Introduction
Breast cancer (BC) is one of the most common
malignancies in women. There are >1,000,000 new cases diagnosed
annually worldwide. A marked increase in incidence occurs annually
and in particular among women of younger age, which poses a serious
threat to women’s physical and mental health (1). The occurrence, progression and
prognosis of various types of cancer are complex processes,
involving numerous factors, genes and proteins. Therefore, it is
difficult to determine the biological behavior and prognosis of BC
based on the assessment of a single factor.
Immunohistochemical (IHC) detection has become
essential to many malignancies and plays a key role in tumor
diagnosis, treatment and prognostic assessment. In this study, we
collected 286 cases of invasive BC, confirmed at our pathology
laboratory, detected the expression of estrogen receptor (ER),
progesterone receptor (PR), human epidermal growth factor
receptor-2 (HER2), vascular endothelial growth factor (VEGF),
epidermal growth factor receptor (EGFR), p53, type II toposomerase
(TOPO II) and Ki-67 proteins by IHC and analyzed the associations
between these indicators and the clinicopathological
characteristics, designed to further investigate the associations
of the expressions of hormone receptors, oncogenes and proteins
with BC biological behavior and prognosis, in order to guide
clinical diagnosis and comprehensive treatment.
Materials and methods
Materials
Tissue samples from 286 patients with invasive BC
were collected in Jiangsu Cancer Hospital, Affiliated to Nanjing
Medical University, between February, 2011 and July, 2012. All the
samples were primary cancers, with complete medical records and a
confirmed diagnosis. The patients had not received any treatment
prior to surgery. All patients were female, aged 28–79 years
(median, 51 years). A total of 146 cases were >50 years of age
and the remaining 140 cases were ≤50 years of age. The tumor size
was >2 cm in 122 cases and ≤2 cm in 164 cases. Lymph node
metastasis was identified in 134 cases and 152 cases presented with
non-metastatic lymph nodes, as determined by IHC. Histological
grades were classified according to the WHO histological
classification standards for evaluation of BC (2003). Among the
cases there were 24 grade I, 184 grade II and 78 grade III cases.
Monoclonal antibodies against ER, PR, HER2, VEGF, EGFR, p53, TOPO
II and Ki-67, as well as IHC kits, were purchased from Zhongshan
Jinqiao Biotechnology Co., Ltd. (Beijing, China).
Methods
The samples were fixed in 10% neutral formalin,
desiccated and embedded in paraffin, then sliced into 4-μm
sections. Envision ldpe-g-nvp was used as the staining method. The
primary antibody dilution and process of staining were performed
according to the manufacturer’s instructions. Equivalent
phosphate-buffered saline (PBS) was used as a negative control for
primary antibodies. The results were observed under a microscope.
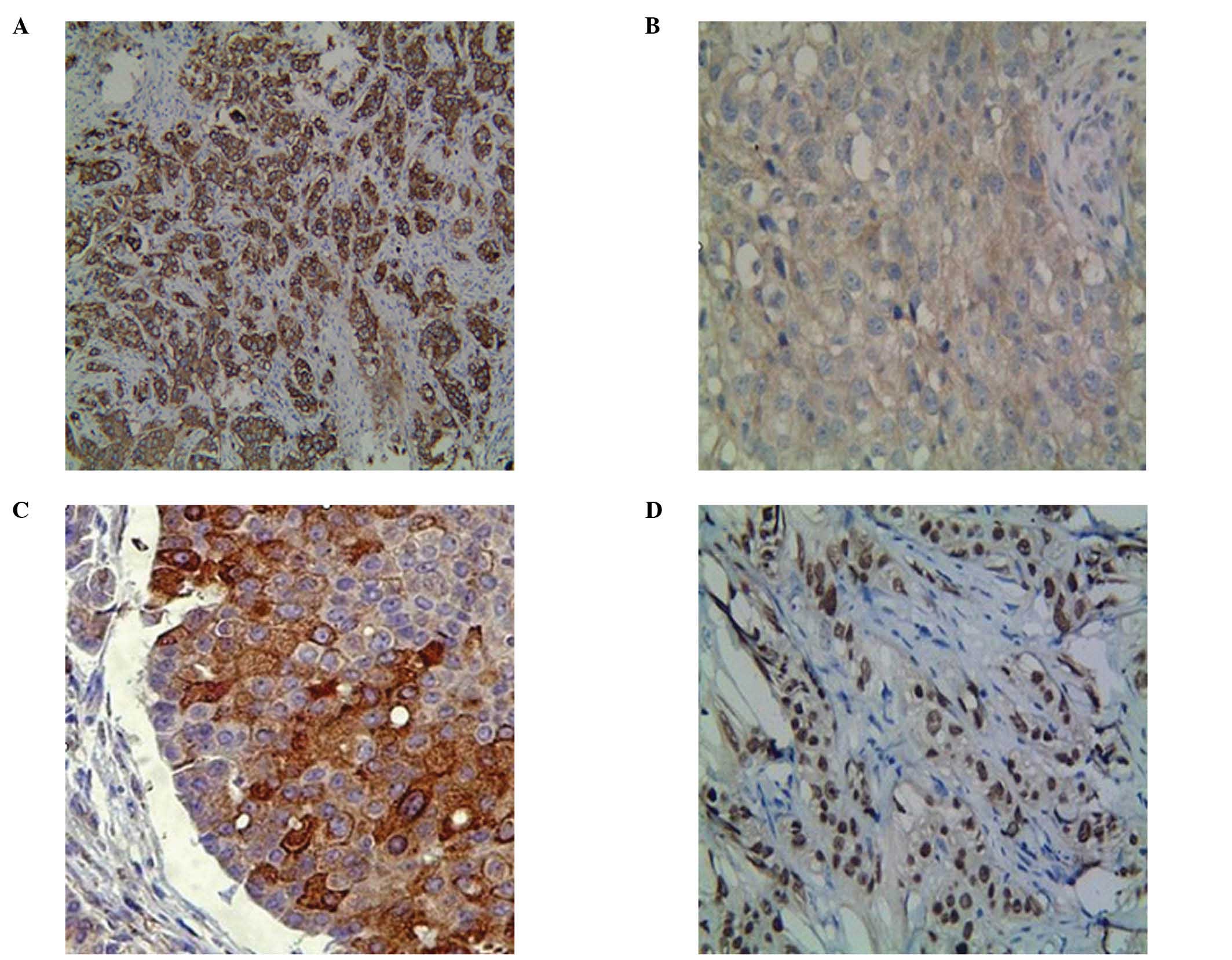
The staining of HER2 was mainly localized in the membrane, EGFR was
localized mainly in the cytoplasm and to a limited extent in the
membrane, VEGF was localized in the cytoplasm and the membrane,
whereas ER, PR, p53, TOPO II and Ki-67 were localized in the
nucleus (Fig. 1). Cells were
classified according to the positive rate and colour intensity as
follows: negative (−), number of positive cells <5%; weak
positive (+), pale brown particles, number of positive cells 6–25%;
positive (++), brown particles, number of positive cells 26–50%;
strong positive (+++), dark brown particles, number of positive
cells >50%. The results of the assessment of HER2-positive cells
were in accordance with those of a previous study (2).
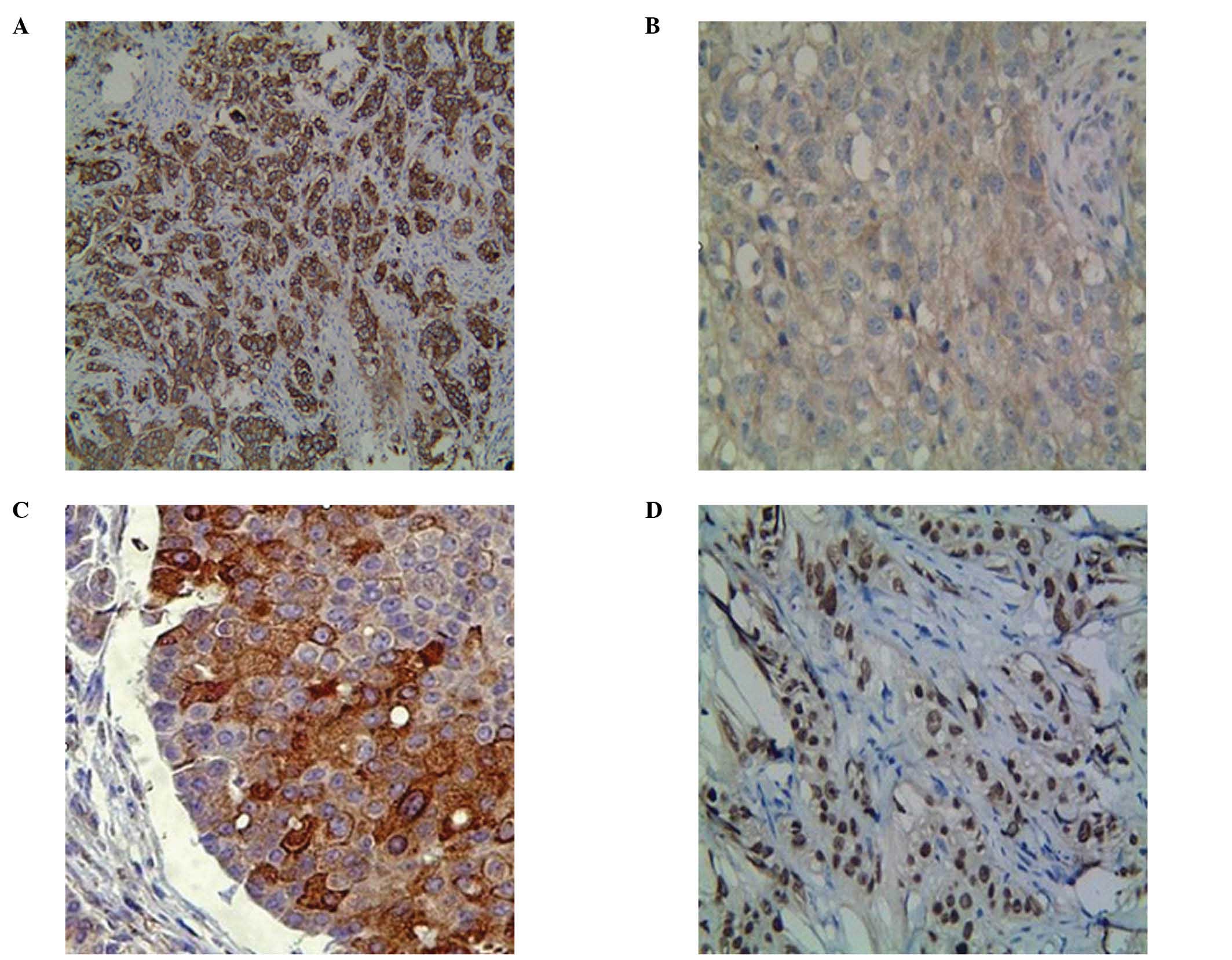 | Figure 1Positive expressions of
immunohistochemical (IHC) indices in invasive breast cancer
tissues. Indices that (A) exist only in the membrane (human
epidermal growth factor receptor-2, HER2), (B) are present mainly
in the cytoplasm (epidermal growth factor receptor, EGFR), (C) are
present in both the cytoplasm and the membrane (vascular
endothelial growth factor, VEGF), (D) are detected only in the
nucleus [estrogen receptor (ER), progesterone receptor (PR), p53,
type II topoisomerase (TOPO II) and Ki-67] are shown. Images were
IHC 3+ or fluorescence in situ hybridisation
(FISH)-positive. EnVision (magnification, ×100/×400). |
Statistical analysis
Statistical analysis was performed with SPSS
software v. 16.0 and the enumeration data were compared with the
Chi-square (χ2) test. P≤0.05 was considered to indicate
a statistically significant difference.
Results
Association between the expressions of
ER, PR and HER2 in breast cancers (BCs) and clinicopathological
characteristics
As shown in Table
I, the positive rates of ER or PR, as well as the
double-positive rate of ER and PR, were highest in the lower age
group (69.51, 55.71 and 51.43%, respectively). ER expression
exhibited a negative correlation with age, tumor size and
histological grade (χ2=4.9284, P=0.0260; χ2=
4.3281, P=0.0370; and χ2=4.1706, P=0.0410,
respectively), PR expression exhibited a negative correlation with
age and histological grade (χ2=10.6550, P=0.0011 and
χ2=4.1649, P=0.0410, respectively) and the
double-positive expression of ER and PR also exhibited a negative
correlation with age and histological grade (χ2=8.6617,
P=0.0033 and χ2=4.1141, P=0.0430, respectively).
However, there was no statistically significant difference among
the indices in lymph node metastasis. The positive rate of HER2 was
highest in the lymph node metastasis group (62.69%); although no
correlation with age, tumor size, lymph node metastasis and
histological grade was evident.
 | Table I.Association between the expressions
of ER, PR and HER2 in BCs and clinicopathological characteristics
[cases, (%)]. |
Table I.
Association between the expressions
of ER, PR and HER2 in BCs and clinicopathological characteristics
[cases, (%)].
| Clinicopathological
characteristics | No. | ER
| PR
| HER2
| ER and PR
|
|---|
| (+) | P-value | (+) | P-value | (+) | P-value | (+) | P-value |
|---|
| Age (years) | | | | | | | | | |
| ≤50 | 140 | 100 (71.42) | 0.0260a | 78 (55.71) | 0.0011b | 74 (52.86) | 0.2280 | 72 (51.43) | 0.0033b |
| >50 | 146 | 78 (54.80) | 4.9284 | 42 (28.76) | 10.6550 | 90 (61.64) | - | 40 (20.40) | 8.6617 |
| Tumor size
(cm) | | | | | | | | | |
| ≤2 | 164 | 114 (69.51) | 0.0370a | 74 (45.12) | 0.3740 | 92 (56.10) | 0.7270 | 70 (42.68) | 0.3170 |
| >2 | 122 | 64 (52.45) | 4.3281 | 46 (37.70) | - | 72 (59.02) | - | 42 (34.42) | - |
| Lymph node
metastasis | | | | | | | | | |
| Positive | 134 | 82 (61.19) | 0.8090 | 50 (37.31) | 0.2900 | 84 (62.69) | 0.2250 | 44 (32.84) | 0.1460 |
| Negative | 152 | 96 (63.16) | - | 70 (46.05) | - | 80 (52.63) | - | 68 (44.74) | - |
| Histological
grade | | | | | | | | | |
| I–II | 208 | 140 (67.31) | 0.0410a | 98 (47.12) | 0.0410a | 118 (56.73) | 0.8090 | 92 (44.23) | 0.0430a |
| III | 78 | 38 (48.71) | 4.1706 | 22 (28.21) | 4.1649 | 46 (58.97) | - | 20 (25.64) | 4.1141 |
Association of the expressions of ER, PR
and HER2 in BCs
As shown in Table
II, the positive rates of ER and PR in the HER2-negative cases
(80.33 and 54.10%, respectively) were significantly higher compared
to the HER2-positive cases (48.78 and 32.93%, respectively). The
expression of PR was closely associated with the ER status
(χ2=42.5299, P=0.0000) and the expressions of ER and PR
were negatively correlated with HER2 (χ2=14.8123,
P=0.0001 and χ2= 6.4381, P= 0.0110, respectively).
 | Table II.Association among the expressions of
ER, PR and HER2 in BCs [cases, (%)]. |
Table II.
Association among the expressions of
ER, PR and HER2 in BCs [cases, (%)].
| Indices | No. | PR
| HER2
|
|---|
| (+) | P-value | (+) | P-value |
|---|
| ER | | | | | |
| (+) | 178 | 112 (66.29) | 0.0000b | 80 (44.94) | 0.0001b |
| (−) | 108 | 8 (7.41) | 42.5299 | 84 (77.78) | 14.8123 |
| PR | | | | | |
| (+) | 120 | - | - | 54 (45.00) | 0.0110a |
| (−) | 166 | - | - | 110 (66.27) | 6.4381 |
| HER2 | | | | | |
| (+) | 164 | 54 (32.93) | 0.0110a | - | - |
| (−) | 122 | 66 (54.10) | 6.4381 | - | - |
Association between the expression of
VEGF, EGFR, p53, TOPO II and Ki-67 in BCs and clinicopathological
characteristics
As shown in Table
III, the expression of EGFR was highest in the lymph node
metastasis group (89.55%) and exhibited a positive correlation with
lymph node metastasis (χ2=5.0690, P=0.0240). The
positive rates of p53 and Ki-67 were highest in the poor
histological grade group (61.54 and 84.62%, respectively), p53
expression was correlated with tumor size and histological grade
(χ2=4.7314, P=0.0300 and χ2=4.6443, P=0.0310,
respectively) and Ki-67 expression was correlated with histological
grade (χ2=5.5000, P=0.0190). The expressions of VEGF and
TOPO II did not statistically differ with age, tumor, lymph node
metastasis and histological grade.
 | Table III.Association between the expressions
of VEGF, EGFR, p53, TOPO II and Ki67 in BCs and clinicopathological
characteristics [cases, (%)]. |
Table III.
Association between the expressions
of VEGF, EGFR, p53, TOPO II and Ki67 in BCs and clinicopathological
characteristics [cases, (%)].
| Clinicopathological
characteristics | No. | VEGF
| EGFR
| p53
| TOPO II
| Ki-67
|
|---|
| (+) | P-value | (+) | P-value | (+) | P-value | (+) | P-value | (+) | P-value |
|---|
| Age (years) | | | | | | | | | | | |
| ≤50 | 140 | 68 (48.57) | 0.2150 | 112 (80.00) | 0.3047 | 64 (45.71) | 0.7893 | 70 (50.00) | 0.2850 | 104 (74.29) | 0.2660 |
| >50 | 146 | 86 (58.90) | - | 122 (83.56) | - | 70 (47.95) | - | 86 (58.90) | - | 96 (65.75) | - |
| Tumor size
(cm) | | | | | | | | | | | |
| ≤2 | 164 | 86 (52.44) | 0.6960 | 132 (80.49) | 0.6320 | 64 (39.02) | 0.0300a | 86 (52.44) | 0.5580 | 110 (67.07) | 0.3880 |
| >2 | 122 | 68 (55.74) | - | 102 (83.61) | - | 70 (57.38) | 4.7314 | 70 (57.38) | - | 90 (73.77) | - |
| Lymph node
metastasis | | | | | | | | | | | |
| Positive | 134 | 80 (59.70) | 0.1870 | 120 (89.55) | 0.0240a | 56 (41.79) | 0.2550 | 70 (52.24) | 0.6030 | 96 (71.64) | 0.6750 |
| Negative | 152 | 74 (48.68) | - | 114 (75.00) | 5.0690 | 78 (51.32) | - | 86 (56.58) | - | 104 (68.42) | - |
| Histological
grade | | | | | | | | | | | |
| I-II | 208 | 110 (52.88) | 0.7060 | 168 (80.77) | 0.5950 | 86 (41.35) | 0.0310a | 108 (51.92) | 0.3040 | 134 (64.42) | 0.0190a |
| III | 78 | 44 (56.41) | - | 66 (84.62) | - | 48 (61.54) | 4.6443 | 48 (61.54) | - | 66 (84.62) | 5.5000 |
Association between the expressions of
ER, PR and HER2 and the expressions of VEGF, EGFR, p53, TOPO II and
Ki-67 in BCs
As shown in Table
IV, the expression of VEGF exhibited a negative correlation
with ER and PR status (χ2=5.7384, P=0.0166 and
χ2=10.0099, P=0.0016, respectively) and a positive
correlation with HER2 expression (χ2=5.3917, P=0.0202).
The expressions of EGFR, p53, TOPO II and Ki-67 were closely
associated with HER2 status (χ2=9.1730, P=0.0020;
χ2=18.1705, P=0.0000; χ2=14.6526, P=0.0000
and χ2=7.9717, P=0.0050, respectively).
 | Table IV.Association between the expressions
of ER, PR and HER2 and the expressions of VEGF, EGFR, p53, TOPO II
and Ki67 in BCs [cases, (%)]. |
Table IV.
Association between the expressions
of ER, PR and HER2 and the expressions of VEGF, EGFR, p53, TOPO II
and Ki67 in BCs [cases, (%)].
| Indices | No. | VEGF
| EGFR
| p53
| TOPO II
| Ki-67
|
|---|
| (+) | P-value | (+) | P-value | (+) | P-value | (+) | P-value | (+) | P-value |
|---|
| ER | | | | | | | | | | | |
| (+) | 178 | 82 (46.07) | 0.0166a | 144 (80.90) | 0.7140 | 82 (46.07) | 0.8090 | 98 (55.06) | 0.8750 | 120 (67.42) | 0.4000 |
| (−) | 108 | 72 (66.67) | 5.7384 | 90 (83.33) | - | 52 (48.15) | - | 58 (53.70) | - | 80 (74.07) | - |
| PR | | | | | | | | | | | |
| (+) | 120 | 46 (38.33) | 0.0016b | 92 (76.67) | 0.1740 | 52 (43.33) | 0.4730 | 62 (51.67) | 0.5040 | 78 (65.00) | 0.2740 |
| (−) | 166 | 108 (65.06) | 10.0099 | 142 (85.54) | - | 82 (49.40) | - | 94 (56.63) | - | 122 (73.49) | - |
| HER2 | | | | | | | | | | | |
| (+) | 164 | 102 (62.20) | 0.0202a | 148 (90.24) | 0.0020b | 102 (62.20) | 0.0000b | 112 (68.29) | 0.0000b | 130 (79.27) | 0.0050b |
| (−) | 122 | 52 (42.62) | 5.3917 | 86 (70.49) | 9.1730 | 32 (26.23) | 18.1705 | 44 (36.07) | 14.6526 | 70 (57.38) | 7.9717 |
Association among the expressions of
VEGF, EGFR, p53, TOPO II and Ki-67 in BCs
As shown in Table
V, the expression of TOPO II exhibited a negative correlation
with EGFR and a positive correlation with p53 and Ki-67
(χ2=4.40160, P=0.03600; χ2=10.12500,
P=0.00150 and χ2=14.66030, P=0.00013, respectively). The
expression of Ki-67 was significantly correlated with p53
(χ2=11.17360, P=0.00083). The association between the
expression of VEGF and the levels of EGFR, p53, TOPO II and Ki-67
was not statistically significant.
 | Table V.Association among the expressions of
VEGF, EGFR, p53, TOPO II and Ki67 in BCs [cases, (%)]. |
Table V.
Association among the expressions of
VEGF, EGFR, p53, TOPO II and Ki67 in BCs [cases, (%)].
| Indices | No. | EGFR
| p53
| TOPO II
| Ki-67
|
|---|
| (+) | P-value | (+) | P-value | (+) | P-value | (+) | P-value |
|---|
| VEGF | | | | | | | | | |
| (+) | 154 | 132 (85.71) | 0.19200 | 70 (45.45) | 0.97900 | 82 (53.25) | 0.73600 | 108 (70.13) | 0.95500 |
| (−) | 132 | 102 (77.27) | - | 64 (48.48) | - | 74 (56.06) | - | 92 (69.69) | - |
| EGFR | | | | | | | | | |
| (+) | 234 | - | - | 110 (40.01) | 0.93700 | 118 (50.43) | 0.03600a | 166 (70.94) | 0.57600 |
| (−) | 52 | - | - | 24 (46.15) | - | 38 (70.08) | 4.40160 | 34 (65.38) | - |
| p53 | | | | | | | | | |
| (+) | 134 | 110 (82.09) | 0.93700 | - | - | 92 (68.66) | 0.00150b | 112 (83.58) | 0.00083b |
| (−) | 152 | 124 (81.58) | - | - | - | 64 (42.11) | 10.12500 | 88 (57.89) | 11.17360 |
| TOPO II | | | | | | | | | |
| (+) | 156 | 118 (75.64) | 0.03600a | 92 (58.97) | 0.00150b | - | - | 130 (83.33) | 0.00013b |
| (−) | 130 | 116 (89.23) | 4.40160 | 42 (32.31) | 10.12500 | - | - | 70 (53.85) | 14.66030 |
Association between the IHC approximate
molecular subtypes of BC and clinicopathological
characteristics
As shown in Table
VI, in all the cases, the percentages of Luminal A, Luminal B,
HER2/neu and triple-negative subtype were 20.98, 45.45, 26.57 and
9.09%, respectively. The proportion of Luminal A subtype was
highest in the non-metastatic lymph node group (25%) and decreased
with increasing histological grade; however, there was no
statistically significant difference in these data. The proportion
of Luminal B subtype was highest in the lower age group (58.57%),
with a statistically significant difference (χ2=9.5156,
P=0.0020). However, it was higher in the poor histological grade
group, although the difference was not statistically significant.
The proportion of the HER2/neu subtype was highest in the poor
histological grade group (38.46%) and exhibited a statistically
significant difference in age and histological grade
(χ2=8.2871, P= 0.0040 and χ2=3.8841,
P=0.0490, respectively). The proportion of the triple-negative
subtype was highest in the poor histological grade group (17.95%),
the difference was statistically significant (χ2=5.0910,
P=0.0240) and exhibited no correlation with age, tumor size or
lymph node metastasis.
 | Table VI.Association between the IHC
approximate molecular subtypes of BC and clinicopathological
characteristics [cases, (%)]. |
Table VI.
Association between the IHC
approximate molecular subtypes of BC and clinicopathological
characteristics [cases, (%)].
| Clinicopathological
characteristics | No. | Luminal A
| Luminal B
| HER2/neu subtype
(non-Luminal)
| Triple-negative
|
|---|
| Yes | P-value | Yes | P-value | Yes | P-value | Yes | P-value |
|---|
| Age (years) | | | | | | | | | |
| ≤50 | 140 | 28 (20.00) | 0.7780 | 82 (58.57) | 0.0020b | 22 (15.71) | 0.0040b | 12 (8.57) | 0.8320 |
| >50 | 146 | 32 (21.92) | - | 48 (32.87) | 9.5156 | 54 (36.98) | 8.2871 | 14 (9.59) | - |
| Tumor size
(cm) | | | | | | | | | |
| ≤2 | 164 | 38 (23.17) | 0.4550 | 78 (47.56) | 0.5580 | 34 (20.73) | 0.0670 | 14 (8.54) | 0.7890 |
| >2 | 122 | 22 (18.03) | - | 52 (42.62) | - | 42 (34.43) | - | 12 (9.84) | - |
| Lymph node
metastasis | | | | | | | | | |
| Positive | 134 | 22 (16.42) | 0.2080 | 66 (49.25) | 0.3920 | 40 (29.85) | 0.4050 | 10 (7.46) | 0.5250 |
| Negative | 152 | 38 (25.00) | - | 64 (42.11) | - | 36 (23.68) | - | 16 (10.52) | - |
| Histological
grade | | | | | | | | | |
| I-II | 208 | 50 (24.04) | 0.1423 | 100 (48.08) | 0.3040 | 46 (22.12) | 0.0490a | 12 (5.77) | 0.0240a |
| III | 78 | 10 (12.82) | - | 30 (38.46) | - | 30 (38.46) | 3.8841 | 14 (17.95) | 5.0910 |
Discussion
Several tumors are hormone-dependent and BC is a
typical example. ER and PR play important roles in the growth and
differentiation of BCs while their expression levels are decisive
factors guiding the endocrine treatment of BCs, and important
prognostic markers. Our data demonstrated that the positive rates
of ER and PR were 62.24 and 41.96%, which was in agreement with the
findings of a previous study (3).
Furthermore, this study demonstrated that ER expression decreased
with increasing histological grade, indicating that the lower the
tumor cell differentiation, the lower the estrogen dependence, thus
affecting the sensitivity to hormone therapy. The association
between ER expression and lymph node metastasis was diverse in
previous studies (4,5). Our results demonstrated that the
expression of ER was negatively correlated with age and tumor size
and had no correlation with lymph node metastasis. ER expression
may not be an independent prognostic factor, as PR and ER are
steroid hormone receptors that belong to the nuclear receptor
superfamily and PR is a derivative of estrogen and ER combination.
A previous study showed that the tumor-free survival of PR-positive
BC patients was significantly longer compared to those of
PR-negative BC patients (6). PR
may downregulate the expression of breast cancer resistance protein
(BCRP) and increase chemosensitivity (7). Our study showed that the expression
of PR exhibited statistically significant differences with age and
histological grade, which may be related to the presence of
independent regulatory pathways affected by PR but not ER. Data
also showed that PR expression was decreased in lymph node
metastasis. Further analysis demonstrated that the double-positive
rate of ER and PR was 39.16% and it was significantly different in
lymph node metastasis and histological grade. Thus, it is essential
that ER and PR are assessed as a whole to determine patient
prognosis. With the development of the tumor, part of ER-positive
and/or PR-positive patients start exhibiting hormone therapy
resistance and this ‘escape’ mechanism of ER and PR requires
further investigation (8,9).
HER2, a proto-oncogene, also known as c-erbB-2 or
HER2/neu, located on chromosome 17q21, is considered to be closely
associated with the occurrence and development of BC (10). Under normal physiological
conditions HER2 is inactive; however, once activated, it may
enhance tumor invasion and metastasis and increase the degree of
malignancy (11). A previous study
reported that HER2 overexpression in BCs indicated poor prognosis
(12). Schillaci et al
(13) identified NuclErbB-2
positivity as a significant independent predictor of worse overall
survival (OS) in patients with MembErbB-2 overexpression. Our
results demonstrated that the expressions of ER and PR were
significantly correlated with c-erbB-2 status, which was in
agreement with findings reported by previous studies (14,15).
The presence of HER2 reduced the efficacy of endocrine therapy,
therefore, the efficacy of endocrine therapy was increased with
targeted inhibition of the expression of HER2 (16). Our study identified an association
between HER2 status and the expressions of ER and PR: HER2
overexpression may exert an inhibitory effect on the expressions of
ER and/or PR. Our results also demonstrated that the expression of
HER2 was enhanced with increasing age and lymph node metastasis;
although, these data were not statistically significant. The
anti-HER2 monoclonal antibodies have been used in the clinical
treatment of BC patients. However, due to the variations of
chromosome 17 and HER2/neu genetic heterogeneity, IHC and FISH
assay assessment of HER2 expression is required prior to targeted
therapy (17).
Thus far, VEGF is known as the most important
angiogenesis-promoting factor, is highly expressed in several
malignant tumors and plays an important role in the occurrence,
development and metastasis of tumors (18,19).
Combining VEGF with p53 status may result in a better prognostic
prediction in BC patients (20).
Our results demonstrated that the positive rate of VEGF expression
in BCs was 53.85% and the positive expression levels were higher in
the lymph node metastasis group compared to the non-metastatic
group; however, there were no statistically significant differences
with age, tumor size, lymph node metastasis and histological grade,
a finding consistent with those of Jobim et al (21). Our data also showed that VEGF
expression was negatively correlated with ER and PR status and
positively correlated with HER2 status, which was in agreement with
the findings of Linderholm et al (22), who reported that triple-negative
BCs (TNBCs) have a higher VEGF level compared to non-TNBC.
EGFR belongs to the tyrosine kinase receptor family
and is associated with cell growth, proliferation and
differentiation. It was previously demonstrated that 50–70% of
TNBCs express EGFR (23) and EGFR
overexpression was associated with TNBCs and unfavorable prognosis
(24). TNBCs with a low EGFR
expression exhibited a lower incidence of metastasis (25). Our data showed that the positive
rate of EGFR expression in BCs was as high as 81.82% and its
expression was significantly correlated with lymph node metastasis
and HER2 status (P<0.05). Its expression in ER- or PR-positive
groups was lower compared to that in ER- or PR-negative groups;
however, the difference was not statistically significant, which is
consistent with the findings of a previous study (26).
The p53 gene is located on human chromosome 17p13.1
and its main function is to induce cell cycle arrest and apoptosis
and to promote cell differentiation. The p53 gene may be found as
wild-type or mutant and the mutant form prevents the wild-type p53
gene from inhibiting tumor formation, leading to cell
transformation and cancerization (27). The five-year survival rate of
patients with p53-positive BC was significantly lower compared to
that of p53-negative BC patients (28). Our results showed the positive rate
of p53 protein is 46.8% in BCs, which was statistically correlated
with tumor size and histological grade and its expression in the
lymph node metastasis group was higher compared to that in the
non-metastatic group, although the difference was not statistically
significant, which was in agreement with the above viewpoints and
the findings of a previous study (29). Futhermore, we observed that the p53
positive expression rates in the ER- or PR-positive groups were
lower compared to those in the ER- or PR-negative groups and had a
positive correlation with HER2 status, which was in agreement with
the findings of previous studies (29,30),
indicating that they may exert a synergistic effect on endocrine
and targeted therapies.
The TOPO II gene is located on human chromosome
17q21.3 and plays a key role in DNA melting, linking, repair and
replication. Our study demonstrated that TOPO II expression in BC
tissues was higher in the poor histological grade and lymph node
metastasis groups, a finding consistent with those reported by a
previous study (31). Therefore,
the level of TOPO II expression may reflect the proliferation and
metastatic status of BCs, guiding clinical treatment. Our data
demonstrated that TOPO II expression exhibited a significant
positive correlation with HER2 status, which was in agreement with
previous findings (32). We also
observed that TOPO II expression was significantly correlated with
the status of EGFR, p53 and Ki-67 (P<0.05), indicating the
presence of interactions among these indicators, regulating the
progression of tumorigenesis and metastasis of BCs.
Ki-67 is a nuclear antigen related to cell
proliferation, only expressed by the proliferating cell nucleus.
The expression of Ki-67 is an IHC index detecting cell
proliferative activity (33). The
levels of Ki-67 expression in BCs were significantly higher
compared to those in benign breast lesions and were elevated with
increasing cancer cell atypia, which was significant for evaluating
the prognosis of BCs (34,35). Our data showed that Ki-67
expression was significantly correlated with poor histological
grade and was higher in the lymph node metastasis group compared to
the non-metastatic group, indicating that Ki-67 expression is
associated with tumor cell differentiation, invasion and
metastasis. Ki-67 expression exhibited a significantly positive
correlation with HER2 status, more pronounced in the ER- or
PR-negative BCs compared to the ER- or PR-positive BCs, which was
in agreement with previous findings (36). Furthermore, our study also
demonstrated that the expression of Ki-67 exhibited a significantly
positive correlation with cell proliferation-associated nuclear
proteins, p53 and TOPO II, suggesting that Ki-67 is closely related
to the proliferation of BC cells.
To divide BCs into various subtypes is an inevitable
trend for the investigation and treatment of BCs. In accordance
with the intrinsic genotyping, BC is divided into four subtypes:
Luminal A, Luminal B, HER2/neu and basal-like subtype. Luminal B
type was further subdivided into the high Ki-67 expression and
HER2-positive subtypes according to Cheang et al (37). However, most experts agree that
practically, the results of the detection of ER, PR, HER-2 and
Ki-67 indices, equally divide BCs into four types as close
substitutes, including Luminal A, Luminal B, HER2/neu and
triple-negative subtypes (Table
VII). The triple-negative subtype exhibits an almost 80%
overlap with the basal-like subtype. Xue et al (38) collected a total of 5,809 patients
with invasive ductal carcinoma and retrospectively analyzed their
clinicopathological characteristics and survival rates. Of these
patients, 31.1% were Luminal A, 30.4% were Luminal B (high Ki-67),
13.1% were Luminal B (HER2/neu+), 9.0% were HER2/neu and 16.5% were
triple-negative subtype. The patients with Luminal B subtype were
mainly distributed in the lower age group (<43 years old), the
HER2/neu subtype was closely associated with tumor size, lymph
node-positive status and vascular invasion and the triple-negative
BCs were associated with poor histological grade (38). Our study results were mostly
consistent with these findings, however, there were also certain
differences: for example, the ratio of the patients with the
HER2/neu subtype was 26.57% and it exhibited a significantly
negative correlation with age, a finding that was in agreement with
those of Munjal et al (39).
 | Table VII.Definition and treatment strategies
of BC subtypes according to the St. Gallen consensus in 2011. |
Table VII.
Definition and treatment strategies
of BC subtypes according to the St. Gallen consensus in 2011.
| Subtypes | Definition | Treatment
strategies |
|---|
| Luminal A | ER+ and/or PR+,
HER2 and Ki-67 low expression (<14%) | Endocrine
therapy |
| Luminal B | Luminal B
(HER2-negative) | Endocrine therapy ±
cytotoxic therapy |
| ER+ and/or PR+,
HER2 and Ki-67 high expression (≥14%) | |
| Luminal B
(HER2/neu+) | |
| ER+ and/or PR+,
HER2 overexpression and Ki-67 uncertain | Endocrine therapy ±
cytotoxic therapy + anti-HER2 therapy |
| Her2/neu | HER2/neu subtype
(non-Luminal) | Cytotoxic therapy +
anti-HER2 therapy |
| ER and PR
deficiency | |
| HER2 overexpression
or proliferation | |
|
Triple-negative | ER and PR
deficiency, HER2 | Cytotoxic
therapy |
In conclusion, the development of malignancy is a
process involving multiple factors, genes and steps. Our study
demonstrated that ER, PR, HER2, VEGF, EGFR, p53, TOPO II and Ki-67
exhibited high expression levels in invasive BCs and they also
exhibited certain interactions. As regards the associations between
these indices and the clinicopathological characteristics of BCs,
our results were mostly consistent with those of related previous
studies, with certain differences and novel observations. Joint
detection of various IHC indices may more accurately determine the
biological characteristics and predict the prognosis of BCs, as
well as provide a theoretical basis for the diagnosis and treatment
of BCs (40). The ongoing
scientific investigation may lead to the identification of novel
IHC indices associated with BCs.
Acknowledgements
This study was supported by the
Natural Science Foundation of China (30840093) and the Social
Science and Technology Development Projects in Jiangsu
(BS2007077).
References
|
1.
|
Liu C, Zhang H, Shuang C, Lu Y, Jin F, Xu
H and Lu P: Alterations of ER, PR, HER-2/neu, and P53 protein
expression in ductal breast carcinomas and clinical implication.
Med Oncol. 27:747–752. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Hicks DG and Kulkarni S: HER2+ breast
cancer: review of biologic relevance and optimal use of diagnostic
tools. Am J Clin Pathol. 129:263–273. 2008.
|
|
3.
|
Recăreanu F, Simionescu C, Georgescu CV
and Pirici E: Ductal invasive mammary carcinoma -
clinicopathological prognostic factors related to
immunohistochemical expression of hormonal receptors and Her2/neu
oncoprotein. Rom J Morphol Embryol. 52:1059–1064. 2011.
|
|
4.
|
Woolcott CG, SenGupta SK, Hanna WM and
Aronson KJ: Estrogen and progesterone receptor levels in
nonneoplastic breast epithelium of breast cancer cases versus
benign breast biopsy-controls. BMC Cancer. 8:1302008. View Article : Google Scholar
|
|
5.
|
Walker RA: Immunohistochemical markers as
predictive tools for breast cancer. J Clin Pathol. 61:689–696.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Wang ZB, Zhao P, Liu M and Li XH:
Expression of ER, PR and Cyclin D1 in breast infiltrating ductal
carcinoma and their clinicopathological significance. Zhonghua Yi
Xue Za Zhi. 85:514–517. 2005.(In Chinese).
|
|
7.
|
Wu X, Zhang X, Zhang H, et al:
Progesterone receptor down-regulates breast cancer resistance
protein expression via binding to the progesterone response element
in breast cancer. Cancer Sci. 103:959–967. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Daniel AR, Hagan CR and Lange CA:
Progesterone receptor action: defining a role in breast cancer.
Expert Rev Endocrinol Metab. 6:359–369. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Wargon V, Fernandez SV, Goin M, et al:
Hypermethylation of the progesterone receptor A in constitutive
antiprogestin-resistant mouse mammary carcinomas. Breast Cancer Res
Treat. 126:319–332. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Gown AM: Current issues in ER and HER-2
testing by IHC in breast cancer. Mod Pathol. 21(Suppl 2): S8–S15.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Guo H and Bai O: Relationship between the
expression of ER, PR, Her -2 in breast cancer and its clinical
pathological features. Chin J Lab Diagn. 12:1390–1392. 2008.
|
|
12.
|
Bagaria SP, Ray PS, Wang J, et al:
Prognostic value of basal phenotype in HER2-overexpressing breast
cancer. Ann Surg Oncol. 19:935–940. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Schillaci R, Guzmán P, Cayrol F, et al:
Clinical relevance of ErbB-2/HER2 nuclear expression in breast
cancer. BMC Cancer. 12:742012. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Hussein MR, Abd-Elwahed SR and Abdulwahed
AR: Alterations of estrogen receptors, progesterone receptors and
c-erbB2 oncegene protein expression in ductal carcinomas of the
breast. Cell Biol Int. 32:698–707. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Taucher S, Rudas M, Mader RM, et al: Do we
need HER-2/neu testing for all patients with primary breast
carcinoma? Cancer. 98:2547–2553. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Prat A and Baselga J: The role of hormonal
therapy in the management of hormonal-receptor-positive breast
cancer with co-expression of HER2. Nat Clin Pract Oncol. 5:531–542.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Murthy SS, Sandhya DG, Ahmed F, et al:
Assessment of HER2/Neu status by fluorescence in situ hybridization
in immunohistochemistry-equivocal cases of invasive ductal
carcinoma and aberrant signal patterns: a study at a tertiary
cancer center. Indian J Pathol Microbiol. 54:532–538. 2011.
View Article : Google Scholar
|
|
18.
|
Kowanetz M and Ferrara N: Vascular
endothelial growth factor signaling pathways: therapeutic
perspective. Clin Cancer Res. 12:5018–5022. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Zhao YC, Ni XJ, Wang MH, Zha XM, Zhao Y
and Wang S: Tumor-derived VEGF-C, but not VEGF-D, promotes sentinel
lymph node lymphangiogenesis prior to metastasis in breast cancer
patients. Med Oncol. 29:2594–2600. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Linderholm BK, Lindahl T, Holmberg L,
Klaar S, Lennerstrand J, Henriksson R and Bergh J: The expression
of vascular endothelial growth factor correlates with mutant p53
and poor prognosis in human breast cancer. Cancer Res.
61:2256–2260. 2001.PubMed/NCBI
|
|
21.
|
Jobim FC, Schwartsmann G, Xavier NL, et
al: Expression of MMP-9 and VEGF in breast cancer: correlation with
other prognostic indicators. Rev Bras Ginecol Obstet. 30:287–293.
2008.(In Portuguese).
|
|
22.
|
Linderholm BK, Hellborg H, Johansson U, et
al: Significantly higher levels of vascular endothelial growth
factor (VEGF) and shorter survival times for patients with primary
operable triple-negative breast cancer. Ann Oncol. 20:1639–1646.
2009. View Article : Google Scholar
|
|
23.
|
Burness ML, Grushko TA and Olopade Ol:
Epidermal growth factor receptor in triple-negative and basal-like
breast cancer: promising clinical target or only a marker? Cancer
J. 16:23–32. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Kallel I, Khabir A, Boujelbene N, et al:
EGFR overexpression relates to triple negative profile and poor
prognosis in breast cancer patients in Tunisia. J Recept Signal
Transduct Res. 32:142–149. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
Viale G, Rotmensz N, Maisonneuve P, et al:
Invasive ductal carcinoma of the breast with the ‘triple-negative’
phenotype: prognostic implications of EGFR immunoreactivity. Breast
Cancer Res Treat. 116:317–328. 2009.
|
|
26.
|
Skobe M, Hawighorst T, Jackson DG, et al:
Induction of tumor lymphangiogenesis by VEGF-C promotes breast
cancer metastasis. Nat Med. 7:192–198. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Kazemi M, Salehi Z and Chakosari RJ: TP53
codon 72 polymorphism and breast cancer in northern Iran. Oncol
Res. 18:25–30. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Dookeran KA, Dignam JJ, Ferrer K, et al:
p53 as a marker of prognosis in African-American women with breast
cancer. Ann Surg Oncol. 17:1398–1405. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
González-Rodilla I, Verna V, Muñoz AB,
Estévez J, Boix M and Schneider J: Expression of the
apoptosis-related genes Bcl-2 and p53 in clinical samples from
endometrial carcinoma patients. Anticancer Res. 31:4191–4193.
2011.PubMed/NCBI
|
|
30.
|
Mao XY, Fan CF, Zheng HC, Wei J, Yao F and
Jin F: p53 nuclear accumulation and ERalpha expression in ductal
hyperplasia of breast in a cohort of 215 Chinese women. J Exp Clin
Cancer Res. 29:1122010. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Tokiniwa H, Horiguchi J, Takata D, et al:
Topoisomerase II alpha expression and the Ki-67 labeling index
correlate with prognostic factors in estrogen receptor-positive and
human epidermal growth factor type-2-negative breast cancer. Breast
Cancer. 19:309–314. 2012. View Article : Google Scholar
|
|
32.
|
Tanner B, Pilch H, Schäffer U, et al:
Expression of c-erbB-2 and topoisomerase II alpha in relation to
chemoresistance in ovarian cancer. Zentralbl Gynakol. 124:176–183.
2002.(In German).
|
|
33.
|
Urruticoechea A, Smith IE and Dowsett M:
Proliferation marker Ki-67 in early breast cancer. J Clin Oncol.
23:7212–7220. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
de Azambuja E, Cardoso F, de Castro G Jr,
et al: Ki-67 as prognostic marker in early breast cancer: a
meta-analysis of published studies involving 12,155 patients. Br J
Cancer. 96:1504–1513. 2007.PubMed/NCBI
|
|
35.
|
Dowsett M, Nielsen TO, A’hern R, et al:
Assessment of Ki67 in breast cancer: recommendations from the
International Ki67 in Breast Cancer Working Group. J Natl Cancer
Inst. 103:1656–1664. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
36.
|
Endo Y, Toyama T, Takahashi S, et al: High
estrogen receptor expression and low Ki67 expression are associated
with improved time to progression during first-line endocrine
therapy with aromatase inhibitors in breast cancer. Int J Clin
Oncol. 16:512–518. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Cheang MC, Chia SK, Voduc D, et al: Ki67
index, HER2 status, and prognosis of patients with Luminal B breast
cancer. J Natl Cancer Inst. 101:736–750. 2009. View Article : Google Scholar
|
|
38.
|
Xue C, Wang X, Peng R, et al:
Distribution, clinicopathologic features and survival of breast
cancer subtypes in Southern China. Cancer Sci. 103:1679–1687. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Munjal K, Ambaye A, Evans MF, Mitchell J,
Nandedkar S and Cooper K: Immunohistochemical analysis of ER, PR,
Her2 and CK5/6 in infiltrative breast carcinomas in Indian
patients. Asian Pac J Cancer Prev. 10:773–778. 2009.PubMed/NCBI
|
|
40.
|
Moriya T, Kanomata N, Kozuka Y, et al:
Molecular morphological approach to the pathological study of
development and advancement of human breast cancer. Med Mol
Morphol. 43:67–73. 2010. View Article : Google Scholar : PubMed/NCBI
|