1. Introduction to electronic
cigarettes
Electronic cigarettes (ECIGs), also known as
‘smokeless cigarettes,’ ‘e-hookahs,’ ‘vape pens’ and ‘vapes’, are
electronic devices that heat and vaporize a solution that usually
contains a mixture of glycerol, propylene glycol, water, flavors
and various nicotine concentrations (1). The first electronic cigarette patents
date back to 1965(2). The concept
of this new product was a ‘smokeless nontobacco cigarette’, to
provide ‘a safe and harmless tool and method for smoking’ (3). However, ECIGs were not commercially
available until 2004. Since they have been marketed, they have
become one of the products with the highest commercial growth rate
(4).
2. ECIGs components, function and
categories
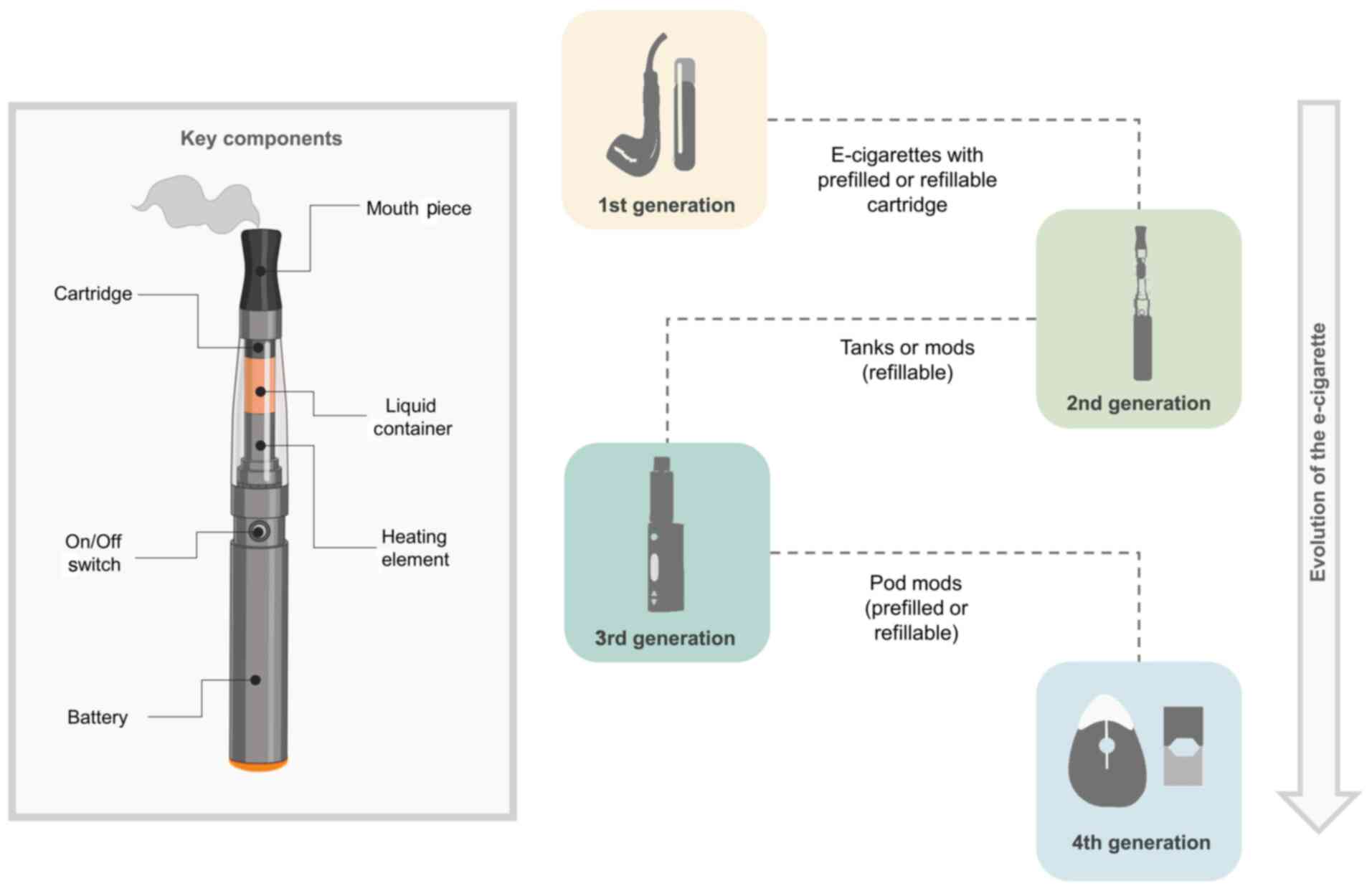
ECIG devices have 3 key components: A power source,
a cartridge containing an atomizer to heat a solution that
typically contains nicotine and a mouthpiece. The liquid solution
(often termed e-liquid or e-juice) that is stored in the cartridge,
heats up in the device producing an aerosol inhaled by the user
through the mouthpiece (Fig. 1)
(5).
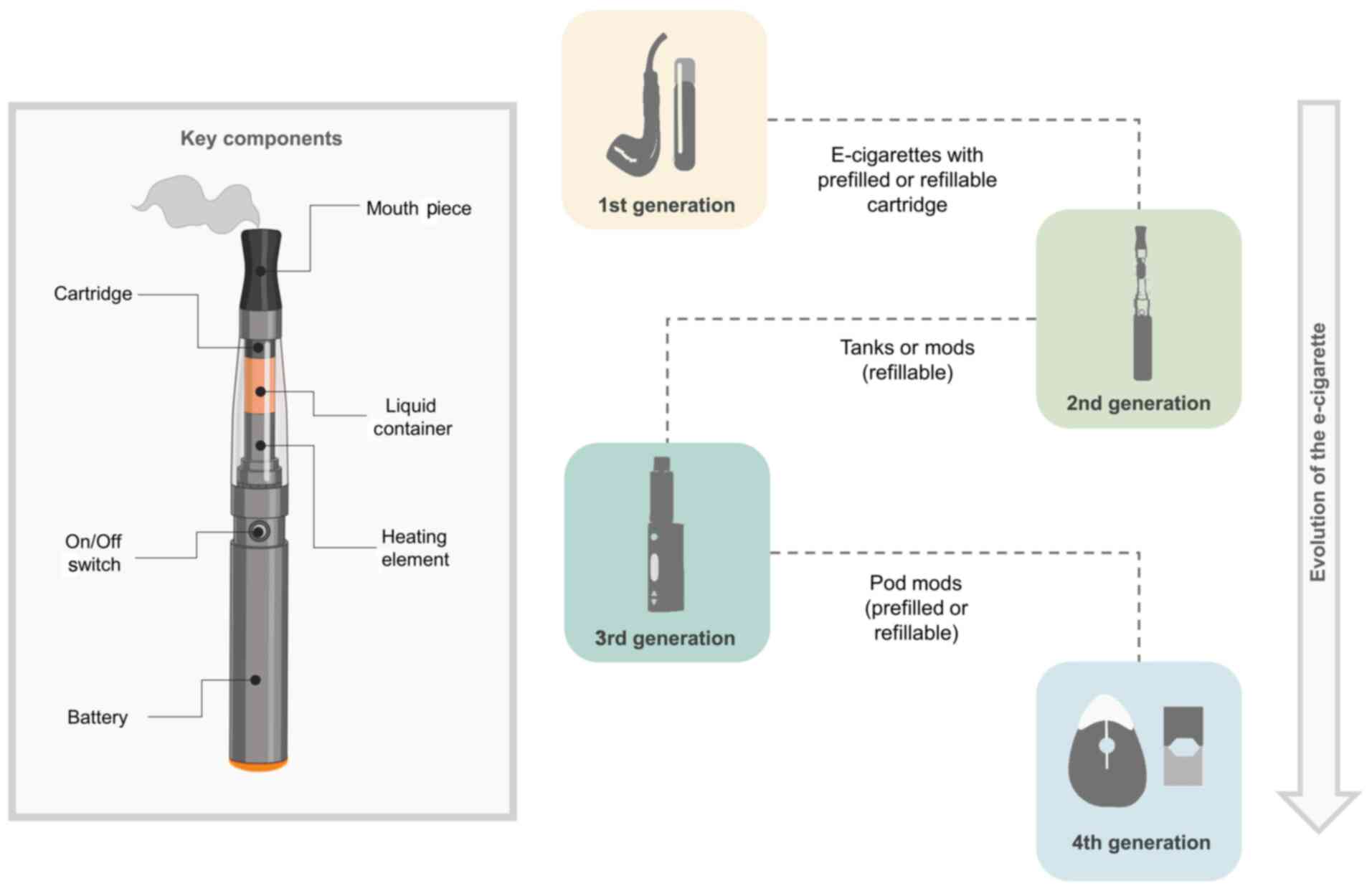 | Figure 1ECIGs: Evolution and components.
Throughout the evolution of ECIGs, essential parts such as the
mouthpiece, cartridge tank (holds the liquid juice), heating
element, on/off switch, cartridge, and battery remain. The first
generation are non-refillable devices designed for single use that
mimic the appearance of traditional cigarettes. The second
generation are rechargeable devices, with interchangeable substance
cartridges and interchangeable battery spare parts. The third
generation are modifiable devices (‘mods’) that allow users to
customize the substances in the device with a tank that contributes
to the generation of increased vapor and delivery of substances
such as nicotine. Finally, fourth generation are compact
capsule-like devices (Pod Mods) attached via magnets that demand
less energy and generate more steam. Pod Mods typically use
nicotine salts instead of the free-base nicotine used in most
others ECIGs. The figure was modified from CDC, E-Cigarette, or
Vaping, Products Visual Dictionary, 2019 (https://www.cdc.gov). Created with BioRender.com. ECIGs, electronic cigarettes. |
In the evolution of ECIGs, companies have used
technology to improve devices. Four generations of ECIGs can be
identified. The first generation, originally designed to imitate
the conventional cigarette in appearance, is also known as the
young category, or Cig-a-like. It was built with a disposable
filter, an integrated atomizer, and cotton soaked in e-liquid
(6). The majority of Cig-a-likes
are built with low-voltage batteries and low-volume, non-refillable
reservoirs made of sponge-like polyfill (Fig. 1) (7).
The second generation had the enhancement of a
high-capacity rechargeable battery and a separated tank (6). As the years passed and ECIG technology
improved, third- and fourth-generation ‘intelligent vaping systems’
included new features, such as voltage regulation from 3.4 to 4.8
V, battery improvement (third generation), and better internal
device resistances (fourth generation) (Fig. 1) (6).
Fourth generation ECIGs were introduced in the last
5 years. Also known as ‘Pod-Mods’, they are new and highly popular.
Their main innovation is fusing atomizer and tank in a simplified
piece, known as a ‘Pod,’ that contains and vaporizes the e-liquid.
The Pod is fastened to an USB or to a tear-shaped rechargeable
battery. Another difference in ‘Pod-Mods’ is the use of a new
e-liquid formula with protonated nicotine. Inhaling these new
formulas do not cause the side-effects caused by high-nicotine
concentrations. This innovation increases acceptance rates and
increases the risk of addiction among young users (Fig. 1) (8).
Some ECIGs are designed to be totally disposable.
The majority of other ECIGs are reusable. The reusable contain a
rechargeable lithium battery and a replaceable vaporization
chamber, wicking system, and nicotine/flavoring cartridge (9).
A survey conducted by the National Youth Tobacco
Survey (NYTS) to estimate the prevalence of ECIGs in the United
States from 2011 to 2012 demonstrated that 1.78 million students
had used ECIGs in that time period. In 2012, approximately 160,000
students using ECIGs had never used conventional cigarettes
(10). In a recent study, 4.04
million high-school students and 840,000 middle-school students
were at that time using some tobacco product; ECIGs were used the
most (11).
3. Chemical compounds found in ECIGs
Along with characteristic tobacco odor and flavor
options, one of the most attractive features of ECIGs for younger
individuals is the perception that consumption has a ‘low risk’ to
health (12). While the use of
ECIGs does reduces consumption levels of toxic compounds compared
to traditional cigarettes, it remains a source of exposure to
harmful substances.
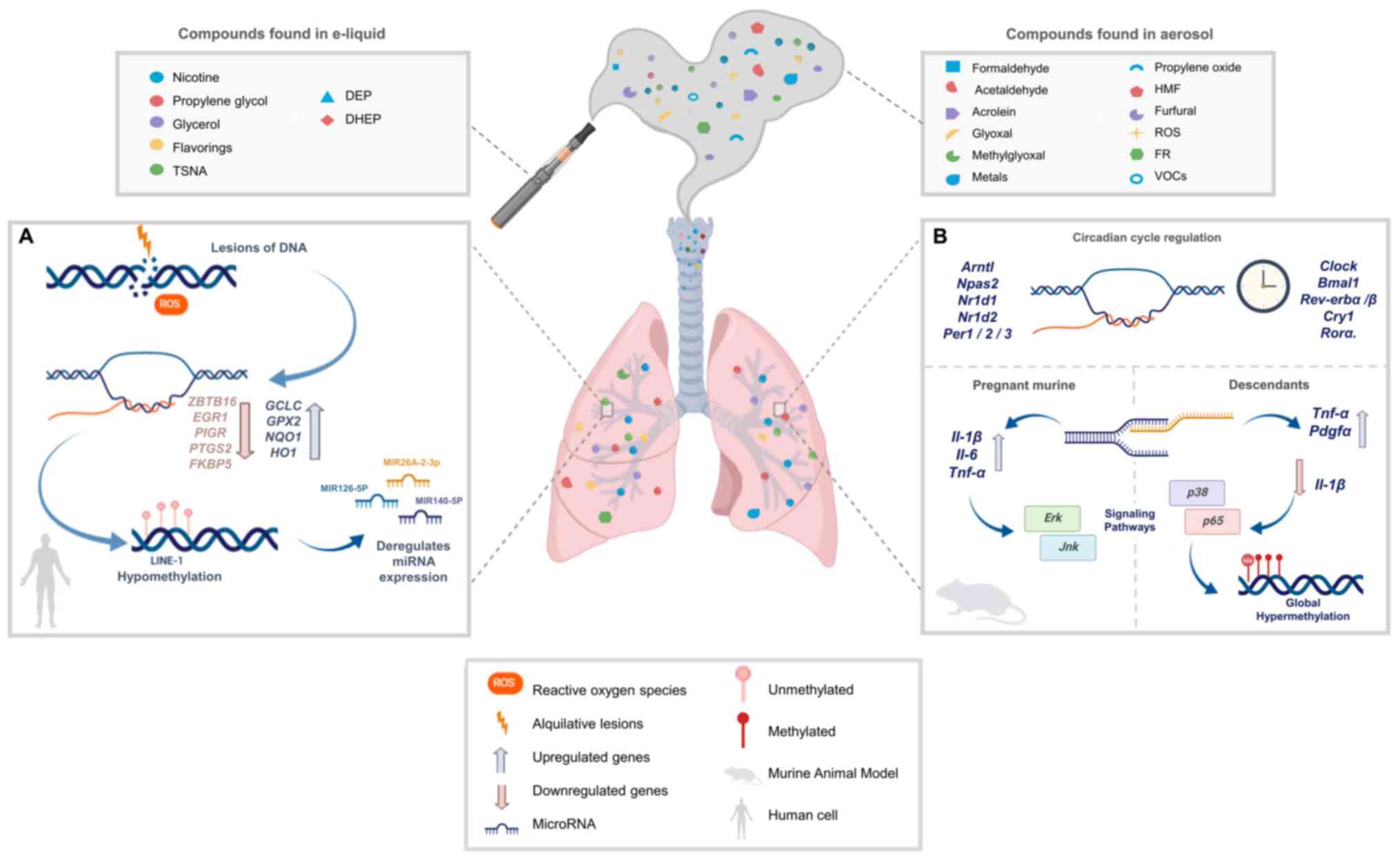
Some investigations have examined the chemical
composition of commercial e-liquids from >50 brands. An average
of 87 (from 60 to 113) chemical compounds were identified in ECIGs
cartridges, e-liquids and aerosols (13-15).
Compounds identified in ECIG liquids and aerosols include nicotine,
solvent vehicles such as propylene glycol (PG) and glycerol;
tobacco-specific nitrosamines (TSNAs), aldehydes, metals, volatile
organic compounds (VOCs), phenolic compounds, polycyclic aromatic
hydrocarbons (PAH), flavorings, and minor tobacco alkaloids
(Fig. 2) (13,16,17).
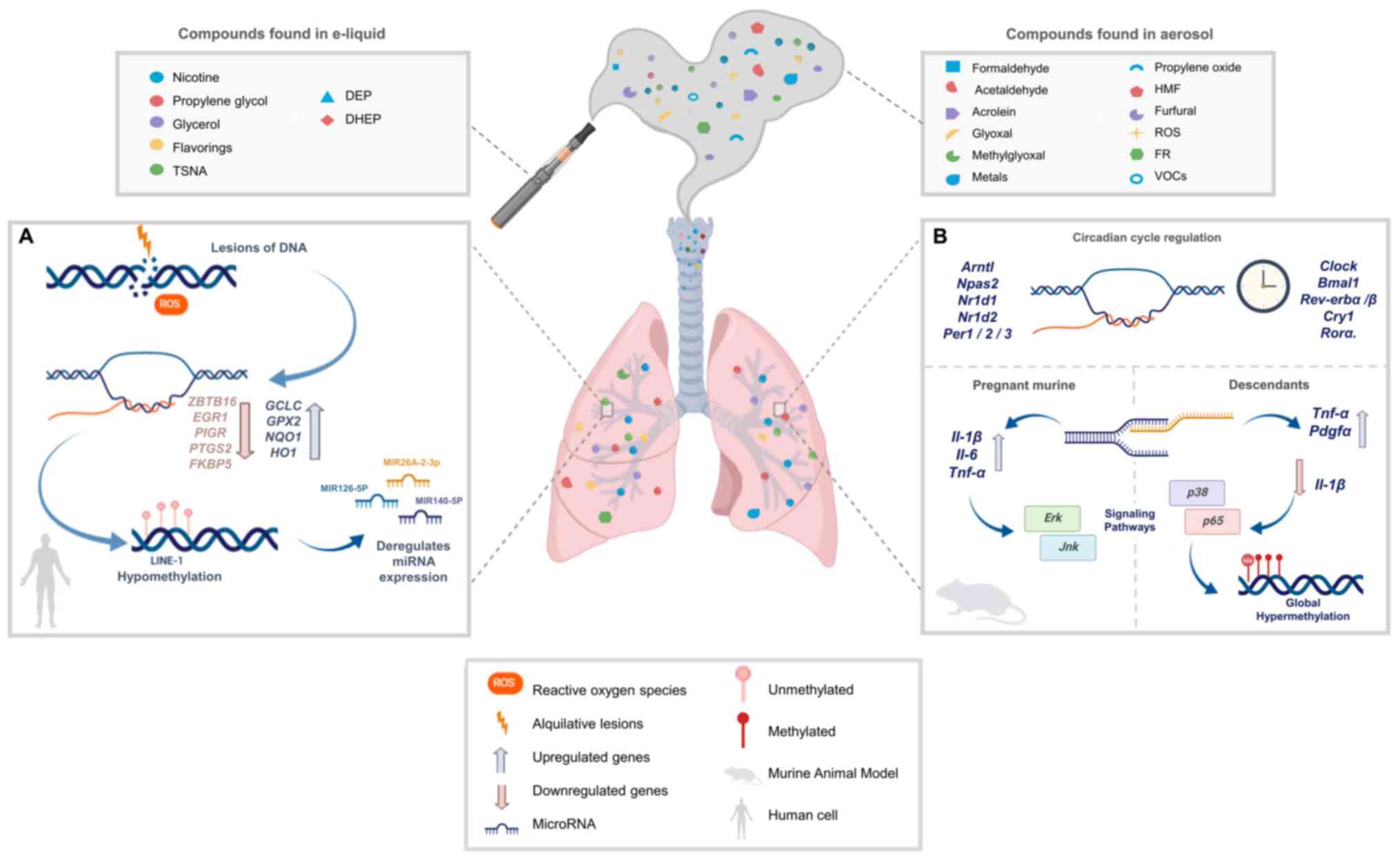 | Figure 2Pulmonary genetic and epigenetic
impact of chemical components derived from ECIGs. Summary of the
main chemical components found in e-liquids and aerosols and
schematic representation of their genetic and epigenetic effects,
which are evidenced in studies in (A) humans and (B) mice. (A)
Exposition of ECIGs aerosol in humans may cause oxidative and
alkylating lesions directly over the DNA. It also causes
transcriptome alterations, such as reduced expression of genes
related to the immune system and an increased expression of genes
involved in the oxidative stress response. As regards the effects
ECIGs on the epigenome, the hypomethylation of class I transposable
elements (LINE-1) and the dysregulation of miRNA expression should
be highlighted. (B) Following ECIGs aerosol exposition in a murine
model, the alteration of genes involved in control and correct
functioning of circadian rhythm is evidenced. Another murine model
demonstrated that ECIG aerosol intake was detrimental to fetal and
maternal respiratory health (56,57).
This effect was due to an induction of inflammatory response at
pulmonary tissue in mother and litter. Specifically, an increased
expression of IL-1β, IL-6 and TNF-α and altered ERK1/2 and JNK
pathways are being identified in mouse mothers. Also, an increase
of TNF-α and PDGFα expression, a decrease of IL-1β expression, and
a dysregulation of p38 and p65 pathways are identified in their
breed. Vapor produced by ECIGs leads to changes on the epigenetic
profile of exposed breed in utero, where a global
hypomethylation state is being shown. The figure was created with
BioRender.com. ECIGs, electronic cigarettes. |
Currently, there are >7,000 flavorings for ECIGs
(18), which are manufactured using
chemical compounds such as alcohols, acids, esters, lactones,
aldehydes, ketones, heterocycles and mercaptans (Table I). These flavorings, as well as
propylene glycol (PG) and glycerol, are classified as ‘generally
recognized as safe’ (GRAS) by the FDA (12,19),
which suggests that they are safe to consume if they are used as
food additives. However, other administrations, such as inhalation,
may be harmful. Although data on long-term inhalation exposure to
PG and glycerol is currently limited (20,21),
exposure to PG is known to cause irritation to the eyes and
respiratory tract (13,22), in addition to increasing the
probability of developing asthma (23-25).
 | Table IMain chemical compounds found in
electronic cigarettes. |
Table I
Main chemical compounds found in
electronic cigarettes.
| Chemical group | Chemical
compound | Source | Main health effects
from exposure | Respiratory or lung
irritant | (Refs.) |
|---|
| Acids | Butyric acid | E-liquid
flavors | Moderate skin and
eye irritation | No evidence | (13) |
| Alcohols | Menthol | | Skin irritation and
severe eye irritation | No evidence | (13) |
| | Benzaldehyde | | Aerosolized form
generates irritation in the membranes of the airways | Yes | (28) |
| | Cinnamaldehyde | | Damage to the
homeostasis of the respiratory system, increase in DNA breaks,
decrease in cell growth and increase in cell death | Yes | (27) |
| Heterocycles | Furfural | E-liquid
aerosol | Exhibits
tumorigenicity in mice | Yes | (13,29) |
| |
5-Hydroxymethylfurfural | | Exhibits
tumorigenicity in mice | Yes | (22,29) |
| | Maltol | | Cytotoxic | Yes | (13) |
| |
2-Acetylpyrrole | | Skin
irritation | Yes | |
| Solvents | Glycerol | E-liquid | Associated to
lipoid pneumonia Minimal squamous metaplasia of the epiglottis | Yes | (25) |
| | Propylene
glycol | | Increases the risk
of developing asthma and irritates eyes | Yes | (13,25) |
| | Ethylene
glycol | | Harmful effects in
animal models | Yes | (21) |
| Carbonyl | Formaldehyde | E-liquid
aerosol | Classified as a
human carcinogen (Group 1) | No evidence | (22) |
| | Acetaldehyde | | Classified as
possibly carcinogenic to humans (Group 2B) | No evidence | (22) |
| | Acrolein | | Causes irritation
of the nasal cavity and damages the lining of the lungs through
oxidative stress and its involved in COPD development | Yes | (13,41) |
| | Propylene
oxide | | Classified as
potentially carcinogenic by the IARC | Yes | (31) |
| | Glyoxal | | Shows
mutagenicity | No evidence | (36) |
| Nitrosamines
(TSNAs) |
N'-nitrosonornicotine (NNN) | E-liquid with
nicotine | Low levels have
been found. Are potent carcinogenic chemicals. Can cause throat or
mouth cancer | No evidence | (41,42) |
| | N'-nitrosoanabasine
(NAB) | | Classified as a
human carcinogen (Group 3) | No evidence | |
| VOCs | Benzene | E-liquid
aerosol | Classified as
highly carcinogenic by the IARC, related to depression of the CNS
when inhaled | Yes | (13,26) |
| | Methanol | | Increases the risk
of developing myeloid leukemia and affection of sexual organs, also
its metabolites are toxic and may cause eye damage | Yes | |
| Phthalates | Diethyl phthalate
(DEP) | E-liquid
package | Favors inflammation
and oxidative stress, and are risk factors | Yes | (44) |
| | Di-2-ethylhexyl
phthalate (DHEP) | | for the development
of neurological, gastrointestinal and asthma disorders. DHEP is
classified as probably carcinogenic | Yes | |
| Metals | Nickel | Probably from ECIGs
chamber | Impaired lung
function, classified as a human carcinogen (Group 1). | Yes | (45-48) |
| | Copper | | Mitochondrial
oxidative stress and DNA fragmentation | No evidence | |
| | Cadmium | | May cause toxicity
to multiple organs | | |
| | Manganese | | | | |
| | Aluminum | | | | |
| | Iron | | Impaired lung
function and fibrosis | Yes | |
Even more compounds (approximately 18) are observed
in the inhaled aerosols, given that additional chemicals are
generated at high temperatures during vaporization (14). Some are potentially harmful
chemicals and ultrafine particles, including carbonyl compounds,
VOCs, TSNAs, metals and silicates (Fig.
2) (26). These substances are
potentially toxic and carcinogenic, and they increase the risk of
respiratory and heart diseases (13). The heating of flavorings generates
other substances in quantities exceeding the maximum limit allowed,
including aldehydes, toxic furans, benzene, methanol and ethanol.
These can produce multiple adverse health effects (27-29).
When PG and glycerol are heated to high temperatures and
aerosolized, thermal dehydration reactions are facilitated, and
several toxic carbonyl compounds are generated (30). Recent studies in e-liquids have
found toxic carbonyls such as formaldehyde, acetaldehyde, acrolein,
glyoxal, and methylglyoxal, in addition to propylene oxide, all
known to be potentially carcinogenic and causing irritation of the
upper respiratory tract (Table I)
(22,31-36).
What is of concern is that the numbers of substances and their
concentrations are highly variable, due to the differences in the
manufacturing of ECIGs. Temperature can influence a higher
production of carbonyl compounds (31,37).
In some studies, as voltage rises to heat devices, formaldehyde,
acetaldehyde and acetone levels increase as much as 200 percent,
representing a major risk to health (38,39).
TSNAs are found in some ECIGs and have a high
carcinogenic potential. They form in the curing process during the
nitrosation of amines (40,41). Minor alkaloids have also been found;
however, their effects on health are currently unknown (30). Other relevant compounds are diethyl
phthalate (DEP) and di-2-ethylhexyl phthalate (DHEP). They probably
develop from the e-liquid package in the production process and
have serious adverse effects on health (42,43).
Various studies have detected different metals in
e-liquids and their aerosols (Table
I) (13,44). The levels and concentrations of
these metals, except for cadmium, are higher compared to those in
traditional cigarettes. These metals can originate in the chamber
that aerosolizes the e-liquid, or from other ECIGs components that
infiltrate the aerosol (13,45).
One study reported that these metals might be inhaled, affecting
normal chromium and nickel body levels, resulting in high toxicity
to multiple organs (46). Copper is
specifically associated with mitochondrial oxidative stress and DNA
fragmentation (13,46,47).
Finally, reactive oxygen species (ROS) and free
radicals (FRs) are produced by normal aerobic metabolism and can
also be derived from external sources, such as tobacco smoke. The
increase in ROS and FR creates homeostatic imbalance and oxidative
stress, which exerts negative effects, such as breakdowns in
cellular function and cellular damage (48). This may trigger cardiovascular and
respiratory diseases (chronic obstructive pulmonary disease,
asthma) and even cancer development, due to DNA damage.
In summary, the majority of ECIGs, regardless of
their nicotine content, contain and emit potentially toxic
substances that may, with long-term exposure, alter the homeostasis
of certain organs and can cause damage. These changes in
microenvironment exposure may alter the epigenome, transcriptome,
and even the genome itself. Those effects of vaping will be the
main focus of discussion below.
4. Noxious effects of ECIGs on DNA
Aerosol generated by ECIGs is composed of various
toxic agents. Some are reported to exert an effect at the cellular
level similar to that of tobacco smoke, principally increased
levels of oxidative stress and inflammation (49), and to lead to changes in gene
expression (50,51).
For this reason, it is essential to determine
whether ECIG aerosol exposure can cause DNA damage to pulmonary and
oral epithelial cells. Ganapathy et al (52) determined the genotoxicity and
mechanisms induced by ECIG aerosol extract in human epithelial
normal bronchial cells (Nuli1) and human oral squamous cell
carcinoma (UM-SCC-1). After 1 h of aerosol exposure in both cell
types, oxidative and alkylation DNA lesions were observed. It was
also shown that DNA damage was dose-dependent, as more damage was
evidenced as exposure to ECIG aerosols increased (Table II). These harmful effects may be
associated with formaldehyde and the ROS levels in aerosols
(Fig. 2A) (52).
 | Table IISummary of main studies on the
effects of electronic cigarette smoking on genetic, epigenomic and
transcriptomic alterations. |
Table II
Summary of main studies on the
effects of electronic cigarette smoking on genetic, epigenomic and
transcriptomic alterations.
| Study model | Aim of the
study | Type of
exposure/study | Genotoxic or
epigenotoxic effect | Target
gene/pathway | Main findings | (Refs.) |
|---|
| NHBE cells and
human oral squamous carcinoma cells | To determine the
genotoxicity induced by ECIGs aerosol extracts on human oral and
NHBE cells | 1 h to ECIGs
aerosol extract (doses equivalent to 1, 10, or 100 puffs/5
liters) | Oxidative and
alkylation lesions of DNA | n/a | Suppression of
cellular antioxidant defenses and significant DNA damage | (52) |
| Nasal epithelial
cells from tobacco cigarette smokers, ECIGs smokers, and
nonsmokers | To determine the
effect of tobacco and ECIG smoking on expression of genes related
to immune response in nasal epithelial cells | Average 12
cigarettes smoked per day/average 200 ECIG puffs per day | Decrease in
immune-related gene expression in both groups. Most of these genes
codify for transcription factors | Tobacco group:
Decrease in the expression of 53 genes (EGR1, DPP4,
CXCL2, CX3CR1, CD28, etc.). ECIGs group:
Decrease in the expression of additional 305 unique genes
(ZBTB16, EGR1, PIGR, PTGS2,
FKBP5, etc.) | Possible induction
of immunosuppression states due to repression of genes involved in
the immune response in the nasal mucous membrane | (54) |
| BALB/c female
mice | To assess the
effect of ECIGs use on circadian molecular clock | Nicotine-free and
flavor-free ECIG steam at various solvent concentrations, 2 h per
day for 8 weeks | Inhalation of both
solvents modulates the expression of genes that play an important
role in the circadian cycle machinery and regulation | Alteration in
circadian molecular clock characteristic genes, such as
Arntl, Npas2, Nr1d1, Nr1d2, Per1, Per2,
and Per3 | Major solvents used
in ECIGs changes the expression of some circadian molecular clock
genes | (57) |
| C57BL/6J murine
model | To determine the
impact of WPS and ECIGs vapor on pulmonary circadian molecular
clock disruption | E-liquid containing
25 mg/ml nicotine vs. 100% nicotine-free PG base, 2 h per day for 3
days | Alterations in the
expression of genes related to the circadian clock machinery and
regulation of the lungs | Changes in the
expression patterns of genes as Clock and Bmal1.
Upregulation of the genes Rev-erbα, Rev-erbβ, Per2,
Cry1, and Rorα | Alteration
circadian molecular clock genes expression in the lungs, after
acute exposure to WPS and ECIGs vapor containing nicotine | (56) |
The significant mutagenic capacity of toxic
compounds in ECIGs has not yet been described, at least to the best
of our knowledge. However, conventional smoking has been proven to
cause multiple epigenetic alterations. Given that ECIGs contain
numerous noxious chemical compounds, they can alter epigenetic
mechanisms that regulate gene expression as well.
Toxic chemicals in ECIGs can generate changes in the
cellular microenvironment, leading to deregulation in gene
expression through epigenetic alterations, such as DNA aberrant
methylation or hypomethylation, histone modifications, chromatin
remodeling and microRNA (miRNA/miR) expression. Alterations in
these mechanisms can support the development of different
pathologies, particularly in the lungs (53).
5. Effect ECIGs on genes involved in the
immune response
The study by Martin et al (54) in 2016 on conventional smokers,
non-smokers and ECIG users, compared the expression of 597 genes in
nasal mucous epithelial cells related to the immune response. The
expression of 53 genes in smokers and 305 in ECIGs users decreased
(Table II).
It is important to note that the decrease in the
expression of genes associated with exposure to conventional
cigarettes was also observed in cells exposed to ECIGs. The levels
of the early growth response protein 1 (EGR1), dipeptidyl
peptidase-4 (DPP4), chemokine (C-X-C motif) ligand 2
(CXCL2), CX3C chemokine receptor 1 (CX3CR1) and
cluster of differentiation 28 (CD28) genes were shown to be
downregulated in conventional cigarette smokers, while the levels
of the zinc finger and BTB domain-containing protein 16
(ZBTB16), EGR1, polymeric immunoglobulin receptor
(PIGR), prostaglandin-endoperoxide synthase 2 (PTGS2)
and FKBP prolyl isomerase 5 (FKBP5) genes were downregulated
in ECIG users. The majority of the downregulated genes in cigarette
smokers and ECIG users code for transcription factors (TFs) that
regulate downstream genes associated with the immune system
(54). One of these is the
colony-stimulating factor 1 (CSF-1), a gene that codes for a
cytokine involved in the activation of innate immunity in infection
response (55). The CSF-1 is
a target of EFR1 TF, the expression of which is significantly
decreased in smokers and ECIG users (Fig. 2A). This suggests that the use of
ECIGs may induce immunosuppression states associated with the
suppression of the expression of genes involved in the immune
response of nasal mucous cells. This may increase susceptibility to
various infections (Table II)
(54).
6. Effect of ECIGs on genes involved in the
circadian clock
The circadian molecular clock is important for
homeostasis and biologic functions, such as glucose metabolism and
immune/inflammatory responses. Circadian clock disruption in the
lungs may alter respiratory function and affect inflammatory
responses. ROS production may cause DNA damage and mucus
hypersecretion, contributing to the development and advance of
chronic obstructive pulmonary disease (COPD) (56). Alterations in organs other than the
lungs have been associated with the development of cancer, obesity
and cardiovascular risk, among other illnesses (57).
E-liquids contain a high amount of PG and glycerol.
To assess the effects of these substances on health, a previous
study exposed a murine model (female BALB/c) to steam from
nicotine-free and flavor-free ECIGs at various solvent
concentrations (PG 70% and glycerol 30%, glycerol 100% and PG 100%)
(57). The lung transcriptomic
results revealed that the inhalation of both components modulated
the expression of 37 genes, most conspicuously aryl hydrocarbon
receptor nuclear translocator like (Arntl), neuronal PAS
domain protein 2 (Npas2), nuclear receptor subfamily 1 group
D member 1 (Nr1d1), nuclear receptor subfamily 1 group D
member 2 (Nr1d2), period circadian regulator (Per),
Per2 and Per3. These genes belong to the circadian
clock machinery and play an important role in circadian cycle
regulation. Surprisingly, these affected genetic expression not
only in pulmonary tissue, but also in the liver, brain, skeletal
muscle and kidneys (Table II).
Likewise, the expression of the heat shock 70 kDa protein 1
(Hspa1a, also known as Hsp72) and heat shock protein family
A (Hsp70) member 1B (Hspa1b) genes, Hsp70 member was
altered following exposure to PG and glycerol, suggesting that
although Hspa1a and Hspa1b are not part of the
circadian clock control, they may be affected because their
expression depends on this physiologic process (Fig. 2B) (57).
A similar study by Khan et al (56) demonstrated that chronic exposure to
smoke and aerosols from ECIGs and water-pipes in a C57BL/6J murine
model produced specific pulmonary alterations to the abundance and
expression of genes related to the circadian clock control and to
the output of genes controlled by the circadian clock. Water-pipe
smoke exposure produced alterations in the circadian clock
expression patterns of the pulmonary-specific genes, Clock
and Bmal1, and in the upregulation of the output genes,
Rev-erbα, Rev-erbβ, Per2, Cry1 and Rorα (Fig. 2B). Exposure to ECIG aerosols also
alters circadian clock genetic expression in lung tissue,
particularly when e-liquids contain nicotine (Table II) (56).
7. Effects of ECIGs on the epigenome
Smoking tobacco cigarettes has been one of the risk
factors most related to epigenome alterations. Recently the impact
of ECIGs on the epigenome has also been questioned. Caliri et
al (58) proved the association
between vaping and a loss of DNA methylation levels. They analyzed
peripheral blood samples of ECIGs users, conventional smokers and
non-smokers for methylation levels (5-mC) on the transposable
elements, long interspersed nucleotide element 1 (LINE-1). The loss
of methylation in LINE-1 coding regions results in latent
retrotransposon activation. This can lead to a genomic instability
status, a hallmark of cancer. Their study demonstrated a
significant decrease in methylation (5-mC) in LINE-1 elements
(Fig. 2A), 18% in vapers and 13% in
cigarette smokers, compared to a non-smoker control group, with no
significant differences between vapers and smokers. The
hydroxymethylation (5-hmC) was also quantified on the DNA,
decreased in vapers (66%) and cigarette smokers (88%) (58). Epigenetic alterations found in that
study are linked to DNA hypomethylation, and they suggest a
possible association between ECIGs use and cancer risk (Table II).
Exposure to liquids and aerosols of ECIGs, with or
without nicotine, induces the gene expression of glutamate-cysteine
ligase catalytic subunit (GCLC), glutathione peroxidase 2
(GPX2), NAD(P)H dehydrogenase [quinone] 1 (NQO1) and
heme oxygenase 1 (HO1) in response to oxidative stress in
normal human bronchial epithelial cells (NHBE). The maximum
response to oxidative stress is produced when ECIG aerosols contain
nicotine (59).
On the other hand, exposure to ECIGs deregulates the
expression of >125 miRNAs. This was first evidenced by Solleti
et al (59), using RNA-seq.
These results confirmed the increased expression of the miRNAs,
miR-26A-2-3p, miR-126-5P, miR-140-5P, miR-29A-2-5P, miR-374A-3P and
miR-147B. The results were focused on miR-126-5P, expressed in
highly vascularized tissues like that found in lungs and the heart,
inducing the decrease in its gene targets, MAS-related G-protein
coupled receptor member X3 (MRGPRX3) and MYC,
involved in apoptosis, transformation and cellular differentiation
processes (Table II). This
exposure also increases NQO1 protein and HO1 enzyme expression,
both with antioxidative function in response to oxidative stress
(Fig. 2A) (59).
It is currently known that conventional cigarette
consumption during pregnancy is detrimental to fetal respiratory
health, increasing post-natal susceptibility to respiratory
infections and pulmonary dysfunction (1,2,32,34).
For this reason, some have the perception that the use of ECIGs is
a safer smoking alternative and acceptable for use by pregnant
women.
In pregnant murine models (BALB/c mice) exposed to
ECIGs, with and without nicotine, epigenetic alterations were
observed, among mothers and their descendants, in genes involved in
the inflammatory response of the lungs (56,57).
The expression of the genes, interleukin (Il)-1β, Il-6 and
tumor necrosis factor (Tnf)-α increased in the lungs of
mothers and the hatchlings exhibited an increased Tnf-α
expression, but decreased Il-1β levels. In addition,
signaling routes involved in the inflammatory response were
differentially altered in mothers and hatchlings, with changes on
the Erk1/2 and Jnk expression in mothers and p38 and
p65 changes in hatchlings (Table
II) (54,56-62).
The intrauterine exposure of mice to ECIGs with or
without nicotine has revealed increased mRNA levels of
platelet-derived growth factor α-receptor (Pdgfα) in the
postnatal stage. An increment in Pdgfα expression has been
shown to be involved in the pathologic process of pulmonary
fibrosis (61). In uterus,
ECIG aerosol exposure produces epigenetic alterations. An increase
in global methylation was previously evidenced in the lungs of
BALB/c mice hatchlings exposed to ECIGs during pregnancy,
regardless of the nicotine concentration (Fig. 2B) (61).
Apart from altering the genetic expression of
molecules related to the inflammatory response and the methylation
of fetal DNA, it has been evidenced in different animal models that
ECIG exposure generates embryonic development alterations. Exposure
to ECIG aerosols provokes orofacial alteration during Xenopus
laevis embryonic development. These may include middle facial
cleft, middle face hypoplasia, and alterations of muscle
development and vasculature distribution (54,56-62).
These alterations also occur in mammals. The
aberrant expression of the vasculogenesis gene, vascular
endothelial growth factor (VEGF) and the markers involved in
the formation of Fgf2, Sox9, and Col2a1 cartilage were observed in
the murine neural crest cell line, O91, following exposure to
different brands of electronic cigarettes (Table II) (54,56-62).
These alterations are caused by ECIGs components,
such as PG, vegetal glycerin and various concentrations of nicotine
in the e-liquids (62). This
evidence suggests that vaping during pregnancy may exert adverse
effects, such as those caused by traditional smoking. Further
investigations however, are necessary to fully elucidate these
effects.
8. Effects of nicotine administration
systems on pulmonary function
There is limited information regarding the effects
of vaping on pulmonary function. Several studies have evaluated the
acute effects, demonstrating variable results (63). In the study conducted by Flouris
et al (64), the acute
impact of active and passive ECIGs smoking on serum nicotine and
lung function was assessed and compared to active and passive
tobacco cigarette smoking. The results revealed that ECIGs and
tobacco cigarettes generated similar (P<0.001) effects on serum
nicotine levels with active and passive smoking. There was no
significant difference in pulmonary function parameters between
active and passive ECIGs smoking (64,65).
Ferrari et al (66) performed a study comparing the
effects of using nicotine-free ECIGs and traditional cigarettes for
5 min in healthy adult smokers (n=10) and non-smokers (n=10),
evaluating pulmonary function. As was expected, traditional
cigarettes induced a significant decrease from baseline in forced
expiratory flow at 75% of vital capacity (FEF75) in non-smokers.
There were significant decreases in forced expiratory flow at 25%
of vital capacity (FEF25), forced expiratory volume in 1 sec
(FEV1), and peak expiratory flow (PEF) in smokers. The only
statistically significant effects induced by the nicotine-free
ECIGs in smokers were reductions in FEV1 and FEF25(66). Other studies found that acute
exposure to ECIGs induced vasoreactivity and decreased PEF, though
they identified non-significant changes in FEV1, forced vital
capacity (FVC), and the ratio between FEV1 and FVC (FEV1/FVC)
(67).
A randomized trial in Brussels with 30 patients
(68) demonstrated that acute
nicotine and nicotine-free vaping decreased transcutaneous oxygen
tension (TcpO2) and slightly decreased peripheral oxygen
saturation (SpO2) despite its lack of sensitivity to
small changes in arterial O2 partial pressure. This
further indicates potential disturbances in lung gas exchanges
caused by vaping.
In another randomized, double-blind study,
occasional smokers (maximum 10 tobacco cigarettes per month) were
exposed to ECIGs aerosol for 30 min following a washout period of 1
week minimum. Dynamic spirometry and impulse oscillometry were then
evaluated. The results revealed a significant decrease in vital
capacity and resonance frequency, but increased levels of
fractional exhaled nitric oxide and increased resistance to
airflow, indicating an obstructive pattern after the exposure
(69).
As presented above, a number of studies have
explored short-term effects of vaping. Information on the long-term
effects is limited; however, generating increasing concern. A
recent observational 3.5 year-study compared health outcomes in 9
daily ECIGs users who had never smoked tobacco and a control group
of 12 individuals who had never smoked. The results revealed no
statistically significant changes from baseline in the EC users (or
between EC users and controls) in any of the investigated health
outcomes [blood pressure, heart rate, body weight, lung function,
respiratory symptoms, exhaled nitric oxide (eNO), exhaled carbon
monoxide (eCO) and high-resolution computed tomography (HRCT)]
(70).
Due to the newness of vaping and the multitude of
devices, flavorings and nicotine concentrations on the market,
there is a shortage of data regarding its long-term effects on the
respiratory system. The consequences of long-term vaping remain
unclear (71). Further studies are
required to pinpoint involved pathogenesis mechanisms, and to
identify the potential long-term consequences of ECIG usage.
To date, there are no specific policies on the
manufacturing standards of e-cigs. As regards ECIs regulation, the
WHO Framework Convention for Tobacco Control (FCTC/Law 1109 of
2006) at the seventh meeting of WHO Framework Convention on Tobacco
Control, invited FCTC parties to consider prohibiting or regulating
ECIGs. On the other hand, the United States Congress raised the
minimum age to buy tobacco and electronic cigarettes in the country
from 18 to 21 years of age on November, 2019; the measure approved
was far from what the US administration was considering a total
prohibition on flavored electronic cigarettes (72-75).
9. Conclusion
The majority of ECIGs, whether they contain nicotine
or not, emit potentially toxic substances when used. What is of
concern is that the number of these toxic substances and their
concentration are highly variable, as are the manufacturing
specifications for, as well as ECIGs manufacturing characteristics.
This variability may result in increased exposure to these
compounds with clinically demonstrated adverse health effects.
While the use of ECIGs reduces the consumption of toxic compounds
compared to traditional cigarettes, it remains a source of exposure
to substances with high carcinogenic potential that alter
epigenomic and transcriptomic processes, promote cell injury,
hijack normal inflammatory response and, at high doses, affect
normal fetal development. Further investigations are required in
order to better understand the underlying mechanisms. Preventive
measures and guidelines for the use of these devices can then be
established.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Hospital
Universitario San Ignacio-Research Office
Availability of data and materials
Not applicable.
Authors' contributions
NN, LGB, DMG, CB, FG, DL, MJP, CC, IM, PS, AR, SH,
CT, SRA, RC and MG contributed to manuscript writing and
data/literature searching for this review. AC and AR contributed to
the concept and design of the study, and to manuscript writing. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Herr C, Tsitouras K, Niederstraßer J,
Backes C, Beisswenger C, Dong L, Guillot L, Keller A and Bals R:
Cigarette smoke and electronic cigarettes differentially activate
bronchial epithelial cells. Respir Res. 21(67)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gilbert AH: Smokeless non-tobacco
cigarette. US Patent US3200819A. Filed April 17, 1963; issued
August 17, 1965.
|
|
3
|
Franck C, Budlovsky T, Windle SB, Filion
KB and Eisenberg MJ: Electronic cigarettes in North America:
History, use, and implications for smoking cessation. Circulation.
129:1945–1952. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hammond D, Reid JL, Rynard VL, Fong GT,
Cummings KM, McNeill A, Hitchman S, Thrasher JF, Goniewicz ML,
Bansal-Travers M, et al: Prevalence of vaping and smoking among
adolescents in Canada, England, and the United States: Repeat
national cross sectional surveys. BMJ. 365(l2219)2019.PubMed/NCBI View Article : Google Scholar : Erratum in: BMJ
370: m2579, 2020.
|
|
5
|
Grana A, Benowitz M and Stanton GA:
Background Paper on E-cigarettes (Electronic Nicotine Delivery
Systems). UCSF WHO Tobacco Control Papers, 2013.
|
|
6
|
Protano C, Avino P, Manigrasso M, Vivaldi
V, Perna F, Valeriani F and Vitali M: Environmental electronic vape
exposure from four different generations of electronic cigarettes:
Airborne particulate matter levels. Int J Environ Res Public
Health. 15(2172)2018.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Farsalinos KE, Gillman G, Thornburg JW,
Hecht SS and Polosa R: Analytical assessment of e-cigarettes: From
contents to chemical and particle exposure profiles. Elsevier,
2016.
|
|
8
|
Barrington-Trimis JL and Leventhal AM:
Adolescents' Use of ‘Pod Mod’ E-Cigarettes - Urgent Concerns. N
Engl J Med. 379:1099–1102. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Marcham CL and Springston JP: Electronic
cigarettes in the indoor environment. Rev Environ Health.
34:105–124. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Corey C, Wang B, Johnson SE, et al:
Centers for Disease Control and Prevention (CDC): Notes from the
field: Electronic cigarette use among middle and high school
students - United States, 2011-2012. MMWR Morb Mortal Wkly Rep.
62:729–730. 2013.PubMed/NCBI
|
|
11
|
Gentzke AS, Creamer M, Cullen KA, Ambrose
BK, Willis G, Jamal A and King BA: Vital Signs: Tobacco product use
among middle and high school students - United States, 2011-2018.
MMWR Morb Mortal Wkly Rep. 68:157–164. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Barrington-Trimis JL, Berhane K, Unger JB,
Cruz TB, Huh J, Leventhal AM, Urman R, Wang K, Howland S, Gilreath
TD, et al: Psychosocial factors associated with adolescent
electronic cigarette and cigarette use. Pediatrics. 136:308–317.
2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Stratton K, Kwan LY and Eaton DL: Public
Health Consequences of E-Cigarettes. The National Academies Press,
2018.
|
|
14
|
Herrington JS and Myers C: Electronic
cigarette solutions and resultant aerosol profiles. J Chromatogr A.
1418:192–199. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kucharska M, Wesołowski W, Czerczak S and
Soćko R: Testing of the composition of e-cigarette liquids -
Manufacturer-declared vs. true contents in a selected series of
products. Med Pr. 67:239–253. 2016.PubMed/NCBI View Article : Google Scholar : (In Polish).
|
|
16
|
Hahn J, Monakhova YB, Hengen J,
Kohl-Himmelseher M, Schüssler J, Hahn H, Kuballa T and Lachenmeier
DW: Electronic cigarettes: Overview of chemical composition and
exposure estimation. Tob Induc Dis. 12(23)2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sassano MF, Davis ES, Keating JE, Zorn BT,
Kochar TK, Wolfgang MC, Glish GL and Tarran R: Evaluation of
e-liquid toxicity using an open-source high-throughput screening
assay. PLoS Biol. 16(e2003904)2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Zhu SH, Zhuang YL, Wong S, Cummins SE and
Tedeschi GJ: E-cigarette use and associated changes in population
smoking cessation: Evidence from US current population surveys.
BMJ. 358(j3262)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
U.S. Food and Drug Administration (FDA):
Select committee on GRAS substances opinion: Propylene glycol and
propylene glycol monostearate. FDA, Washington, DC, 1973.
|
|
20
|
Jimenez Ruiz CA, Solano Reina S, de Granda
Orive JI, Signes-Costa Minaya J, de Higes Martinez E, Riesco
Miranda JA, Altet Gómez N, Lorza Blasco JJ, Barrueco Ferrero M and
de Lucas Ramos P: The electronic cigarette. Official statement of
the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) on
the efficacy, safety and regulation of electronic cigarettes. Arch
Bronconeumol. 50:362–367. 2014.PubMed/NCBI View Article : Google Scholar : (In English).
|
|
21
|
Gomes R, Liteplo R and Meek ME: Ethylene
glycol: human health aspects. World Health Organization, Geneva,
2002.
|
|
22
|
Grana R, Benowitz N and Glantz SA:
E-cigarettes: A scientific review. Circulation. 129:1972–1986.
2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Oh AY and Kacker A: Do electronic
cigarettes impart a lower potential disease burden than
conventional tobacco cigarettes? Review on E-cigarette vapor versus
tobacco smoke. Laryngoscope. 124:2702–2706. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
German Cancer Research Center (ed):
Electronic Cigarettes-An Overview. Vol 19. German Cancer Research
Center, Heidelberg, 2013.
|
|
25
|
Papaefstathiou E, Stylianou M and Agapiou
A: Main and side stream effects of electronic cigarettes. J Environ
Manage. 238:10–17. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Copaja MS: Methanol: Toxicity, Regulation
and Analysis. What is methanol? AGQ Labs Chile, 2018.
|
|
27
|
Behar RZ, Luo W, Lin SC, Wang Y, Valle J,
Pankow JF and Talbot P: Distribution, quantification and toxicity
of cinnamaldehyde in electronic cigarette refill fluids and
aerosols. Tob Control. 25 (Suppl 2):ii94–ii102. 2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kosmider L, Sobczak A, Prokopowicz A,
Kurek J, Zaciera M, Knysak J, Smith D and Goniewicz ML:
Cherry-flavoured electronic cigarettes expose users to the
inhalation irritant, benzaldehyde. Thorax. 71:376–377.
2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Irwin R: National Toxicology Program. NTP
Toxicology and Carcinogenesis Studies of Furfural (CAS No. 98-01-1)
in F344/N Rats and B6C3F1 Mice (Gavage Studies). Natl Toxicol
Program Tech Rep Ser. 382:1–201. 1990.PubMed/NCBI
|
|
30
|
Sleiman M, Logue JM, Montesinos VN,
Russell ML, Litter MI, Gundel LA and Destaillats H: Emissions from
electronic cigarettes: Key parameters affecting the release of
harmful chemicals. Environ Sci Technol. 50:9644–9651.
2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Bekki K, Uchiyama S, Ohta K, Inaba Y,
Nakagome H and Kunugita N: Carbonyl compounds generated from
electronic cigarettes. Int J Environ Res Public Health.
11:11192–11200. 2014.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Hajek P, Etter JF, Benowitz N, Eissenberg
T and McRobbie H: Electronic cigarettes: Review of use, content,
safety, effects on smokers and potential for harm and benefit.
Addiction. 109:1801–1810. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Hutzler C, Paschke M, Kruschinski S,
Henkler F, Hahn J and Luch A: Chemical hazards present in liquids
and vapors of electronic cigarettes. Arch Toxicol. 88:1295–1308.
2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kim KH, Kabir E and Jahan SA: Review of
electronic cigarettes as tobacco cigarette substitutes: Their
potential human health impact. J Environ Sci Health Part C Environ
Carcinog Ecotoxicol Rev. 34:262–275. 2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Papoušek R, Pataj Z, Nováková P, Lemr K
and Barták P: Determination of acrylamide and acrolein in smoke
from tobacco and E-cigarettes. Chromatographia. 77:1145–1151.
2014.
|
|
36
|
Uchiyama S, Inaba Y and Kunugita N:
Determination of acrolein and other carbonyls in cigarette smoke
using coupled silica cartridges impregnated with hydroquinone and
2,4-dinitrophenylhydrazine. J Chromatogr A. 1217:4383–4388.
2010.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Geiss O, Bianchi I and Barrero-Moreno J:
Correlation of volatile carbonyl yields emitted by e-cigarettes
with the temperature of the heating coil and the perceived
sensorial quality of the generated vapours. Int J Hyg Environ
Health. 219:268–277. 2016.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Kosmider L, Sobczak A, Fik M, Knysak J,
Zaciera M, Kurek J and Goniewicz ML: Carbonyl compounds in
electronic cigarette vapors: Effects of nicotine solvent and
battery output voltage. Nicotine Tob Res. 16:1319–1326.
2014.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Cai H and Wang C: Graphical review: The
redox dark side of e-cigarettes; exposure to oxidants and public
health concerns. Redox Biol. 13:402–406. 2017.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hoffmann D, Rivenson A, Murphy SE, Chung
FL, Amin S and Hecht SS: Cigarette smoking and adenocarcinoma of
the lung: the relevance of nicotine-derived N-nitrosamines. J
Smoking-Related Disord. 4:165–189. 1993.
|
|
41
|
Cheng T: Chemical evaluation of electronic
cigarettes. Tob Control. 23 (Suppl 2):ii11–ii17. 2014.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Oh J-A and Shin H-S: Identification and
quantification of several contaminated compounds in replacement
liquids of electronic cigarettes by Gas chromatography-mass
spectrometry. J Chromatogr Sci. 53:841–848. 2015.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Badia Tahull MB, Leiva Badosa E, Colls
González M and Llop Talaverón J: Endocrine disruptors in artificial
nutrition. Nutr Hosp. 35:469–473. 2018.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
44
|
Hess CA, Olmedo P, Navas-Acien A, Goessler
W, Cohen JE and Rule AM: E-cigarettes as a source of toxic and
potentially carcinogenic metals. Environ Res. 152:221–225.
2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Goniewicz ML, Knysak J, Gawron M, Kosmider
L, Sobczak A, Kurek J, Prokopowicz A, Jablonska-Czapla M,
Rosik-Dulewska C, Havel C, et al: Levels of selected carcinogens
and toxicants in vapour from electronic cigarettes. Tob Control.
23:133–139. 2014.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Mikheev VB, Brinkman MC, Granville CA,
Gordon SM and Clark PI: Real-time measurement of electronic
cigarette aerosol size distribution and metals content analysis.
Nicotine Tob Res. 18:1895–1902. 2016.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Williams M, Bozhilov K, Ghai S and Talbot
P: Elements including metals in the atomizer and aerosol of
disposable electronic cigarettes and electronic hookahs. PLoS One.
12(e0175430)2017.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Carvajal C: Reactive oxygen species:
training, function and oxidative stress. Med Leg Costa Rica.
36:91–100. 2019.
|
|
49
|
Lerner CA, Sundar IK, Yao H, Gerloff J,
Ossip DJ, McIntosh S, Robinson R and Rahman I: Vapors produced by
electronic cigarettes and e-juices with flavorings induce toxicity,
oxidative stress, and inflammatory response in lung epithelial
cells and in mouse lung. PLoS One. 10(e0116732)2015.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Park SJ, Walser TC, Perdomo C, Wang T,
Pagano PC, Liclican EL, Krysan K, Larsen JE, Minna JD, Lenburg ME,
et al: Abstract B16: The effect of e-cigarette exposure on airway
epithelial cell gene expression and transformation. Clin Cancer
Res. 20 (Suppl 2):B16. 2014.
|
|
51
|
Cressey D: E-cigarettes affect cells.
Nature. 508(159)2014.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Ganapathy V, Manyanga J, Brame L, McGuire
D, Sadhasivam B, Floyd E, Rubenstein DA, Ramachandran I, Wagener T
and Queimado L: Electronic cigarette aerosols suppress cellular
antioxidant defenses and induce significant oxidative DNA damage.
PLoS One. 12(e0177780)2017.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Tommasi S, Bates SE, Behar RZ, Talbot P
and Besaratinia A: Limited mutagenicity of electronic cigarettes in
mouse or human cells in vitro. Lung Cancer. 112:41–46.
2017.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Martin EM, Clapp PW, Rebuli ME, Pawlak EA,
Glista-Baker E, Benowitz NL, Fry RC and Jaspers I: E-cigarette use
results in suppression of immune and inflammatory-response genes in
nasal epithelial cells similar to cigarette smoke. Am J Physiol
Lung Cell Mol Physiol. 311:L135–L144. 2016.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Chitu V and Stanley ER: Colony-stimulating
factor-1 in immunity and inflammation. Curr Opin Immunol. 18:39–48.
2006.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Khan NA, Yogeswaran S, Wang Q, Muthumalage
T, Sundar IK and Rahman I: Waterpipe smoke and e-cigarette vapor
differentially affect circadian molecular clock gene expression in
mouse lungs. PLoS One. 14(e0211645)2019.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Lechasseur A, Jubinville É, Routhier J,
Bérubé JC, Hamel-Auger M, Talbot M, Lamothe J, Aubin S, Paré MÈ,
Beaulieu MJ, et al: Exposure to electronic cigarette vapors affects
pulmonary and systemic expression of circadian molecular clock
genes. Physiol Rep. 5(e13440)2017.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Caliri AW, Caceres A, Tommasi S and
Besaratinia A: Hypomethylation of LINE-1 repeat elements and global
loss of DNA hydroxymethylation in vapers and smokers. Epigenetics.
15:816–829. 2020.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Solleti SK, Bhattacharya S, Ahmad A, Wang
Q, Mereness J, Rangasamy T and Mariani TJ: MicroRNA expression
profiling defines the impact of electronic cigarettes on human
airway epithelial cells. Sci Rep. 7(1081)2017.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Ganapathy V, Manyanga J, Brame L, McGuire
D, Sadhasivam B, Floyd E, Rubenstein DA, Ramachandran I, Wagener T
and Queimado L: Electronic cigarette aerosols suppress cellular
antioxidant defenses and induce significant oxidative DNA damage.
PLoS One. 12(e0177780)2017.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Chen H, Li G, Chan YL, Chapman DG,
Sukjamnong S, Nguyen T, Annissa T, McGrath KC, Sharma P and Oliver
BG: Maternal E-Cigarette Exposure in Mice Alters DNA Methylation
and Lung Cytokine Expression in Offspring. Am J Respir Cell Mol
Biol. 58:366–377. 2018.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Kennedy AE, Kandalam S, Olivares-Navarrete
R and Dickinson AJG: E-cigarette aerosol exposure can cause
craniofacial defects in Xenopus laevis embryos and mammalian neural
crest cells. PLoS One. 12(e0185729)2017.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Allen JG, Flanigan SS, LeBlanc M,
Vallarino J, MacNaughton P, Stewart JH and Christiani DC: Flavoring
chemicals in e-cigarettes: Diacetyl, 2,3-pentanedione, and acetoin
in a sample of 51 products, including fruit-, candy-, and
cocktail-flavored e-cigarettes. Environ Health Perspect.
124:733–739. 2016.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Flouris AD, Chorti MS, Poulianiti KP,
Jamurtas AZ, Kostikas K, Tzatzarakis MN, Wallace Hayes A, Tsatsakis
AM and Koutedakis Y: Acute impact of active and passive electronic
cigarette smoking on serum cotinine and lung function. Inhal
Toxicol. 25:91–101. 2013.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Coppeta L, Magrini A, Pietroiusti A,
Perrone S and Grana M: Effects of smoking electronic cigarettes on
pulmonary function and environmental parameters. Open Public Health
J. 11:360–368. 2018.
|
|
66
|
Ferrari M, Zanasi A, Nardi E, Morselli
Labate AM, Ceriana P, Balestrino A, Pisani L, Corcione N and Nava
S: Short-term effects of a nicotine-free e-cigarette compared to a
traditional cigarette in smokers and non-smokers. BMC Pulm Med.
15(120)2015.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Kerr DMI, Brooksbank KJM, Taylor RG, Pinel
K, Rios FJ, Touyz RM and Delles C: Acute effects of electronic and
tobacco cigarettes on vascular and respiratory function in healthy
volunteers: A cross-over study. J Hypertens. 37:154–166.
2019.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Chaumont M, Tagliatti V, Channan EM, Colet
JM, Bernard A, Morra S, Deprez G, Van Muylem A, Debbas N, Schaefer
T, et al: Short halt in vaping modifies cardiorespiratory
parameters and urine metabolome: A randomized trial. Am J Physiol
Lung Cell Mol Physiol. 318:L331–L344. 2020.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Antoniewicz L, Brynedal A, Hedman L,
Lundbäck M and Bosson JA: Acute effects of electronic cigarette
inhalation on the vasculature and the conducting airways.
Cardiovasc Toxicol. 19:441–450. 2019.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Polosa R, Cibella F, Caponnetto P, Maglia
M, Prosperini U, Russo C and Tashkin D: Health impact of
E-cigarettes: A prospective 3.5-year study of regular daily users
who have never smoked. Sci Rep. 7(13825)2017.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Grigg J: E-cigarette regulation: Getting
it wrong costs lives. Lancet Respir Med. 7:994–995. 2019.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Kennedy RD, Awopegba A, De León E and
Cohen JE: Global approaches to regulating electronic cigarettes.
Tob Control. 26:440–445. 2017.PubMed/NCBI View Article : Google Scholar
|
|
73
|
World Health Organization (WHO): Parties
to the WHO Framework Convention on Tobacco Control. WHO Framework
Convention on Tobacco Control, 2020.
|
|
74
|
Institute for Global Tobacco Control:
Country Laws Regulating E-cigarettes: A Policy Scan. Johns Hopkins
Bloomberg School of Public Health, Baltimore, MD, 2020. https://www.globaltobaccocontrol.org/e-cigarette_policyscan.
Last Updated May 18, 2020.
|
|
75
|
World Health Organization (WHO):
Electronic nicotine delivery systems: Report by WHO. Conference of
the Parties to the WHO Framework Convention on Tobacco Control,
Moscow, 2014.
|