Introduction
Follicular cholangitis is difficult to diagnose, as
it is particularly challenging to distinguish from primary
sclerosing cholangitis, immunoglobulin G4 (IgG4)-related sclerosing
cholangitis and hilar cholangiocarcinoma (1–4).
Follicular cholangitis is relatively rare; it was first reported by
Aoki et al (5) in 2003, and
only a few cases have been reported to date (5–9). Imaging
findings representative of this disease include biliary stricture
associated with dilatation of the peripheral bile duct and lymph
node enlargement. Certain patients have undergone surgical
treatment for preoperative diagnosis of cholangiocarcinoma, which
was finally diagnosed as a benign condition (10).
It was previously demonstrated that the majority of
the cases are diagnosed as cholangiocarcinoma due to the severe
biliary stricture and the presence of symptoms, which commonly
include abdominal pain and jaundice. Follicular cholangitis has
recently been reported to be among several diseases that cause
biliary stricture. The reported pathological findings of this
disease are fibrotic thickening of the wall of the hilar bile duct;
prominent hyperplastic lymph follicles with germinal centers in the
subserosal layer, without tumorous growth, which were considered to
be reactive hyperplastic follicles, with localization of the
lesions in the proximal extrahepatic bile duct and hepatic hilum,
and with almost intact peripheral intrahepatic bile ducts (8).
We herein report the case of a 69-year-old woman
with follicular cholangitis associated with a focal biliary
stricture, who underwent left hepatectomy after 8 years of
follow-up.
Case report
A 69-year-old woman was referred to our hospital due
to repeated hepatolithiasis and cholangitis of the left hepatic
lobe over an 8-year follow-up period. The patient was 148 cm in
height and weighed 36.5 kg, had undergone abdominal surgery,
including hysterectomy for myoma and a laparoscopic cholecystectomy
7 years earlier, and had no history of autoimmune disease. The
laboratory data revealed no elevation in the levels of
hepatobiliary enzymes or tumor markers, such as carcinoembryonic
antigen and carbohydrate antigen 19-9. Internal drainage to the B3
using endoscopic retrograde biliary drainage had been performed
annually for cholangitis. Endoscopic treatment for cholangitis had
also been repeatedly performed due to obstruction of the tube. On
abdominal ultrasonography, there was dilatation of the left
intrahepatic duct to a width of ≤2 cm, and stones with an acoustic
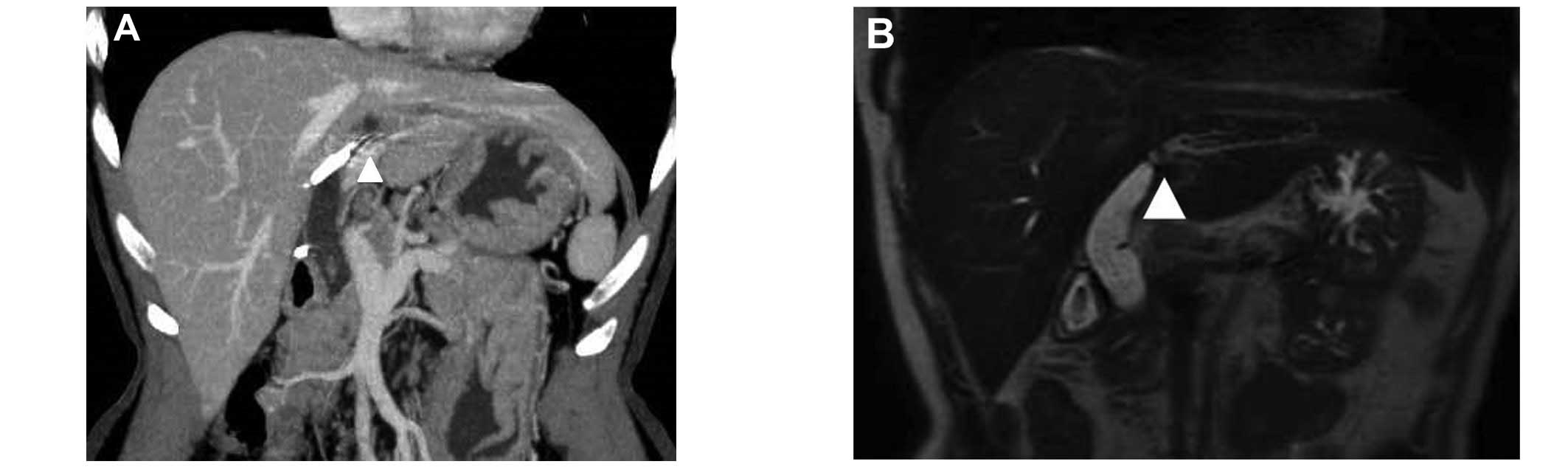
shadow. Computed tomography (CT) and magnetic resonance
cholangiopancreatography (MRCP) revealed severe stricture of the
left intrahepatic biliary duct and dilatation of the peripheral
biliary duct (Fig. 1). Tumors or
enlarged lymph nodes were not identified. A drainage tube was
inserted into the B3 and small stones were identified in the common
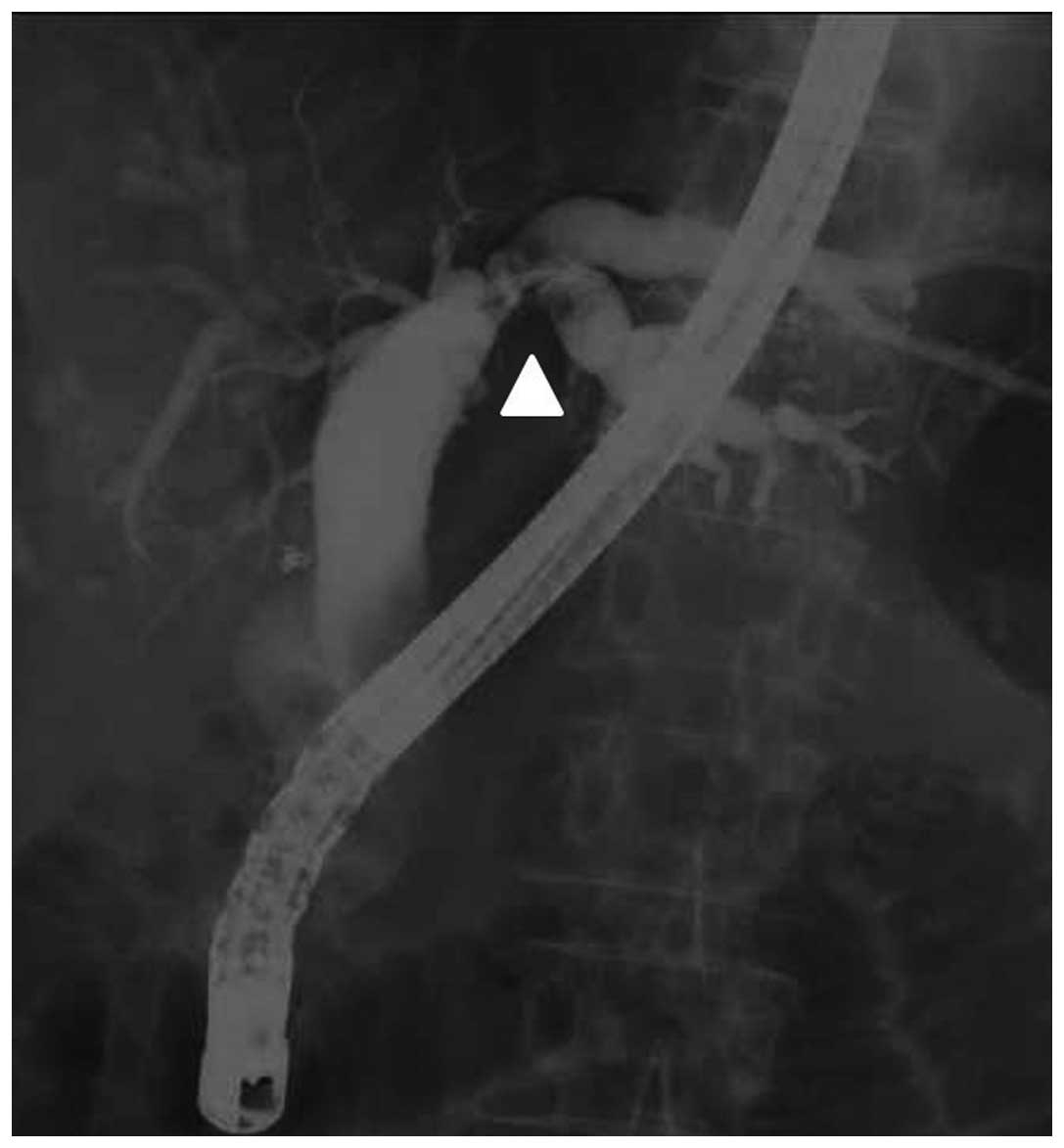
bile duct. Endoscopic retrograde cholangiopancreatography (ERCP)
revealed a severe stricture of the left intrahepatic biliary duct
and dilatation of the peripheral biliary duct, which was consistent
with the MRCP findings (Fig. 2). A
left hepatectomy was performed. No mass lesions were detected
around the liver hilum intraoperatively; however, a focal bile
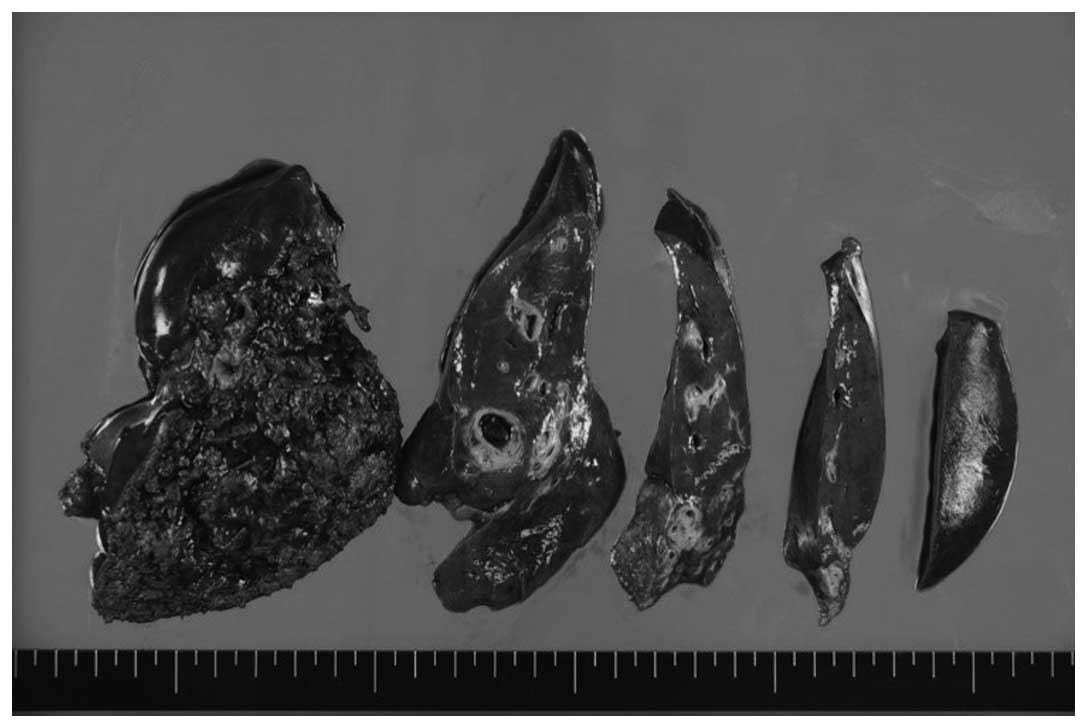
stricture was observed in the left liver hilum. Macroscopically,
inflamed granulation tissue was only found around the thickened
biliary duct. There was no mass lesion around the liver hilum;
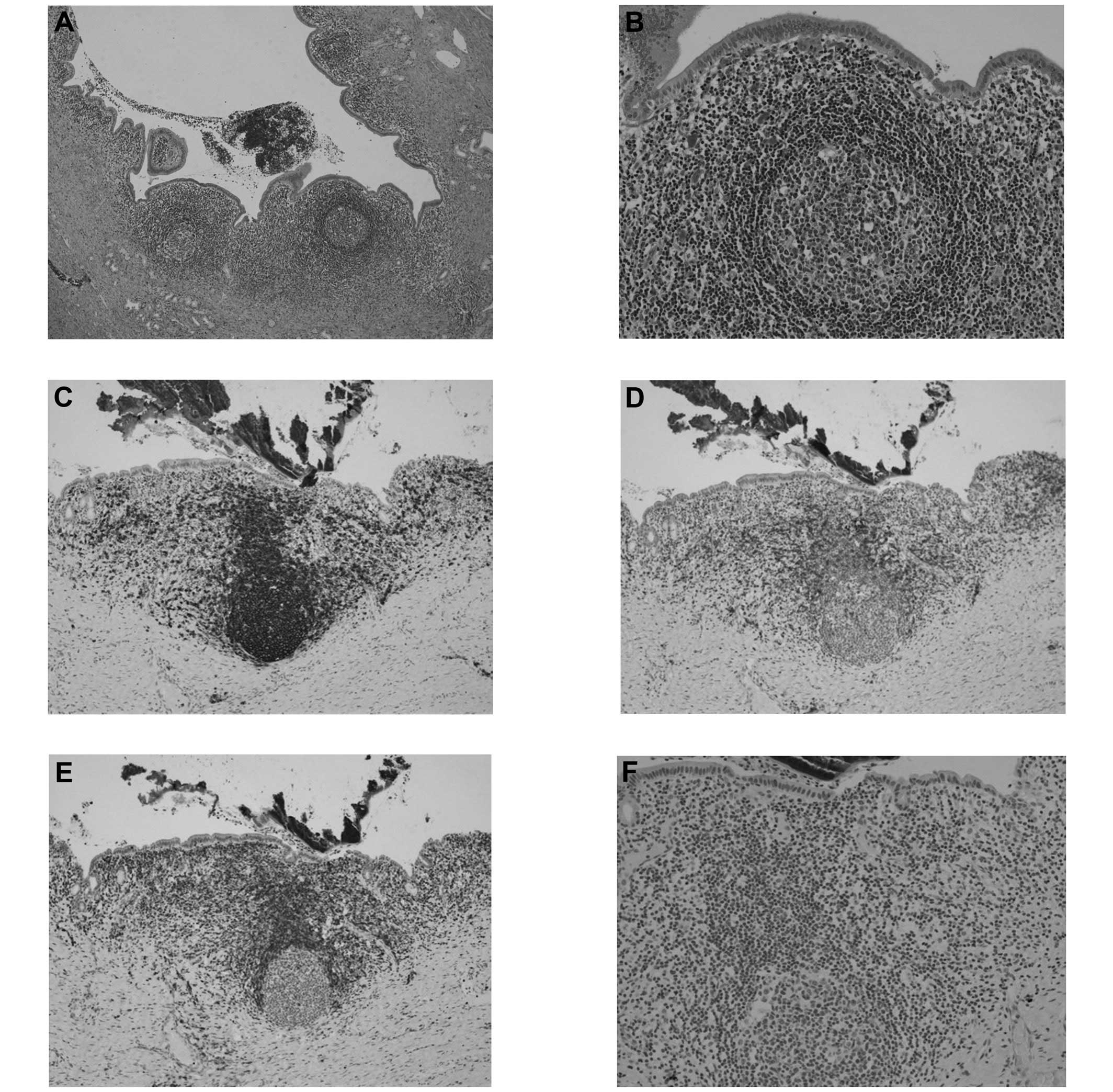
however, the wall of the duct was markedly thickened (Fig. 3). Microscopically, there was dense
fibrosis under the mucosal layer, which was accompanied by marked
formation of lymph follicles containing germinal centers. The
peribiliary glands were infiltrated by lymphocytes and plasma
cells. No obliterative phlebitis or vasculitis were observed. There
were few IgG4-positive cells (Fig.
4). The pathological findings were consistent with follicular
cholangitis. The patient did not experience recurrence of
cholangitis postoperatively for 1 year.
Discussion
Making a precise diagnosis upon identifying a
biliary stricture is difficult, and distinguishing a benign
stricture from malignant disease may be particularly challenging.
Follicular cholangitis is extremely rare and, to the best of our
knowledge, only 9 cases have been reported to date since Aoki et
al (5) first described this
condition in 2003. A review of previous reports on follicular
cholangitis is presented in Table I.
The radiological findings commonly indicate biliary stricture,
which mimics hilar cholangiocarcinoma, and there are no specific
symptoms or radiological findings that may be used to exclude
malignancy. The only ways to diagnose this disease are
histopathological analysis, or observation over an extended period
of time in order to determine whether it is progressive.
 | Table I.Clinical characteristics of the 9
patients with follicular cholangitis. |
Table I.
Clinical characteristics of the 9
patients with follicular cholangitis.
| Authors (Refs.) | Age, years | Gender | Symptoms at
onset | Progression of
disease | Pattern of
stricture | Response to
steroids | Long-term
outcome | Operation | Preoperative
diagnosis |
|---|
| Aoki et al
(5) | 57 | F | Elevation of LEs | Gradual | Focal | N/A | N/A | Extended right
hepatectomy |
Cholangiocarcinoma |
| Lee et al
(6) | 61 | M | Abdominal pain,
jaundice, elevation of LEs | Gradual | Focal | N/A | N/A | Resection of
extrahepatic bile duct and right intrahepatic duct |
Cholangiocarcinoma |
| Fujita et al
(7) | 44 | M | Elevation of LEs | Gradual | Focal | Moderate | Reccurence | Extended right
hepatectomy |
Cholangiocarcinoma |
|
| 58 | F | Elevation of LEs | Gradual | Focal | N/A | Death | Extended left
hepatectomy |
Cholangiocarcinoma |
| Zen et al
(8) | 73 | F | Abdominal pain and
jaundice, elevation of LEs | N/A | Focal | N/A | N/A | Right
hepatectomy |
Cholangiocarcinoma |
|
| 70 | M | Elevation of LEs | N/A | N/A | N/A | N/A | Left hepatectomy |
Cholangiocarcinoma |
|
| 42 | F | Pruritus and
jaundice | Gradual | N/A | N/A | N/A | Liver
transplantation | PSC |
| Fujii et al
(9) | 60 | F | Pruritus and
jaundice, general fatigue | N/A | Focal | N/A | N/A | Left hepatectomy |
Cholangiocarcinoma |
| Present case | 68 | F | Abdominal pain and
elevation of LEs | Gradual | Focal | N/A | 1 year | Left hepatectomy | Hepatolithiasis |
Representative histological findings have shown that
follicular cholangitis is characterized by dense fibrosis under the
mucosal layer, which is accompanied by marked formation of lymph
follicles that contain germinal centers. The peribiliary glands are
infiltrated by lymphoplasmacytic cells that are negative for IgG4
but positive for CD20, B-cell lymphoma 2 and CD4. These
pathological findings, rather than the radiological findings and
clinical presentation, are the only ones to definitively diagnose
follicular cholangitis. Our pathological findings were consistent
with those reported for follicular cholangitis. Fujii et al
(9) described the clinical
presentation and the step-by-step diagnosis of this disease.
Follicular cholangitis commonly occurs during middle age and in
patients with no significant history. The majority of the patients
presented with a gradual progression of the disease; the focal
stricture was localized to the hilum of the liver; the majority of
the patients underwent surgical treatment for suspicion of
cholangiocarcinoma. A total of 2 patients experienced recurrence of
cholangitis; 1 succumbed to liver failure, whereas the remaining
patient was treated with corticosteroids and achieved a moderate
improvement with close follow-up (6).
This is the first case in which the patient finally
underwent hepatectomy due to repeated attacks of cholangitis after
8 years of follow-up. We were able to identify the stricture of the
root of the left biliary duct on presentation in 2006. However, the
decision for surgical resection was based on the symptomatic
hepatolithiasis. The indications for hepatectomy for
hepatolithiasis are as follows: Hepatolithiasis in the unilateral
lobe, severe stricture or dilatation of the biliary duct,
hepatolithiasis associated with intrahepatic bile duct carcinoma,
accompanied by formation of hepatic abscesses or atrophy of the
liver (11,12). The radiological findings mimicked
those of intrahepatic cholangiocarcinoma; however, repeated
cytology of the bile juice revealed no malignancy. Following close
radiological follow-up, lymph node enlargement or progressive
biliary stricture were not observed. Therefore, conservative
treatment was selected. Over this long-term follow-up period, there
were no findings on ERCP and CT indicating progression.
This case suggests that close follow-up is
recommended if a conservative approach is selected following
identification of a focal biliary stricture, since its clinical
presentation and radiological findings are similar to those of
cholangiocarcinoma.
Herein, we presented a case of follicular
cholangitis with a focal intrahepatic stricture. It is difficult to
differentiate follicular cholangitis from hilar cholangiocarcinoma;
thus, surgical treatment should be performed if close follow-up is
not possible. Clinicians must consider causes of benign biliary
stricture, such as follicular cholangitis, which are
indistinguishable from malignancy.
References
|
1
|
Tamada K, Kanai N, Wada S, Tomiyama T,
Ohashi A, Satoh Y, Ido K and Sugano K: Utility and limitations of
intraductal ultrasonography in distinguishing longitudinal cancer
extension along the bile duct from inflammatory wall thickening.
Abdom Imaging. 26:623–631. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
van Leeuwen DJ and Reeders JWAJ: Primary
sclerosing cholangitis and cholangiocarcinoma as a diagnostic and
therapeutic dilemma. Ann Oncol. 10(Suppl 4): 89–93. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lee YM and Kaplan MM: Primary sclerosing
cholangitis. N Engl J Med. 332:924–933. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hamano H, Kawa S, Uehara T, Ochi Y,
Takayama M, Komatsu K, Muraki T, Umino J, Kiyosawa K and Miyagawa
S: Immunoglobulin G4-related lymphoplasmacytic sclerosing
cholangitis that mimics infiltrating hilar cholangiocarcinoma: Part
of a spectrum of autoimmune pancreatitis? Gastrointest Endosc.
62:152–157. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Aoki T, Kubota K, Oka T, Hasegawa K, Hirai
I and Makuuchi M: Follicular cholangitis: Another cause of benign
biliary stricture. Hepatogastroenterology. 50:639–642.
2003.PubMed/NCBI
|
|
6
|
Lee JY, Lim JH and Lim HK: Follicular
cholangitis mimicking hilar cholangiocarcinoma. Abdom Imaging.
30:744–747. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fujita T, Kojima M, Kato Y, Gotohda N,
Takahashi S, Konishi M and Kinoshita T: Clinical and
histopathological study of ‘follicular cholangitis’: Sclerosing
cholangitis with prominent lymphocytic infiltration masquerading as
hilar cholangiocarcinoma. Hepatol Res. 40:1239–1247. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zen Y, Ishikawa A, Ogiso S, Heaton N and
Portmann B: Follicular cholangitis and pancreatitis -
clinicopathological features and differential diagnosis of an
under-recognized entity. Histopathology. 60:261–269. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fujii M, Shiode J, Niguma T, Ito M,
Ishiyama S, Fujiwara A, Nose S, Yoshioka M and Mimura T: A case of
follicular cholangitis mimicking hilar cholangiocarcinoma. Clin J
Gastroenterol. 7:62–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gerhards MF, Vos P, van Gulik TM, Rauws
EAJ, Bosma A and Gouma DJ: Incidence of benign lesions in patients
resected for suspicious hilar obstruction. Br J Surg. 88:48–51.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Uchiyama K, Onishi H, Tani M, Kinoshita H,
Ueno M and Yamaue H: Indication and procedure for treatment of
hepatolithiasis. Arch Surg. 137:149–153. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chijiiwa K, Yamashita H, Yoshida J, Kuroki
S and Tanaka M: Current management and long-term prognosis of
hepatolithiasis. Arch Surg. 130:194–197. 1995. View Article : Google Scholar : PubMed/NCBI
|