Introduction
Late intraperitoneal hemorrhage is a potentially
life-threatening complication following laparoscopic surgery and
requires timely and precise identification of its source for
definitive treatment. Endovascular treatment has recently gained
wide acceptance due to its minimal invasiveness compared to surgery
(1). In this study, we present a
rare case of two episodes of intraperitoneal hemorrhage from the
gastroduodenal artery stump and the right gastric artery stump,
respectively. Endovascular treatment was performed twice to achieve
hemostasis. The patient recovered well after the second
interventional procedure with coil embolization of the hepatic
artery proper. The interventional procedure of angiography and coil
embolization was reviewed and discussed.
Case report
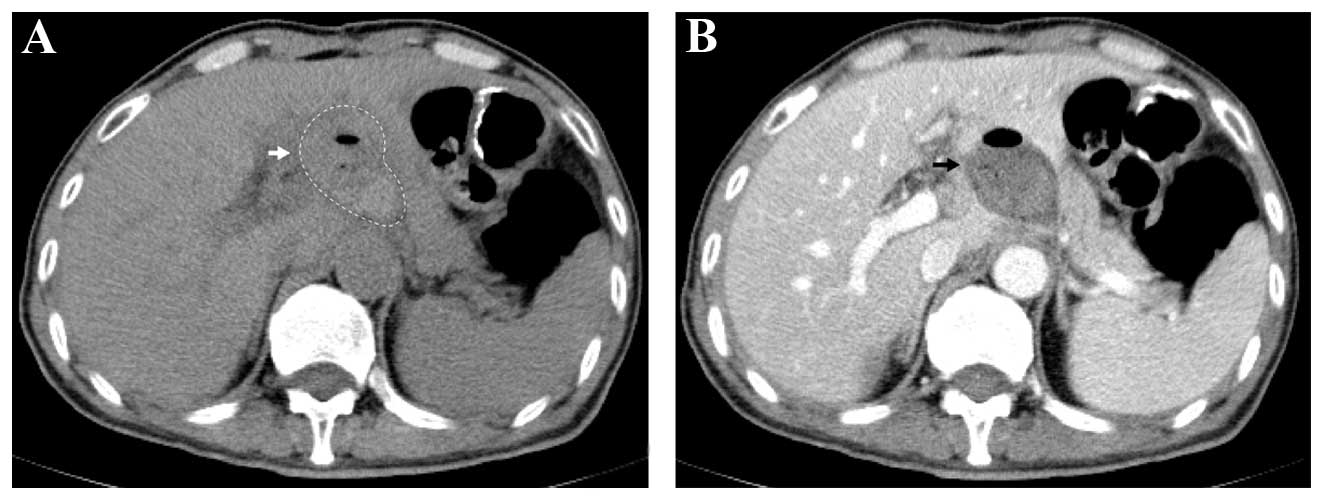
A 56-year-old male patient underwent laparoscopic
gastrectomy for gastric cancer. The postoperative period was
uneventful until sudden onset of epigastric pain 45 days after the
surgery. Following readmission, emergency computed tomography (CT)
detected a hemoperitoneum (Fig.
1). The patient underwent urgent exploratory laparotomy. The
abdominal exploration revealed moderate hemoperitoneum (300 ml) but
the culprit vessel was not identified. An indwelling catheter was
placed into the abdominal cavity. The hematocrit of the patient
continued to decrease according to the hemogram and hemorrhagic
fluid was persistently drained from the catheter after laparotomy.
Therefore, the patient was referred to our department for
interventional treatment. Angiography and embolization was
performed after obtaining written informed consent from the patient
and his family.
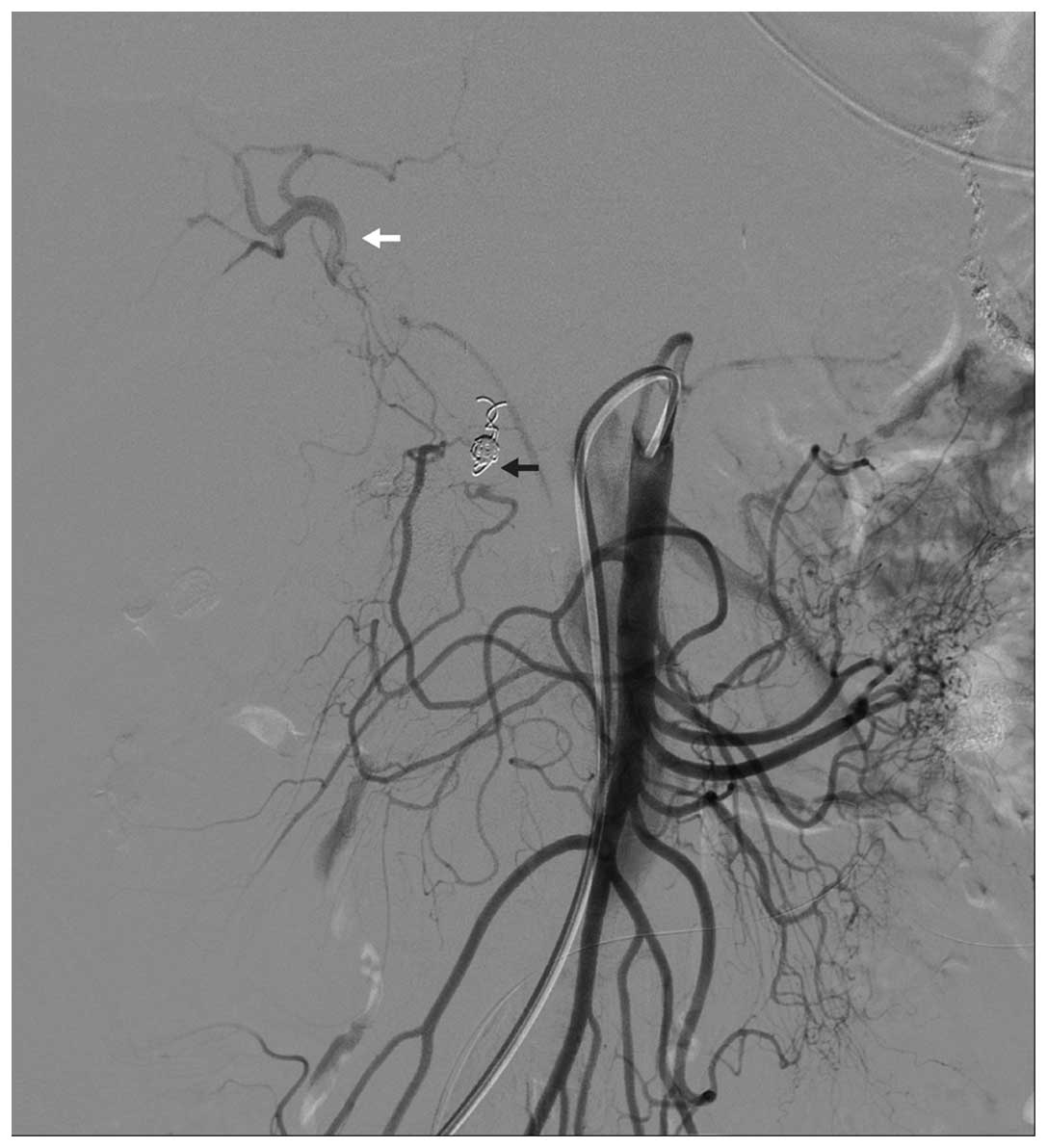
Via the right femoral arterial approach, a 5-F
catheter (Yashiro; Terumo, Tokyo, Japan) was placed through a 5-F
sheath and positioned in the celiac artery. The celiac arteriogram
confirmed aneurysmal dilatation of the gastroduodenal artery stump
(Fig. 2). There was no obvious
active extravasation from the gastroduodenal artery stump; however,
there was a distinct decrease in the hemoglobin concentration of
≥30 g/l. Therefore, we decided to perform the embolization. A
coaxial technique was used to insert a 2.9-F microcatheter
(Progreat™; Terumo) into the sac and microcoils (Tornado
Embolization Microcoil™; Cook, Bloomington, IN, USA) were deployed
to fill the sac and the gastroduodenal artery stump. A celiac
artery angiogram after the embolization confirmed the successful
occlusion of the lesion and the patency of the hepatic artery
proper (Fig. 3). The right hepatic
artery was visualized through selective superior mesenteric
arteriography and superselective angiogram due to collateral flow
via the pancreaticoduodenal arcade without filling of the sac
(Fig. 4).
The bleeding ceased, with no hemorrhagic fluid in
the indwelling catheter, and the patient recovered well after the
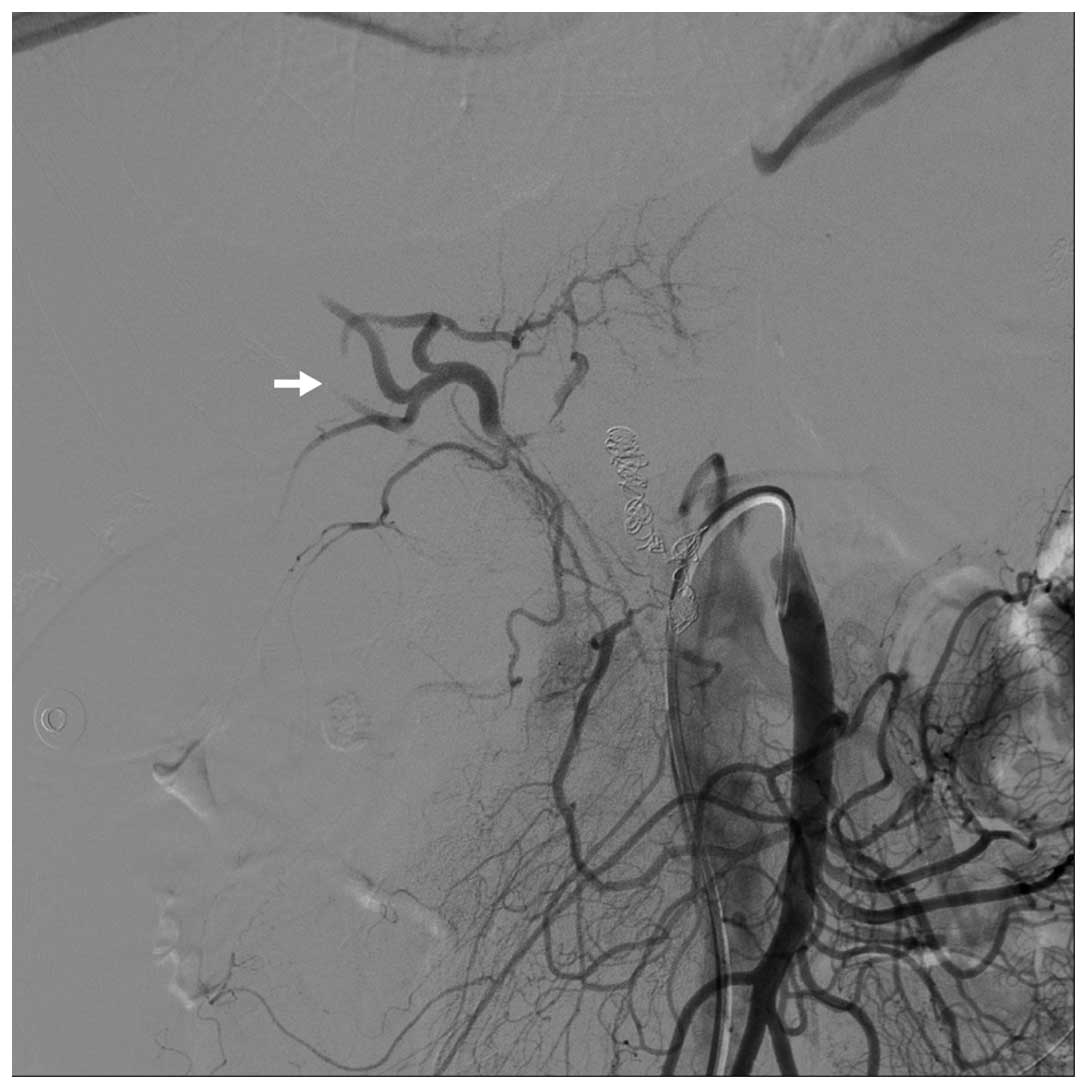
embolization. However, a second episode of intraperitoneal
hemorrhage occurred 7 days after the first interventional
procedure. This time the patient was hemodynamically unstable, with
>400 ml blood drained from the indwelling catheter. Urgent
endovascular management was attempted again to locate and control
the bleeding. The celiac arteriogram confirmed a well-embolized
gastroduodenal artery stump and active extravasation from the right
gastric artery stump (Fig. 5).
However, the right gastric artery stump was too short to be
embolized through catheterization. Following a discussion on the
therapeutic options between the surgeons and interventional
radiologists, relaparotomy was considered, although it would not be
possible to control the bleeding without ligating the hepatic
artery proper; furthermore, there was a minimal possibility of
liver ischemia due to the collateral circulation from the superior
mesenteric artery. Therefore, embolization of the hepatic artery
proper distal as well as proximal to the right gastric artery stump
was performed with microcoils. The completion celiac angiography
confirmed immediate hemostasis and occlusion of the hepatic artery
proper. Filling of the right hepatic artery via the collateral
pathway of superior mesenteric artery was demonstrated by
post-embolization angiography (Fig.
6).
The patient quickly regained hemodynamic stability
after the second endovascular procedure. There was a transient mild
elevation in the serum transaminases, but the enzyme levels
returned to normal within 10 days, with no evidence of severe liver
insufficiency or ischemia. A contrast-enhanced CT obtained 3 days
after the second embolization confirmed good perfusion of the liver
(Fig. 7). The hemoglobin level was
stable (88–96 g/l) following the second embolization procedure and
there was little hemorrhagic fluid drained from the intraperitoneal
indwelling catheter. The patient was discharged 20 days after the
second interventional procedure.
Discussion
Laparoscopic gastrectomy is an alternative operative
treatment modality that is widely accepted due to its minimal
invasiveness compared to open gastrectomy (2–4).
Postoperative bleeding is one of the most common operation-related
severe complications mentioned in the literature (2,5).
Immediate and accurate diagnosis is essential in order to prevent a
massive and life-threatening delayed hemorrhage. The traditional
approach to late hemorrhage following abdominal surgery is
reoperation; however, the mortality rates associated with
reintervention are high (6).
Furthermore, it is difficult to determine the precise source of the
bleeding, due to the surrounding large amount of clotted blood.
Definitive treatment may be more difficult in certain cases, even
when the precise bleeding site has been located. Endovascular
procedures provide a safe and effective method for diagnostic and
therapeutic purposes and are widely used in similar situations,
such as hemorrhage following pancreaticoduodenectomy (1). In fact, late intraperitoneal
hemorrhage occurred more frequently following
pancreaticoduodenectomy and endovascular procedures have been
proven to be effective (1).
Delayed hemorrhage has been defined differently in
the literature, ranging between 1 and 5 or more postoperative days
(6,7). The duration of 45 days between the
laparoscopic gastrectomy and the onset of hemorrhage is relatively
long. The titanium clamp was displaced postoperatively and was
considered to be the cause of the delayed hemorrhage from the right
gastric artery. Approximately 80% of the right gastric artery
originates from the proximal branches of the hepatic trunk
(8). The anatomical
characteristics necessitate the occlusion of the hepatic trunk when
selective embolization of the right gastric artery is not feasible.
Moreover, the right gastric artery stump was too short for further
ligation or coil embolization in this case, which made it
impossible to maintain hepatic blood flow while controlling the
bleeding by laparoscopy or open surgery.
CT angiography (CTA) is widely applied; however, we
recommend angiography as the first-line modality for
intraperitoneal hemorrhage following surgery. Selective visceral
angiography is accurate in detecting the source of hemorrhage that
would otherwise be undetectable with exploratory laparotomy. The
greatest advantage of selective visceral angiography over CTA is
that endovascular treatment may be performed in the same
setting.
Liver failure following common hepatic artery
embolization was feared, as fatal liver failure was previously
reported following embolization of the common hepatic artery
(7). However, similar situations
were reported to be safe in the currently available literature
(1,9). The risk of liver failure is
relatively low due to the dual blood supply from the portal and the
arterial circulation (6).
Collateral vessels are also important in maintaining liver
perfusion, as in this case.
It was previously reported that stent grafts allow
for excluding hemorrhagic lesions without compromising blood flow
to the liver (6,10). The use of a stent graft was
proposed to avoid the potentially severe complications of arterial
occlusion (6). However,
anticoagulation should be administered to prevent thrombus
formation following stenting, which was considered unacceptable by
the surgeons for fear of recurrence of bleeding from other lesions
in this case.
In conclusion, we recommend angiography as a
first-line modality for late intraperitoneal hemorrhage following
laparoscopic gastrectomy and transcatheter coil embolization of the
hepatic artery proper is safe and effective in selected cases.
References
|
1
|
Yamashita Y, Taketomi A, Fukuzawa K, et
al: Risk factors and management of delayed intraperitoneal
hemorrhage after pancreatic and biliary surgery. Am J Surg.
193:454–459. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kodera Y, Fujiwara M, Ohashi N, et al:
Laparoscopic surgery for gastric cancer: a collective review with
meta-analysis of randomized trial. J Am Coll Surg. 211:677–686.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee SW, Nomura E, Bouras G, et al:
Long-term oncologic outcomes from laparoscopic gastrectomy for
gastric cancer: a single-center experience of 601 consecutive
resections. J Am Coll Surg. 211:33–40. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ohtani H, Tamamori Y, Noguchi K, et al:
Meta-analysis of laparoscopy-assisted and open distal gastrectomy
for gastric cancer. J Surg Res. 171:479–485. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bo T, Zhihong P, Peiwu Y, et al: General
complications following laparoscopic-assisted gastrectomy and
analysis of techniques to manage them. Surg Endosc. 23:1860–1865.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Boufi M, Hashemi AA, Azghari A, et al:
Endovascular management of severe bleeding after major abdominal
surgery. Ann Vasc Surg. 27:1098–1104. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Choi SH, Moon HJ, Heo JS, et al: Delayed
hemorrhage after pancreaticoduodenectomy. J Am Coll Surg.
199:186–191. 2004. View Article : Google Scholar
|
|
8
|
Lee SW, Shinohara H, Matsuki M, et al:
Preoperative simulation of vascular anatomy by three-dimensional
computed tomography imaging in laparoscopic gastric cancer surgery.
J Am Coll Surg. 197:927–936. 2003. View Article : Google Scholar
|
|
9
|
Hur S, Yoon CJ, Kang S-G, et al:
Transcatheter arterial embolization of gastroduodenal artery stump
pseudoaneurysms after pancreaticoduodenectomy: safety and efficacy
of two embolization techniques. J Vasc Interv Radiol. 22:294–301.
2011. View Article : Google Scholar
|
|
10
|
Pasklinsky G, Gasparis A, Labropoulos N,
et al: Endovascular covered stenting for visceral artery
pseudoaneurysm rupture: report of 2 cases and a summary of the
disease process and treatment options. Vasc Endovascular Surg.
42:601–606. 2008. View Article : Google Scholar
|