) were purchased from Abcam (Cambridge, MA, USA).
An Olympus BX51 fluorescence microscope was
purchased from Olympus (Tokyo, Japan). The HPIAS-100 medical color
picture analysis system was purchased from Wuhan Champion Image
Engineering Company (Wuhan, China). A OneTouch ultra blood glucose
meter was purchased from LifeScan (Milipitas, CA, USA).
Animal groups and animal model
The present study was approved by the ethics
committee of Qingdao University (Qingdao, China). The rats (n=40)
were randomly divided into four groups: Normal control group,
diabetes group, diabetes + β-anhydroicaritin group and diabetes +
urate group (n=10 in each group). Following an overnight fast,
diabetes was introduced by intraperitoneal injection of 30 mg/kg
STZ diluted in citrate buffer (pH 4.4; Sigma-Aldrich, St. Louis,
MO, USA).
At three days following STZ injection, the animals
with blood glucose levels >15 mmol/l and urine glucose above +++
were considered as diabetic. Following the establishment of the
diabetes models, the diabetes + β-anhydroicaritin group were
administered 100 mg/kg/day β-anhydroicaritin and the diabetes +
urate group were administered 100 mg/kg/day urate. All rats had
free access to water and food, and were maintained under a 12:12 h
light/dark cycle at 22±2°C and 65–69% relative humidity for 12
weeks. At week 12, the blood glucose, urine glucose and body weight
were assessed (12).
Specimen collection
Following being maintained for 12 weeks, the rats
were euthanized by femoral artery bleeding following a 12 h-fast.
The maxilla was extracted immediately and was fixed in 10%
formaldehyde solution (Beyotime Biotechnology, Shanghai,
China).
Histological detection
The maxilla samples were placed in 0.01 M phosphate
buffered saline (PBS; pH 7.4) for 12 h and the solution was renewed
twice over this time-period. The samples were enucleated and fixed
in formaldehyde, then processed and embedded in paraffin (Leica
Microsystems, Wetzlar, Germany) using routine procedures (13). At the maxillary first molar tooth,
along the long axis of the proximal and distal length, tooth
periodontal slices (6 μm) were cut.
The slices were dewaxed with xylene (Beyotime
Biotechnology) and rehydrated with a descending graded series of
alcohol. The slices were subsequently rinsed with tap water and
hematoxylin-stained for 5 min. The slices were then rinsed, 1%
diluted ammonia was added for 30 sec to retrieve the blue color,
and the slices were again rinsed. The slices were stained with
eosin for 5 min, rinsed, dehydrated with a graded series of
alcohol, made transparent with xylene and finally mounted with
neutral gum (Beyotime Biotechnology).
Immunohistochemical analysis of TNF-α and
MMP-3
Routine paraffin sectioning, dewaxing and hydration
using 3% hydrogen peroxide (Beyotime Biotechnology) were performed
to remove the endogenous peroxidase. Following this, ~50 μl
(1:50) rabbit polyclonal anti-TNF-α and rabbit polyclonal
anti-MMP-3 (1:1,000) antibody were added, and the mixture was
incubated at 4°C overnight. Following incubation, ~50 μl
biotinylated goat anti-rabbit immunoglobulin G secondary antibody
(1:100; cat. no. A0277; Beyotime Biotechnology) working solution
was added, the mixture was incubated at 37°C for 30 min, and
colored using diaminobenzidine. The sample was stained with
hematoxylin (Beyotime Biotechnology), separated using ethanol and
hydrochloric acid (Beyotime Biotechnology), saturated with lithium
carbonate (Sigma-Aldrich) until the color returned to blue,
dehydrated with a graded alcohol series and xylene, and mounted
with neutral gum.
The positive standard for immunohistochemistry was
cytoplasmic and was stained yellow or brown. According to the color
depth (HPIAS-100), staining intensity was scored as: Negative (−),
not coloring; weakly positive (+), slight staining; positive (++),
medium staining; strong positive (+++), deep staining.
For grey value determination, the color multimedia
image analysis system was used to analyze the immunohistochemistry
staining results of each specimen semi-quantitatively. At a
magnification of ×200, a positive signal (grey value) was regarded
in the first molar gingival and distal root in the 1/3 region of
the periodontal membrane as parameter to analyze the results. The
present study analyzed five sections and considered the average as
the result. The grey background of each section was measured in
order to eliminate the differences between sections.
Statistical analysis
The data are expressed as the means ± standard
deviation. SPSS 15.0 (SPSS, Inc, Chicago, IL, USA) was used for the
statistical analysis. One-way analysis of variance was used to
compare the data and the level of the test was a=0.05. Following
determination of a statistically significant difference, further
two-two comparison was performed. P<0.05 was considered to
indicate a statistically significant difference.
Results
Confirmation of the diabetic model at
three days following STZ injection
The average normal fasting blood glucose was 5.73
mmol/l, urine (−). The blood glucose level in the STZ injection
rats was >15 mmol/l, urine (+++), which was significantly
increased compared with that the normal group (P<0.01; Table I).
 | Table IGlucose levels in the blood and urine
of rats. |
Table I
Glucose levels in the blood and urine
of rats.
| Group | n | Blood glucose
(mmol/l) | Urine glucose
(mmol/l) |
|---|
| Control | 10 | 5.73±0.61 | − |
| Diabetes | 10 | 19.74±1.82a | +++ |
| Diabetes +
β-anhydroicaritin | 10 | 19.46±1.75a | +++ |
| Diabetes + urate | 10 | 19.83±1.78a | +++ |
Changes in the physiological features,
body weight and blood glucose of the rats
The normal group demonstrated normal appearance and
behavior, while the diabetes group appeared markedly thin and
presented with a dull coat, unresponsiveness to stimuli,
polydipsia, polyuria, polyphagia. The β-anhydroicaritin treatment
group and the urate treatment group exhibited similar features to
those in the diabetes group; however, these were milder compared
with those in the diabetes group.
Comparison of fasting blood glucose and body weight
in each group prior to and following the experiment revealed that
at 12 weeks, the fasting blood glucose in the normal group
exhibited no significant change (P>0.05) and the body weight
increased significantly (P<0.05). The blood glucose in the
diabetic group exhibited no significant change (P>0.05);
however, the body weight significantly decreased (P<0.01). The
blood glucose in the β-anhydroicaritin treatment group was
significantly decreased (P<0.01) and the body weight also
significantly decreased (P<0.01). In the urate treatment group,
the blood glucose exhibited no significant change (P>0.05);
however, the body weight was significantly decreased (P<0.01;
Tables II and III).
 | Table IIComparison of fasting glucose prior to
and following the experiment. |
Table II
Comparison of fasting glucose prior to
and following the experiment.
| Group | n | Glucose prior to
experiment (mmol/l) | Glucose following
experiment (mmol/l) |
|---|
| Control | 10 | 5.73±0.61 | 5.62±0.58 |
| Diabetes | 10 | 19.74±1.82 | 19.53±1.67 |
| Diabetes +
β-anhydroicaritin | 10 | 19.46±1.75 | 12.92±1.64a |
| Diabetes + urate | 10 | 19.83±1.78 | 18.76±1.92 |
 | Table IIIComparison of body weight prior to and
following the experiment. |
Table III
Comparison of body weight prior to and
following the experiment.
| Group | n | Weight prior to
experiment (g) | Weight following
experiment (g) |
|---|
| Control | 10 | 211.75±7.66 |
348.56±11.35a |
| Diabetes | 10 | 209.16±8.34 | 162.91±9.54b |
| Diabetes +
β-anhydroicaritin | 10 | 210.62±7.92 | 154.68±8.38b |
| Diabetes +
urate | 10 | 210.68±7.84 | 158.83±9.49b |
Comparison of the levels of fasting blood glucose
and weight in each group following the experiment revealed that the
blood glucose levels in the diabetes group, the β-anhydroicaritin
treatment group and the urate treatment group were significantly
higher compared with those in the normal group (P<0.01), and the
body weight was significantly lower compared with that in the
normal group (P<0.01). The blood glucose levels in the
β-anhydroicaritin treatment group were significantly lower compared
with those in the diabetic group (P<0.01) and the urate
treatment group (P<0.01). The blood glucose levels in the urate
treatment group and the diabetic group were not significantly
different from each other (P>0.05). Furthermore, the body weight
of the β-anhydroicaritin treatment group, the urate treatment group
and the diabetes group were not significantly different from each
other (P>0.05; Table IV).
 | Table IVComparison of fasting glucose and
body weight following the experiment. |
Table IV
Comparison of fasting glucose and
body weight following the experiment.
| Group | n | Blood glucose
(mmol/l) | Body weight
(g) |
|---|
| Control | 10 | 5.62±0.58 | 348.56±11.35 |
| Diabetes | 10 | 19.53±1.67a | 162.91±9.54a |
| Diabetes +
β-anhydroicaritin | 10 | 12.92±1.64a,b,c | 154.68±8.38a |
| Diabetes +
urate | 10 | 18.76±1.92 | 158.83±9.49a |
HE staining
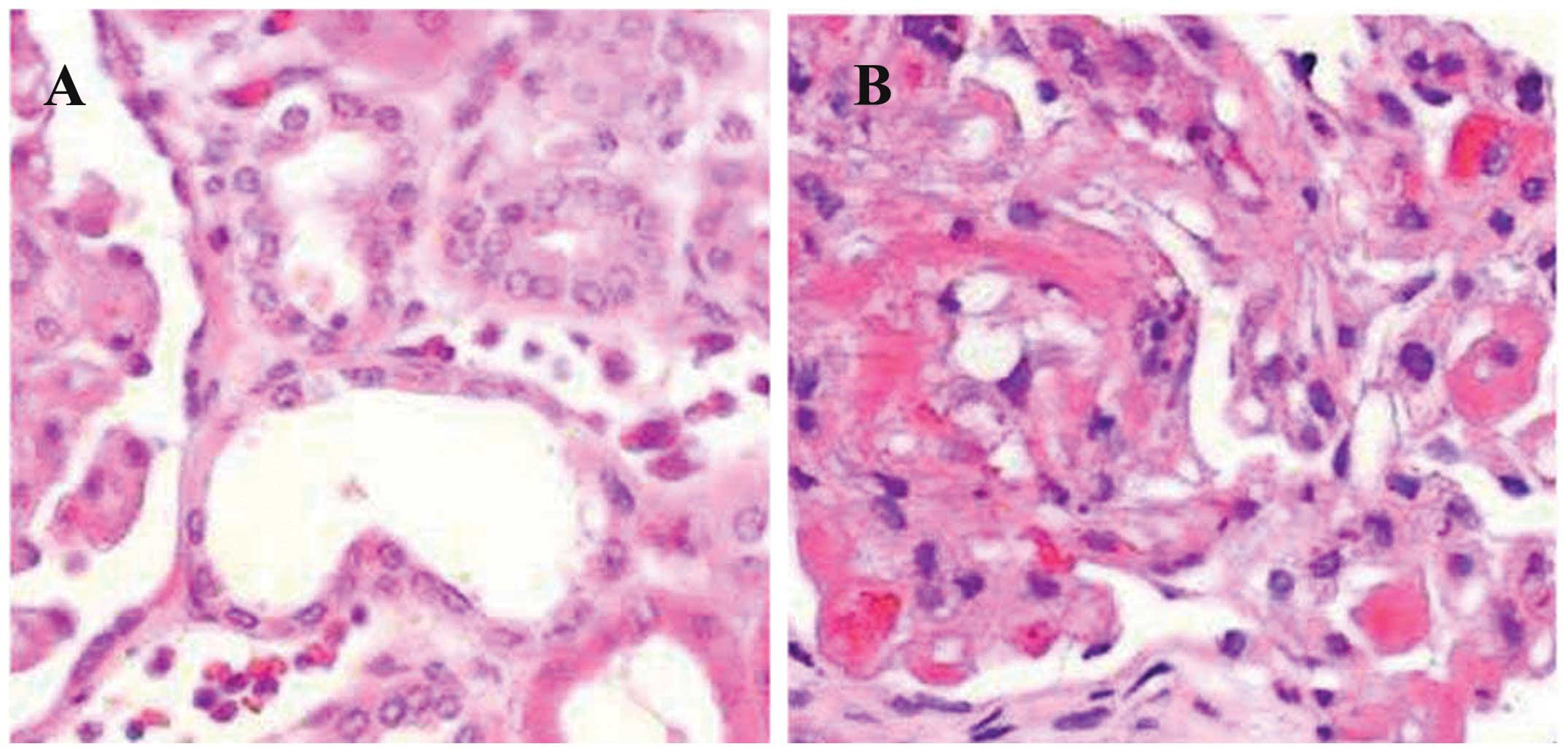
In the control group, the junctional epithelium was
attached to the cementumenamel junction and was firmly combined
with the tooth tissue. No inflammatory infiltration was observed in
the epithelium and the gingival and periodontal ligament fibers
were arranged orderly and neatly. The alveolar bone edge was smooth
and no osteoclast was observed. The alveolar ridge crest exhibited
no absorption (Fig. 1).
The diabetes group exhibited junctional epithelium
attached to the cementumenamel junction. The gingival epithelium
and lamina propria exhibted moderate infiltration of inflammatory
cells and the number of capillaries in the gingival and periodontal
membrane increased. The capillaries demonstrated dilatation and
congestion. Fibers were disordered and ruptured. The bone
resorption lacunae along the alveolar bone increased and
osteoclasts were observed. The alveolar ridge crest exhibited no
absorption (Fig. 2).
The diabetes + β-anhydroicaritin group exhibited
junctional epithelium attached to the cementumenamel junction. The
gingival epithelium and lamina propria demonstrated moderate
infiltration of inflammatory cells. The capillaries exhibited no
marked dilatation and congestion, and the fibers appeared
regenerated and ordered. Bone resorption lacunae along the alveolar
bone decreased. Osteoclasts were significantly reduced and the
number of osteoblasts was increased as compared with those in the
diabetes group. The alveolar ridge crest exhibited no absorption
(Fig. 3).
In the diabetes + urate group, the results were
similar to those in the diabetes + β-anhydroicaritin group
(Fig. 4).
Expression levels of TNF-α and MMP-3 in
the periodontal tissue
Immunohistochemical analysis showed that in the
control group, the expression of TNF-α was weakly positive in the
gingival epithelial layer, granular layer, spinous layer and basal
layer cells, fibroblasts and the cytoplasm of endothelial cells.
The expression of MMP-3 was predominantly weakly positive in
fibroblasts and the cytoplasm of alveolar bone cells (mainly
osteoblasts), and negatively expressed in the gingival epithelium
(Table V).
 | Table VGrey values of TNF-α and MMP-3 in the
periodontal tissue. |
Table V
Grey values of TNF-α and MMP-3 in the
periodontal tissue.
| Group | n | TNF-α | MMP-3 |
|---|
| Control | 10 | 97.67±24.65 | 82.66±17.61 |
| Diabetes | 10 | 73.24±21.41a | 52.14±16.32b |
| Diabetes +
β-anhydroicaritin | 10 | 95.17±23.28c | 63.25±16.64c |
| Diabetes +
urate | 10 |
108.61±26.92d,e | 93.35±18.47d,f |
In the diabetes group, the expression of TNF-α was
strongly positive in the gingival epithelial layer, granular layer
and stratum spinosum cells, fibroblasts, vascular endothelial
cells, osteoblasts, osteoclasts and the cytoplasm of bone marrow
stromal cells, and was positively expressed in the gingival
epithelial basal layer (Fig. 5).
The expression of MMP-3 was strongly positive in the gingival
epithelial layer, granular layer and stratum spinosum cells,
fibroblasts, alveolar bone cells (mainly osteoclasts) and the
cytoplasm of bone marrow stromal cells, and was negatively
expressed in the gingival epithelial basal layer (Fig. 6).
In the diabetes + β-anhydroicaritin group, the
expression of TNF-α was weakly positive in the gingival epithelium
and fibroblasts. The expression of MMP-3 was weakly positive in the
gingival epithelium, fibroblasts and the cytoplasm (Fig. 7).
In the diabetes + urate group, the results were
similar to those in the diabetes + β-anhydroicaritin group (results
not shown).
The grey value of TNF-α was determined for all
groups. The diabetic group exhibited a significantly lower grey
value compared with that in the normal group (P<0.05). The
β-anhydroicaritin treatment group exhibited no significant
difference in TNF-α levels compared with those in the normal group
(P>0.05); however, they were significantly higher compared with
those in the diabetic group (P<0.05). The β-anhydroicaritin
treatment group exhibited a lower grey value compared with that in
the urate treatment group (P<0.05; Table V).
The grey value of MMP-3 in the diabetic group was
significantly lower compared with that in the normal group
(P<0.01). MMP-3 levels in the β-anhydroicaritin treatment group
and urate treatment group exhibited no significant difference
compared with those in the control group (P>0.05); however, they
were significantly higher compared with those in the diabetic group
(P<0.05). The β-anhydroicaritin treatment group exhibited a
lower MMP-3 grey value compared with that in the urate treatment
group (P<0.05; Table V).
Discussion
STZ is a broad-spectrum antibiotic, which has
anti-bacterial and anti-tumor properties, and causes side effects
which lead to diabetes mellitus. STZ has highly selective toxic
effects on islet cells in experimental animals, which leads to
direct destruction of pancreatic β cells of the islet tissue or
causes an immune response and decreases the insulin secretion of
islets, which leads to diabetes (14,15).
This model has advantages, including a simple preparation method,
low dosage, low toxicity and specific islet cell damage, and it has
become the preferred method of establishing a rat model of diabetes
(16). The animals used to
establish the model are usually inbred Wistar rats or Sprague
Dawley rats. Daniel et al (17) reported that the success rate of
model establishment in male rats was significantly higher compared
with that in female rats. Monea et al (18) reported that the sensitivity of rats
to STZ occurred in an age-dependent manner. The present study used
male Wistar rats with an average body weight of 212.62 g. Following
an overnight fast, diabetes was introduced by intraperitoneal
injection of 30 mg/kg STZ diluted in citrate buffer (pH 4.4). At
three days following the STZ injection, the blood glucose and urine
glucose levels were assessed. The animals with blood glucose levels
>15 mmol/l and urine glucose of +++ were considered as diabetic.
At week 12, the blood glucose, urine glucose and body weight were
assessed. The body weight of the diabetic rats was significantly
reduced (P<0.01) and glucose levels were >15 mmol/l, which
indicated that animals were diabetic from the establishment of the
diabetic model until the end of the experiment.
Diabetes is a disease characterized by chronic high
blood glucose and it is associated with genetic and environmental
factors. It is due to a defect in insulin secretion and/or action,
which causes disordered sugar, fat and protein metabolism (19,20).
Patients with diabetes often suffer from periodontitis. Previous
studies indicated that diabetes affected periodontitis incidence,
severity and wound healing (21).
Previous reports have demonstrated that rats exhibited alveolar
bone resorption at one month of diabetes, which was aggravated with
the extension of duration. The extension of bone resorption
expanded, spreading to the alveolar bone to which the majority of
periodontal fibers were attached, destroying the Haversian system
and invading the bone marrow cavity (22,23).
Demmer et al (24) found
that bone resorption in the diabetic rat was present. The formation
of new bone was slow and alveolar bone destruction exceeded bone
repair.
The results of the present study suggested that
junctional epithelium in the control group was attached to the
cementumenamel junction and was firmly combined with the tooth
tissue. No inflammatory infiltration was observed in the
epithelium, and gingival and periodontal ligament fibers were
arranged orderly and neatly. The alveolar bone edge was smooth and
no osteoclasts were observed. The alveolar ridge crest exhibited no
absorption. However, in the diabetes group, the junctional
epithelium was attached to the cementumenamel junction, and the
gingival epithelium and lamina propria exhibited moderate
infiltration of inflammatory cells. The number of capillaries in
the gingival and periodontal membrane increased, and the capillary
demonstrated dilatation and congestion. The fibers were in
disordered and ruptured, and bone resorption lacunae along the
alveolar bone increased. Osteoclasts were observed and the alveolar
ridge crest exhibited no absorption. These results suggested that
diabetes alone was not able to cause periodontitis; however, it may
destroy the normal structure of the periodontal tissue, which leads
to a vulnerable state of the periodontal tissue. As a result,
periodontitis is easily caused by a local stimulus.
TNF is one of the important inflammatory factors,
which can be divided into two types: TNF-α and TNF-β. TNF-α is
produced and secreted by several cells, including
monocytes/macrophages, fibroblasts, vascular endothelial cells,
osteoblasts, osteoclasts, T lymphocytes, smooth muscle cells and
adipocytes (25,26). TNF-α can cause a variety of
biological effects when acting on different target cells. When
acting on fibroblasts, it can promote cell proliferation and the
generation of prostaglandin 2; when acting on vascular endothelial
cells, it can increase vascular permeability; and when acting on
bone and cartilage tissue, it can cause bone absorption (27,28).
These characteristics of TNF-α suggest that it is associated with
the destruction of the connective tissue of the periodontal tissue
and the alveolar bone absorption (29). MMP-3 (also termed stromelysin-1) is
an important member of the MMP family, which is secreted by
fibroblasts, endothelial cells and other connective tissue cells.
It has an important role in tissue degradation, as its functions
are to decompose protein polysaccharide and break down type I, V,
IX, XI collagen, fibronectin and laminin (30,31).
The predominant role of MMP-3 in the process of periodontal tissue
destruction is that it directly degrades the extracellular matrix
and causes more extensive destruction of the periodontal tissue
through inducing the expression and activation of MMP-1, MMP-8 and
MMP-9 (32). Therefore, increased
expression of MMP-3 is more significant compared with the increased
expression of other MMPs.
The expression levels of TNF-α and MMP-3 are low in
normal periodontal tissue (33).
The present study demonstrated that in the control group, the
expression of TNF-α was weakly positive in the gingival epithelial
layer, granular layer, spinous layer and basal layer cells,
fibroblasts and cytoplasm of endothelial cells. The expression of
MMP-3 was predominantly weakly positive in fibroblasts and the
cytoplasm of alveolar bone cells (mainly osteoblasts), and
negatively expressed in the gingival epithelium. The results
indicated that normal periodontal tissue produced a certain amount
of TNF-α and MMP-3 in order to ensure that the periodontal tissue
remodeling was in a dynamic balance. Once the balance was
disturbed, it led to structural changes in the periodontal
tissue.
The high-permeability state of diabetes, AGEs and a
variety of secreted cytokines induced by abnormal oxide are
important in the pathophysiological process of the body and tissue
damage caused by diabetes (34).
Hyperglycemia leads to the non-enzymatic glycosylation of a group
of proteins and lipids. They are combined with high-affinity
receptors on the macrophage surface, triggering the secretion of
TNF-α, IL-1β, IL-6 as well as other inflammatory mediators
(35). At the same time,
hyperglycemia leads to the upregulation of the expression levels of
MMPs and nitric oxide. These factors may lead to bone absorption
and the destruction of connective tissue (36).
The present study demonstrated that
β-anhydroicaritin ameliorated the degradation of periodontal tissue
and inhibited the synthesis and secretion of TNF-α and MMP-3 in
diabetic rats. In conclusion, the results of the present study
suggest that β-anhydroicaritin may be used in the treatment of
periodontitis in patients with diabetes. However, the mechanisms by
which β-anhydroicaritin ameliorates periodontal degradation, i.e.
whether it directly inhibits or regulates the body’s metabolic
function through the elimination of ONOO− and further
inhibits TNF-α and MMP-3 expression indirectly, remains to be
elucidated. Further investigations are required to shed light upon
these questions.
References
|
1
|
Xu JL, Meng HX, Li Z, Li FY and Zhang L:
Effect of periodontal therapy on metabolic control and serum
biochemical markers in subjects with type 2 diabetes and chronic
periodontitis. Beijing Da Xue Xue Bao. 45:27–32. 2013.In Chinese.
PubMed/NCBI
|
|
2
|
Schara R, Skaleric E, Seme K and Skaleric
U: Prevalence of periodontal pathogens and metabolic control of
type 1 diabetes patients. J Int Acad Periodontol. 15:29–34.
2013.PubMed/NCBI
|
|
3
|
Bascones-Martínez A, Arias-Herrera S,
Criado-Cámara E, Bascones-Ilundáin J and Bascones-Ilundáin C:
Periodontal disease and diabetes. Adv Exp Med Biol. 771:76–87.
2012.
|
|
4
|
Li H, Li W, Ding Y, et al: Affect of
protein tyrosine phosphatase non-receptor type 2 and nuclear
factor-kappaB on periodontal destruction with diabetes. Hua Xi Kou
Qiang Yi Xue Za Zhi. 30:598–602. 2012.In Chinese.
|
|
5
|
Al-Khabbaz AK and Al-Shammari KF: Diabetes
mellitus and periodontal health: dentists’ knowledge. Med Princ
Pract. 20:538–544. 2011. View Article : Google Scholar
|
|
6
|
Chen L, Luo G, Xuan D, et al: Effects of
non-surgical periodontal treatment on clinical response, serum
inflammatory parameters and metabolic control in patients with type
2 diabetes: a randomized study. J Periodontol. 83:435–443. 2012.
View Article : Google Scholar
|
|
7
|
Silva JA, Ferrucci DL, Peroni LA, et al:
Sequential IL-23 and IL-17 and increased Mmp8 and Mmp14 expression
characterize the progression of an experimental model of
periodontal disease in type 1 diabetes. J Cell Physiol.
227:2441–2450. 2012. View Article : Google Scholar
|
|
8
|
Cai L, Wang J, Li Y, Sun X, Wang L, Zhou Z
and Kang YJ: Inhibition of superoxide generation and associated
nitrosative damage is involved in metallothionein prevention of
diabetic cardiomyopathy. Diabetes. 54:1829–1837. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee WH, Gounarides JS, Roos ES and Wolin
MS: Influence of peroxynitrite on energy metabolism and cardiac
function in a rat ischemia-reperfusion model. Am J Physiol Heart
Circ Physiol. 285:H1385–H1395. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nassar H, Kantarci A and van Dyke TE:
Diabetic periodontitis: A model for activated innate immunity and
impaired resolution of inflammation. Periodontol 2000. 43:233–244.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mahadev K, Wu X, Zilbering A, Zhu L,
Lawrence JT and Goldstein BJ: Hydrogen peroxide generated during
cellular insulin stimulation is integral to activation of the
distal insulin signaling cascade in 3T3-L1 adipocytes. J Biol Chem.
276:48662–48669. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Soares AF, Carvalho RA, Veiga FJ, et al:
Restoration of direct pathway glycogen synthesis flux in the
STZ-diabetes rat model by insulin administration. Am J Physiol
Endocrinol Metab. 303:E875–E885. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pacios S, Andriankaja O, Kang J, et al:
Bacterial infection increases periodontal bone loss in diabetic
rats through enhanced apoptosis. Am J Pathol. 183:1928–1935. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Xiong X, Elkind-Hirsch KE, Xie Y, et al:
Periodontal disease as a potential risk factor for the development
of diabetes in women with a prior history of gestational diabetes
mellitus. J Public Health Dent. 73:41–49. 2013. View Article : Google Scholar
|
|
15
|
Almeida Abdo J, Cirano FR, Casati MZ, et
al: Influence of dyslipidemia and diabetes mellitus on chronic
periodontal disease. J Periodontol. 84:1401–1408. 2013. View Article : Google Scholar
|
|
16
|
Sgolastra F, Severino M, Pietropaoli D,
Gatto R and Monaco A: Effectiveness of periodontal treatment to
improve metabolic control in patients with chronic periodontitis
and type 2 diabetes: a meta-analysis of randomized clinical trials.
J Periodontol. 84:958–973. 2013. View Article : Google Scholar
|
|
17
|
Daniel R, Gokulanathan S, Shanmugasundaram
N, Lakshmigandhan M and Kavin T: Diabetes and periodontal disease.
J Pharm Bioallied Sci. 4(Suppl 2): S280–S282. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Monea A, Mezei T and Monea M: The
influence of diabetes mellitus on periodontal tissues: a
histological study. Rom J Morphol Embryol. 53:491–495.
2012.PubMed/NCBI
|
|
19
|
Al-Khabbaz AK, Al-Shammari KF, Hasan A and
Abdul-Rasoul M: Periodontal health of children with type 1 diabetes
mellitus in Kuwait: a case-control study. Med Princ Pract.
22:144–149. 2013. View Article : Google Scholar
|
|
20
|
Oates TW: Gingival blood glucose may
screen for type 2 diabetes in patients with periodontal disease. J
Evid Based Dent Pract. 12:154–155. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Obradović R, Kesić L, Mihailović D,
Jovanović G, Antić S and Brkić Z: Low-level lasers as an adjunct in
periodontal therapy in patients with diabetes mellitus. Diabetes
Technol Ther. 14:799–803. 2012. View Article : Google Scholar
|
|
22
|
Boissonneault G; CHAC: Diabetes: exploring
a periodontal connection. JAAPA. 25:18–20. 2012.PubMed/NCBI
|
|
23
|
Haseeb M, Khawaja KI, Ataullah K, Munir MB
and Fatima A: Periodontal disease in type 2 diabetes mellitus. J
Coll Physicians Surg Pak. 22:514–518. 2012.PubMed/NCBI
|
|
24
|
Demmer RT, Holtfreter B, Desvarieux M, et
al: The influence of type 1 and type 2 diabetes on periodontal
disease progression: prospective results from the study of health
in Pomerania (SHIP). Diabetes Care. 35:2036–2042. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bastos AS, Graves DT, Loureiro AP, et al:
Lipid peroxidation is associated with the severity of periodontal
disease and local inflammatory markers in patients with type 2
diabetes. J Clin Endocrinol Metab. 97:E1353–E1362. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chang PC, Chien LY, Yeo JF, et al:
Progression of periodontal destruction and the roles of advanced
glycation end products in experimental diabetes. J Periodontol.
84:379–388. 2013. View Article : Google Scholar
|
|
27
|
Yoon AJ, Cheng B, Philipone E, Turner R
and Lamster IB: Inflammatory biomarkers in saliva: assessing the
strength of association of diabetes mellitus and periodontal status
with the oral inflammatory burden. J Clin Periodontol. 39:434–440.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rajhans NS, Kohad RM, Chaudhari VG and
Mhaske NH: A clinical study of the relationship between diabetes
mellitus and periodontal disease. J Indian Soc Periodontol.
15:388–392. 2011. View Article : Google Scholar
|
|
29
|
Sjödin B, Edblad E, Sondell K and Dahlén
G: Minor manifestations of periodontal diseases in young adults
with type 1 diabetes mellitus. Periodontal and microbiological
findings. Acta Odontol Scand. 70:589–596. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Silva JA, Lopes Ferrucci D, Peroni LA, et
al: Periodontal disease-associated compensatory expression of
osteoprotegerin is lost in type 1 diabetes mellitus and correlates
with alveolar bone destruction by regulating osteoclastogenesis.
Cells Tissues Organs. 196:137–150. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Franek E, Januszkiewicz-Caulier J, Blach
A, et al: Intima-media thickness and other markers of
atherosclerosis in patients with type 2 diabetes and periodontal
disease. Kardiol Pol. 70:7–13. 2012.PubMed/NCBI
|
|
32
|
Botero JE, Yepes FL, Roldán N, et al:
Tooth and periodontal clinical attachment loss are associated with
hyperglycemia in patients with diabetes. J Periodontol.
83:1245–1250. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Obradović R, Kesić L, Mihailović D, et al:
A histological evaluation of a low-level laser therapy as an
adjunct to periodontal therapy in patients with diabetes mellitus.
Lasers Med Sci. 28:19–24. 2013. View Article : Google Scholar
|
|
34
|
Field CA, Gidley MD, Preshaw PM and
Jakubovics N: Investigation and quantification of key periodontal
pathogens in patients with type 2 diabetes. J Periodontal Res.
47:470–478. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Nassar PO, Walker CS, Salvador CS,
Felipetti FA, Orrico SR and Nassar CA: Lipid profile of people with
diabetes mellitus type 2 and periodontal disease. Diabetes Res Clin
Pract. 96:35–39. 2012. View Article : Google Scholar
|
|
36
|
Lakschevitz F, Aboodi G, Tenenbaum H and
Glogauer M: Diabetes and periodontal diseases: interplay and links.
Curr Diabetes Rev. 7:433–439. 2011. View Article : Google Scholar : PubMed/NCBI
|