|
1
|
Lin NN, Wang P, Zhao D, Zhang FJ, Yang K
and Chen R: Significance of oral cancer-associated fibroblasts in
angiogenesis, lymphangiogenesis, and tumor invasion in oral
squamous cell carcinoma. J Oral Pathol Med. 46:21–30. 2017.
View Article : Google Scholar
|
|
2
|
Haddad RI and Shin DM: Recent advances in
head and neck cancer. N Engl J Med. 359:1143–1154. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Döbrossy L: Epidemiology of head and neck
cancer: Magnitude of the problem. Cancer Metastasis Rev. 24:9–17.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rodrigues-Lisoni FC, Peitl P Jr, Vidotto
A, Polachini GM, Maniglia JV, Carmona-Raphe J, Cunha BR, Henrique
T, Souza CF, Teixeira RA, et al Head and Neck Genome Project
GENCAPO: Genomics and proteomics approaches to the study of
cancer-stroma interactions. BMC Med Genomics. 3:142010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kalluri R and Zeisberg M: Fibroblasts in
cancer. Nat Rev Cancer. 6:392–401. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hanna E, Quick J and Libutti SK: The
tumour microenvironment: A novel target for cancer therapy. Oral
Dis. 15:8–17. 2009. View Article : Google Scholar
|
|
7
|
Zhou B, Chen WL, Wang YY, Lin ZY, Zhang
DM, Fan S and Li JS: A role for cancer-associated fibroblasts in
inducing the epithelial-to-mesenchymal transition in human tongue
squamous cell carcinoma. J Oral Pathol Med. 43:585–592. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vered M, Dayan D, Yahalom R, Dobriyan A,
Barshack I, Bello IO, Kantola S and Salo T: Cancer-associated
fibroblasts and epithelial-mesenchymal transition in metastatic
oral tongue squamous cell carcinoma. Int J Cancer. 127:1356–1362.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li H, Zhang J, Chen SW, Liu LL, Li L, Gao
F, Zhuang SM, Wang LP, Li Y and Song M: Cancer-associated
fibroblasts provide a suitable microenvironment for tumor
development and progression in oral tongue squamous cancer. J
Transl Med. 13:1982015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
De Wever O and Mareel M: Role of tissue
stroma in cancer cell invasion. J Pathol. 200:429–447. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jewett A, Head C and Cacalano NA: Emerging
mechanisms of immunosuppression in oral cancers. J Dent Res.
85:1061–1073. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
De Wever O, Demetter P, Mareel M and
Bracke M: Stromal myofibroblasts are drivers of invasive cancer
growth. Int J Cancer. 123:2229–2238. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wheeler SE, Shi H, Lin F, Dasari S,
Bednash J, Thorne S, Watkins S, Joshi R and Thomas SM: Enhancement
of head and neck squamous cell carcinoma proliferation, invasion,
and metastasis by tumor-associated fibroblasts in preclinical
models. Head Neck. 36:385–392. 2014. View Article : Google Scholar
|
|
14
|
Sappino AP, Skalli O, Jackson B, Schürch W
and Gabbiani G: Smooth-muscle differentiation in stromal cells of
malignant and non-malignant breast tissues. Int J Cancer.
41:707–712. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lazard D, Sastre X, Frid MG, Glukhova MA,
Thiery JP and Koteliansky VE: Expression of smooth muscle-specific
proteins in myoepithelium and stromal myofibroblasts of normal and
malignant human breast tissue. Proc Natl Acad Sci USA. 90:999–1003.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mueller MM and Fusenig NE: Friends or foes
- bipolar effects of the tumour stroma in cancer. Nat Rev Cancer.
4:839–849. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rønnov-Jessen L, Petersen OW and Bissell
MJ: Cellular changes involved in conversion of normal to malignant
breast: Importance of the stromal reaction. Physiol Rev. 76:69–125.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
el-Naggar AK, Lai S, Luna MA, Zhou XD,
Weber RS, Goepfert H and Batsakis JG: Sequential p53 mutation
analysis of pre-invasive and invasive head and neck squamous
carcinoma. Int J Cancer. 64:196–201. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kellermann MG, Sobral LM, da Silva SD,
Zecchin KG, Graner E, Lopes MA, Kowalski LP and Coletta RD: Mutual
paracrine effects of oral squamous cell carcinoma cells and normal
oral fibroblasts: Induction of fibroblast to myofibroblast
transdifferentiation and modulation of tumor cell proliferation.
Oral Oncol. 44:509–517. 2008. View Article : Google Scholar
|
|
20
|
Daly AJ, McIlreavey L and Irwin CR:
Regulation of HGF and SDF-1 expression by oral
fibroblasts–implications for invasion of oral cancer. Oral Oncol.
44:646–651. 2008. View Article : Google Scholar
|
|
21
|
Thiery JP, Acloque H, Huang RY and Nieto
MA: Epithelial-mesenchymal transitions in development and disease.
Cell. 139:871–890. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Potenta S, Zeisberg E and Kalluri R: The
role of endothelial-to-mesenchymal transition in cancer
progression. Br J Cancer. 99:1375–1379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kalluri R and Weinberg RA: The basics of
epithelial-mesenchymal transition. J Clin Invest. 119:1420–1428.
2009. View
Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chen C, Zimmermann M, Tinhofer I, Kaufmann
AM and Albers AE: Epithelial-to-mesenchymal transition and cancer
stem(-like) cells in head and neck squamous cell carcinoma. Cancer
Lett. 338:47–56. 2013. View Article : Google Scholar
|
|
25
|
Lee JM, Dedhar S, Kalluri R and Thompson
EW: The epithelial-mesenchymal transition: New insights in
signaling, development, and disease. J Cell Biol. 172:973–981.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yang J, Mani SA, Donaher JL, Ramaswamy S,
Itzykson RA, Come C, Savagner P, Gitelman I, Richardson A and
Weinberg RA: Twist, a master regulator of morphogenesis, plays an
essential role in tumor metastasis. Cell. 117:927–939. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang C, Huang H, Huang Z, Wang A, Chen X,
Huang L, Zhou X and Liu X: Tumor budding correlates with poor
prognosis and epithelial-mesenchymal transition in tongue squamous
cell carcinoma. J Oral Pathol Med. 40:545–551. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Lydiatt WM, Patel SG, O'Sullivan B,
Brandwein MS, Ridge JA, Migliacci JC, Loomis AM and Shah JP: Head
and neck cancers-major changes in the American Joint Committee on
cancer eighth edition cancer staging manual. CA Cancer J Clin.
67:122–37. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Brierley JD, Gospodarowicz MK and
Wittekind C: TNM Classification of Malignant Tumours. 8th edition.
Wiley-Blackwell; Chichester: 2017
|
|
30
|
Lim KP, Cirillo N, Hassona Y, Wei W,
Thurlow JK, Cheong SC, Pitiyage G, Parkinson EK and Prime SS:
Fibroblast gene expression profile reflects the stage of tumour
progression in oral squamous cell carcinoma. J Pathol. 223:459–469.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kawashiri S, Tanaka A, Noguchi N, Hase T,
Nakaya H, Ohara T, Kato K and Yamamoto E: Significance of stromal
desmoplasia and myofibroblast appearance at the invasive front in
squamous cell carcinoma of the oral cavity. Head Neck.
31:1346–1353. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang J, Min A, Gao S and Tang Z: Genetic
regulation and potentially therapeutic application of
cancer-associated fibroblasts in oral cancer. J Oral Pathol Med.
43:323–334. 2014. View Article : Google Scholar
|
|
33
|
Olumi AF, Grossfeld GD, Hayward SW,
Carroll PR, Tlsty TD and Cunha GR: Carcinoma-associated fibroblasts
direct tumor progression of initiated human prostatic epithelium.
Cancer Res. 59:5002–5011. 1999.PubMed/NCBI
|
|
34
|
Takahashi H, Sakakura K, Kudo T, Toyoda M,
Kaira K, Oyama T and Chikamatsu K: Cancer-associated fibroblasts
promote an immunosuppressive microenvironment through the induction
and accumulation of protumoral macrophages. Oncotarget.
8:8633–8647. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Johansson AC, Ansell A, Jerhammar F, Lindh
MB, Grénman R, Munck-Wikland E, Östman A and Roberg K:
Cancer-associated fibroblasts induce matrix
metalloproteinase-mediated cetuximab resistance in head and neck
squamous cell carcinoma cells. Mol Cancer Res. 10:1158–1168. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Sinha N, Mukhopadhyay S, Das DN, Panda PK
and Bhutia SK: Relevance of cancer initiating/stem cells in
carcinogenesis and therapy resistance in oral cancer. Oral Oncol.
49:854–862. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Matsushita Y, Yanamoto S, Takahashi H,
Yamada S, Naruse T, Sakamoto Y, Ikeda H, Shiraishi T, Fujita S,
Ikeda T, et al: A clinicopathological study of perineural invasion
and vascular invasion in oral tongue squamous cell carcinoma. Int J
Oral Maxillofac Surg. 44:543–548. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Velez-delValle C, Marsch-Moreno M,
Castro-Muñozledo F, Galván-Mendoza IJ and Kuri-Harcuch W:
Epithelial cell migration requires the interaction between the
vimentin and keratin intermediate filaments. Sci Rep. 6:243892016.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Ramaekers FC, Haag D, Kant A, Moesker O,
Jap PH and Vooijs GP: Coexpression of keratin- and vimentin-type
intermediate filaments in human metastatic carcinoma cells. Proc
Natl Acad Sci USA. 80:2618–2622. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Pagan R, Martín I, Alonso A, Llobera M and
Vilaró S: Vimentin filaments follow the preexisting cytokeratin
network during epithelial-mesenchymal transition of cultured
neonatal rat hepatocytes. Exp Cell Res. 222:333–344. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
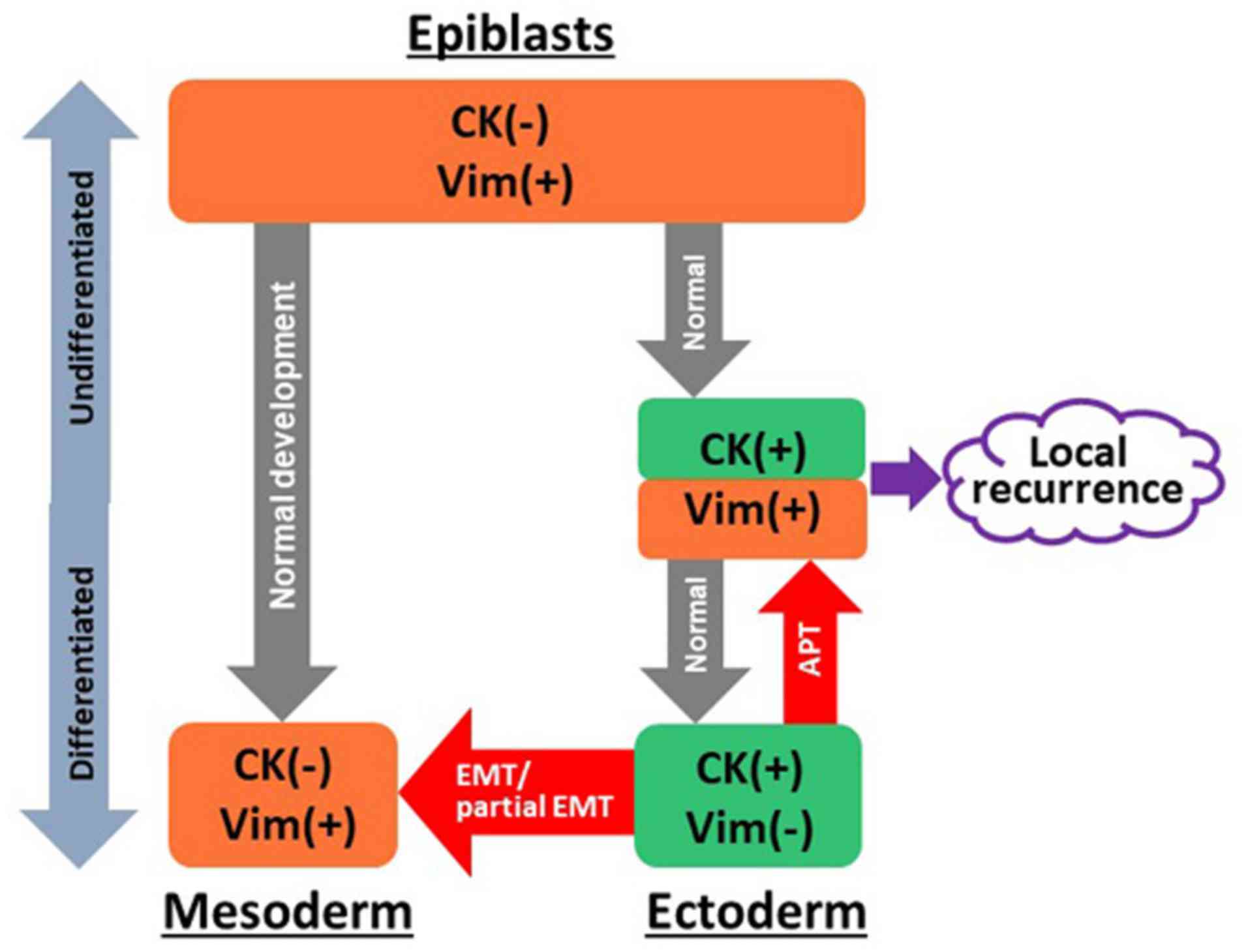
Grigore AD, Jolly MK, Jia D, Farach-Carson
MC and Levine H: Tumor Budding: The Name is EMT. Partial EMT J Clin
Med. 5:E512016. View Article : Google Scholar
|
|
42
|
Pradella D, Naro C, Sette C and Ghigna C:
EMT and stemness: Flexible processes tuned by alternative splicing
in development and cancer progression. Mol Cancer. 16:82017.
View Article : Google Scholar : PubMed/NCBI
|