Introduction
Colon cancer is second in morbidity and the third
cause of cancer-related mortality worldwide (1). With the advances in diagnostic
techniques, early diagnosis of metastases in patients with colon
cancer has also improved, allowing patients to access treatment
timely and effectively (2).
Hematogenous metastasis is the main route of metastasis of colon
cancer cells (3). Hence, the
metastatic cells are able to invade distal organs and structures.
The most common site of metastatic tumors originating from colon
cancer is the liver, followed by the lungs, bone and other internal
organs (4). Although liver
metastases from colon cancer has a relatively favorable prognosis
(progression-free survival of ~23 months), metastases from colon
cancer remain to be further investigated (4,5).
Moreover, colon cancer metastases to rare sites, such as the oral
cavity, carry a worse prognosis (6).
Metastatic oral tumors are rare, contributing to ~1%
of all oral tumors (7).
Theoretically, all types of tumors may metastasize to the oral
cavity, the most common primary organs being the lungs in men and
the breast in women. However, metastatic tumors in the oral cavity
originating from the colon are rare, and the number of relevant
clinical studies is limited. The lack of clinical observations
makes the diagnosis and treatment of oral metastases difficult. We
herein report an unusual case of colon carcinoma, where the patient
originally presented with oral bleeding, with ulceration and edema
of the gingival region of the mandible. The patient was later
diagnosed with a metastatic gingival tumor originating from a
primary colon adenocarcinoma with partial squamous
differentiation.
Case report
The patient, a 60-year-old male, is currently
undergoing chemotherapy for colon adenocarcinoma, which was
diagnosed in April, 2014. A radical operation was performed at the
time for the adenocarcinoma; however, liver metastases from colon
cancer appeared postoperatively (December, 2014). The patient
subsequently received successive bouts of chemotherapy (FOLFOX4,
XELIRI, FOLFIRI, Raltitrexed + irinotecan and S-1 + apatinib) and
radiotherapy. The metastatic lesions were treated with injections
of anhydrous alcohol and ultrasound-guided radiofrequency ablation,
but the cancer progressed (increase in the size of the hepatic
lesions and the levels of carcinoembryonic antigen and carbohydrate
antigen 19-9). In May 2016, the patient complained of oral
bleeding, ulceration and edema of the left gingival region of the
mandible over several weeks. The patient was originally prescribed
oral metronidazole by an oral clinician. As the aforementioned
symptoms were not relieved with this treatment, the patient
reported the symptoms to his doctor at the Cancer Center of the
Union Hospital (Wuhan, China) in June, 2016, during his
chemotherapy session for colon cancer. An initial extraoral
examination yielded no significant findings, and the patient had no
family history of oral diseases. However, a reddish nodule was
found in the gingival mucosa of the left mandible, and the patient
also reported pain and looseness of the teeth in the vicinity of
the nodule. The patient was referred to our oral clinician for a
consultation. It was suggested that proliferative response to
inflammation, benign neoplasms and primary or metastatic tumors of
the oral cavity should be considered in the differential diagnosis.
During that time, the patient continued to receive the scheduled
chemotherapy. With the suspicion of oral cavity metastases from the
colon adenocarcinoma, an excisional biopsy was performed. The
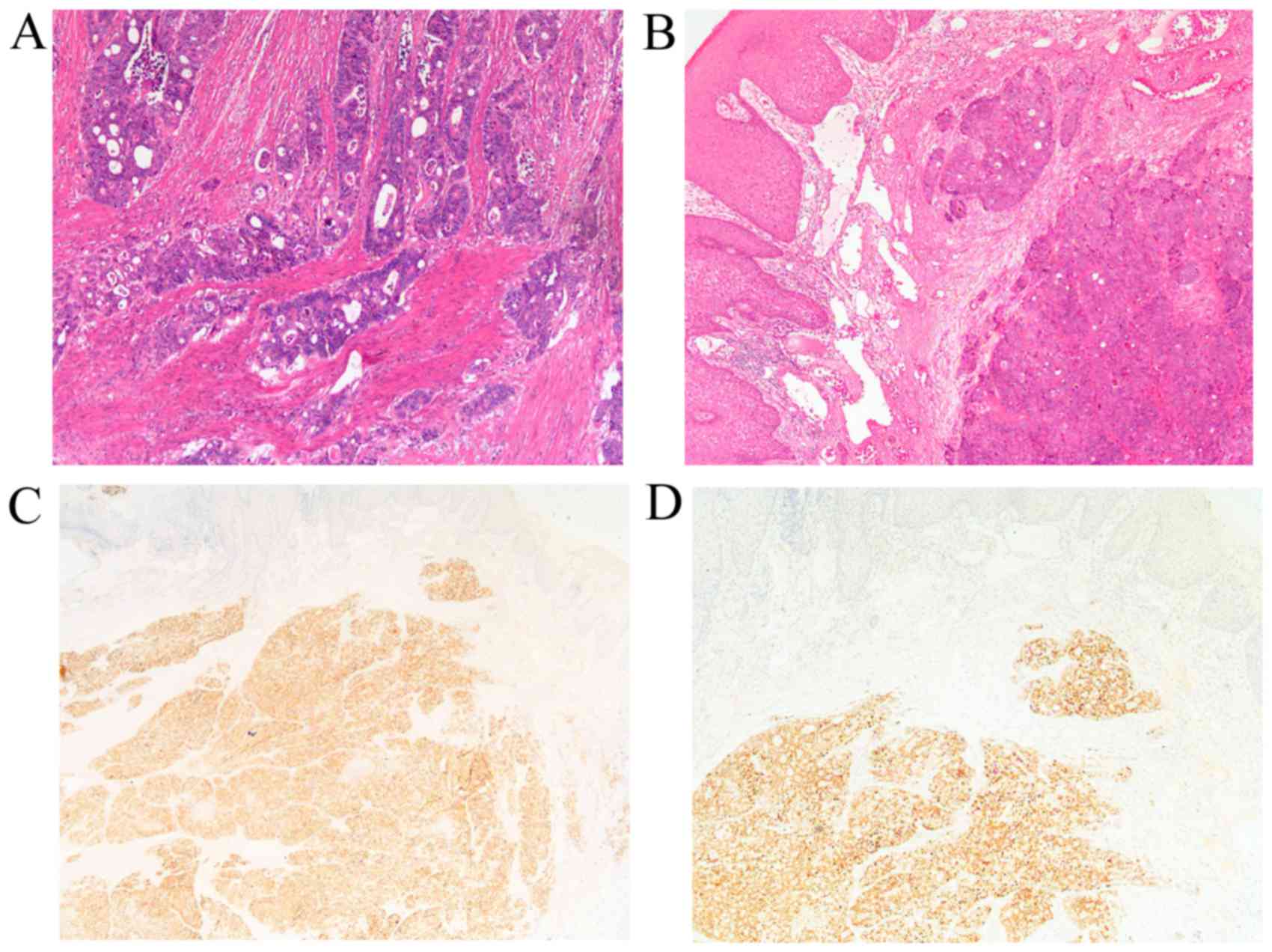
result of the pathological examination revealed poorly
differentiated adenocarcinoma, indicative of metastatic
adenocarcinoma originating in the colon, with partial squamous cell
differentiation (Fig. 1). The
patient was ultimately diagnosed with gingival metastases from the
colon adenocarcinoma with partial squamous differentiation.
Chemotherapy and local radiotherapy of the left gingival region was
then scheduled.
Discussion
Despite advances in medicine, the incidence and
mortality of colon cancer are on the increase in developing
countries. Moreover, once metastases occur, tolerance to treatment
commonly develops, which is associated with a poor prognosis
(1,8). As metastasis of colon cancer to the
oral cavity is rare, clinical observations and studies are scarce.
To the best of our knowledge, this is the first case of oral cavity
metastases from colon adenocarcinoma to be accompanied by partial
squamous differentiation.
On immunohistochemical examination, the tumor cells
of the gingival lesion were positive for cytokeratin (CK)20,
villin, CDX2, P63, P40, CK5/6, and sporadically for CK7, whereas
they were negative for synaptophysin and chromogranin A. Tumor
cells expressing CDX2 and villin were hypothesized to have
originated from the digestive tract, while positive immunostaining
for CK20 and sporadic CK7 positivity aided in the preliminarily
confirmation of metastases from colon cancer (9). Of note, CK5/6, P40 and P63, which are
biomarkers for squamous carcinomas, were also highly expressed.
Finally, the definitive diagnosis was gingival metastasis from
sigmoid adenocarcinoma with partial occult squamous
differentiation. To the best of our knowledge, this is the first
reported case of this type of gingival metastasis. While the origin
of the gingival metastases from the colon adenocarcinoma was
confirmed, the presence of the partial squamous differentiation in
the gingival lesion has not been fully elucidated. This finding may
be attributed to squamous differentiation of the adenocarcinoma;
however, there is also a possibility of a second malignancy,
particularly since the majority of primary cancers of the head and
neck (including the oral cavity) are squamous cell carcinomas. At
present, in addition to continuing chemotherapy, the patient was
scheduled for local radiotherapy to the gingival region.
To better understand the association between oral
cavity metastases and colon cancer, 12 cases of oral cavity
metastases of colon cancer, including the present case, were
reviewed [6,7,10–18); Table I]. It
was observed that mandibular metastases from colon cancer regularly
occurred the sixth and seventh decades of life. Oral metastases in
patients with colon cancer may be correlated with age, whereas
there was no significant difference according to gender. There is a
well-known age-associated decline in function of the immune system;
in addition, the immune state of the patients and inflammation have
been suggested to play an important role in the invasion and
metastasis of tumor cells (19,20).
Therefore, it is hypothesized that a reduced immune response may
contribute to the higher incidence of oral cavity metastases from
colon cancer. It was also observed that the most common site of
oral metastases in colon cancer patients was the mandible (8/13),
followed by the gingiva, accounting for one-fourth of all oral
metastases (4/13). Approximately one-fourth (5/13) of the reviewed
cases reported synchronous diagnosis of oral cavity metastases and
primary colon cancer. Of note, colon cancer also metastasized to
extraoral tissues and organs, in addition to the oral cavity.
Furthermore, it appears that the liver is the first organ to
develop metastasis from colon cancer, followed by the lungs, bone
and other rare sites. A potential underlying mechanism may include
specific tissues and organs releasing respective ligands to attract
metastatic cancer cells of differential origins. Furthermore,
patients with oral metastases responded poorly to treatment and
were unable tolerate follow-up treatment.
 | Table I.Previously reported case studies on
soft tissue oral cavity metastasis from colon carcinomas. |
Table I.
Previously reported case studies on
soft tissue oral cavity metastasis from colon carcinomas.
| No. | Author/year | Gender/age | Site of soft tissue
in the oral cavity | Other metastases | Diagnostic
sequence | Treatment for oral
metastases | Follow-up | (Refs.) |
|---|
| 1 | Naylor/1989 | F/65 | Mandible | Yes | Colon to oral, 5
years later | Radiotherapy | ND | (10) |
| 2 | Nitzan/1990 | F/75 | Mandible | Yes | Oral to colon,
SD | ND | ND | (11) |
| 3 | Babu/1996 | M/75 | Mandible | Yes | Oral to colon,
SD | Chemotherapy,
radiotherapy | Alive, ND | (12) |
| 4 | Bentley/1997 | F/70 | Zygoma | Yes | Colon to oral, 6
years later | Radiotherapy | ND | (13) |
| 5 | Mason/2005 | M/73 | Mandible | Yes | Oral to colon,
SD | None | Died, shortly | (14) |
| 6 |
AlvarezAlvarez/2006 | M/73 | Gingiva | Yes | Colon to oral, 6
months later | None | Died, 6 months
later | (15) |
| 7 | Chen/2008 | M/64 | Mandible | Yes | Colon to oral,
SD | Chemotherapy,
radiotherapy | Died, 6 months
later | (16) |
| 8 | Favia/2010 | F/66 | Mandible | No | Colon to oral, 15
years later | ND | ND | (17) |
| 9 | Favia/2010 | F/35 | Mandible | No | Colon to oral, 1 year
later | ND | ND | (17) |
| 10 | Amin/2011 | M/75 | Mandible | Yes | Colon to oral, 5
months later | Radiotherapy | ND | (7) |
| 11 | Soares/2011 | M/42 | Gingiva | No | Oral to colon,
SD | Chemotherapy | Alive, ND | (6) |
| 12 | Yang/2014 | F/74 | Gingiva | Yes | Colon to oral, 2
years later | Palliative
treatment | Died, 3 months
later | (18) |
| 13 | Present case | M/60 | Gingiva | Yes | Colon to oral, 2
years later | Chemotherapy,
radiotherapy | Alive |
|
We herein report a rare case of oral metastasis from
a colon adenocarcinoma with partial squamous differentiation. Based
on our observations and the review of similar case studies to
highlight the general characteristics of oral metastases in cancer
patients, several key points should be accounted for when
diagnosing colon cancer patients. First, attention should be
focused on oral symptoms, such as gingival bleeding, ulcerations
and abscesses, when examining cancer patients, particularly elderly
patients. Clinical examination and past medical history should also
be carefully evaluated, utilizing a multidisciplinary approach to
differential diagnosis to ensure the most comprehensive assessment
of the patients. Most importantly, excisional biopsies and
pathological examination are invaluable for accurately diagnosing
the type of tumor, in order to optimize the efficacy of treatment
for adenocarcinomas and squamous carcinomas and improve survival
time and quality of life prior to the onset of cachexia.
Incorporating these aspects in diagnosis will assist clinical
physicians in making accurate diagnoses, ensuring a better
prognosis.
References
|
1
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Miller KD, Siegel RL, Lin CC, Mariotto AB,
Kramer JL, Rowland JH, Stein KD, Alteri R and Jemal A: Cancer
treatment and survivorship statistics, 2016. CA Cancer J Clin.
66:271–289. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gutman M and Fidler IJ: Biology of human
colon cancer metastasis. World J Surg. 19:226–234. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Riihimäki M, Hemminki A, Sundquist J and
Hemminki K: Patterns of metastasis in colon and rectal cancer. Sci
Rep. 6:297652016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Bruera G, Cannita K, Giuliante F, Baldi P
Lanfiuti, Vicentini R, Marchetti P, Nuzzo G, Antonucci A, Ficorella
C and Ricevuto E: Effectiveness of liver metastasectomies in
patients with metastatic colorectal cancer treated with FIr-B/FOx
triplet chemotherapy plus bevacizumab. Clin Colorectal Cancer.
11:119–126. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Soares AB, Thomaz LA, Duarte MT, de
Camargo de Moraes P and de Araújo VC: Metastatic adenocarcinoma of
the colon: Early manifestation in gingival tissue. Head Neck
Pathol. 5:140–143. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Amin A, Jha M and Reddy A: Lower lip
numbness in a patient with colorectal cancer. BMJ case Rep.
2011.pii:bcr0120113682. 2011.
|
|
8
|
Ukegjini K, Zadnikar M, Warschkow R,
Müller S, Schmied BM and Marti L: Baseline mortality-adjusted
survival in colon cancer patients. Langenbecks Arch Surg.
401:633–641. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Meer S and Altini M: CK7+/CK20-
immunoexpression profile is typical of salivary gland neoplasia.
Histopathology. 51:26–32. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Naylor GD, Auclair PL, Rathbun WA and Hall
EH: Metastatic adenocarcinoma of the colon presenting as
periradicular periodontal disease: A case report. Oral Surg Oral
Med Oral Pathol. 67:162–166. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nitzan DW, Livni N, Marmary Y, Ben-Baruch
N, Sela J and Catane R: The use of monoclonal anti-CEA antibody
immunohistochemistry in detecting the origin of oral cavity
metastasis. Int J Oral Maxillofac Surg. 19:162–164. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Babu KG, Raud C, Kumaraswamy SV and
Lalitha N: Carcinoma colon with mandible and liver metastases. Br J
Oral Maxillofac Surg. 34:133–134. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bentley RP and Worrall SF: Carcinoma of
the colon with mandible and liver metastases. Br J Oral Maxillofac
Surg. 35:221–222. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mason AC, Azari KK, Farkas LM, Duvvuri U
and Myers EN: Metastatic adenocarcinoma of the colon presenting as
a mass in the mandible. Head Neck. 27:729–732. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Alvarez-Alvarez C, Iglesias-Rodríguez B,
Pazo-Irazu S and Delgado-Sánchez-Gracián C: Colonic adenocarcinoma
with metastasis to the gingiva. Med Oral Patol Oral Cir Bucal.
11:E85–E87. 2006.(In English, Spanish). PubMed/NCBI
|
|
16
|
Chen HL, Chang WH, Shih SC, Pang KK and
Bair MJ: Trismus and trigeminal neuralgia in one patient with colon
cancer. J Natl Med Assoc. 100:740–742. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Favia G, Maiorano E and Lo Muzio L:
Gingival metastasis from colonic adenocarcinoma. Clin Gastroenterol
Hepatol. 8:A282010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yang RH, Chu YK and Li WY: Unusual site of
metastasis detected with FDG PET/CT in a case of recurrent
rectosigmoid cancer. Clin Nucl Med. 39:355–357. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mager LF, Wasmer MH, Rau TT and Krebs P:
Cytokine-induced modulation of colorectal cancer. Front Oncol.
6:962016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Koh SJ, Kim JM, Kim IK, Ko SH and Kim JS:
Anti-inflammatory mechanism of metformin and its effects in
intestinal inflammation and colitis-associated colon cancer. J
Gastroenterol Hepatol. 29:502–510. 2014. View Article : Google Scholar : PubMed/NCBI
|