Introduction
Retroperitoneal liposarcoma is a rare malignant
tumor with an incidence of 2.5/1,000,000 individuals (1). Although the incidence rate is very low,
early diagnosis is often difficult since symptoms appear only when
the tumor becomes very large. Retroperitoneal liposarcoma is
classified into five subtypes, according to the World Health
Organization Classification: i) Well-differentiated; ii)
dedifferentiated; iii) myxoid cell; iv) pleomorphic; v) mixed-type
(2). The kidney is the most
frequently invaded organ. Surgical resection is the predominant
treatment method for this disease, and negative margins must be
achieved to improve survival rate (1,3,4). It remains controversial as to whether
resection of adjacent organs extends the 5− or 10-year survival
rate. Additionally, the 10-year survival rate is not prolonged
following multi-organ resection (5–8).
Considering the complications of multi-organ resection, whether
nephrectomy or other organ resection is required remains to be
elucidated. The present study reported a case with retroperitoneal
liposarcoma managed at Guihang Guiyang Hospital (Guiyang, China),
and also performed a literature review on presentation, management
and prognosis of this patient.
Case report
A 60-year-old female presented to Guihang Guiyang
Hospital with abdominal distension in the right side for the
previous 2-months, with a touchable mass identified for the
previous 1-month. The clinical symptom was just abdominal
distension and no significant history relevant to this case was
determined. The physical examination indicated a 10×15 cm flexible
mass located in right side of the stomach. This mass lacked
tenderness and exhibited an unclear boundary. The laboratory
examinations, including assessment of tumor markers, routine blood,
urine and stool tests, revealed no clear abnormalities. Computed
tomography (Fig. 1) and magnetic
resonance imaging (Fig. 2)
demonstrated a huge mass in the right abdomen. The diagnosis was
well-differentiated retroperitoneal liposarcoma. No evidence was
found to support distant metastasis, with the exception that it is
possible that the tumor had invaded the kidney.
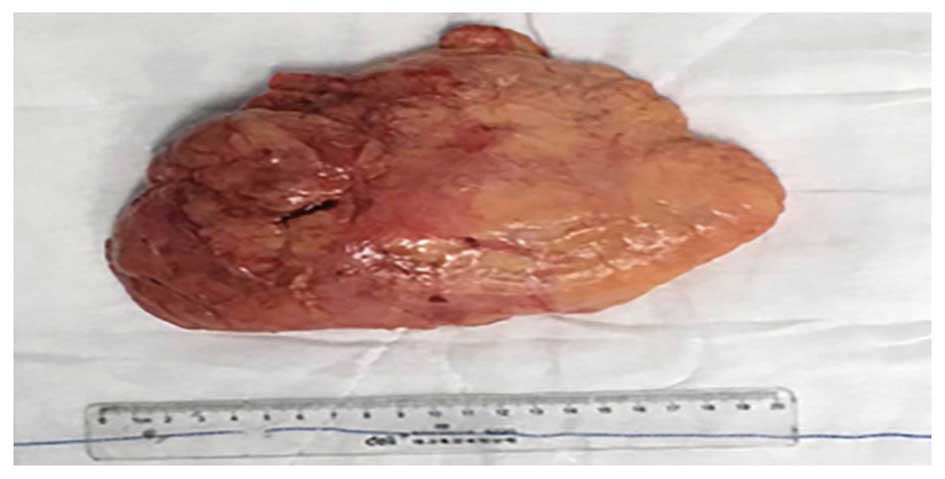
During surgery, it was revealed that the mass
originated from the right fatty renal capsule and the kidney was
covered by the carcinoma. The patient received complete resection
of the liposarcoma and the right kidney was preserved. The
carcinoma covering the kidney was removed. Renal fascia was intact
and no sign of invasion was visible. The renal periphery was
completely bare, including the renal portal, the ureter and the
inferior vena cava. The total mass was 20×15×10 cm in size
(Figs. 3 and 4).
Hematoxylin and eosin staining of tissue shows that
retroperitoneal well-differentiated liposarcoma, with negative
margins, full of lipocytes. It was confirmed that the carcinoma had
invaded the fatty renal capsule (Fig.
5). Immunohistochemical analysis was performed at the
Department of Pathology, Guihang Guiyang Hospital. The mass was
positive for CD63 and CD163 (data not shown). The patient recovered
well and was transferred to the Oncology Department 2 weeks after
surgery for chemotherapy and radiotherapy. No tumor recurrence was
observed at the 6-month follow-up.
Discussion
Liposarcoma is one of the most common soft-tissue
sarcomas that frequently occurs between the ages of 40 and 70 years
(9). Since retroperitoneal
liposarcoma has no characteristic symptom, the complaints of
patients are predominantly associated with direct invasion or
compression of other adjacent organs. No significant laboratory
abnormalities are observed in the earlier stages and the tumor
often has to grow to a larger size before diagnosis can be made.
Such tumors are often identified using a diagnostic modality,
including computed tomography or magnetic resonance imaging. R0
resection of retroperitoneal liposarcoma had been suggested as the
only way to cure the patients (2,8,10).
In order to achieve the R0 resection, contiguous
organ resection, including nephrectomy, is always performed when
the intraoperative histological results are dedifferentiated,
myxoid/round cell, pleomorphic or mixed-type (10). A recent report demonstrates that with
R0 resection, the 5-year survival for well-differentiated subtypes
is 90%, while 5-year survival for pleomorphic subtypes is only
30–50%. Dedifferentiated and myxoid/round cell subtypes have 5-year
survival rates of 75% and 60–90%, respectively (11). Since it is difficult to detect the
retroperitoneal liposarcoma from adjacent normal fat, even if
resection of the contiguous organ is performed, the rate of local
recurrence is notably high, particularly in high-grade subtypes
(12). In order to obtain the free
margin, although the single or multi-organ resection may improve
clinical outcome, the complication and the quality of life must be
considered. The long-term survival rate has been confirmed in a
subset of patients after R2 resection (5), particularly with good histological
characteristics, including the well-differentiated type. At a
6-month follow-up of the present case, no signs of metastasis or
recurrence were observed. Previously, more and more investigations
and case reports are inclined to preserve-organ surgery combined
with neoadjuvant chemotherapy and radiotherapy to improve the
clinical outcome (12–14). It is of great surprise that a new
drug, Eribulin mesylate (Halaven), has been approved to treat
non-resectable or metastasized liposarcoma (15). Recent research, including 228
patients with retroperitoneal liposarcoma, undergoing surgery in
Russia, revealed that the 10-year survival rate was 26% following
combined organ surgeries, compared with 35% following surgery on
patients not requiring multi-organ resection in dedifferentiated,
myxoid cell, pleomorphic and mixed-type cases (7). Low-grade liposarcoma is an expansively
growing tumor and so invasion to other organs is relatively rare.
Surgical excision with a wide margin will increase the adverse
effects, particularly on intestines. Adjacent organ resection is
often not necessary since the invasion potential of these tumor
types is low (11). Therefore, the
present study suggested that nephrectomy must only be performed if
required to accomplish a complete gross resection R0 in others
histological subtypes. Numerous previous studies have shown that
histological subtype, incomplete resection, contiguous organ
resection and increasing age are markedly associated with mortality
from this tumor. However, tumor burden and nephrectomy were not
associated with disease-specific survival (10). Therefore, according to the
intraoperative histological subtype, combined organ resection may
not be required if confirmed as a well-differentiated tumor. In
addition, it is important to have intraoperative histological
confirmation on obtained free margins. R0 resection is a
gold-standard for retroperitoneal liposarcoma. However, if free
margins cannot be achieved by combined organ resection, the
decision should be made as to whether combined organ resection can
be performed, particularly in low-grade tumor types. Maybe R1 or R2
resection combined with neoadjuvant chemotherapy and radiotherapy
are a novel therapeutic method (5,13).
Therefore, each aspect of the tumor histological characteristics,
the quality of life of the patients, the complications of
organ-resection, the benefit of the R0 resection and the long-team
survival rate must be considered.
In conclusion, it is unnecessary to performed
aggressive surgery, including organ resection, for the majority of
well-differentiated retroperitoneal liposarcomas. However, the
other subtypes of tumor may require expanding resection, including
nephrectomy, in order to obtain negative margins according to the
intraoperative histological outcome. A novel therapeutic method,
including R1 or R2 resection combined with neoadjuvant chemotherapy
and radiotherapy can be performed. However, multi-center, large
sample investigations must be performed to further confirm this
hypothesis.
References
|
1
|
Sato Y, Yamamoto S and Fujita S:
Retroperitoneal liposarcoma with Colonic Involvement: A Case
Report. Jpn J Clin Oncol. 44:374–378. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Caizzone A, Saladino E, Fleres F,
Paviglianiti C, Iaropoli F, Mazzeo C, Cucinotta E and Macrì A:
Giant retroperitoneal liposarcoma: Case report and review of the
literature. int J Surg Case Rep. 9:23–22. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gemici K, Buldu İ, Acar T, Alptekin H,
Kaynar M, Tekinarslan E, Karatağ T, Efe D, Çolak H, Küçükkartallar
T and İstanbulluoğlu MO: Management of patients with
retroperitoneal tumors and a review of the literature. World J Surg
Oncol. 13:1432015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang WD, Liu DR, Que RS, Zhou CB, Zhan
CN, Zhao JG and Chen LI: Management of retroperitoneal liposarcoma:
A case report and review of the literature. Oncol Lett. 10:405–409.
2015.PubMed/NCBI
|
|
5
|
Klooster B, Rajeev R, Chrabaszcz S,
Charlson J, Miura J, Bedi M, Gamblin TC, Johnston F and Turaga KK:
Is long-term survival possible after margin-positive resection of
retroperitoneal sarcoma (RPS)? J Surg Oncol. 113:823–827. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tseng WW, Madewell JE, Wei W, Somaiah N,
Lazar AJ, Ghadimi MP, Hoffman A, Pisters PW, Lev DC and Pollock RE:
Locoregional disease patterns in well-differentiated and
dedifferentiated retroperitoneal liposarcoma: Implications for
extent of resection? Ann Surg Oncol. 21:2136–2143. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Stilidi IS, Nikulin MP, Nered SN, Davydov
MM, Bolotskiĭ VI and Gubina GI: Combined operations by
retroperitoneal liposacomas. Khirurgiia (Mosk). 20–25. 2013.(In
Russian). PubMed/NCBI
|
|
8
|
Ikeguchi M, Urushibara S, Shimoda R, Saito
H and Wakatsuki T: Surgical treatment of retroperitoneal
liposarcoma. Yonago Acta Med. 57:129–132. 2014.PubMed/NCBI
|
|
9
|
Oh SE, Kim HJ, Choi SJ, Oh SY, Roh CR and
Kim JH: A case of huge retroperitoneal liposarcoma in pregnancy.
Obstet Gynecol Sci. 57:236–239. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Singer S, Antonescu CR, Riedel E and
Brennan MF: Histologic subtype and margin of resection predict
pattern of recurrence and survival for retroperitoneal liposarcoma.
Ann Surg. 238:358–371, 370–371. 2003.PubMed/NCBI
|
|
11
|
Karadayi K, Yildiz C, Karakus S, Kurt A,
Bozkurt B, Soylu S, Cicekli AA, Egilmez R and Cetin A:
Well-differentiated abdominal liposarcoma: Experience of a tertiary
care center. World J Surg Oncol. 13:1662015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kirane A and Crago AM: The importance of
surgical margins in retroperitoneal sacoma. J Surg Oncol.
113:270–276. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Cheng H, Miura JT, Lalehzari M, Rajeev R,
Donahue AE, Bedi M, Gamblin TC, Turaga KK and Johnston FM:
Neoadjuvant radiotherapy for retroperitoneal sarcoma: A systematic
review. J Surg Oncol. 113:628–634. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Abdelfatah E, Guzzetta AA, Nagarajan N,
Wolfgang CL, Pawlik TM, Choti MA, Schulick R, Montgomery EA, Meyer
C, Thornton K, et al: Long-term outcomes in treatment of
retroperitoneal sarcomas: A 15 year single-institution evaluation
of prognostic features. J Surg Oncol. 114:56–64. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aschenbrenner DS: The first drug to
improve survival in liposarcoma. Am J Nurs. 116:242016. View Article : Google Scholar
|