Introduction
Muscle-invasive bladder cancer (MIBC), which
constitutes 30% of all bladder cancers (BCs), is responsible for an
annual death toll of ∼15,000 individuals in the United States
(1). A viable treatment option for
MIBC includes trimodality therapy with a combination of
transurethral bladder resection (TURBT), chemotherapy and radiation
(with cystectomy for failures), although this method has never been
compared to radical cystectomy in randomized clinical trials. This
type of treatment has achieved cure rates comparable to extirpative
surgery, while preserving a functional bladder (2–4).
This combined-modality approach is also a treatment of choice for
several patients who may be unsuitable for surgery.
Chemotherapy administered either sequentially or
concomitantly with radiation is crucial for organ preservation in
BC by improving local effectiveness (5–7) and
increasing survival (7). When
administered as systemic agents for BC, platinum- and/or
gemcitabine-based regimens are effective in metastatic disease and
are also increasingly utilized in the neoadjuvant and adjuvant
settings (8). However, the
selection of the most appropriate chemotherapy regimen varies, with
certain physicians favoring cisplatin-based regimens, such as
methotrexate, vinblastine, doxorubicin and cisplatin, or cisplatin,
methotrexate and vinblastine, due to their long history of use,
whereas others favor gemcitabine-based regimens, which are more
tolerable (8). Molecular markers
that may aid the selection of appropriate chemotherapy regimens are
currently under investigation; however, the number of available
studies investigating the molecular prognostic markers in
trimodality therapy is currently limited.
Ribonucleoside reductase subunit M1 (RRM1), a
substrate-binding and regulatory subunit of ribonucleotide
reductase, is the primary cellular target of gemcitabine (9). The overexpression of RRM1 was
implicated in resistance to gemcitabine in various tumor cell lines
and models (9–11). Excision repair
cross-complementation group 1 (ERCC1) is a key part of the
nucleotide-excision repair pathway that removes platinum-DNA
adducts and counteracts the cytotoxic effects of platinum agents
(12). ERCC1 expression was
reported to confer resistance to platinum derivatives and has been
evaluated as a predictive and prognostic marker in various tumors,
where platinum is the cornerstone of chemotherapy (12–17).
ERCC1 was also implicated in repairing DNA double-strand breaks and
conferring resistance to ionizing radiation, which may help
identify the patients that are most suitable to undergo radical
cystectomy compared to trimodality therapy (15,18).
The aim of this study was to test the hypothesis
that RRM1 and ERCC1 expression predict tumor response and clinical
outcome in patients with MIBC treated with combined platinum- or
gemcitabine-based chemotherapy and radiation.
Materials and methods
Patients and treatment
An institutional review board-approved study was
undertaken on patients treated with chemoradiotherapy for MIBC in
the University of Michigan (Ann Arbor, MI, USA) between 1999 and
2012. A total of 83 patients with MIBC were identified, among whom
39 had pretreatment tumor samples suitable for the construction of
tissue microarrays (TMAs). There was no uniform treatment protocol
for MIBC; thus, the patients were treated with either neoadjuvant
polychemotherapy followed by radiation or with concomitant
chemoradiotherapy from the beginning. Prior to treatment, all the
patients underwent cystoscopy, TURBT and abdominopelvic and chest
imaging by computed tomography (CT). Following treatment and during
follow-up, the patients underwent periodic cystoscopy and CT every
3–4 months for the first 2 years and less frequently
thereafter.
For radiotherapy planning, all the patients
underwent CT-based simulation. The target volume included either
the bladder alone with a margin of ≥1.5–cm, or the bladder with
margins and the pelvic lymph nodes. The prescribed dose to the
bladder was 59.4–64.8 Gy and to the pelvis 39.6–50 Gy. Radiation
was delivered in 1.8- to 2-Gy daily fractions using ≥6 MV photons.
For the statistical analysis, all the fractions were converted into
2-Gy equivalent dose using an α/β ratio of 10.
Immunohistochemical analysis of ERCC1 and
RRM1 expression
There is currently no standard method for the
evaluation of ERCC1 and RRM1 expression; thus, immunohistochemical
analysis and quantitative reverse transcription-polymerase chain
reaction (qRT-PCR) were previously used to determine ERCC1 and RRM1
expression. The decision to use immunostaining in our study was
based on a previous study reporting that ERCC1 and RRM1 mRNA
measurements by qRT-PCR were not correlated with
immunohistochemical findings and that immunostaining was better
correlated with survival parameters compared to mRNA measurements
in non-small-cell lung cancer (NSCLC) patients (16). TMAs were constructed from the most
representative non-necrotic areas of the formalin-fixed,
paraffin-embedded tissue blocks (19). Immunohistochemical analysis was
performed on the Dako Autostainer (Dako, Carpinteria, CA, USA)
using a Dako LSAB+ kit and diaminobenzidine as the chromogen.
Serial sections of deparaffinized TMA were labeled for RRM1 (goat
polyclonal antibody, 1:100, SC-11731; Santa Cruz Biotechnology,
Inc., Santa Cruz, CA, USA) and ERCC1 (mouse monoclonal antibody,
8F1, 1:200, MS-671; Neomarkers, Inc., Fremont, CA, USA). Microwave
citric acid epitope retrieval was used for the two antibodies.
Appropriate negative (no primary antibody) and positive control
cores (breast cancer tissue for RRM1 and tonsillar tissue for
ERCC1) were included in the construction of the TMA. Each core on
the TMA was assessed for RRM1 and ERCC1 expression by a
genitourinary pathologist who was blinded to the outcomes. An
H-score of 0–300 was calculated for both markers by multiplying the
staining intensity of the tumor cells (0, no staining; 1, weak; 2,
moderate; and 3, strong staining) with the percentage of stained
tumor cells in the TMA core (0–100%). For RRM1, nuclear and/or
cytoplasmic staining was considered, while for ERCC1 only nuclear
staining was considered. The final H-score was the average score
obtained from two 1-mm diameter cores that represented each tumor
sample. For ERCC1, tumors with an H-score higher than the median
were considered to be expressing the marker (13,14).
The receiver operating characteristic (ROC) curve analysis was then
used to determine the cutoff point between tumors with high or low
expression of RRM1, as the former was better correlated with
distant metastasis (DM) and cancer-specific survival (CSS) compared
to the median value or the semi-quantitative H-score.
Treatment outcomes
Complete response (CR) was defined as no evidence of
BC, including carcinoma in situ (CIS) and papillary BC (Ta),
documented by cystoscopy and body imaging following completion of
all therapies. Local recurrence (LR) was defined as histologically
documented reappearance of BC, including CIS and Ta, in the bladder
and/or irradiated volume following documented CR to
chemoradiotherapy. DM was defined as any clinical, radiographic or
histological evidence of metastasis and BC-specific death (BCSD)
was defined as death from BC or from any cause following the
development of DM. Freedom from LR (FFLR), freedom from DM (FFDM)
and CSS were calculated from the initiation of the treatment to the
date of LR, DM or BCSD, respectively.
Statistical analysis
The clinical and treatment characteristics of the
patients were compared by analysis of variance for continuous
variables and the χ2 test for categorical variables. The
Kaplan-Meier method and log-rank test were used for the univariate
analysis. A multivariate analysis (MVA) was performed using the Cox
proportional hazards regression model. All the statistical
analyses, including ROC curve analysis, were performed with MedCalc
v.12 software (MedCalc, Ostend, Belgium). P<0.05 was considered
to indicate a statistically significant difference.
Results
Patient characteristics and clinical
outcome
The clinical characteristics and treatment details
of 39 patients with MIBC treated with chemoradiotherapy are
presented in Table I. All the
tumors were high-grade transitional cell urothelial carcinomas. A
total of 4 patients had T4 tumors and 3 had positive pelvic lymph
nodes (stage IV). The median follow-up was 19 months [interquartile
range (IQR), 11–50 months].
 | Table I.Clinical characteristics and treatment
outcomes of 39 patients with transitional cell carcinoma of the
bladder. |
Table I.
Clinical characteristics and treatment
outcomes of 39 patients with transitional cell carcinoma of the
bladder.
| Characteristics | No. (%) |
|---|
| Median age, years
(IQR) | 72 (67–80) |
| Median follow-up,
months (IQR) | 19 (11–50) |
| Histology | |
| Aberrant
differentiation | 11 (28) |
| Adjacent carcinoma
in situ | 16 (41) |
| Vascular
invasion | 7 (18) |
| Hydronephrosis | 10 (26) |
| Clinical
stagea | |
| II | 21 (54) |
| III | 15 (38) |
| IV (N+) | 3 (8) |
| Median prescribed
dose of radiation, 2-Gy equivalent (IQR) | 60.0 (60.0–64.0) |
| Chemotherapy | |
| Neoadjuvant | 19 (49) |
| Concomitant | 26 (67) |
| Chemotherapy
regimens | |
| Gemcitabine | 22 (56)b |
| Platinum
agents | 20 (51)b |
|
Fluoropyrimidines | 13 (33) |
| Paclitaxel | 12 (31) |
| Response to
therapy | |
| Complete
response | 31 (79) |
| Treated with
gemcitabine (n=22) | 19 (86) |
| Treated with
platinum agent (n=20) | 15 (75) |
| Local
recurrence | 8 (21) |
| Non MP-invasive
carcinoma (Ta, T1) | 3 |
| Carcinoma in
situ (Tis) | 1 |
| MP-invasive
carcinoma (T2-4) | 4 |
| Distant
metastasis | 11 (28) |
| Total deaths | 22 (61) |
| Bladder cancer
deaths | 12 (31) |
The most common neoadjuvant agent was platinum
(cisplatin or carboplatin; n=18) followed by gemcitabine (n=14) and
paclitaxel (n=12), with some patients receiving combination
regimens with 2 (n=6) or 3 (n=10) agents. The most common
neoadjuvant regimen was carboplatin-gemcitabine-paclitaxel (n=8)
(20), followed by
cisplatin-gemcitabine (n=5), carboplatin-paclitaxel (n=3),
cisplatin-etoposide (n=2) and gemcitabine-paclitaxel (n=1). The
most common concomitant agents administered during radiotherapy
were fluoropyrimidines (5-fluorouracil or capecitabine) (n=13)
(21) followed by biweekly
gemcitabine (n=18) (22) and
platinum (n=7) (data not shown).
The rate of CR at the end of the treatment was 79%,
although no patients underwent immediate cystectomy, even with
incomplete response. LR occurred in 8 patients (21%) following CR
at the median time of 9 months (IQR, 7–12 months) after the
completion of radiotherapy. Salvage cystectomy was performed in 2
patients at 11 and 64 months after the completion of
chemoradiotherapy. DM was observed in 28% of patients; among those
with LR, 2 patients with invasive LR (25%) developed DM thereafter.
The crude rate of BCSDs (n=12; 31%) marginally outnumbered DM
(n=11; 28%), since 1 patient succumbed to the complications of a
locally advanced tumor.
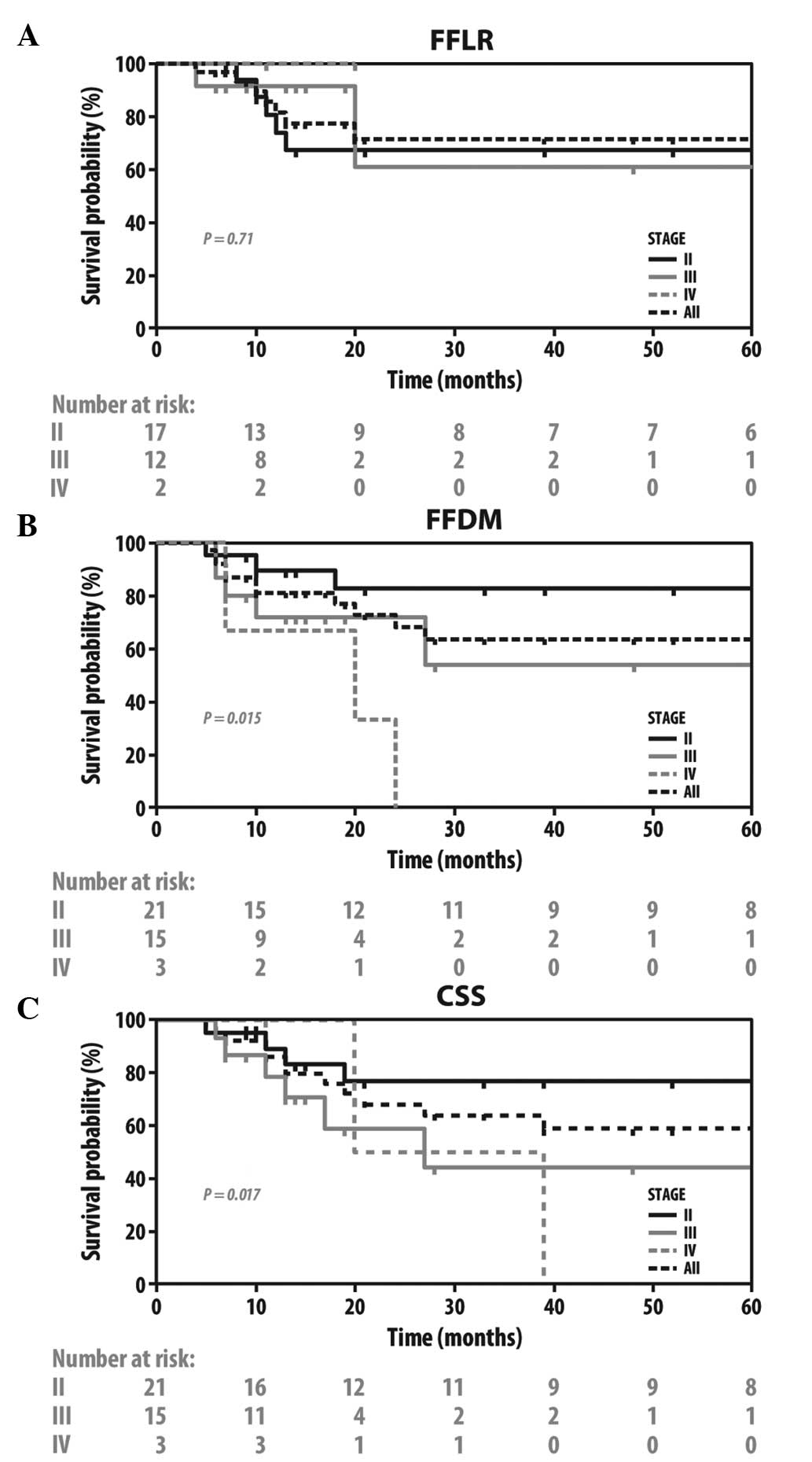
FFLR, FFDM and CSS in all the patients and in those
grouped by tumor stage are illustrated in Fig. 1. There was a significant difference
in FFDM (P=0.015) and CSS (P=0.017) between the various tumor
stages, but not in FFLR (P=0.71). Similarly, there were differences
in FFDM and CSS, but not in FFLR, when the patients were grouped by
the presence or absence of pretreatment hydronephrosis [hazard
ratio (HR)=3.5, 95% confidence interval (CI): 0.52–23.54; P=0.20
for FFLR; HR=5.4, 95% CI: 1.17–25.20; P=0.001 for FFDM; and
HR=5.29, 95% CI: 1.18–23.73; P=0.030 for CSS] or vascular invasion
(VI) (HR=1.17, 95% CI: 0.13–10.79; P=0.88 for FFLR; HR=10.21, 95%
CI: 1.96–53.15; P=0.006 for FFDM; and HR=2.80, 95% CI: 0.58–13.58;
P=0.076 for CSS). There were no such differences when the patients
were grouped by the presence or absence of CIS (HR=0.95, 95% CI:
0.23–3.95; P=0.95 for FFLR; HR=0.30, 95% CI: 0.28–3.23; P=0.94 for
FFDM; and HR=0.86, 95% CI: 0.27–2.78; P=0.80 for CSS) (data not
shown).
Association between RRM1 and ERCC1 status
and clinical outcome
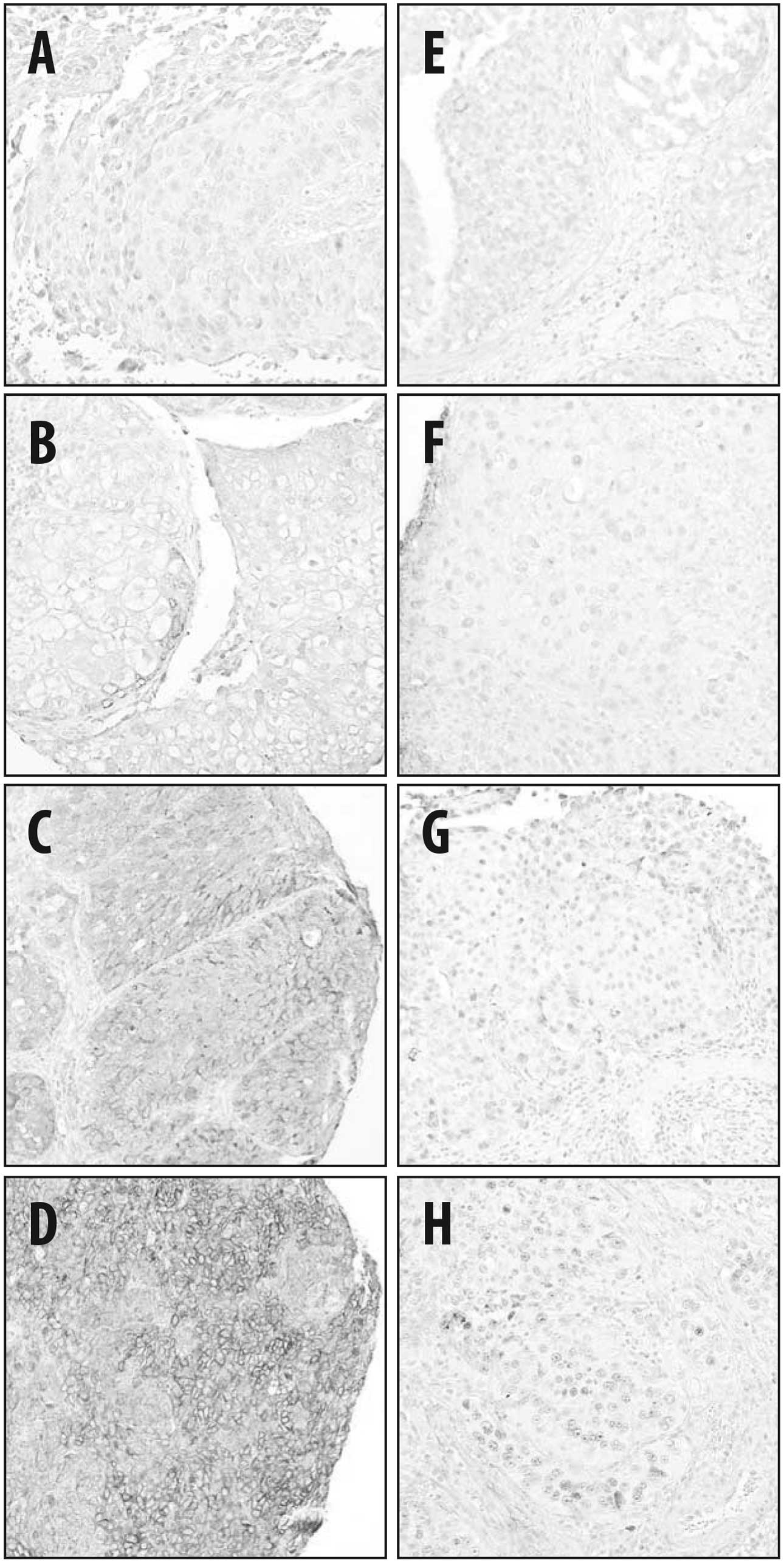
Among the 39 tumor samples available, 36 were
successfully processed for RRM1 and 37 for ERCC1 analysis (Fig. 2). The median H-score was 50 (IQR,
0–100) for the RRM1 and 10 (IQR, 0–60) for the ERCC1 staining. The
cutoff point for high expression of RRM1 at an H-score of >60
was determined by a non-biased ROC curve, with a specificity and
sensitivity of 72.7 and 64.0% for the BCSD, respectively [P=0.038,
area under the curve (AUC)=0.71], and a specificity and sensitivity
of 70.0 and 61.5% for DM, respectively (P=0.12, AUC=0.67). While
the cutoff RRM1 H-score for CR obtained from the ROC curve analysis
was >0 (P=0.0003, AUC=0.78), we selected >60, as it was
associated with clinically meaningful CSS and DM (data not shown)
and it was close to the median value, which was utilized as the
cutoff score in previous studies (10,16).
The ROC curve did not reveal an association between ERCC1
expression and the clinical outcome (P=0.39, AUC=0.60 for CR;
P=0.49, AUC=0.57 for DM; and P=0.84, AUC=0.52 for BC deaths).
Therefore, the median H-score of >10, as previously reported for
BC (13,14), was utilized as a cutoff point.
Based on these criteria of positivity, 16 patients (44%) had tumors
that highly expressed RRM1, 12 (32%) had tumors that highly
expressed ERCC1, 7 (19%) had tumors that highly expressed both
markers and 15 patients (42%) had tumors exhibiting low expression
of RRM1 and ERCC1. There was no correlation between RRM1 and ERCC1
expression (Spearman’s rs=0.198, P=0.25).
When grouped by RRM1 or ERCC1 status, there were no
statistically significant differences between the groups for
clinical and treatment characteristics (Table II), except for a trend to a higher
rate of hydronephrosis (P=0.073) in the group highly expressing
RRM1. However, following treatment, the tumors exhibiting high
expression of RRM1 had a lower rate of CR (56 vs. 95%, P=0.012).
When the patients were grouped by whether they received
gemcitabine-based chemoradiotherapy or not, there was a
statistically significant difference between CR rates only in the
group of patients that received gemcitabine (P=0.036 vs. P=0.29)
(Table II). The CR rate was lower
in patients with tumors that expressed ERCC1; however, the
difference was not statistically significant (67 vs. 84%, P=0.39)
and there was no LR after attaining CR in this group of patients.
When only platinum-treated patients were considered, the rates of
CR following chemoradiotherapy were indistinguishable between
groups based on the ERCC1 status (71 vs. 75%, P=1.0).
 | Table II.Clinical characteristics and
treatment outcomes of patients grouped by RRM1 and ERCC1
status. |
Table II.
Clinical characteristics and
treatment outcomes of patients grouped by RRM1 and ERCC1
status.
|
Characteristics | RRM1 IHC
(n=36) | P-value | ERCC1 IHC
(n=37) | P-value |
|---|
|
|
|---|
| High n=16
(44%) | Low n=20 (56%) | High n=12
(32%) | Low n=25 (68%) |
|---|
| Median age, years
(IQR) | 72 (69–79) | 73 (66–81) | 0.41a | 75 (66–79) | 71 (67–81) | 0.62a |
| Median follow-up,
months (IQR) | 14 (10–35) | 19 (11–52) | 0.26a | 14 (9–24) | 20 (11–52) | 0.22a |
| Histology | | | | | | |
| Aberrant
differentiation | 6 (38) | 5 (25) | 0.48b | 3 (25) | 8 (32) | 1.0b |
| Adjacent
carcinoma in situ | 8 (50) | 8 (40) | 0.74b | 4 (16) | 10 (40) | 1.0b |
| Vascular
invasion | 5 (31) | 2 (10) | 0.20b | 3 (25) | 4 (16) | 0.66b |
| Hydronephrosis | 7 (44) | 3 (15) | 0.073b | 5 (42) | 5 (20) | 0.24b |
| Clinical stage | | | | | | |
| II | 7 (44) | 12 (60) | 0.50b | 4 (33) | 16 (64) | 0.16b |
| III | 7 (44) | 7 (35) | 0.72b | 7 (58) | 7 (28) | 0.44b |
| IV | 2 (13) | 1 (5) | 0.069b | 1 (8) | 2 (7) | 0.37b |
| Chemotherapy | | | | | | |
| Neoadjuvant | 10 (63) | 8 (40) | 0.32b | 7 (58) | 11 (44) | 0.50b |
| Concomitant | 10 (63) | 14 (70) | 0.73b | 6 (50) | 19 (76) | 0.15b |
| Chemotherapy
regimens | | | | | | |
| Gemcitabine | 7 (44) | 12 (60) | 0.50b | 7 (58) | 13 (52) | 1.0b |
| Platinum
agents | 10 (63) | 9 (45) | 0.34b | 7 (58) | 12 (48) | 0.73b |
|
Fluoropyrimidines | 7 (44) | 6 (30) | 0.49b | 5 (42) | 8 (32) | 0.72b |
| Paclitaxel | 6 (38) | 5 (25) | 0.48b | 6 (50) | 5 (20) | 0.12b |
| Complete
response | 9 (56) | 19 (95) | 0.012b | 8 (67) | 21 (84) | 0.39b |
| Local
recurrence | 2 (13) | 5 (25) | 1.0b | 0 | 7 (28) | 0.142b |
| Distant
metastasis | 8 (50) | 3 (15) | 0.12b | 2 (17) | 8 (32) | 0.56b |
| Total deaths | 14 (88) | 8 (40) | 0.078b | 6 (50) | 14 (56) | 0.99b |
| Bladder cancer
deaths | 9 (56) | 3 (15) | 0.057b | 3 (25) | 8 (32) | 0.96b |
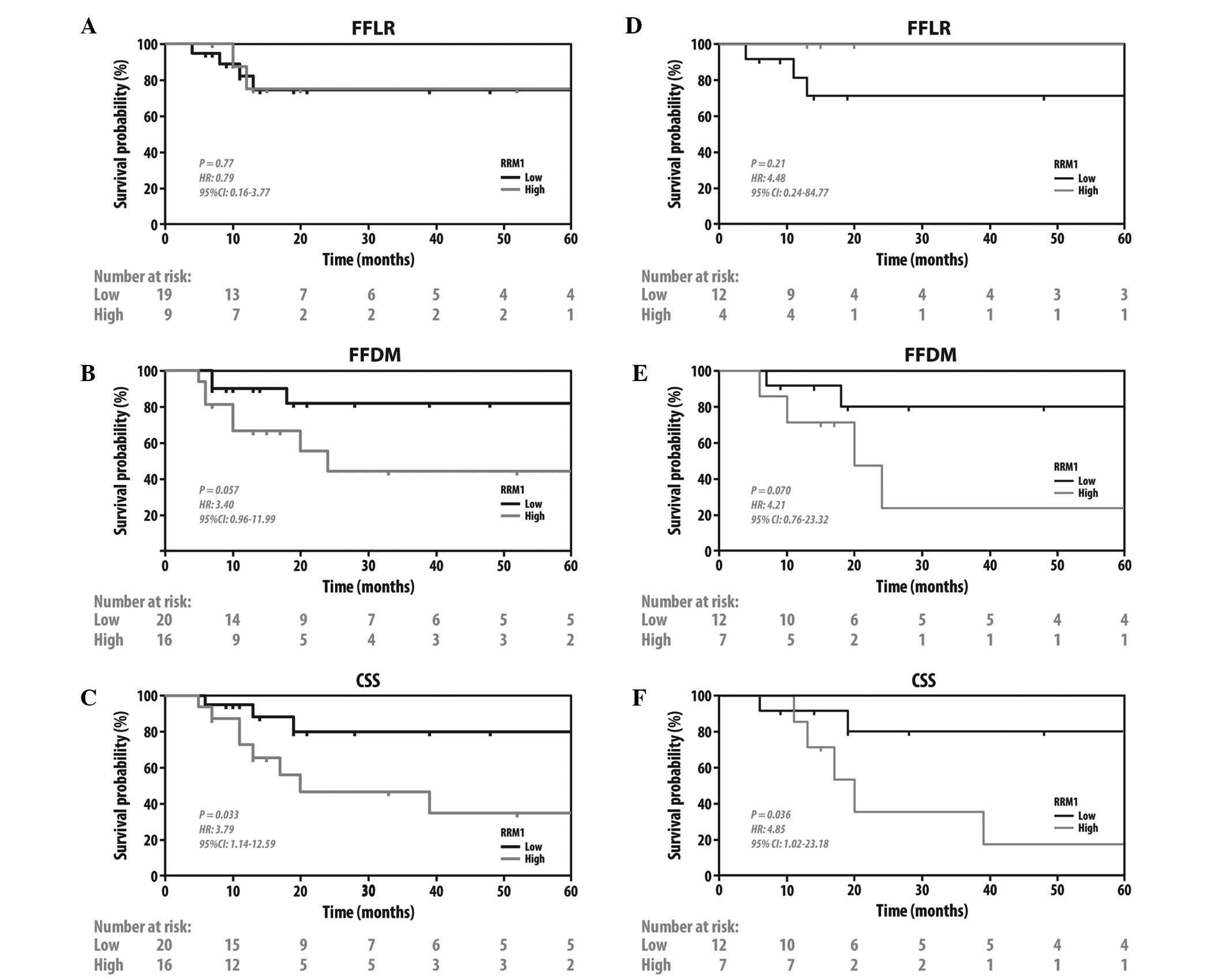
Since CR to chemoradiation was shown to be
prognostic for later clinical endpoints (23), the effects of RRM1 and ERCC1
expression on other clinically significant endpoints were
investigated. The patients with tumors with a low expression of
RRM1 exhibited better CSS (HR=3.79, 95% CI: 1.14–12.59; P=0.033)
and a trend to FFDM (HR=3.4, 95% CI: 0.96–11.99; P=0.057), but no
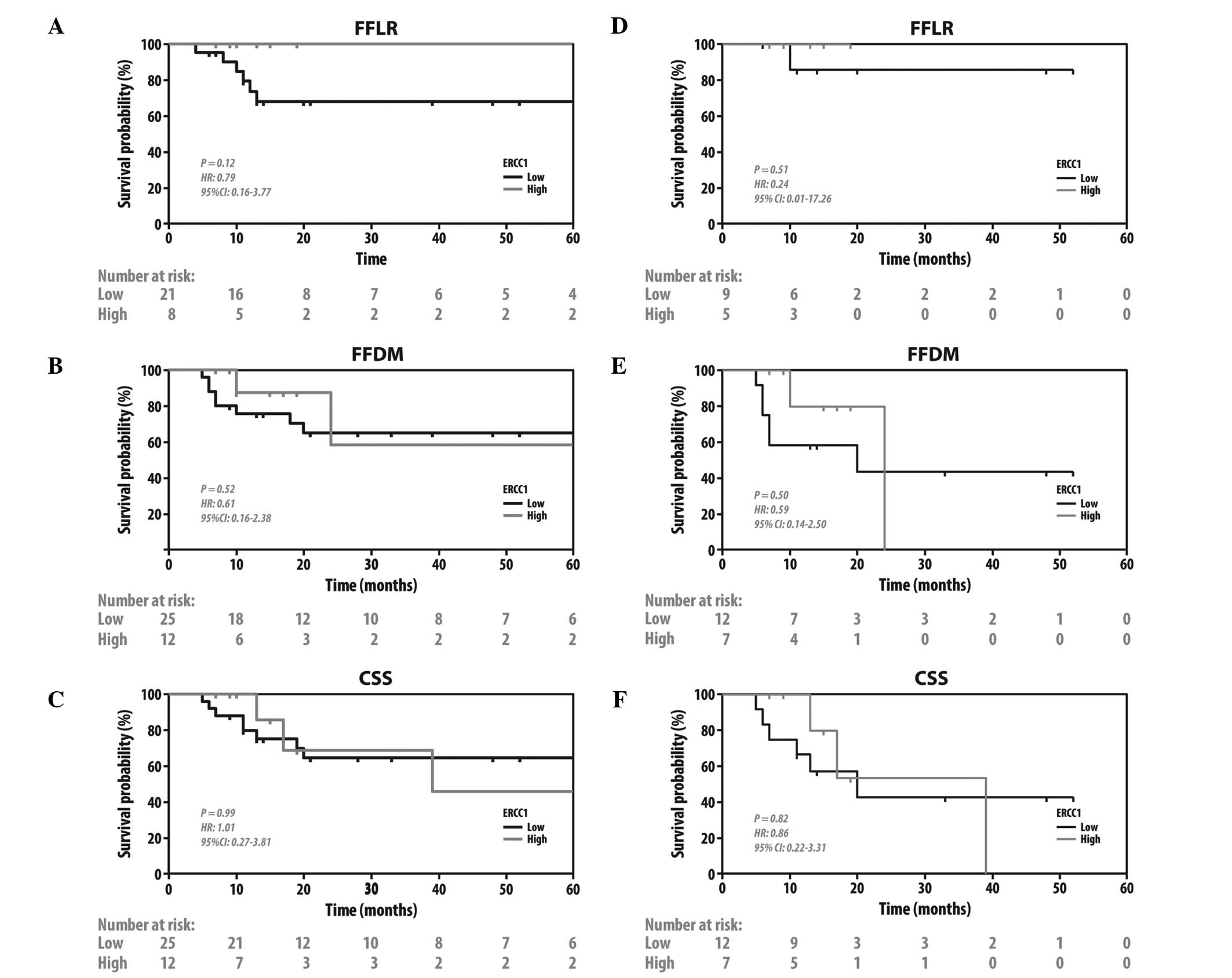
difference in FFLR (HR=0.79, 95% CI: 0.16–3.77; P=0.77) (Fig. 3A–C). There were no such differences
when the patients were grouped by ERCC1 status. (Fig. 4A–C). To further investigate the
prognostic significance of RRM1 and ERCC1, we evaluated FFDM and
CSS when only patients treated with gemcitabine-based chemotherapy
were grouped by RRM1 status (Fig.
3D–F) and patients treated with platinum-based chemotherapy
were grouped by ERCC1 status (Fig.
4D–F). Consistent with the previous findings of the present
study, patients with tumors with a low expression of RRM1 exhibited
a better CSS (HR=4.85, 95%CI: 1.02–23.18; P=0.036) and a trend to
FFDM (HR=4.21, 95% CI: 0.76–23.32; P=0.070) on receiving
gemcitabine-based therapy. No such difference was observed in
patients with tumors with a high expression of RRM1 who did not
receive gemcitabine (HR=3.01, 95% CI: 0.42–21.4; P=0.32 for FFDM;
and HR=2.91, 95% CI: 0.41–20.7; P=0.33 for CSS, data not shown).
Unlike RRM1, the ERCC1 status did not predict whether the patients
had a survival benefit from platinum- or non-platinum-based
regimens.
As the patients with tumors exhibiting high
expression of RRM1 also had higher, albeit non-significantly, rates
of advanced tumor stage and other known adverse prognostic factors,
we evaluated the prognostic value of RRM1 in MVA, which considered
tumor stage (II vs. III–IV), hydronephrosis and VI. Although the
negative effect of RRM1 was greatest as measured by the HR when
including these 4 variables, none of the variables retained
statistical significance (Table
III).
 | Table III.Multivariate analysis. |
Table III.
Multivariate analysis.
| Variables | Bladder
cancer-specific mortality | Distant
metastasis |
|---|
|
|
|---|
| HR | P-value | 95% CI | HR | P-value | 95% CI |
|---|
| Tumor stage | | | | | | |
| II | | Reference | | | Reference | |
| III-IV | 1.5 | 0.63 | 0.31–7.0 | 1.1 | 0.90 | 0.18–6.9 |
| Vascular
invasion | | | | | | |
| No | | Reference | | | Reference | |
| Yes | 1.2 | 0.89 | 0.27–4.8 | 2.3 | 0.29 | 0.50–10.2 |
| Hydronephrosis | | | | | | |
| No | | Reference | | | Reference | |
| Yes | 1.9 | 0.40 | 0.43–8.4 | 3.7 | 0.12 | 0.72–18.7 |
| RRM1
expression | | | | | | |
| Low | | Reference | | | Reference | |
| High | 3.0 | 0.15 | 0.69–12.8 | 1.7 | 0.52 | 0.35–7.8 |
Discussion
BC is a radiosensitive and chemosensitive tumor with
65% response and 42% CR rates following irradiation with 50 Gy
(24). Cisplatin-based regimens,
which achieve 40–65% response and 10–20% CR rates in metastatic
disease (8), were also shown to
improve survival in patients with localized BC when administered
prior to cystectomy or radiation (7). Bladder preservation protocols
combining TURBT, radiotherapy and chemotherapy achieve CR rates of
>70% and result in survival rates comparable to those of radical
surgery (2,4,23).
Achieving a CR is a strong prognostic factor for a favorable
clinical outcome and, in the majority of organ-preserving
protocols, patients who do not achieve a CR undergo a cystectomy
shortly after completing chemoradiotherapy (4). Therefore, a CR following
chemoradiotherapy may act as an effective biomarker for the
selection of patients for organ preservation treatment, which was
previously reported following induction chemotherapy in laryngeal
cancer (25), where
organ-preserving therapy has become the standard of care. However,
patients with BC typically undergo chemoradiotherapy before their
pathological response is identified. As a result, a molecular
marker, which may help identify patients who are more likely to
achieve a CR or guide the selection of chemotherapy regimens, would
be of significant value.
In the present study, the predictive and prognostic
value of RRM1 and ERCC1 expression was investigated in a group of
patients with MIBC treated with platinum- or gemcitabine-based
chemoradiotherapy. Our findings demonstrated that low RRM1
expression, which was observed in approximately half of the tumors,
was prognostic for CR in patients treated with gemcitabine, but did
not affect response in those not receiving gemcitabine. While high
RRM1 expression status was also found to be correlated with worse
CSS and a trend to worse DM on the univariate analysis, its
predictive value was diminished when other adverse
clinicopathological characteristics were considered. Nevertheless,
the association of CR, DM and CSS with RRM1 expression in patients
receiving gemcitabine was consistent with that reported by previous
studies investigating other malignancies treated with gemcitabine
(9).
RRM1 is the main mechanistic target of gemcitabine
and its overexpression is associated with resistance to this drug
in vitro and in vivo. In addition to being a key
enzyme in the de novo synthesis of nucleotides, RRM1 is also
involved in the control of cell proliferation, migration and
metastasis (9). The prognostic and
predictive properties of RRM1 have been extensively investigated in
localized and metastatic NSCLC, where the response rates to
gemcitabine-based chemotherapy and survival were found to be
inversely correlated with RRM1 expression (26). RRM1 expression was also found to be
directly correlated with overall survival (OS) in 43 young patients
with BC who underwent cystectomy, in a study that did not record
data on LR, DM and the use of chemotherapy and radiotherapy
(10). In another study, involving
57 patients with advanced BC treated with gemcitabine-based
polychemotherapy, RRM1 expression was not found to be correlated
with OS and response (P=0.062), but was correlated with
time-to-disease progression (P=0.045) (27).
Unlike RRM1, ERCC1 expression was not found to be
predictive for the response to platinum-based chemoradiotherapy or
prognostic for the benefits from such treatment. There are several
available clinical and preclinical studies on the association of
ERCC1 expression with resistance to platinum agents (11,12,17,27–29)
and radiosensitivity (15,18,30).
The ERCC1 gene has 10 exons and generates 4 isoforms by alternative
splicing; however, only 1 of these 4 isoforms is actively involved
in the repair of platinum-DNA adducts. These isoforms were found to
be heterogeneously expressed in NSCLC (31). However, none of the 16 commercially
available anti-ERCC1 antibodies was able to accurately discriminate
between the isoforms (31),
limiting the usefulness of ERCC1 detection by immunohistochemistry.
Moreover, due to the sequence homologies between the isoforms, it
is impossible to develop isoform-specific primers for PCR detection
of mRNA (31).
Despite the small sample size, which reflects the
majority of medically operable patients with MIBC being offered
radical surgery (2,32), the present study is one of the very
few focused on chemosensitivity markers in BC treated with
chemoradiotherapy. Kawashima et al (15) previously evaluated ERCC1 expression
in a small and heterogeneous group of 22 patients treated with
radiation and platinum agents. To the best of our knowledge, our
study is the first to evaluate RRM1 expression in patients
undergoing chemoradiotherapy. The limitations of this study lie
with its retrospective nature, which did not allow for the control
of the clinical characteristics of the patients in the different
treatment groups or the heterogeneity of treatment regimens, which
reflects the lack of consensus on the most effective treatment for
this disease.
In conclusion, our study demonstrated that the
expression of RRM1, but not ERCC1, may predict response to
gemcitabine-based chemoradiotherapy. As a result, low expression of
RRM1 may help identify patients appropriately treated with
gemcitabine-based trimodality therapy. Further evaluation of RRM1
as a predictive and prognostic biomarker in larger trials is
required, such as the RTOG 0712 trial (33), which randomized patients between
gemcitabine- and platinum-based regimens concurrent with radiation.
The validation of RRM1 may offer a unique molecular means to select
treatment regimens for patients with MIBC treated with combined
chemotherapy and radiation.
References
|
1.
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012. View Article : Google Scholar
|
|
2.
|
Milosevic M, Gospodarowicz M, Zietman A,
et al: Radiotherapy for bladder cancer. Urology. 69(Suppl 1):
80–92. 2007. View Article : Google Scholar
|
|
3.
|
Efstathiou JA, Bae K, Shipley WU, et al:
Late pelvic toxicity after bladder-sparing therapy in patients with
invasive bladder cancer: RTOG 89-03, 95-06, 97-06, 99-06. J Clin
Oncol. 27:4055–4061. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Efstathiou JA, Spiegel DY, Shipley WU, et
al: Long-term outcomes of selective bladder preservation by
combined-modality therapy for invasive bladder cancer: the MGH
experience. Eur Urol. 61:705–711. 2012. View Article : Google Scholar
|
|
5.
|
Coppin CM, Gospodarowicz MK, James K, et
al: Improved local control of invasive bladder cancer by concurrent
cisplatin and preoperative or definitive radiation. The National
Cancer Institute of Canada Clinical Trials Group. J Clin Oncol.
14:2901–2907. 1996.
|
|
6.
|
James ND, Hussain SA, Hall E, et al:
Radiotherapy with or without chemotherapy in muscle-invasive
bladder cancer. N Engl J Med. 366:1477–1488. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
International Collaboration of Trialists;
Medical Research Council Advanced Bladder Cancer Working Party;
European Organisation for Research and Treatment of Cancer
Genito-Urinary Tract Cancer Group; et al: International phase III
trial assessing neoadjuvant cisplatin, methotrexate, and
vinblastine chemotherapy for muscle-invasive bladder cancer:
long-term results of the BA06 30894 trial. J Clin Oncol.
29:2171–2177. 2011. View Article : Google Scholar
|
|
8.
|
Sternberg CN, Donat SM, Bellmunt J, et al:
Chemotherapy for bladder cancer: treatment guidelines for
neoadjuvant chemo-therapy, bladder preservation, adjuvant
chemotherapy, and metastatic cancer. Urology. 69(Suppl 1): 62–79.
2007. View Article : Google Scholar
|
|
9.
|
Jordheim LP, Seve P, Tredan O and Dumontet
C: The ribo-nucleotide reductase large subunit (RRM1) as a
predictive factor in patients with cancer. Lancet Oncol.
12:693–702. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Harshman LC, Bepler G, Zheng Z, Higgins
JP, Allen GI and Srinivas S: Ribonucleotide reductase subunit M1
expression in resectable, muscle-invasive urothelial cancer
correlates with survival in younger patients. BJU Int.
106:1805–1811. 2010. View Article : Google Scholar
|
|
11.
|
Zheng Z, Chen T, Li X, Haura E, Sharma A
and Bepler G: DNA synthesis and repair genes RRM1 and ERCC1 in lung
cancer. N Engl J Med. 356:800–808. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Gossage L and Madhusudan S: Current status
of excision repair cross complementing-group 1 (ERCC1) in cancer.
Cancer Treat Rev. 33:565–577. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Kim KH, Do IG, Kim HS, et al: Excision
repair cross-complementation group 1 (ERCC1) expression in advanced
urothelial carcinoma patients receiving cisplatin-based
chemotherapy. APMIS. 118:941–948. 2010. View Article : Google Scholar
|
|
14.
|
Sun JM, Sung JY, Park SH, et al: ERCC1 as
a biomarker for bladder cancer patients likely to benefit from
adjuvant chemotherapy. BMC Cancer. 12:1872012. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Kawashima A, Nakayama M, Kakuta Y, et al:
Excision repair cross-complementing group 1 may predict the
efficacy of chemoradiation therapy for muscle-invasive bladder
cancer. Clin Cancer Res. 17:2561–2569. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Vilmar A, Garcia-Foncillas J, Huarriz M,
Santoni-Rugiu E and Sorensen JB: RT-PCR versus immunohistochemistry
for correlation and quantification of ERCC1, BRCA1, TUBB3 and RRM1
in NSCLC. Lung Cancer. 75:306–312. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Ozcan MF, Dizdar O, Dincer N, et al: Low
ERCC1 expression is associated with prolonged survival in patients
with bladder cancer receiving platinum-based neoadjuvant
chemotherapy. Urol Oncol. 31:1709–1715. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18.
|
Ahmad A, Robinson AR, Duensing A, et al:
ERCC1-XPF endonuclease facilitates DNA double-strand break repair.
Mol Cell Biol. 28:5082–5092. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Nocito A, Kononen J, Kallioniemi OP and
Sauter G: Tissue microarrays (TMAs) for high-throughput molecular
pathology research. Int J Cancer. 94:1–5. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Smith DC, Mackler NJ, Dunn RL, et al:
Phase II trial of paclitaxel, carboplatin and gemcitabine in
patients with locally advanced carcinoma of the bladder. J Urol.
180:2384–2388. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Higano CS, Tangen CM, Sakr WA, et al
Southwest Oncology Group Trial 8733: Treatment options for
muscle-invasive urothelial cancer for patients who were not
eligible for cystectomy or neoadjuvant chemotherapy with
methotrexate, vinblastine, doxorubicin, and cisplatin: report of
Southwest Oncology Group Trial 8733. Cancer. 112:2181–2187. 2008.
View Article : Google Scholar
|
|
22.
|
Kent E, Sandler H, Montie J, et al:
Combined-modality therapy with gemcitabine and radiotherapy as a
bladder preservation strategy: results of a phase I trial. J Clin
Oncol. 22:2540–2545. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Shipley WU, Zietman AL, Kaufman DS, Coen
JJ and Sandler HM: Selective bladder preservation by trimodality
therapy for patients with muscularis propria-invasive bladder
cancer and who are cystectomy candidates - the Massachusetts
General Hospital and Radiation Therapy Oncology Group experiences.
Semin Radiat Oncol. 15:36–41. 2005. View Article : Google Scholar
|
|
24.
|
Pollack A, Zagars GK, Dinney CP, et al:
Preoperative radiotherapy for muscle-invasive bladder carcinoma.
Long term follow-up and prognostic factors for 338 patients.
Cancer. 74:2819–2827. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
25.
|
No authors listed. Induction chemotherapy
plus radiation compared with surgery plus radiation in patients
with advanced laryngeal cancer. The Department of Veterans Affairs
Laryngeal Cancer Study Group. N Engl J Med. 324:1685–1690. 1991.
View Article : Google Scholar
|
|
26.
|
Ceppi P, Volante M, Novello S, et al:
ERCC1 and RRM1 gene expressions but not EGFR are predictive of
shorter survival in advanced non-small-cell lung cancer treated
with cisplatin and gemcitabine. Ann Oncol. 17:1818–1825. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Bellmunt J, Paz-Ares L, Cuello M, et al:
Gene expression of ERCC1 as a novel prognostic marker in advanced
bladder cancer patients receiving cisplatin-based chemotherapy. Ann
Oncol. 18:522–528. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Kawashima A, Takayama H and Tsujimura A: A
review of ERCC1 gene in bladder cancer: implications for
carcinogenesis and resistance to chemoradiotherapy. Adv Urol.
2012:8123982012. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Simon GR, Schell MJ, Begum M, et al:
Preliminary indication of survival benefit from ERCC1 and
RRM1-tailored chemo-therapy in patients with advanced nonsmall cell
lung cancer: evidence from an individual patient analysis. Cancer.
118:2525–2531. 2012. View Article : Google Scholar
|
|
30.
|
Liu ZG, Chen HY, Cheng JJ, Chen ZP, Li XN
and Xia YF: Relationship between methylation status of ERCC1
promoter and radiosensitivity in glioma cell lines. Cell Biol Int.
33:1111–1117. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31.
|
Friboulet L, Olaussen KA, Pignon JP, et
al: ERCC1 isoform expression and DNA repair in non-small-cell lung
cancer. N Engl J Med. 368:1101–1110. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Fedeli U, Fedewa SA and Ward EM: Treatment
of muscle invasive bladder cancer: evidence from the National
Cancer Database, 2003 to 2007. J Urol. 185:72–78. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
RTOG 0712 Protocol Information. February
28–2012.http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0712.
Accessed December 17, 2013.
|