Introduction
Methotrexate (MTX) is one of the most popular and
safe antirheumatic drugs under the applied treatment dose (1,2). In
order to obtain a better curative effect in clinical cases, MTX is
also used in combination with other drugs for rheumatoid arthritis
treatment (1,3,4). In
addition, MTX is also used as an anticancer drug (5). Recently, MTX has been widely applied
for the treatment of various cancers, such as hepatoma,
osteosarcoma, leukemia, lymphoma, gastric, breast, head and neck
cancers (5–9). Many studies have demonstrated that MTX
induces cancer cell death via apoptotic death pathways (10–14).
Apoptotic death pathways can be divided into caspase-dependent and
caspase-independent cascades (15,16).
Concerning the MTX-induced apoptotic pathways, most studies have
shown that MTX induces apoptosis via caspase-dependent cascades in
many cancer cell lines (17–21).
However, some studies have indicated that MTX can induce apoptosis
via caspase-independent cascades in osteosarcoma cells (22,23).
The present study found that MTX-induced apoptosis in Hep3B cells
is via the caspase-dependent cascade, similar to most other studies
(17–21).
Two major caspase cascade pathways have been
reported (24–26). One is the caspase-8/-3 cascade,
known as the extrinsic death receptor pathway (CD95/APO-1/Fas
receptor) (27–29). Another is the caspase-9/-3 cascade,
known as the intrinsic mitochondrial death pathway (27,30,31).
Some studies have shown that MTX-induced apoptosis is mediated by
the caspase-9/-3 cascade pathway in choriocarcinoma, breast cancer,
oral squamous carcinoma and hepatoma cells (18,19,21,32,33).
In contrast, some studies demonstrated that MTX-induced apoptosis
is mediated through the caspase-8/-3 cascade pathway in breast
cancer, hepatoma and leukemia cells (17,33,34).
The present study showed that MTX activates the caspase-9/-3
cascade in Hep3B cells, but not the caspase-8/-3 cascade.
Previously, many studies have shown that high-dose
MTX treatment can induce increased oxidative stress, resulting in
renal and liver damage (3,35–37).
However, the specific reactive oxygen species (ROS) induced by MTX
treatment have not been identified. O2− and
H2O2 are ROS families generally existing in
many cells. By using the lucigenin-amplified method (38–40),
our results are the first to demonstrate that MTX can induce
increases in H2O2 levels, but not
O2− levels.
Considering that high-dose MTX treatments can cause
renal and liver damage (35–37),
combination treatments of low-dose MTX and other anticancer drugs
are suggested and applied during clinical cancer therapy in order
to enhance the anticancer effects and decrease MTX-induced
side-effects (9,10,12,18,41).
However, not all anticancer agents can enhance the anticancer
effects of low-dose MTX. A recent study showed that aspirin can
antagonize the MTX-induced cytotoxic effect on lung cancer cells
(42). Alternatively, there have
been many reports on the antioxidant activities of vitamin C
(43–47). Moreover, some studies have
demonstrated that vitamin C can exert anticancer activities in
various cancer cells (48–52). The present study demonstrated that
vitamin C can diminish MTX-induced increases in
H2O2 levels. On the other hand, it is worth
noting that vitamin C can help low-dose MTX exert a cytotoxic
effect on Hep3B cells. Taken together, the study demonstrated that
MTX activates the caspase-9/-3 cascade and induces increased
H2O2 levels, causing cell cytotoxicity in
Hep3B cells, while more importantly, the present study is the first
to demonstrate that vitamin C enhances the anticancer efficiency in
MTX-treated Hep3 cells.
Materials and methods
Chemicals and materials
Methotrexate was purchased from Pfizer Inc. MTT
assay kit was purchased from Bio Basic Canada Inc. Hoechst 33342,
vitamin C, lucigenin and luminol were purchased from Sigma.
Caspase-3 like substrate (Ac-DEVD-pNA), caspase-8 substrate
(Ac-IETD-pNA) and caspase-9 substrate (Ac-LEHD-pNA) were purchased
from AnaSpec, Inc. (San Jose, CA, USA). Fetal bovine serum (FBS),
Dulbecco’s modified Eagle’s medium (DMEM), non-essential amino
acid, L-glutamine and penicillin/streptomycin were purchased from
Gibco-BRL.
Cell cultures
Hep3B cells were cultured in DMEM containing 10%
FBS, 2 mM L-glutamine, 100 IU/ml penicillin/streptomycin, and 0.1
mM non-essential amino acids. The cells were cultured at 37°C in a
humidified atmosphere containing 5% CO2.
Cell viability assay
Hep3B cell viability was assessed using the MTT
assay method according to the manufacturer’s instructions. In
brief, Hep3B cells were maintained in each well of 96-well culture
plates. Every 24 h, the control group and experimental groups were
subjected to the MTT assay kit. After 3 h of incubation, absorbance
at 570 nm for each well containing Hep3B cells was detected under a
multi-well ELISA reader (Molecular Devices). Cell viability was
calculated using the following formula: A570 experimental
group/A570 control group × 100%.
Nuclear condensation and DNA
fragmentation
Apoptotic cells were identified by nuclear
condensation and DNA fragmentation using Hoechst 33342 staining.
Cells were treated with 10 μg/ml Hoechst 33342 for 10 min. Nuclear
condensation and DNA fragmentation were observed under a
fluorescence microscope (excitation, 352 nm; emission, 450 nm)
(53,54).
Caspase activity assay
Caspase activity assays were executed according to
previous studies (55,56). In brief, Hep3B cells were lysed with
a lysis buffer (50 mM Tris-HCl, 120 mM NaCl, 1 mM EDTA, 1% NP-40,
pH 7.5) and protease inhibitors. After centrifugation (15,000 × g,
30 min, 4°C) cell pellets were collected. The working solutions
containing 40 μl cell lysates (80 μg total protein), 158 μl
reaction buffer (20% glycerol, 0.5 mM EDTA, 5 mM dithiothreitol,
100 mM HEPES, pH 7.5) and 2 μl fluorogenic caspase substrate
(Ac-LEHD-pNA, Ac-DEVD-pNA or Ac-IETD-pNA) were incubated at 37°C
for 6 h. Fluorogenic substrate cleavage was determined at 405 nm in
an ultra-microplate reader (BioTek Instruments). The fold increase
in caspase activity was calculated using the following formula:
(A405 experimental group - A405 control group)/A405 control
group.
Determination of
H2O2 and O2−
levels
H2O2 and
O2− levels were examined by using
lucigenin-amplified chemiluminescence according to the
lucigenin-amplified method (57,58).
In brief, for H2O2 levels, the sample (200
μl) was mixed with 0.2 mmol/l luminol solution (100 μl). After
that, the mixture was measured with a chemiluminescence analyzing
system (CLA-FSI; Tohoko Electronic Industrial Co., Ltd., Miyagi,
Japan) for determination. For O2− levels, 200
μl of the sample was mixed with 0.1 mmol/l of lucigenin solution
(500 μl), and was then measured by the CLA-FSI chemiluminescence
analyzing system.
Statistical analysis
Experimental data were calculated from three
independent triplicate experiments and are presented as the mean
values of the chosen triplicate groups. These experimental data are
shown as means with standard deviations.
Results
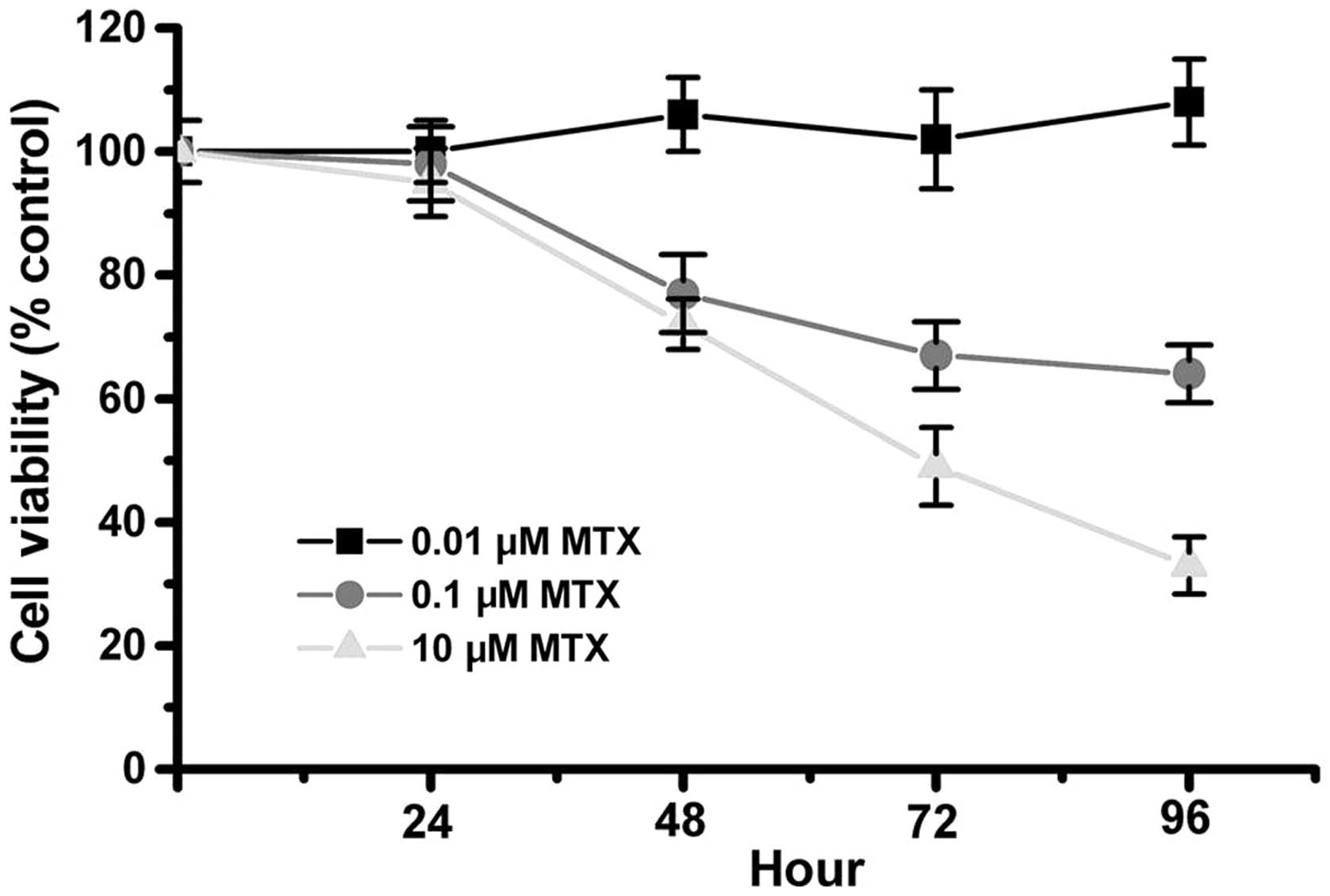
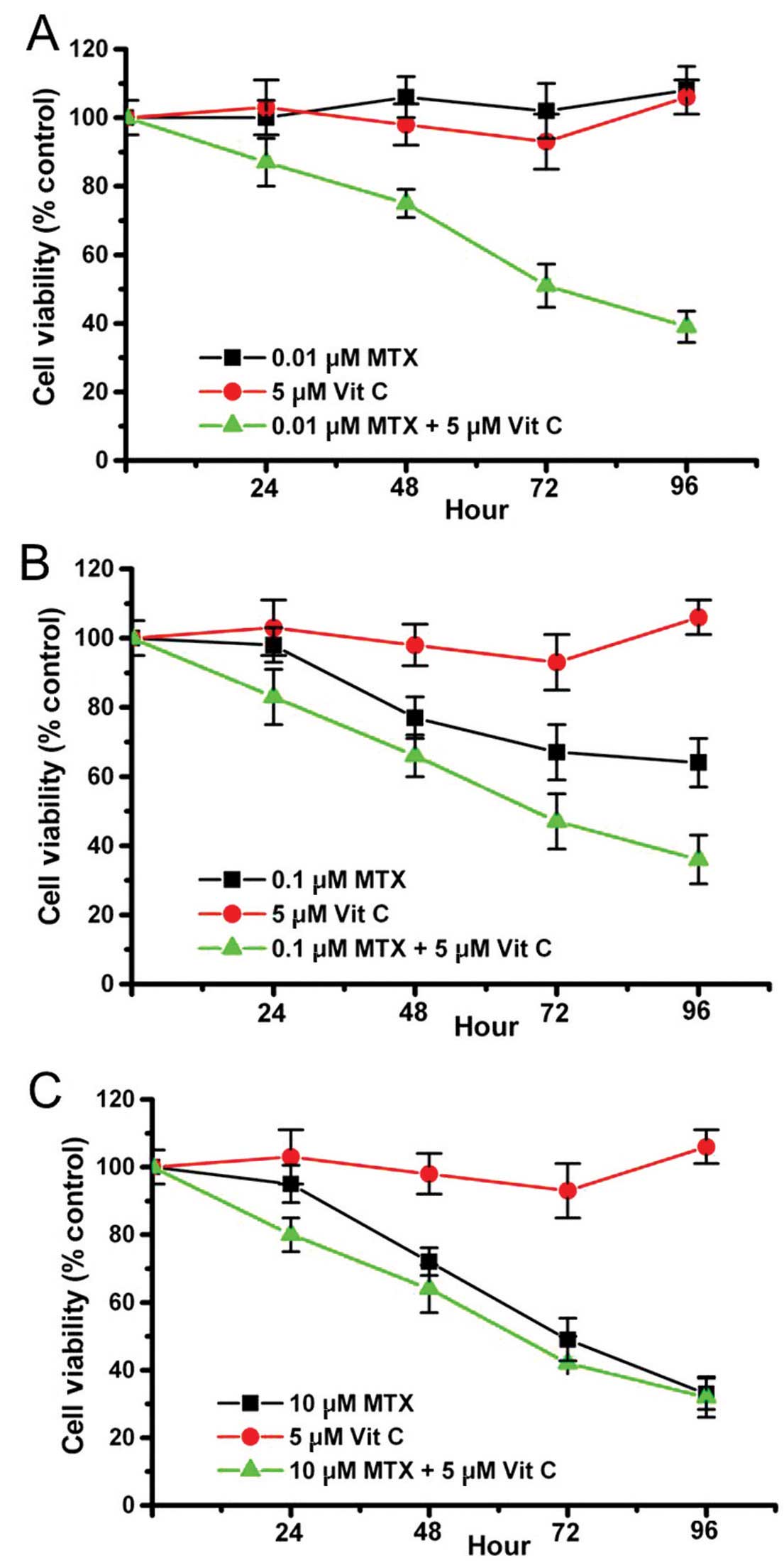
MTX exerts dose-dependent and
time-dependent anticancer effects on Hep3B cells
In clinical cases, 10–25 mg/week MTX (~0.1 μM/day)
is a safely applied dose for rheumatoid arthritis treatment
(1,2,59). In
the present study, 0.1 μM (treatment-dose), 0.01 μM (low-dose) and
10 μM (high-dose) MTX were used for studying the anticancer effects
on Hep3B cells. Hep3B cell viability decreased in the 0.1 and 10 μM
MTX treatment groups, but did not decrease in the 0.01 μM treatment
group (Fig. 1). In addition, the 10
μM MTX treatment group showed a stronger cytotoxic effect in the
Hep3B cells than the 0.1 μM MTX treatment group. These data suggest
that MTX exerts a dose-dependent anticancer effect on Hep3B cells.
In addition, cell viability was observed over different MTX
incubation times, with results showing that the cell viability
decreased incrementally in the 0.1 and 10 μM MTX groups. The
present study indicates that MTX exerts a dose-dependent and
time-dependent anticancer effect on Hep3B cells.
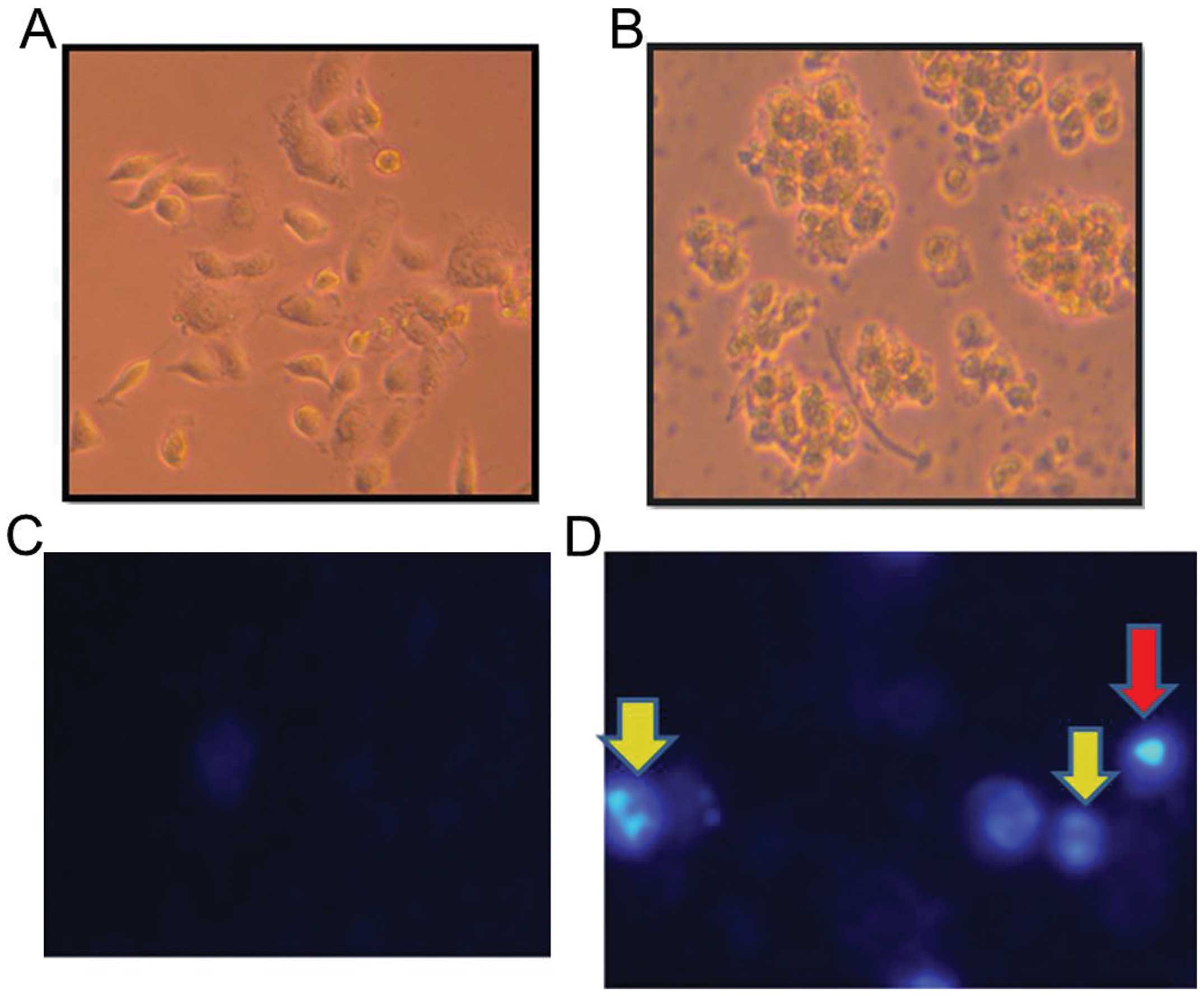
MTX induces apoptosis and activates the
caspase-9/-3 cascade in Hep3B cells
The study investigated whether MTX induces apoptosis
in Hep3B cells. Cell morphology was observed under a phase-contrast
microscope. Hep3B cells survived with morphology intact in the
control group (Fig. 2A). However,
dead cells were noted in the MTX treatment group (Fig. 2B). In addition, nuclear condensation
and DNA fragmentation are apoptotic features and can be observed
using a nuclear staining method, as previously described (55,60).
Compared with the control group (Fig.
2C), nuclear condensation and DNA fragmentation were noted in
the MTX-treated group (Fig. 2D).
The results indicate that MTX induced apoptosis in the Hep3B cells.
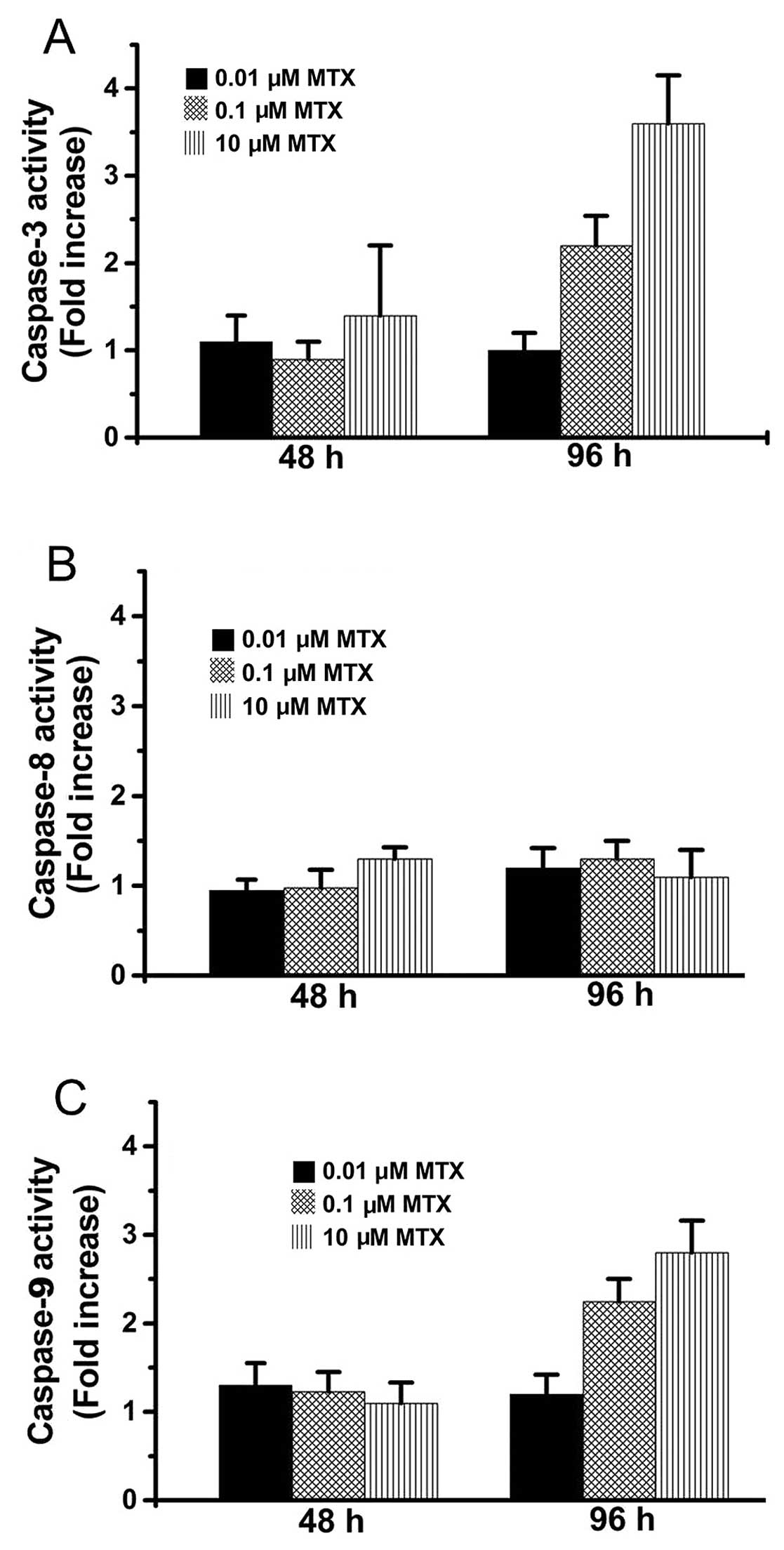
Next, caspase activation was determined in the MTX-treated Hep3B
cells by using a substrate cleavage assay (56,61).
As shown in Fig. 3A, caspase-3
activity increased in the Hep3B cells at 96 h following treatment
with 0.1 and 10 μM MTX while caspase-3 activity did not increase in
Hep3B cells following treatment with 0.01 μM MTX. Caspase-9
activity also increased in the 0.1 and 10 μM MTX-treated Hep3B
cells at 96 h but did not increase in the 0.01 μM MTX-treated cells
(Fig. 3C). However, there was no
obvious increase in caspase-8 activity among the MTX-treated Hep3B
cells (Fig. 3B). These results
suggest that MTX (10 and 0.1 μM) induced apoptosis in the Hep3B
cells via the caspase-9/-3 cascade but not via the caspase-8/-3
cascade.
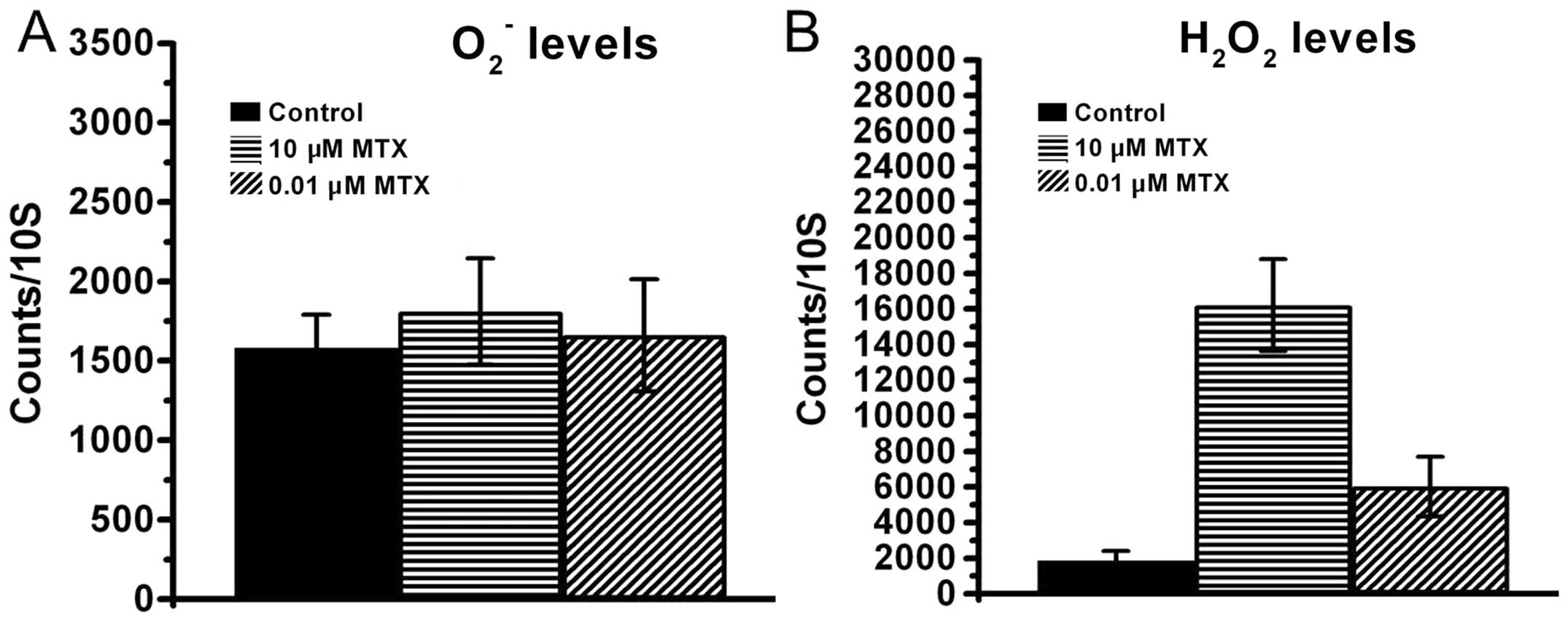
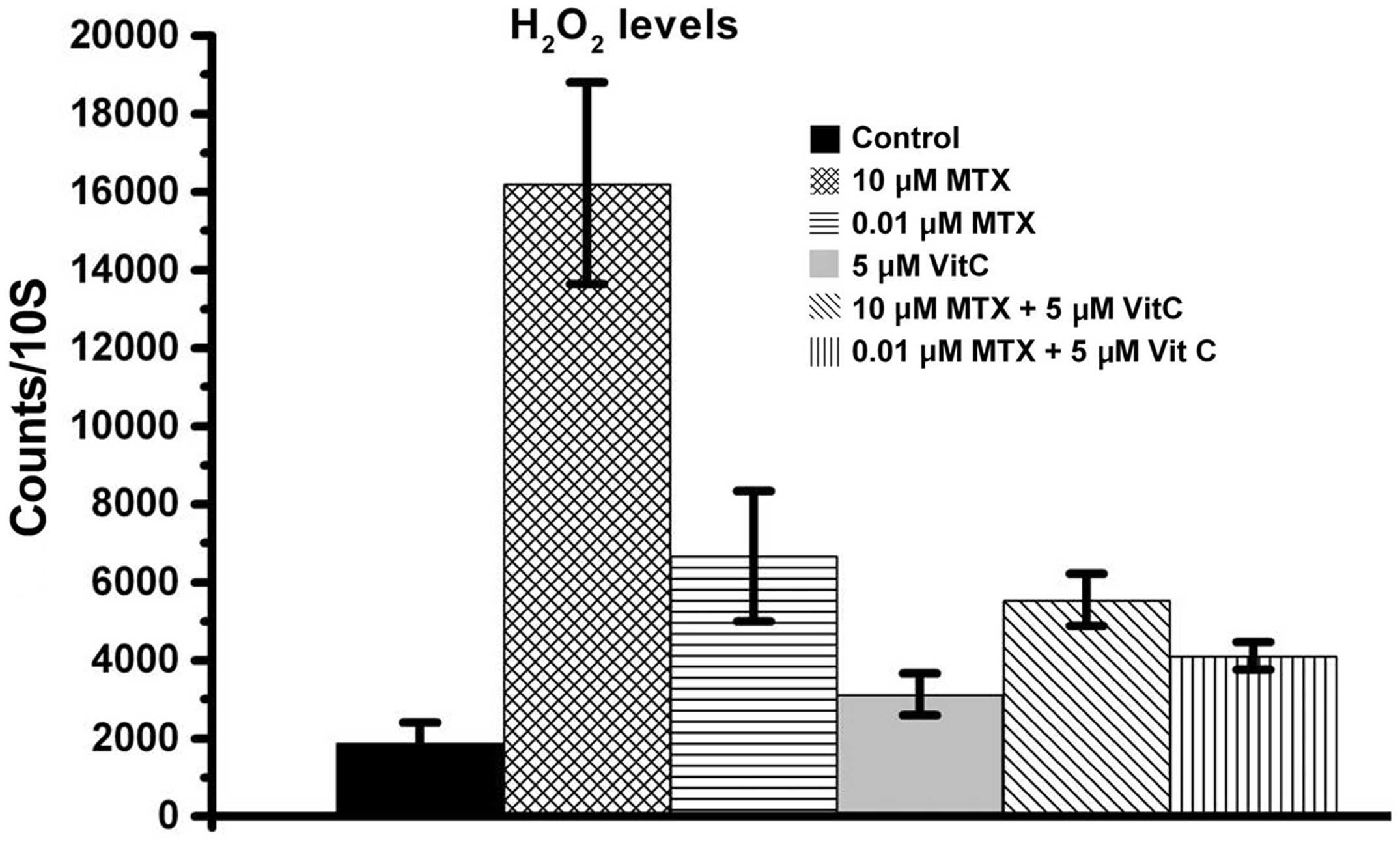
MTX causes increases in
H2O2 levels but not O2−
levels in Hep3B cells
Previous studies have shown that MTX can cause cell
cytotoxicity associated with increases in reactive oxygen species
(ROS) (35–37). Prior to the present study, the
literature has not yet identified which ROS is induced by MTX
treatment. Both O2− and
H2O2 belonging to ROS commonly exist in
cells. Therefore, O2− and
H2O2 levels were examined according to the
lucigenin-amplified method (57,58).
The present study found that MTX did not raise
O2− levels in the Hep3B cells (Fig. 4A). However, both high-dose MTX and
low-dose MTX raised H2O2 levels in the Hep3B
cells (Fig. 4B). Therefore, the
MTX-induced ROS increase is related to H2O2
levels but not related to O2− levels in the
Hep3B cells.
Vitamin C reduces the increase in
H2O2 levels and enhances the anticancer
efficacy in MTX-treated Hep3B cells
Many studies have demonstrated that vitamin C can
prevent oxidative stress-induced cell damage (43–47).
Considering that MTX induces oxidative stress resulting in cell
damage (35–37), this study examined whether vitamin C
could decrease H2O2 levels, essentially
inhibiting MTX-induced cytotoxicity in Hep3B cells. As shown in
Fig. 5, the group receiving a
combination treatment of vitamin C and 10 μM MTX had lower
H2O2 levels than the 10 μM MTX group.
Similarly, the vitamin C and 0.01 μM MTX combination treatment
group had lower H2O2 levels than the 0.01 μM
MTX group. These data indicate that vitamin C reduced the
MTX-induced H2O2 levels. However, to our
surprise, vitamin C did not attenuate cell cytotoxicity in the
MTX-treated Hep3B cells. On the contrary, our data showed that
vitamin C enhanced the anticancer efficacy in MTX-treated Hep3B
cells (Fig. 6). As shown in
Fig. 6A and B, combination
treatments of 5 μM vitamin C and MTX (0.01 or 0.1 μM) exerted a
stronger anticancer effect on Hep3B cells than MTX treatment alone.
It is worth noting that 0.01 μM MTX alone or 5 μM vitamin C alone
did not have a significant cytotoxic effect on Hep3B cells, whereas
a combination treatment of 0.01 μM MTX and 5 μM vitamin C did
induce a cytotoxic effect on Hep3B cells (Fig. 6A). While vitamin C did not enhance
the 10 μM MTX-induced cytotoxic effect on Hep3B cells (Fig. 6C), the present study was important
in indicating that vitamin C can assist low-dose MTX exert an
anticancer effect on Hep3B cells.
Discussion
Previous reports have revealed that MTX-induced
cytotoxicity is related to increased reactive oxygen species (ROS)
(35–37). However, no study has shown which ROS
are induced following MTX treatment. In the present study, two
types of ROS, O2− and
H2O2, were measured.
H2O2 levels in MTX-treated cells rose
significantly while O2− levels did not. In
addition, it is well known that glutathione can convert toxic
H2O2 into non-toxic H2O. We
suggest that the increase in H2O2 levels is a
possible and important reason why N-acetyl cysteine (NAC), a
clinical drug for glutathione synthesis, is used for MTX-induced
cell damage (35,38,39,62).
On the other hand, high-dose MTX-induced H2O2
level increases were higher than low-dose MTX-induced
H2O2 level increases (Fig. 4B). Our data also showed that MTX
induced cytotoxicity in a dose-dependent manner (Fig. 1). Taken together, we consider
increases in the H2O2 level to be one factor
resulting in the inhibition of cell survival following MTX
treatment.
MTX has anticancer effects on various hepatoma cell
lines, including HepG2, MHCC97, Huh7 and Morris 5123 cells
(6,63–67).
Alhough the mechanisms involved in the MTX-induced cytotoxic
effects on different hepatoma cells remain undetermined, a previous
study demonstrated that MTX-induced cytotoxic effects on HepG2
cells are related to the CD95 death receptor pathway (caspase-8/-3
cascade pathway), whereas MTX-induced cytotoxic effects on Huh7 and
Hep3B cells are not related to death receptor pathways (65). Similarly, the caspase-8/-3 cascade
pathway was also found not to be involved in MTX-treated Hep3B
cells in the present study (Fig.
3B). This study further demonstrated that MTX-induced apoptosis
in Hep3B cells occurred through the caspase-9/-3 cascade pathway
(Fig. 3A and C). These previous
studies indicate that MTX induces different caspase pathways in
different hepatoma cell lines. HepG2 is a p53 wild-type hepatoma
cell line, while Hep3B is a p53-deficient hepatoma cell line
(68,69). Thus, we suggest that p53 may be a
possible reason for why the caspase-8/-3 pathway was activated in
the MTX-treated HepG2 cells, while the caspase-9/-3 pathway was
activated in the MTX-treated Hep3B cells.
Previous studies have demonstrated that MTX-induced
cell cytotoxicity is associated with increases in reactive oxygen
species (ROS) (35–37). The present study also indicated that
MTX-induced H2O2 level increases may be one
factor resulting in cell growth inhibition. On the other hand,
vitamin C can reduce oxidative stress against ROS-induced cell
damage (43–47). Here, we also demonstrated that
vitamin C did reduce MTX-induced increases in
H2O2 levels. However, vitamin C did not
inhibit MTX-induced cell cytotoxicity in Hep3B cells. On the
contrary, vitamin C assisted low-dose MTX to exhibit a strong
cytotoxic effect in Hep3B cells. Similarly, recent studies also
indicated that vitamin C can enhance anticancer agents to exert a
strong cytotoxic effect on cancer cells, although the mechanisms
remain unknown (48,70–72).
Thus, MTX-induced increases in H2O2 levels
may be one of the factors resulting in cytotoxicity noted in
MTX-treated Hep3B cells. There are various unclear MTX-induced
death signals that remain to be studied. Regardless, a combination
treatment of vitamin C and low-dose MTX may be a potential method
for hepatoma cancer therapy.
Overall, the present study first demonstrated that
MTX induces an increase in H2O2 levels and
activates the caspase-9/-3 cascade pathway to cause apoptosis in
Hep3B cells. Importantly, a combination treatment of vitamin C and
low-dose MTX exerted a strong anticancer effect in Hep3B cells.
This treatment method may be useful for future clinical cancer
therapy.
Acknowledgements
This work was supported by the following grants:
NSC101-2321-B-039-004; NHRI-EX102-10245BI; TCRD-TPE-102-26 and
TCRD-TPE-103-48.
References
|
1
|
Weinblatt ME: Methotrexate in rheumatoid
arthritis: a quarter century of development. Trans Am Clin Climatol
Assoc. 124:16–25. 2013.PubMed/NCBI
|
|
2
|
Patane M, Ciriaco M, Chimirri S, et al:
Interactions among low dose of methotrexate and drugs used in the
treatment of rheumatoid arthritis. Adv Pharmacol Sci.
2013:3138582013.PubMed/NCBI
|
|
3
|
Cakir T, Ozkan E, Dulundu E, et al:
Caffeic acid phenethyl ester (CAPE) prevents methotrexate-induced
hepatorenal oxidative injury in rats. J Pharm Pharmacol.
63:1566–1571. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Keystone E, Landewe R, van Vollenhoven R,
et al: Long-term safety and efficacy of certolizumab pegol in
combination with methotrexate in the treatment of rheumatoid
arthritis: 5-year results from the RAPID 1 trial and open-label
extension. Ann Rheum Dis. Aug 5–2013.(Epub ahead of print).
View Article : Google Scholar
|
|
5
|
Cordero MD, Sanchez-Alcazar JA,
Bautista-Ferrufino MR, et al: Acute oxidant damage promoted on
cancer cells by amitriptyline in comparison with some common
chemotherapeutic drugs. Anticancer Drugs. 21:932–944. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Otrocka M, Verschueren H and
Malicka-Blaszkiewicz M: The effect of methotrexate on actin and
invasiveness of hepatoma Morris 5123 cells in culture. Acta Biochim
Pol. 48:1051–1060. 2001.PubMed/NCBI
|
|
7
|
Jolivet J, Cowan KH, Curt GA, Clendeninn
NJ and Chabner BA: The pharmacology and clinical use of
methotrexate. N Engl J Med. 309:1094–1104. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Takemura Y and Jackman AL: Folate-based
thymidylate synthase inhibitors in cancer chemotherapy. Anticancer
Drugs. 8:3–16. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shirao K, Boku N, Yamada Y, et al:
Randomized phase III study of 5-fluorouracil continuous infusion
vs. sequential methotrexate and 5-fluorouracil therapy in far
advanced gastric cancer with peritoneal metastasis (JCOG0106). Jpn
J Clin Oncol. 43:972–980. 2013. View Article : Google Scholar
|
|
10
|
Chen Y, Zhang W, Gu J, et al: Enhanced
antitumor efficacy by methotrexate conjugated Pluronic mixed
micelles against KBv multidrug resistant cancer. Int J Pharm.
452:421–433. 2013. View Article : Google Scholar
|
|
11
|
Ding L, Hu XM, Wu H, et al: Combined
transfection of Bcl-2 siRNA and miR-15a oligonucleotides enhanced
methotrexate-induced apoptosis in Raji cells. Cancer Biol Med.
10:16–21. 2013.PubMed/NCBI
|
|
12
|
Florou D, Patsis C, Ardavanis A and
Scorilas A: Effect of doxorubicin, oxaliplatin, and methotrexate
administration on the transcriptional activity of BCL-2 family gene
members in stomach cancer cells. Cancer Biol Ther. 14:587–596.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Saez-Ayala M, Montenegro MF,
Sanchez-Del-Campo L, et al: Directed phenotype switching as an
effective antimelanoma strategy. Cancer Cell. 24:105–119. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yan KH, Lee LM, Hsieh MC, et al: Aspirin
antagonizes the cytotoxic effect of methotrexate in lung cancer
cells. Oncol Rep. 30:1497–1505. 2013.PubMed/NCBI
|
|
15
|
Ohgidani M, Komizu Y, Goto K and Ueoka R:
Residual powders from Shochu distillation remnants induce
apoptosis in human hepatoma cells via the caspase-independent
pathway. J Biosci Bioeng. 114:104–109. 2012.PubMed/NCBI
|
|
16
|
Yu VW and Ho WS: Tetrandrine inhibits
hepatocellular carcinoma cell growth through the caspase pathway
and G2/M phase. Oncol Rep. 29:2205–2210. 2013.PubMed/NCBI
|
|
17
|
Fan CM, Foster BK, Hui SK and Xian CJ:
Prevention of bone growth defects, increased bone resorption and
marrow adiposity with folinic acid in rats receiving long-term
methotrexate. PloS One. 7:e469152012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Okamura M, Hashimoto K, Shimada J and
Sakagami H: Apoptosis-inducing activity of cisplatin (CDDP) against
human hepatoma and oral squamous cell carcinoma cell lines.
Anticancer Res. 24:655–661. 2004.PubMed/NCBI
|
|
19
|
Papachristopoulou G, Talieri M and
Scorilas A: Significant alterations in the expression pattern of
kallikrein-related peptidase genes KLK4, KLK5 and KLK14 after
treatment of breast cancer cells with the chemotherapeutic agents
epirubicin, docetaxel and methotrexate. Tumour Biol. 34:369–378.
2013. View Article : Google Scholar
|
|
20
|
Wehner R, Bitterlich A, Meyer N, et al:
Impact of chemotherapeutic agents on the immunostimulatory
properties of human 6-sulfo LacNAc+(slan) dendritic
cells. Int J Cancer. 132:1351–1359. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang D and Loughran TP Jr: Large granular
lymphocytic leukemia: molecular pathogenesis, clinical
manifestations, and treatment. Hematology Am Soc Hematol Educ
Program. 2012.652–659. 2012.PubMed/NCBI
|
|
22
|
Xie XB, Yin JQ, Wen LL, et al: Critical
role of heat shock protein 27 in bufalin-induced apoptosis in human
osteosarcomas: a proteomic-based research. PloS One. 7:e473752012.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yang TM, Qi SN, Zhao N, et al: Induction
of apoptosis through caspase-independent or caspase-9-dependent
pathway in mouse and human osteosarcoma cells by a new nitroxyl
spin-labeled derivative of podophyllotoxin. Apoptosis. 18:727–738.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Green DR and Reed JC: Mitochondria and
apoptosis. Science. 281:1309–1312. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Thornberry NA and Lazebnik Y: Caspases:
enemies within. Science. 281:1312–1316. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tang CH, Hu CC, Wei CW and Wang JJ:
Synergism of Rana catesbeiana ribonuclease and IFN-γ triggers
distinct death machineries in different human cancer cells. FEBS
Lett. 579:265–270. 2005.
|
|
27
|
Yaoxian W, Hui Y, Yunyan Z, Yanqin L, Xin
G and Xiaoke W: Emodin induces apoptosis of human cervical cancer
hela cells via intrinsic mitochondrial and extrinsic death receptor
pathway. Cancer Cell Int. 13:712013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Beaudouin J, Liesche C, Aschenbrenner S,
Horner M and Eils R: Caspase-8 cleaves its substrates from the
plasma membrane upon CD95-induced apoptosis. Cell Death Differ.
20:599–610. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Yu YL, Wei CW, Chen YL, Chen MH and Yiang
GT: Immunotherapy of breast cancer by single delivery with
rAAV2-mediated interleukin-15 expression. Int J Oncol. 36:365–370.
2010.PubMed/NCBI
|
|
30
|
Zheng B, Wu L, Ma L, et al: Telekin
induces apoptosis associated with the mitochondria-mediated pathway
in human hepatocellular carcinoma cells. Biol Pharm Bull.
36:1118–1125. 2013. View Article : Google Scholar
|
|
31
|
Yiang GT, Harn HJ, Yu YL, et al:
Immunotherapy: rAAV2 expressing interleukin-15 inhibits HeLa cell
tumor growth in mice. J Biomed Sci. 16:472009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chen YX, Lv WG, Chen HZ, Ye F and Xie X:
Methotrexate induces apoptosis of human choriocarcinoma cell line
JAR via a mitochondrial pathway. Eur J Obstet Gynecol Reprod Biol.
143:107–111. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Shiu LY, Chang LC, Liang CH, Huang YS,
Sheu HM and Kuo KW: Solamargine induces apoptosis and sensitizes
breast cancer cells to cisplatin. Food Chem Toxicol. 45:2155–2164.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ehrhardt H, Wachter F, Maurer M, Stahnke K
and Jeremias I: Important role of caspase-8 for chemosensitivity of
ALL cells. Clin Cancer Res. 17:7605–7613. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Caglar Y, Ozgur H, Matur I, et al:
Ultrastructural evaluation of the effect of N-acetylcysteine on
methotrexate nephrotoxicity in rats. Histol Histopathol.
28:865–874. 2013.PubMed/NCBI
|
|
36
|
Kolli VK, Abraham P, Isaac B and
Selvakumar D: Neutrophil infiltration and oxidative stress may play
a critical role in methotrexate-induced renal damage. Chemotherapy.
55:83–90. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Tunali-Akbay T, Sehirli O, Ercan F and
Sener G: Resveratrol protects against methotrexate-induced hepatic
injury in rats. J Pharm Pharm Sci. 13:303–310. 2010.PubMed/NCBI
|
|
38
|
Ciralik H, Bulbuloglu E, Cetinkaya A,
Kurutas EB, Celik M and Polat A: Effects of N-acetylcysteine on
methotrexate-induced small intestinal damage in rats. Mt Sinai J
Med. 73:1086–1092. 2006.PubMed/NCBI
|
|
39
|
Cetinkaya A, Kurutas EB, Bulbuloglu E and
Kantarceken B: The effects of N-acetylcysteine on
methotrexate-induced oxidative renal damage in rats. Nephrol Dial
Transplant. 22:284–285. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wu CS, Yen CJ, Chou RH, et al:
Cancer-associated carbohydrate antigens as potential biomarkers for
hepatocellular carcinoma. PloS One. 7:e394662012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Pyrhonen S, Kuitunen T, Nyandoto P and
Kouri M: Randomised comparison of fluorouracil, epidoxorubicin and
methotrexate (FEMTX) plus supportive care with supportive care
alone in patients with non-resectable gastric cancer. Br J Cancer.
71:587–591. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lu Y, Sun J, Petrova K, et al:
Metabolomics evaluation of the effects of green tea extract on
acetaminophen-induced hepatotoxicity in mice. Food Chem Toxicol.
62:707–721. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Mukhopadhyay PK, Dey A, Mukherjee S and
Pradhan NK: The effect of coadministration of α-tocopherol and
ascorbic acid on arsenic trioxide-induced testicular toxicity in
adult rats. J Basic Clin Physiol Pharmacol. 24:245–253. 2013.
|
|
44
|
Kim H, Bae S, Kim Y, et al: Vitamin C
prevents stress-induced damage on the heart caused by the death of
cardiomyocytes, through down-regulation of the excessive production
of catecholamine, TNF-α, and ROS production in Gulo(−/−) mice. Free
Radic Biol Med. 65C:573–583. 2013.PubMed/NCBI
|
|
45
|
Eroglu S, Pandir D, Uzun FG and Bas H:
Protective role of vitamins C and E in diclorvos-induced oxidative
stress in human erythrocytes in vitro. Biol Res. 46:33–38.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Murata W, Tanaka T, Kubo I and Fujita K:
Protective effects of alpha-tocopherol and ascorbic acid against
cardol-induced cell death and reactive oxygen species generation in
Staphylococcus aureus. Planta Med. 79:768–774. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Hattiwale SH, Saha S, Yendigeri SM, Jargar
JG, Dhundasi SA and Das KK: Protective effect of L-ascorbic acid on
nickel induced pulmonary nitrosative stress in male albino rats.
Biometals. 26:329–336. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Alexander B, Fishman AI, Eshghi M,
Choudhury M and Konno S: Induction of cell death in renal cell
carcinoma with combination of D-fraction and vitamin C. Integr
Cancer Ther. 12:442–448. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Nagappan A, Park KI, Park HS, et al:
Vitamin C induces apoptosis in AGS cells by down-regulation of
14-3-3σ via a mitochondrial dependent pathway. Food Chem.
135:1920–1928. 2012.PubMed/NCBI
|
|
50
|
Vetvicka V and Vetvickova J: Combination
of glucan, resveratrol and vitamin C demonstrates strong anti-tumor
potential. Anticancer Res. 32:81–87. 2012.PubMed/NCBI
|
|
51
|
Lee WJ: The prospects of vitamin C in
cancer therapy. Immune Netw. 9:147–152. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Li W, Wu JX and Tu YY: Synergistic effects
of tea polyphenols and ascorbic acid on human lung adenocarcinoma
SPC-A-1 cells. J Zhejiang Univ Sci B. 11:458–464. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wei CW, Lin CC, Yu YL, et al:
n-Butylidenephthalide induced apoptosis in the A549 human
lung adenocarcinoma cell line by coupled down-regulation of AP-2α
and telomerase activity. Acta Pharmacol Sin. 30:1297–1306. 2009.
View Article : Google Scholar
|
|
54
|
Yu YL, Su KJ, Chen CJ, et al: Synergistic
anti-tumor activity of isochaihulactone and paclitaxel on human
lung cancer cells. J Cell Physiol. 227:213–222. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Yiang GT, Chen YH, Chou PL, Chang WJ, Wei
CW and Yu YL: The NS3 protease and helicase domains of Japanese
encephalitis virus trigger cell death via caspase dependent and
independent pathways. Mol Med Rep. 7:826–830. 2013.PubMed/NCBI
|
|
56
|
Yiang GT, Yu YL, Hu SC, Chen MH, Wang JJ
and Wei CW: PKC and MEK pathways inhibit caspase-9/-3-mediated
cytotoxicity in differentiated cells. FEBS Lett. 582:881–885. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Chen KH, Li PC, Lin WH, Chien CT and Low
BH: Depression by a green tea extract of alcohol-induced oxidative
stress and lipogenesis in rat liver. Biosci Biotechnol Biochem.
75:1668–1676. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lin BR, Yu CJ, Chen WC, et al: Green tea
extract supplement reduces D-galactosamine-induced acute liver
injury by inhibition of apoptotic and proinflammatory signaling. J
Biomed Sci. 16:352009. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Islam MS, Haq SA, Islam MN, et al:
Comparative efficacy of subcutaneous versus oral methotrexate in
active rheumatoid arthritis. Mymensingh Med J. 22:483–488.
2013.PubMed/NCBI
|
|
60
|
Yiang GT, Yu YL, Chou PL, et al: The
cytotoxic protein can induce autophagocytosis in addition to
apoptosis in MCF-7 human breast cancer cells. In Vivo; 26:403–409.
2012.PubMed/NCBI
|
|
61
|
Wei CW, Hu CC, Tang CH, Lee MC and Wang
JJ: Induction of differentiation rescues HL-60 cells from Rana
catesbeiana ribonuclease-induced cell death. FEBS Lett.
531:421–426. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Cetinkaya A, Bulbuloglu E, Kurutas EB and
Kantarceken B: N-acetylcysteine ameliorates methotrexate-induced
oxidative liver damage in rats. Med Sci Monit. 12:BR274–BR278.
2006.PubMed/NCBI
|
|
63
|
Chen J, Xiao XQ, Deng CM, Su XS and Li GY:
Downregulation of xIAP expression by small interfering RNA inhibits
cellular viability and increases chemosensitivity to methotrexate
in human hepatoma cell line HepG2. J Chemother. 18:525–531. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Miller KD, Loehrer PJ, Gonin R, et al: A
phase II study of weekly oral methotrexate and zidovudine (AZT) in
advanced adenocarcinoma of the pancreas and hepatocellular
carcinoma. Invest New Drugs. 14:207–212. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Muller M, Strand S, Hug H, et al:
Drug-induced apoptosis in hepatoma cells is mediated by the CD95
(APO-1/Fas) receptor/ligand system and involves activation of
wild-type p53. J Clin Invest. 99:403–413. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wang Y, Chen H, Liu Y, et al: pH-sensitive
pullulan-based nanoparticle carrier of methotrexate and
combretastatin A4 for the combination therapy against
hepatocellular carcinoma. Biomaterials. 34:7181–7190. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhao R, Hanscom M and Goldman ID: The
relationship between folate transport activity at low pH and
reduced folate carrier function in human Huh7 hepatoma cells.
Biochim Biophys Acta. 1715:57–64. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Aden DP, Fogel A, Plotkin S, Damjanov I
and Knowles BB: Controlled synthesis of HBsAg in a differentiated
human liver carcinoma-derived cell line. Nature. 282:615–616. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Ponchel F, Puisieux A, Tabone E, et al:
Hepatocarcinoma-specific mutant 53-249ser induces mitotic activity
but has no effect on transforming growth factor β 1-mediated
apoptosis. Cancer Res. 54:2064–2068. 1994.PubMed/NCBI
|
|
70
|
Held LA, Rizzieri D, Long GD, et al: A
Phase I study of arsenic trioxide (Trisenox), ascorbic acid, and
bortezomib (Velcade) combination therapy in patients with
relapsed/refractory multiple myeloma. Cancer Invest. 31:172–176.
2013. View Article : Google Scholar
|
|
71
|
Volta V, Ranzato E, Martinotti S, et al:
Preclinical demonstration of synergistic active nutrients/drug
(AND) combination as a potential treatment for malignant pleural
mesothelioma. PloS One. 8:e580512013. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Vuyyuri SB, Rinkinen J, Worden E, Shim H,
Lee S and Davis KR: Ascorbic acid and a cytostatic inhibitor of
glycolysis synergistically induce apoptosis in non-small cell lung
cancer cells. PloS One. 8:e670812013. View Article : Google Scholar : PubMed/NCBI
|