Introduction
Ovarian steroid cell tumors (SCT) are rare sex
cord-stromal tumors of the ovary and comprise <0.1% of all
ovarian tumors (1). Based on the
cell of origin, they may be divided into three subtypes: Leydig
cell tumors arising from Leydig cells in the hilum of the ovary,
stromal luteomas arising from ovarian stromal cells, and steroid
cell tumors not otherwise specified (NOS). The last subtype makes
up ~2/3 of SCTs and tends to affect younger women (mean age, 43
years). SCT-NOS are usually benign; however, clinically malignant
behavior, such as peritoneal metastases, occurs in 25–40% of the
cases (2,3). We herein report a case of an ovarian
SCT-NOS in a 5-year-old female Chinese patient who presented with
sudden abdominal pain and repeated vomiting. Aspects of the
presentation, diagnosis and treatment of these tumors are also
discussed.
Case report
A 5-year-old female Chinese patient presented to the
Department of Obstetrics and Genecology of the Anhui Provincial
Hospital (Hefei, China) on 2/12/2011 with sudden abdominal pain and
repeated vomiting. A computed tomography (CT) pelvic scan and
ultrasound examination in another hospital on the previous day
revealed a pelvic mass. The B-ultrasound scan in our hospital
revealed a solid, right ovarian tumor sized 85×45×73 mm. On
laboratory analysis, the serum carbohydrate antigen (CA) 19-9 level
was 30.25 U/ml (normal, 0–34 U/ml); the β-human chorionic
gonadotropin level was <0.10 IU/l (non-pregnancy, <0.5–2.9
IU/l); the α-fetoprotein level was 1.15 ng/ml (normal, 0–8 ng/ml);
and the CA125 level was 37.71 U/ml (normal, 0–39 U/ml). The patient
underwent urgent exploratory laparotomy, and the right ovary, sized
8×4×7 cm, exhibited a smooth, unruptured surface and was reversed
720 together with the right Fallopian tube and the right ovarian
intrinsic ligament. The patient was then treated by right
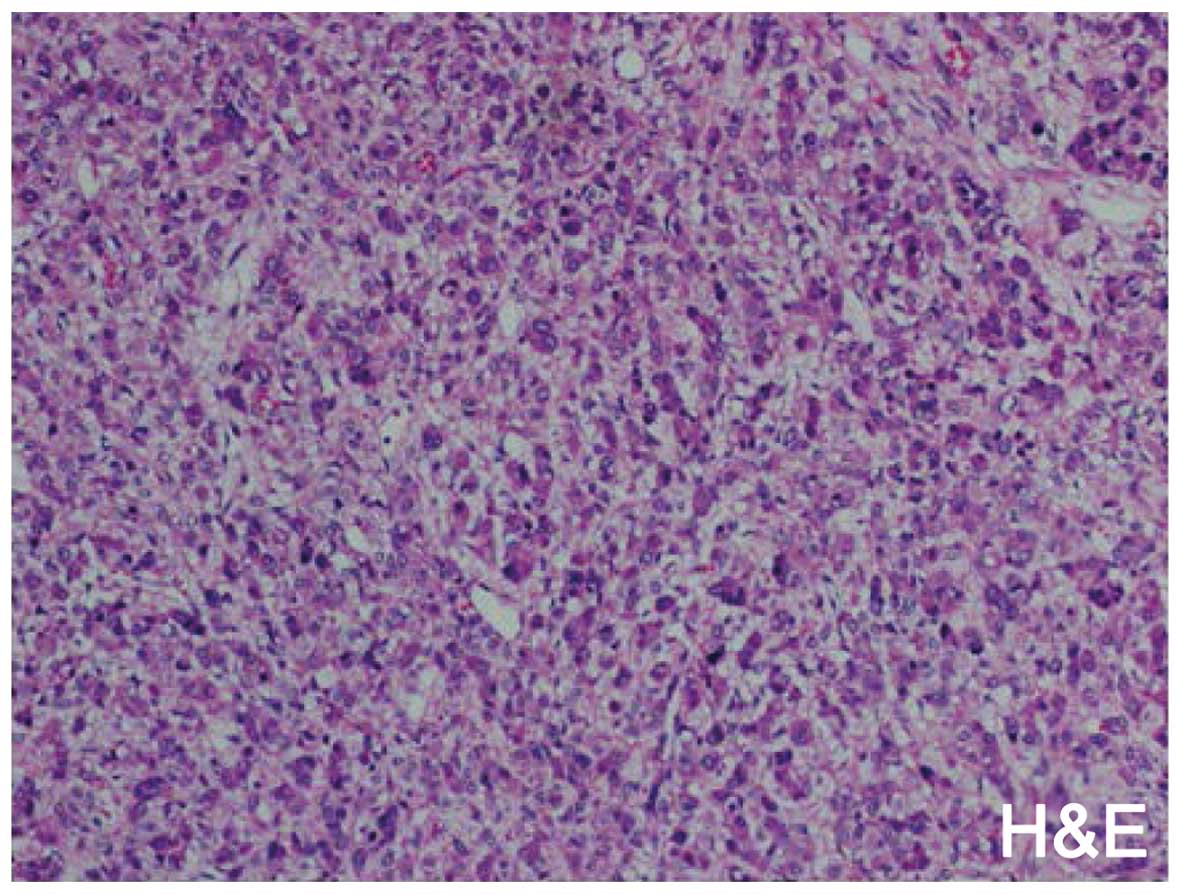
salpingo-oophorectomy. The histopathological examination revealed
an ovarian SCT-NOS (Fig. 1),
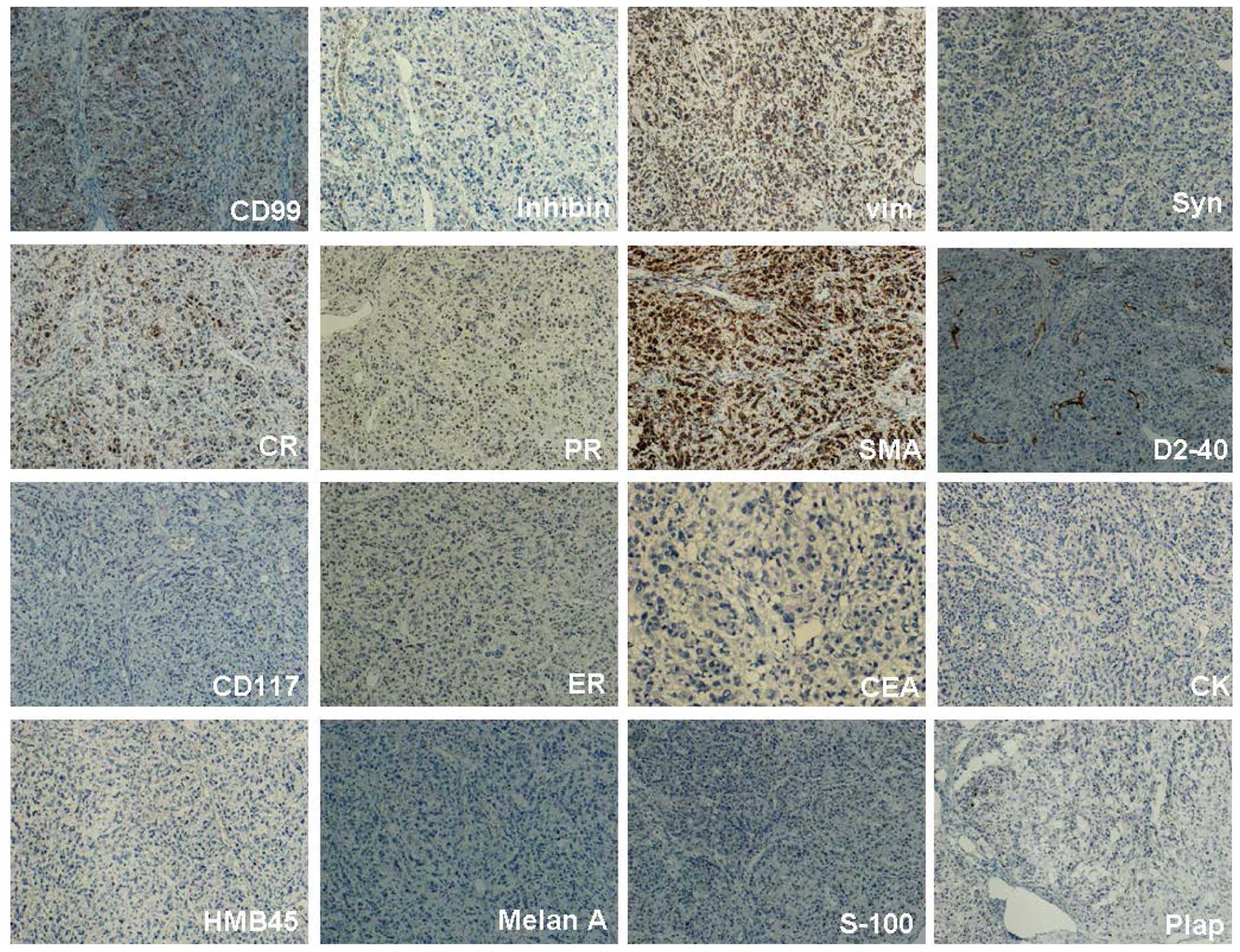
composed of cells positive for inhibin, vimentin, progesterone
receptor, calretinin, somatostatin, synaptophysin, CD99, and weakly
for D2-40, and negative for CD117, estrogen receptor,
carcinoembryonic antigen, cytokeratin, human melanoma black 45,
Melan A, S-100 and placental alkaline phosphatase (Fig. 2). The patient has been followed up
for 5 years since the surgery, without evidence of recurrence or
metastasis, or abnormalities on the laboratory test results.
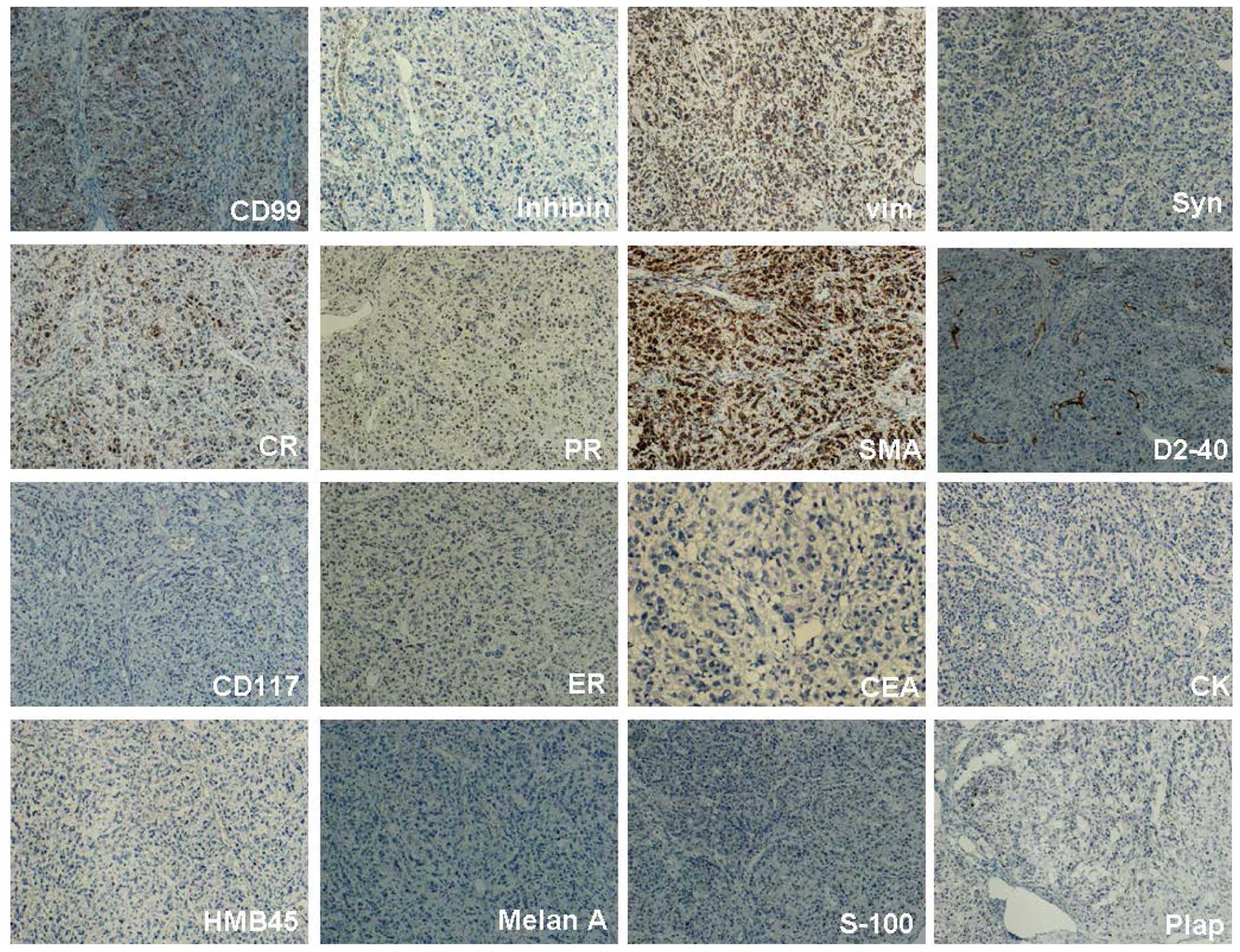 | Figure 2.Immunohistochemical examination of the
ovarian tumor (magnification, ×160). The tumor cells were positive
(brown staining) for inhibin, vimentin (vim), progesterone receptor
(PR), calretinin (CR), somatostatin (SMA), synaptophysin (Syn),
CD99 and weakly positive for D2-40, ER, estrogen receptor; CEA,
carcinoembryonic antigen; CK, cytokeratin; HMB45, human melanoma
black 45; Plap, placental alkaline phosphatase. |
Discussion
The term ‘steroid cell tumors not otherwise
specified’ was first used by Scully and signifies that the cell
lineage is not defined; thus, they cannot be categorized as either
stromal luteomas or Leydig cell tumors (4,5).
Approximately 56–77% of the cases are clinically associated with
androgenic changes, such as hirsutism and virilization; 6–7% of the
cases are clinically associated with Cushing's syndrome; and 25% of
SCT-NOS are non-functional. Ovarian SCT-NOS may occur at any age
(mean age, 43 years) and, occasionally, before puberty (6). In our case, the patient was aged 5
years, without any changes in blood pressure, virilization or
hirsutism. The patient has been followed up for 5 years since the
surgery, without disease recurrence or metastasis. To the best of
our knowledge, the youngest reported patient was aged 2.5 years
when she first presented with virilization; the androgenic changes
subsided following surgical removal of the enlarged cystic right
ovary, but the patient succumbed to diffuse metastatic disease
originating in an apparently unrelated undifferentiated sarcoma of
the oropharynx 17 months after initial diagnosis (7).
According to the study of Hayes and Scully, the
following pathological characteristics may indicate malignancy: ≥2
mitotic figures per 10 high-power fields is associated with a 92%
risk of malignancy; necrosis with an 86% risk of malignancy; a
diameter of >7 cm with a 78% risk of malignancy; hemorrhage with
a 77% risk of malignancy; and grade 2 or 3 nuclear atypia with a
64% risk of malignancy (6). To date,
24 cases of ovarian SCT in young female patients aged 2.5–13 years
have been reported, but none have been malignant (6,8–11). Therefore, ovarian masses suspicious
for SCT in children at an early stage should be approached
conservatively, unless distinct signs of metastasis are present at
the time of surgery (12).
Immunohistochemistry is particularly useful for the accurate
diagnosis of SCTs. Moreover, unilateral salpingo-oophorectomy is
generally considered to be adequate for pediatric patients with
stage I a disease (6). In our
patient, although the diameter of the mass was >7 cm, we opted
for right salpingo-oophorectomy as the tumor was stage Ia. It is
also necessary to monitor the patient's hormone levels as part of
their postoperative follow-up (12).
To date, very few reports have investigated the
efficacy of radiation or chemotherapy for SCTs (13). However, malignant SCT-NOS should be
managed with total abdominal hysterectomy, bilateral
salpingo-oophorectomy and sampling of pelvic and mesenteric lymph
nodes and omentum followed by combination chemotherapy. Though a
definitive chemotherapy regimen is not yet defined, Bleomycin,
Etoposide and Cisplatin (BEP) is favored and often used.
Chemotherapy maybe applied using the BEP regimen [bleomycin (20
U/m2 every 3 weeks for 4 cycles), etoposide (75
mg/m2 on days 1–5, every 3 weeks for 4 cycles) and
cisplatin (20 mg/m2 on days 1–5, every 3 weeks for 4
cycles)] (14), or other medications
(6). Gonadotropin releasing hormone
agonist has been used as therapy for recurrent malignant disease
for its suppressive effect on ovarian steroidogenesis (15).
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant nos. 81001168 and 81272881), the
Anhui Provincial Natural Science Foundation Project (grant no.
1308085MH122), and the Anhui Provincial Natural Science Research
Project of Anhui Provincial Higher University Education (grant no.
1301043053).
References
|
1
|
Liu AX, Sun J, Shao WQ, Jin HM and Song
WQ: Steroid cell tumors, not otherwise specified (NOS), in an
accessory ovary: A case report and literature review. Gynecol
Oncol. 97:260–262. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Haroon S, Idrees R, Fatima S, Memon A and
Kayani N: Ovarian steroid cell tumor, not otherwise specified: A
clinicopathological and immunohistochemical experience of 12 cases.
J Obstet Gynaecol Res. 41:424–431. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sood N, Desai K, Chindris AM, Lewis J and
Dinh TA: Symptomatic ovarian steroid cell tumor not otherwise
specified in a post-menopausal woman. Rare Tumors. 8:62002016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Scully RE: Ovarian tumors. A review. Am J
Pathol. 87:686–720. 1977.PubMed/NCBI
|
|
5
|
Scully RE: Classification of human ovarian
tumors. Environ Health Perspect. 73:15–25. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hayes MC and Scully RE: Ovarian steroid
cell tumors (not otherwise specified). A clinicopathological
analysis of 63 cases. Am J Surg Pathol. 11:835–845. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ammann AJ, Kaufman S and Gilbert A:
Virilizing ovarian tumor in a 2 1/2-year-old girl. J Pediatr.
70:782–787. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lee SH, Kang MS, Lee GS and Chung WY:
Refractory hypertension and isosexual pseudoprecocious puberty
associated with renin-secreting ovarian steroid cell tumor in a
girl. J Korean Med Sci. 26:836–838. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mitty HA and Cohen BA: Adrenal imaging.
Urol Clin North Am. 12:771–785. 1985.PubMed/NCBI
|
|
10
|
Fristachi CE, Santo GC, Pascalicchio JC
and Baracat FF: Lipoid cell tumor of the ovary. Rev Paul Med.
109:88–90. 1991.(In Portuguese). PubMed/NCBI
|
|
11
|
Younis JS, Bercovici B, Zlotogorski A,
Horne T and Glaser B: Lipid cell tumor of the ovary: Steroid
hormone secretory pattern and localization using
75Se-selenomethylcholesterol. Gynecol Obstet Invest. 27:110–112.
1989. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wan J, Chen X and Li X: Ovarian steroid
cell tumor, not otherwise specified: A rare case of postmenopausal
vaginal bleeding. Oncol Lett. 8:1187–1189. 2014.PubMed/NCBI
|
|
13
|
Das A, Panda S and Singh AS: Steroid cell
tumor: A rare virilizing ovarian tumor. J Cancer Res Ther.
11:6602015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Reedy MB, Richards WE, Ueland F, Uy K, Lee
EY, Bryant C and van Nagell JR Jr: Ovarian steroid cell tumors, not
otherwise specified: A case report and literature review. Gynecol
Oncol. 75:293–297. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim JS, Park SN and Kim BR: Recurrent
ovarian steroid cell tumor, not otherwise specified managed with
debulking surgery, radiofrequency ablation, and adjuvant
chemotherapy. Obstet Gynecol Sci. 57:534–538. 2014. View Article : Google Scholar : PubMed/NCBI
|