Introduction
Thymoma is the most common tumor of the anterior
mediastinum. Surgical resection has been advocated as the principal
treatment and completeness of resection has been considered to be
the most important determinant of long-term survival in thymomas
(1–3). Recently, an increase in the incidence
of a small-sized thymoma (SST) has been noted. SST appears to
usually be classified into early stages. However, SSTs are rare and
clinical reports are not currently available.
To identify the individual biological behavior of
thymomas, various factors including p53, bcl-2, matrix
metalloproteinases, proliferating cell nuclear counts, Ki67 index
and podoplanin have been analyzed (4–10).
In a previous study, podoplanin, a 40-kDa mucin-type transmembrane
sialoglycoprotein was correlated with tumor lymphangiogenesis,
tumor invasion, lymph node metastasis of thymoma and poor clinical
outcome of thymoma patients (11).
In the present study, we evaluated the
clinicopathological data of SST patients and assessed the
podoplanin and Ki67 immunohistochemistry of SSTs to determine the
biological behavior of SSTs.
Patients and methods
Clinical data
A retrospective review was conducted of clinical and
pathological data in all patients with thymomas undergoing surgery
at the Nagoya City University Hospital, Japan, between January 1989
and December 2010. During this period of time, 21 tumors were
diagnosed as SST within 30 mm as a maximal diameter (MD). The
present study was approved by the Institutional Review Board (IRB)
of Nagoya City University Hospital.
In the present study, the macroscopical measurements
of resected specimens were utilized as the MD of a tumor, and the
Masaoka-Koga staging system (12)
was used for staging of thymoma. The Masaoka-Koga staging system,
modified with the Masaoka staging system (1), has been recommended by the
International Thymic Malignancy Interest Group (ITMIG) (13,14).
Histopathological analysis
To identify the intensity of malignant behavior the
expression of podoplanin and Ki67 was evaluated.
Immunohistochemistry
MIB-1, a mouse monoclonal anti-human Ki67 antibody
(MIB-1, Dako, Glostrup, Denmark) was used. The Dako Envision system
(Dako EnVision labeled polymer, peroxidase) was used according to
the manufacturer’s instructions. The Ki67 labeling index was
assessed as the percentage of cells showing definite nuclear
staining among 500 randomly selected tumor cells, with high-power
(magnification ×400) fields (7).
D2–40 monoclonal antibodies (Nichirei Bioscience,
Tokyo, Japan) were used for the staining of podoplanin. The
immunohistochemical staining was performed using a Benchmark LT
automated immunostainer (Ventana Japan K.K., Kanagawa, Japan) by
the avidin-biotin-peroxidase method with diaminobenzidine
visualization and hematoxylin counterstaining, according to the
manufacturer’s instructions. The immuno-reactivity of the tumor
cells was assessed semiquantitatively as negative (no evidence of
staining), weakly positive (1–10% of tumor cells were positive), or
positive (>10% of the tumor cells were positive).
Statistical analysis
Survival analysis was performed by the Kaplan-Meier
method. An outcome measure was utilized with overall and
tumor-specific survival. Ki67 labeling indices were presented as
the mean ± standard deviation and analyzed using the unpaired
t-test using Scheffe’s method according to the Masaoka-Koga stage
or the WHO histological subtype. P<0.05 was considered to
indicate a statistically significant difference.
Results
Clinical and pathological data
The study included 10 males and 11 females, with a
mean age of 59 years, ranging between 35 and 77 years. Eleven of
the 21 thymoma patients had myasthenia gravis (MG) symptoms. The
mean of MD of the tumor was 2.4 cm (1.5–3.0). The distribution of
MD was 1.5 < MD ≤ 2.0 cm in 7 tumors, 2.0 < MD ≤ 2.5 cm in 5
tumors and 2.5 < MD ≤ 3.0 cm in 9 tumors. Pathological diagnosis
of thymoma revealed the following types: A (n=1), AB (n=8), B1
(n=5), B2 (n=6) and B3 (n=1). Surgical procedures including
extended thymothymomectomy with sternotomy was performed in 15
patients. These 15 patients included all MG patients (n=11). Tumor
resection (resection of thymoma with margin, but some thymic tissue
may remain) with VATS (video-assisted thoracic surgery) technique
was performed in 6 patients with stage I (n=5) or II (n=1) disease.
Masaoka-Koga stages of 21 thymoma patients were stage I (n=16), II
(n=3), III (n=1) and IVb (n=1) (Table
I).
 | Table IClinicopathological factors in 21
thymoma cases. |
Table I
Clinicopathological factors in 21
thymoma cases.
| Factors | Thymoma cases
(n=21) |
|---|
| Age | 59±11 (35–77) |
| Gender | |
| Male | n=10 |
| Female | n=11 |
| MD (cm) | 2.4±0.5 cm
(1.5–3.0) |
| 1.5 < MD ≤
2.0 | n=7 |
| 2.0 < MD ≤
2.5 | n=5 |
| 2.5 < MD ≤
3.0 | n=9 |
| Operation procedure
1 | |
| Extended
thymothymomectomy | n=15 |
| Tumor resection
only | n=6 |
| Operation procedure
2 | |
| Sternotomy | n=16 |
| VATS | n=5 |
| Masaoka stage | |
| I | n=16 |
| II | n=3 |
| III | n=1 |
| IVb | n=1 |
| WHO histology | |
| A | n=1 |
| AB | n=8 |
| B1 | n=5 |
| B2 | n=6 |
| B3 | n=1 |
| Ki67 labeling
index | 2.7±0.8% (1.4–3.8)
(n=17) |
| WHO histology and
Ki67 labeling index | |
| A + AB | 2.1±0.7% (n=7) |
| B1 | 3.1±0.6% (n=5) |
| B2 + B3 | 3.3±0.4% (n=5) |
| Masaoka stage and
Ki67 labeling index | |
| I | 2.5±0.8% (n=12) |
| II | 3.1±0.8% (n=3) |
| III | 3.8 (n=1) |
| IVb | 3.2 (n=1) |
| Podoplanin
immunohistochemistry | |
| Positive | n=2 |
| Focally
positive | n=3 |
| Negative | n=12 |
| WHO histology | |
| Positive | B2 + B3 (n=2) |
| Focally
positive | B1 (n=2), B2 + B3
(n=1) |
| Negative | A + AB (n=7), B1
(n=3) |
| B2 + B3 (n=2) |
| Masaoka stage | |
| Positive | I (n=1), III + IVb
(n=1) |
| Focally
positive | I (n=3) |
| Negative | I (n=8), II
(n=3) |
| III + IVb (n=1) |
In the case of stage III thymoma, pericardial and
left brachiocephalic vein invasions were observed. This patient
underwent thymothymomectomy with sternotomy and partial resection
of the pericardium and left brachiocephalic vein. In the case of
stage IVb thymoma, phrenic nerve and mediastinal pleura invasion
and anterior mediastinal lymph node metastasis were observed.
Preoperative phrenic nerve paralysis was not observed. This patient
underwent thymothymomectomy with sternotomy and partial resection
of the phrenic nerve. All 21 patients, including the 2 patients at
advanced stage (stage III and IVb), underwent surgery with complete
resection both macroscopically and microscopically. Postoperative
adjuvant radiation was performed in 2 thymoma patients with stage
III and IVb disease. No postoperative complication occurred with
the exception of one case with phrenic nerve resection (Table I).
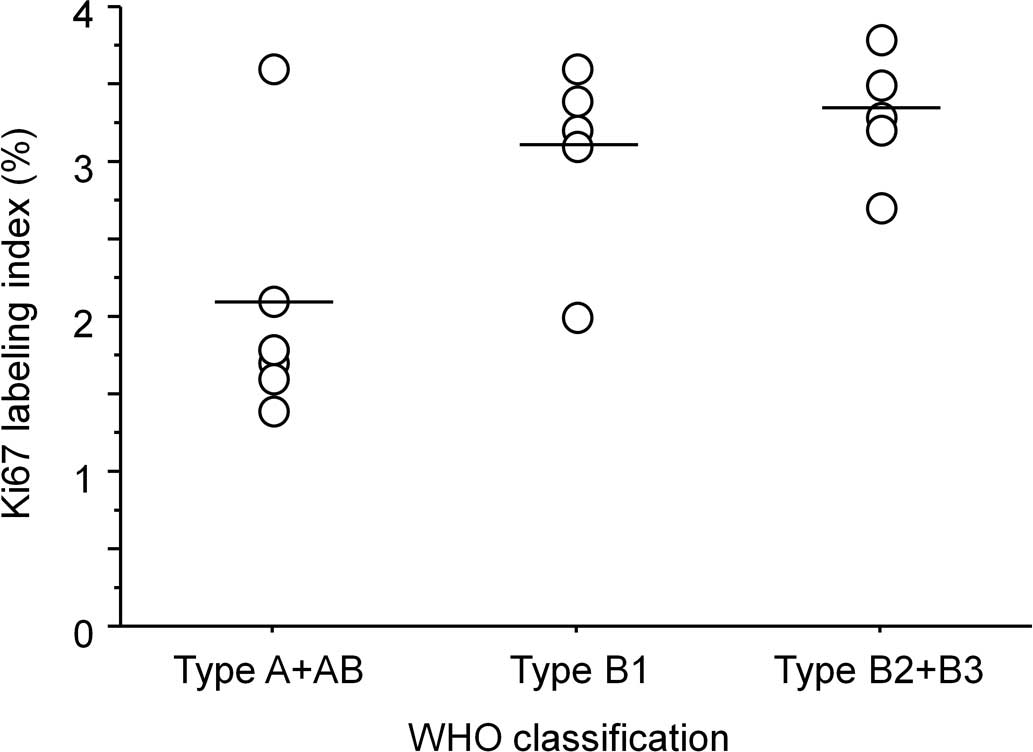
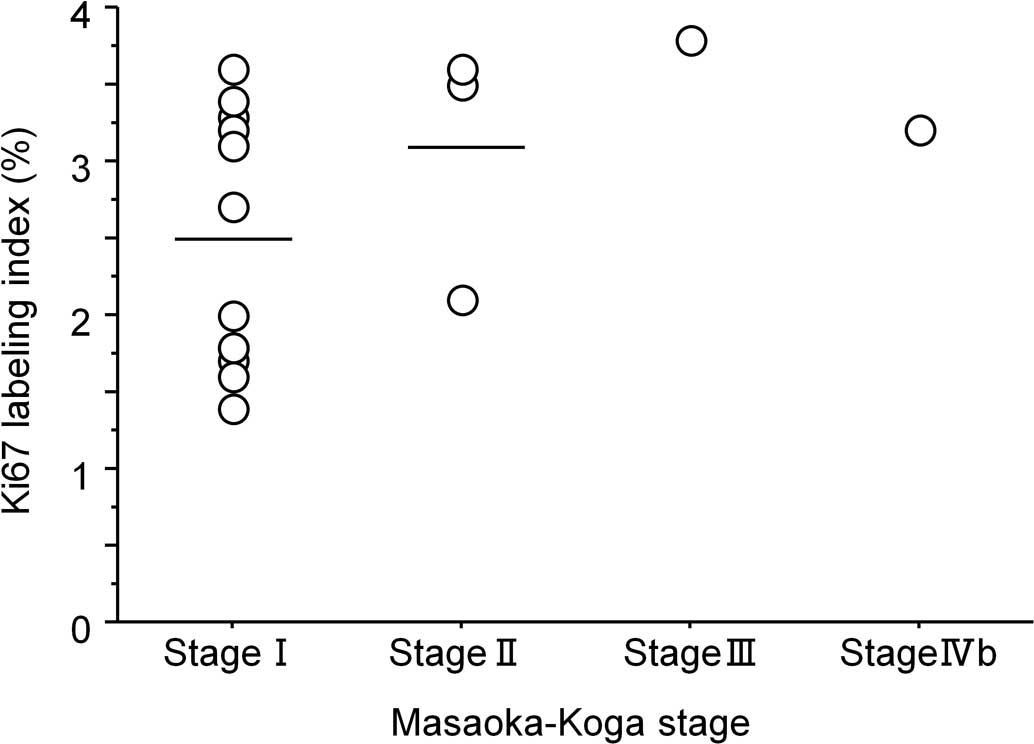
Immunohistochemical analysis
Paraffin blocks from 17 of the 21 thymoma patients
were analyzed using immunohistochemistry. The mean Ki67 labeling
index was 2.7±0.8% (1.4–3.8). The mean Ki67 labeling index of type
A and AB tumors combined was 2.1±0.7%, that of type B1 was 3.1±0.6%
and that of type B2 and B3 tumors combined was 3.3±0.4% (Fig. 1, Table
I). No significant differences were found among the groups. The
mean Ki67 labeling index of stage I was 2.5±0.8; of stage II,
3.1±0.8, of stage III, 3.8 and of stage IVb, 3.2% (Fig. 2, Table
I). No significant differences were observed among the
groups.
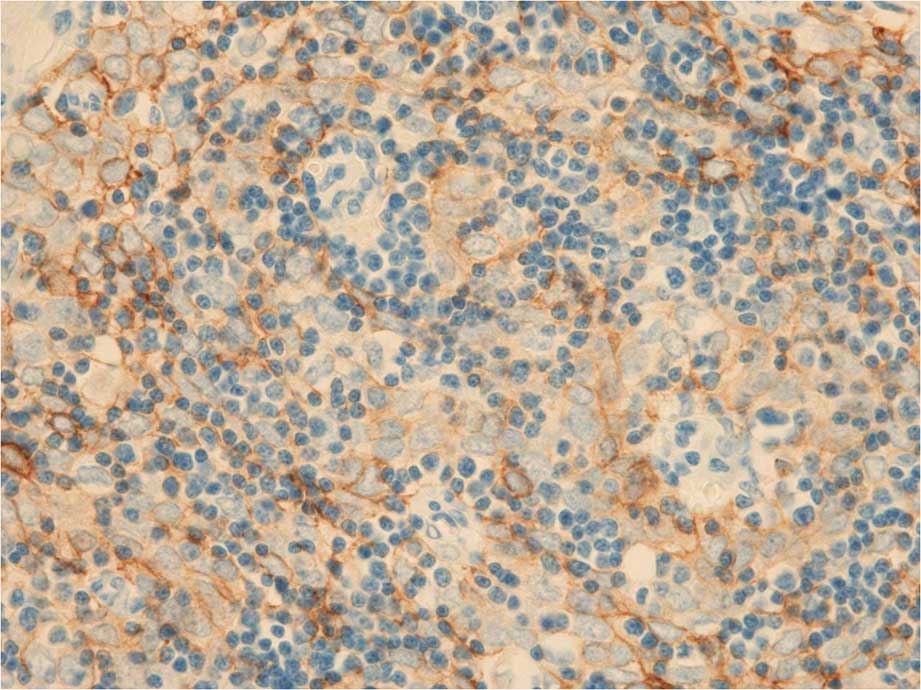
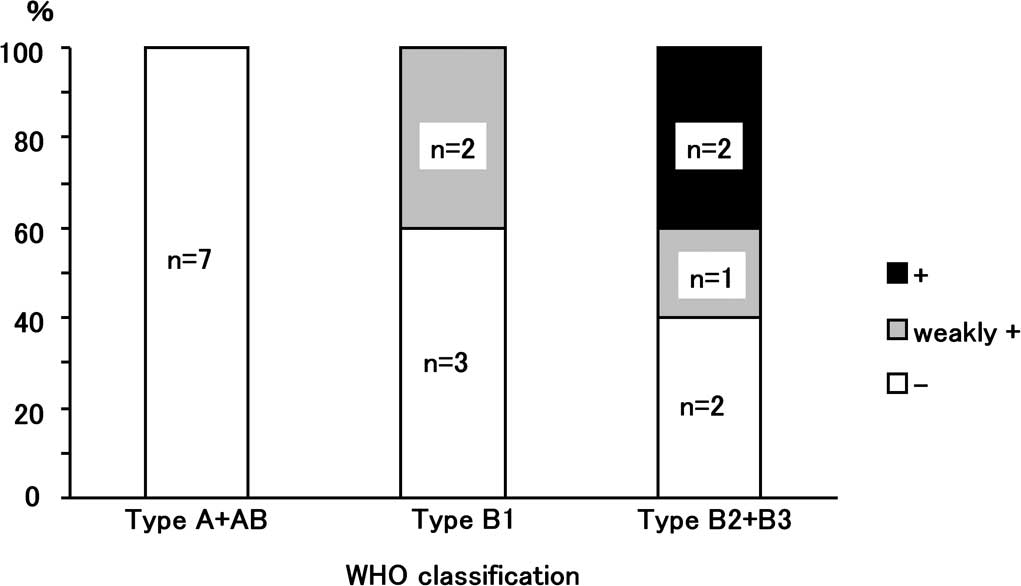
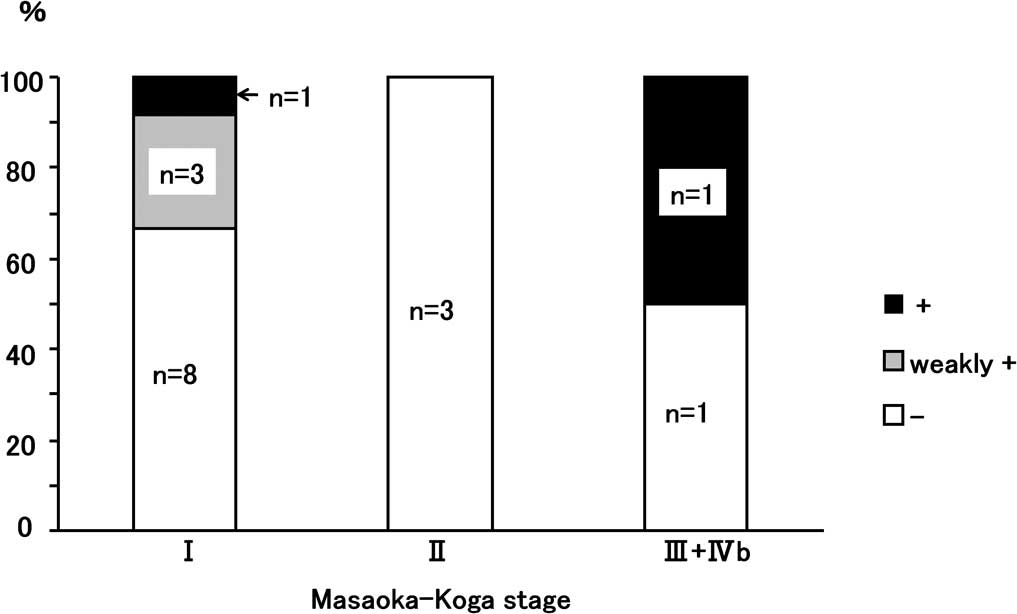
To assess the lymphangiogenesis and ability of
lymphatic invasion, an immunohistchemical analysis was performed
using a D2–40 monoclonal antibody that recognizes human podoplanin.
Fig. 3 shows an example of
positive podoplanin immunohistochemical staining with D2–40. This
case was a WHO-type B2 thymoma. Two cases were positive for D2–40,
3 were weakly positive and 12 were negative. Regarding the WHO
classification, the two D2–40-positive cases were type B2, and 2
cases of type B1 as well as 1 case of type B2 were weakly positive
(Fig. 4). Regarding the
Masaoka-Koga stage, 1 positive case was stage IVb disease and
another was stage I disease. The weakly positive cases were stage I
disease (Fig. 5).
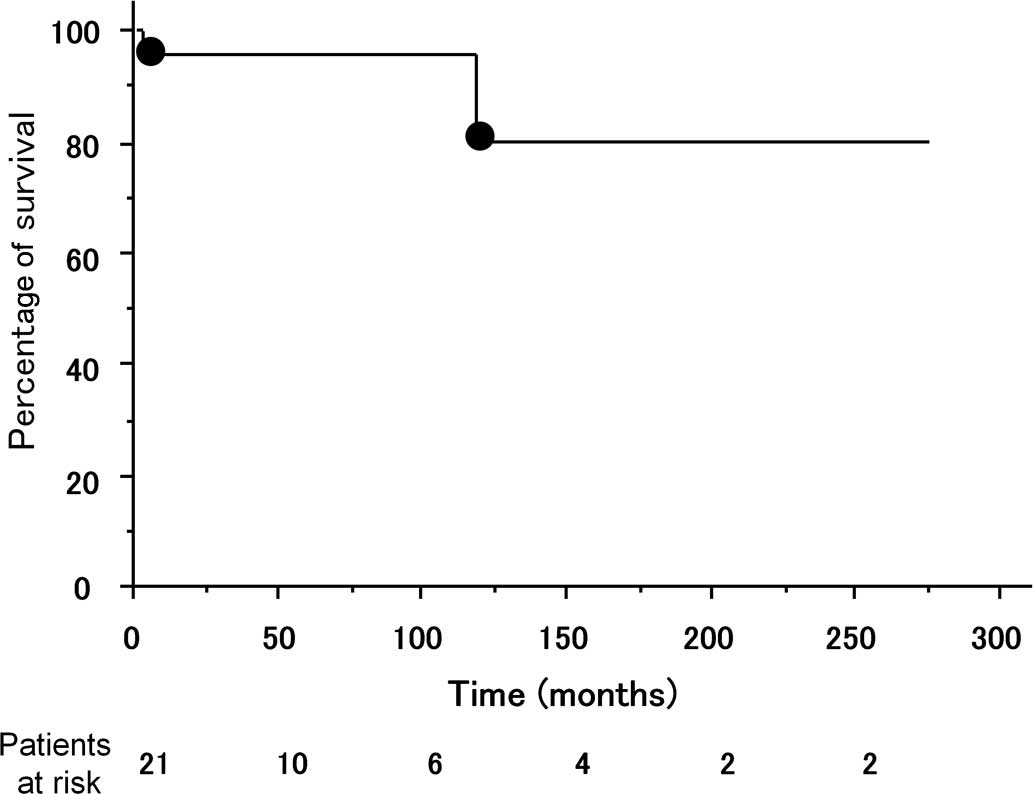
The median observation period was 42.1 months
(2.1–274.4 months after the primary operation). Pleural
disseminated lesions appeared and were diagnosed as a recurrence in
only 1 case of stage IVb thymoma, 46 months after the primary
operation. Resection of the recurrent lesions and chemotherapy were
performed. This patient succumbed to thymoma 118 months after the
primary operation. One patient succumbed to crisis of MG 2 months
after the operation. The overall survival was 95.2% at 5 years and
79.4% at 10 years after the operation (Fig. 6). Tumor-specific survival (only
deaths from thymoma were considered as events) was 100% at 5 years
and 83.3% at 10 years after the operation.
Discussion
Investigators in this study experienced a case of
SST in which the patient succumbed to the disease. The MD of the
tumor was only 2.0 cm but with pericardial invasion and anterior
mediastinal lymph node metastasis. Recurrence appeared 46 months
after the primary operation. This patient succumbed to thymoma 118
months after the primary operation. To analyze this case, we
evaluated 21 SST cases in the present study. Pathological type of
WHO classification of the case that succumbed was type B2, which is
regarded as one of the most common types of SSTs. To analyze the
malignant potential of SSTs, podoplanin and Ki67
immunohistochemistry were utilized. Results showed 2 tumors of
positive signals of podoplanin in SSTs. The tumor of the deceased
case was positive and the Ki67 labeling index was 3.2, higher than
the average index.
The tumor size of thymoma has been identified as a
prognostic factor (2). However, 2
cases with advanced-staged SSTs were observed in this study. The 2
tumors invaded the pericardium, identified using intraoperative
findings. Intraoperative findings are crucial and this
macroscopical diagnosis was included in the Masaoka stage
classification. Usually SSTs are classified into early stages. As
the prognosis of the patients with early-staged thymoma has been
extremely good, limited thymectomy may be utilized. Onuki et
al reported the efficacy of limited thymectomy for stage I or
II thymomas (15). If the tumor
invasion to the surrounding organs is apparent intraoperatively, we
should convert the operative procedures from limited thymectomy to
extended or total thymectomy.
Masaoka stage (1–3) and
WHO histological classifications have been regarded as prognostic
factors (16). However, the
identification of more powerful prognostic factors would be
beneficial for the treatment of thymoma. A number of factors,
including p53, bcl-2, matrix metalloproteinases and proliferating
cell nuclear counts have been assessed thus far. In the present
study, we assessed podoplanin and Ki67 by immunohistochemistry to
determine their role as prognostic indicators.
The Ki67 labeling indices of small-sized thymomas
were less than 4% in all 21 cases in the present study. These
values were relatively low compared to other malignancies (17,18).
In thymic malignancies, Ghazi et al recently reported that
Ki67 labeling indices changed 5% in a thymic typical carcinoid at
the first surgery to 30% in the invasive recurrent lesions at the
second surgery (19). Since Ki67
is a marker of cell proliferation, the result seems to be
reasonable in thymomas with slow growth. Even in the low index of
Ki67, it was of note that the indices showed an increase
concomitant to the progress of staging and histological
classification. These results suggest that the Ki67 labeling index
may not be an optimal biological marker as a prognostic factor of
SSTs.
In a previous study, we showed that podoplanin
correlated with tumor lymphangiogenesis, tumor invasion, lymph node
metastasis of thymoma and poor clinical outcome of thymoma patients
(11). In the present study, a
positive expression of podoplanin was demonstrated only in 2 of 17
SSTs. One thymoma was clinically diagnosed as stage IVb disease as
stated above. The expression of podoplanin in the remaining 15
cases was negative or weakly positive. Podoplanin
immunohistochemistry using a D2–40 antibody may be efficacious to
predict lymphatic metastasis and poor clinical outcome. Although
another thymoma patient with a positive expression of podoplanin is
alive without recurrence, successive follow-up may be
necessary.
While the results of this study are encouraging, it
is acknowledged that any conclusions should be tempered with some
reservations. The small number of patients limited the statistical
analysis of the present study. A larger scale study may reveal the
usefulness of podoplanin immunohistochemistry more clearly and may
demonstrate statistical significance in the analysis of the Ki67
labeling index in SSTs.
In conclusion, we evaluate a deceased case of SST.
Advanced-stage thymomas are possibly included in SSTs although the
majority of SSTs are classified into early stage disease. In
addition, podoplanin analyzed by immunohistochemistry may be useful
in determining the malignant behavior of SSTs.
References
|
1.
|
Masaoka A, Monden Y, Nakahara K and
Tanioka T: Follow-up study of thymomas with special reference to
their clinical stages. Cancer. 48:2485–2492. 1981.
|
|
2.
|
Blumberg D, Port JL, Weksler B, et al:
Thymoma: a multivariate analysis of factors predicting survival.
Ann Thorac Surg. 60:908–913. 1995.
|
|
3.
|
Kondo K and Monden Y: Therapy for thymic
epithelial tumors: a clinical study of 1,320 patients from Japan.
Ann Thorac Surg. 76:878–884. 2003.
|
|
4.
|
Tateyama H, Mizuno T, Tada T, Eimoto T,
Hashimoto T and Masaoka A: Thymic epithelial tumours: evaluation of
malignant grade by quantification of proliferating cell nuclear
antigen and nucleolar organizer regions. Virchows Arch A Pathol
Anat Histopathol. 422:265–269. 1993.
|
|
5.
|
Tateyama H, Eimoto T, Tada T, Mizuno T,
Inagaki H, Hata A, Sasaki M and Masaoka A: p53 protein expression
and p53 gene mutation in thymic epithelial tumors. An
immunohistochemical and DNA sequencing study. Am J Clin Pathol.
104:375–381. 1995.
|
|
6.
|
Pich A, Chiarle R, Chiusa L, Ponti R,
Geuna M, Casadio C, Maggi G and Palestro G: Long-term survival of
thymoma patients by histologic pattern and proliferative activity.
Am J Surg Pathol. 19:918–926. 1995.
|
|
7.
|
Yang WI, Efird JT, Quintanilla-Martinez L,
Choi N and Harris NL: Cell kinetic study of thymic epithelial
tumors using PCNA (PC10) and Ki-67 (MIB-1) antibodies. Hum Pathol.
27:70–76. 1996.
|
|
8.
|
Chen FF, Yan JJ, Jin YT and Su IJ:
Detection of bcl-2 and p53 in thymoma: expression of bcl-2 as a
reliable marker of tumor aggressiveness. Hum Pathol. 27:1089–1092.
1996.
|
|
9.
|
Tateyama H, Eimoto T, Tada T, Inagaki H,
Hattori H and Takino H: Apoptosis, bcl-2 protein, and Fas antigen
in thymic epithelial tumors. Mod Pathol. 10:983–991. 1997.
|
|
10.
|
Takahashi E, Tateyama H, Akatsu H, Fukai
I, Yamakawa Y, Fujii Y and Eimoto T: Expression of matrix
metalloproteinases 2 and 7 in tumor cells correlates with the World
Health Organization classification subtype and clinical stage of
thymic epithelial tumors. Hum Pathol. 34:1253–1258. 2003.
|
|
11.
|
Tateyama H, Sugiura H, Yamatani C and Yano
M: Expression of podoplanin in thymoma: its correlation with tumor
invasion, nodal metastasis, and poor clinical outcome. Hum Pathol.
42:533–540. 2011.
|
|
12.
|
Koga K, Matsuno Y, Noguchi M, Mukai K,
Asamura H, Goya T and Shimosato Y: A review of 79 thymomas:
modification of staging system and reappraisal of conventional
division into invasive and non-invasive thymoma. Pathol Int.
44:359–367. 1994.
|
|
13.
|
Huang J, Detterbeck FC, Wang Z and Loehrer
PJ Sr: Standard outcome measures for thymic malignancies. J Thorac
Oncol. 5:2017–2023. 2010.
|
|
14.
|
Travis WD, Brambilla E, Muller-Hermelink
HK and Harris CC: World Health Organization classification of
Tumours. Pathology and Genetics of Tumours of the Lung, Pleura,
Thymus and Heart. IARC Press; Lyon: pp. 146–151. 2004
|
|
15.
|
Onuki T, Ishikawa S, Iguchi K, et al:
Limited thymectomy for stage I or II thymomas. Lung Cancer.
68:460–465. 2010.
|
|
16.
|
Okumura M, Ohta M, Tateyama H, Nakagawa K,
Matsumura A, Maeda H, Tada H, Eimoto T, Matsuda H and Masaoka A:
The World Health Organization histologic classification system
reflects the oncologic behavior of thymoma: a clinical study of 273
patients. Cancer. 94:624–632. 2002.
|
|
17.
|
Pollack A, DeSilvio M, Khor LY, et al:
Ki-67 staining is a strong predictor of distant metastasis and
mortality for men with prostate cancer treated with radiotherapy
plus androgen deprivation: Radiation Therapy Oncology Group Trial
92-02. J Clin Oncol. 22:2133–2140. 2004.
|
|
18.
|
Yerushalmi R, Woods R, Ravdin PM, Hayes MM
and Gelmon KA: Ki67 in breast cancer: prognostic and predictive
potential. Lancet Oncol. 11:174–183. 2010.
|
|
19.
|
Ghazi AA, Dezfooli AA, Mohamadi F, Yousefi
SV, Amirbaigloo A, Ghazi S, Pourafkari M, Berney D, Ellard S and
Grossman AB: Cushing syndrome secondary to a thymic carcinoid tumor
due to multiple endocrine neoplasia type 1. Endocr Pract.
17:e92–e96. 2011.
|