Introduction
Mucinous cystic neoplasm (MCN) of the pancreas is
characterized by mucin-producing columnar epithelium and dense
ovarian-type stroma. The prognosis for MCNs treated with complete
surgical resection without any additional treatment is excellent,
particularly for the non-invasive type (1,2). By
contrast, anaplastic carcinoma of the pancreas has a poorer
prognosis compared with poorly differentiated ductal adenocarcinoma
of the pancreas (3–7). Anaplastic carcinoma of the pancreas is a
rare pancreatic tumor of epithelial origin, frequently presenting
various morphologies, which include pleomorphic epithelial cells
and relatively mononuclear spindle cells (3,4). MCN in
association with anaplastic carcinoma has rarely been reported to
date (3–7).
The present case study reported an unusual case of a
25-year-old female exhibiting a large pancreatic MCN with
anaplastic carcinoma. In addition, since the patient was a
Jehovah's Witness who refused blood transfusion, intraoperative
blood loss had to be minimized (8,9). To the
best of our knowledge, this is the first case report of MCN with
anaplastic carcinoma of the pancreas in a Jehovah's Witness patient
undergoing pancreatic surgery.
Case report
A 25-year-old female diagnosed with a large
abdominal cystic tumor in a referring hospital was admitted to
Kochi Medical School Hospital (Kochi, Japan). Although the past
medical history of the patient was not notable, the patient was a
Jehovah's Witness and therefore refused blood transfusions.
Physical examination suggested the presence of an elastic hard mass
in the left upper quadrant of the abdomen. Laboratory tests on
admission revealed anemia (hemoglobin, 10.8 g/dl; hematocrit,
33.8%) and a marginal elevation in the white blood cell count
(9,400/µl). Although cancer antigen (CA)19-9 levels were normal,
CA125 and detection of a pancreatic cancer-associated antigen-2
levels were elevated (178 and 710 U/ml, respectively; normal <35
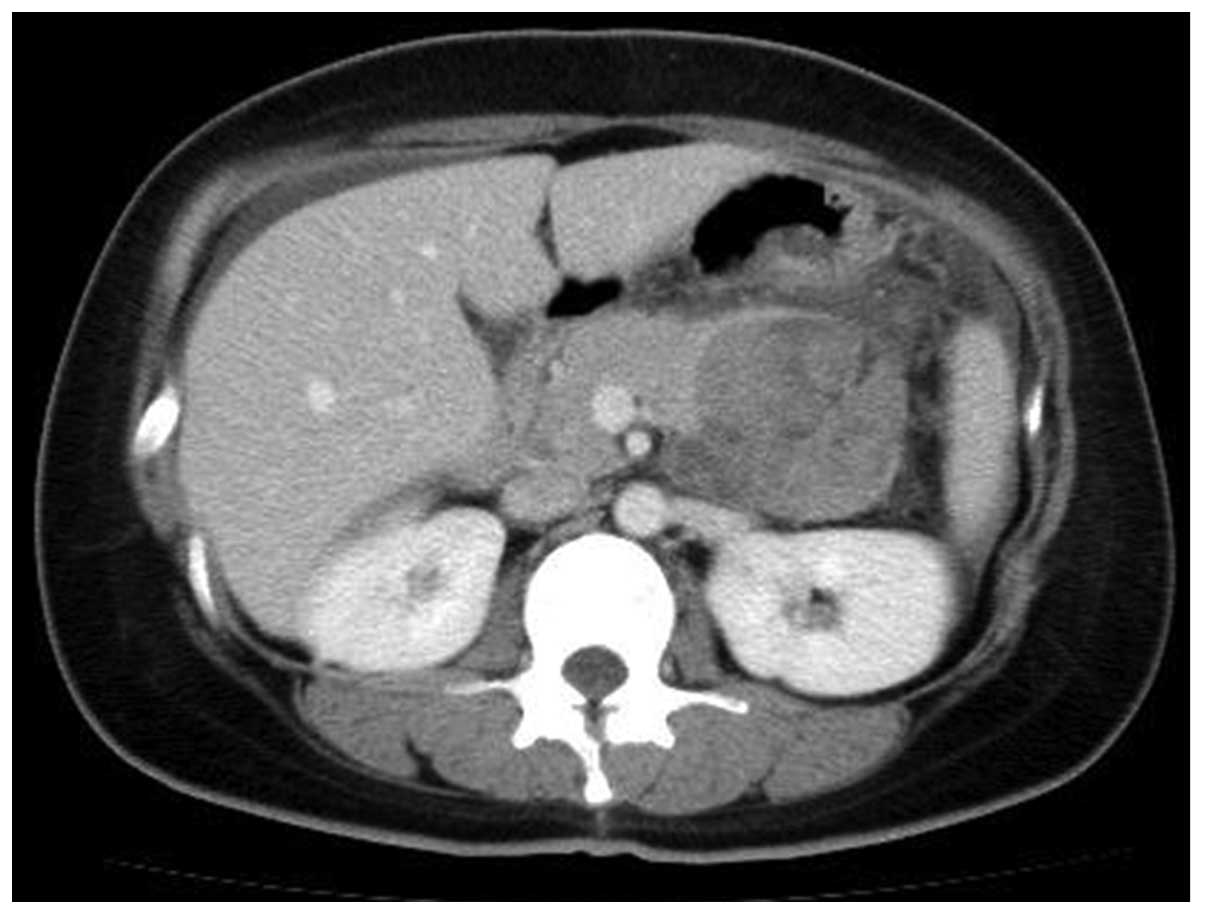
U/ml each). Abdominal computed tomography (CT) revealed a large
complex cystic and solid mass measuring 10×12.5 cm in the body and
tail of the pancreas with a thick capsule (Fig. 1) and ascites in the pouch of Douglas.
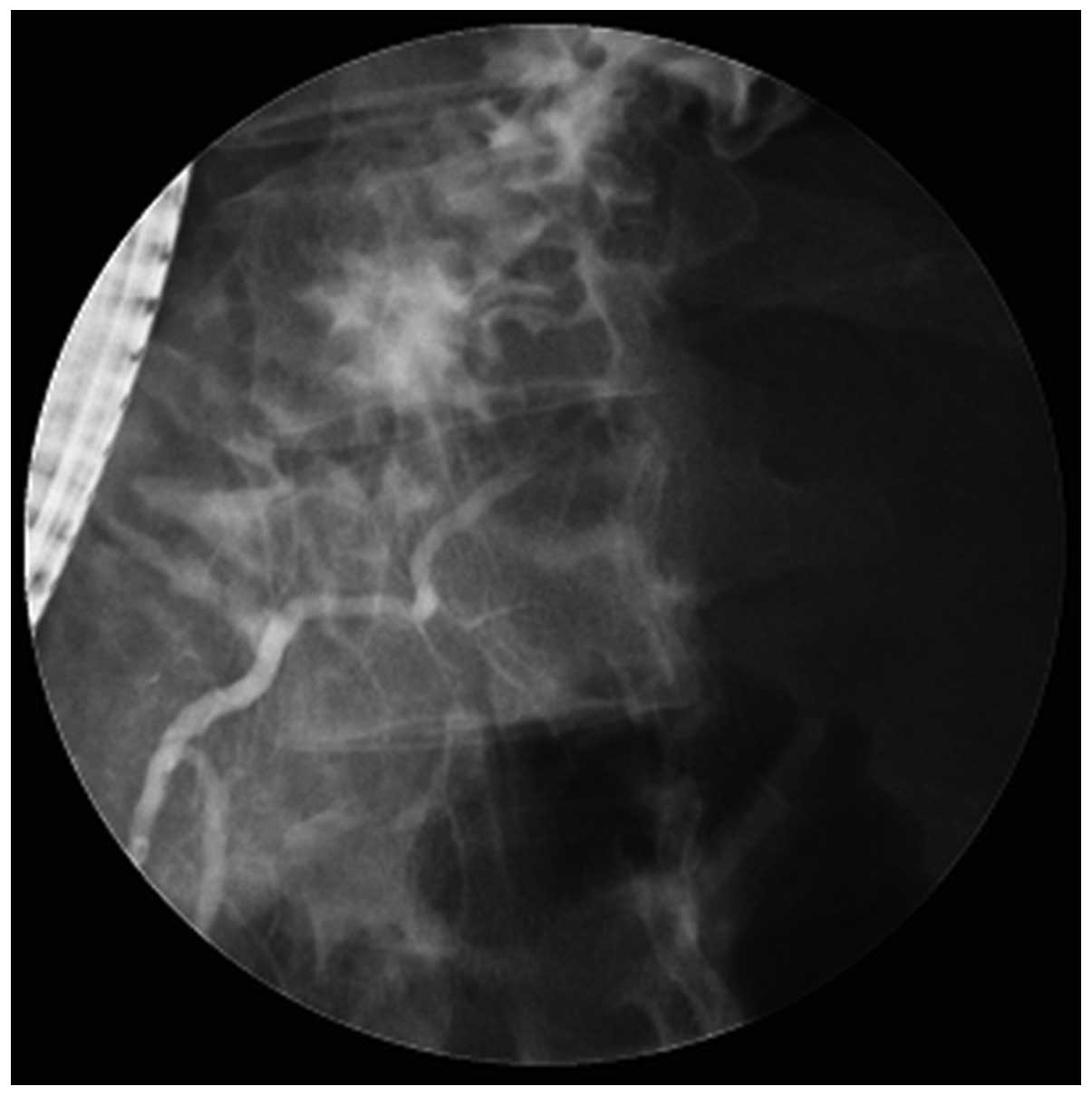
Endoscopic retrograde cholangiopancreatography revealed disruption
of the major pancreatic duct, the duct of Wirsung, in the body of
the pancreas (Fig. 2).
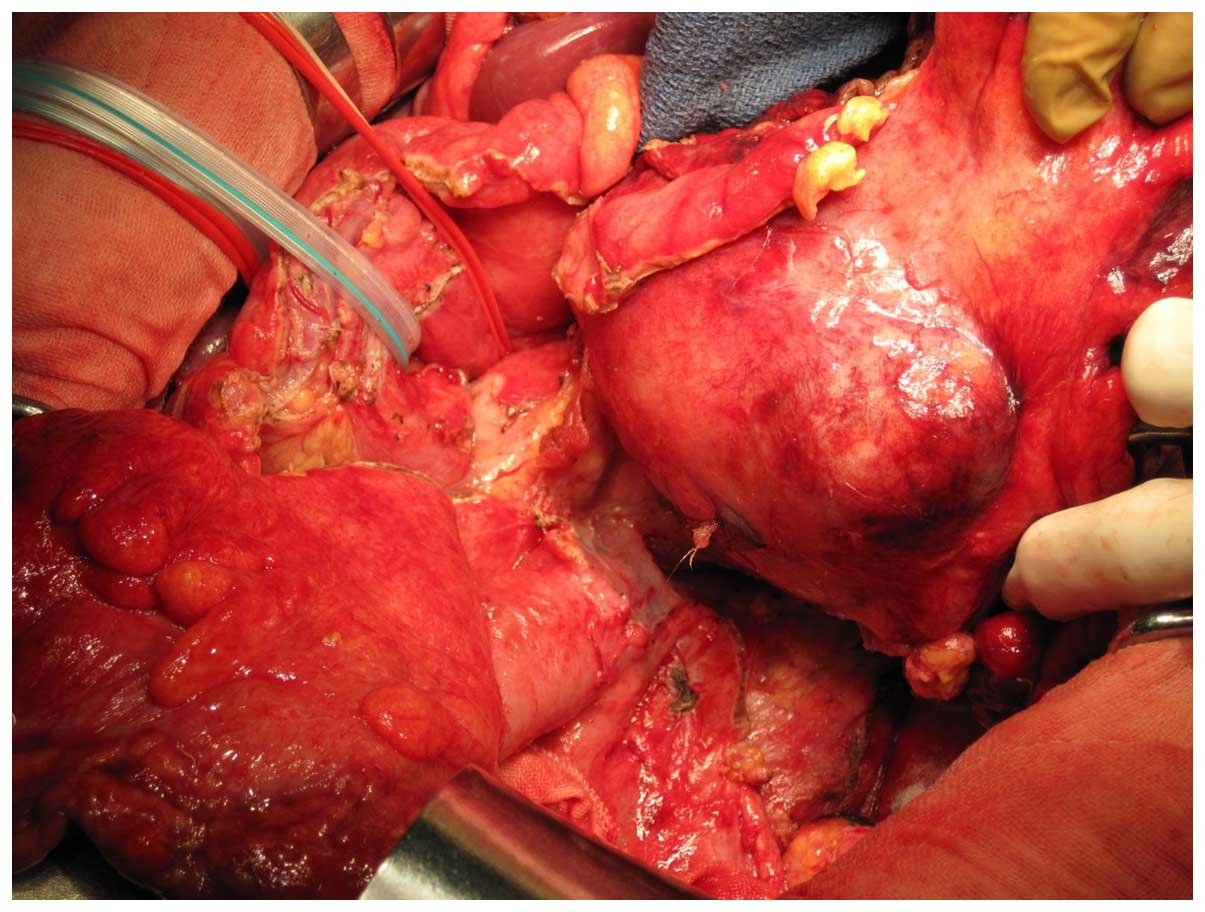
A laparotomy was subsequently performed. No evidence
of distant or systemic metastases were observed. The present study
investigated cytology for ascites during the operation, which was
negative for neoplastic cells. En bloc distal pancreatectomy with
lymphadenectomy, splenectomy and partial resection of the
transverse colon was performed (Fig.
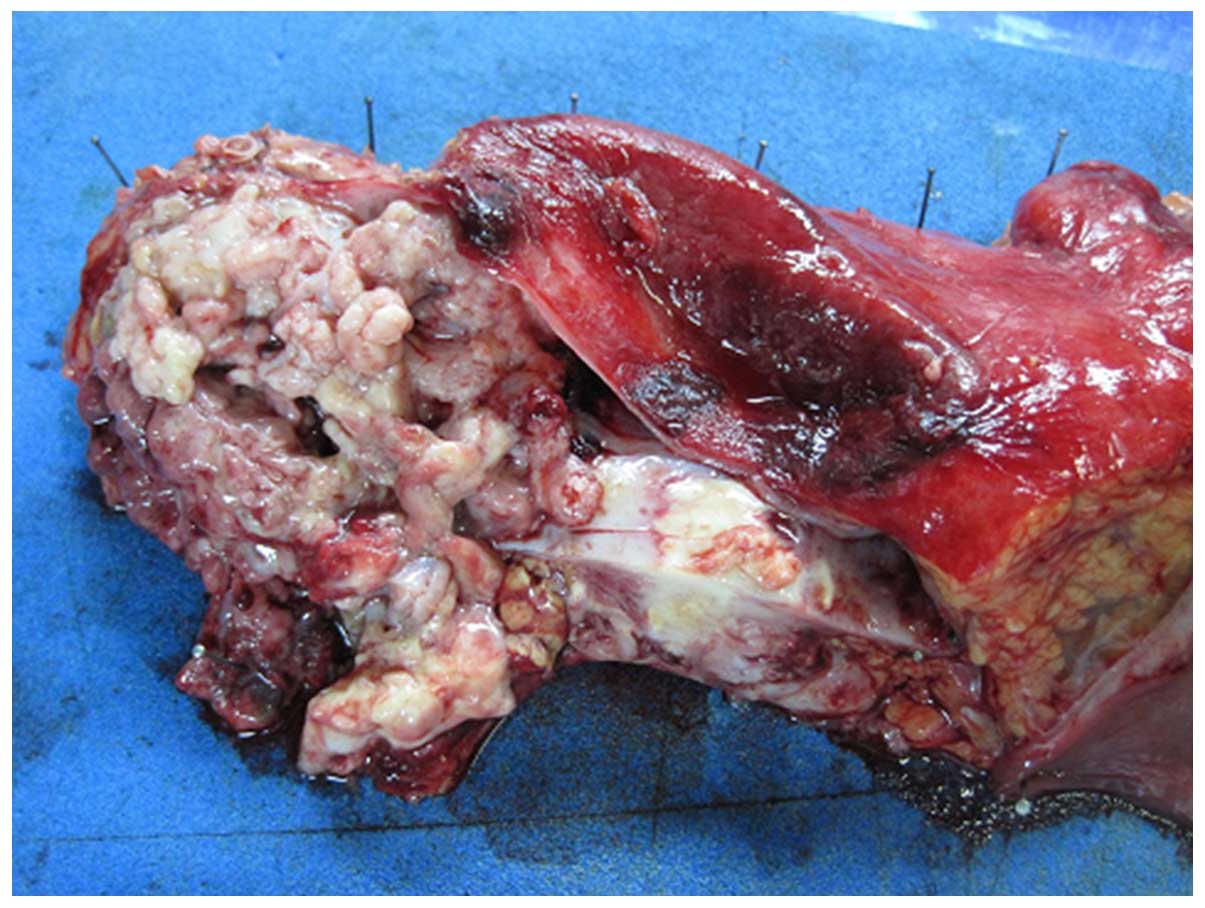
3). The cut surface of the cystic mass exhibited a smooth
external surface, and it was filled with mucinous fluid and a solid
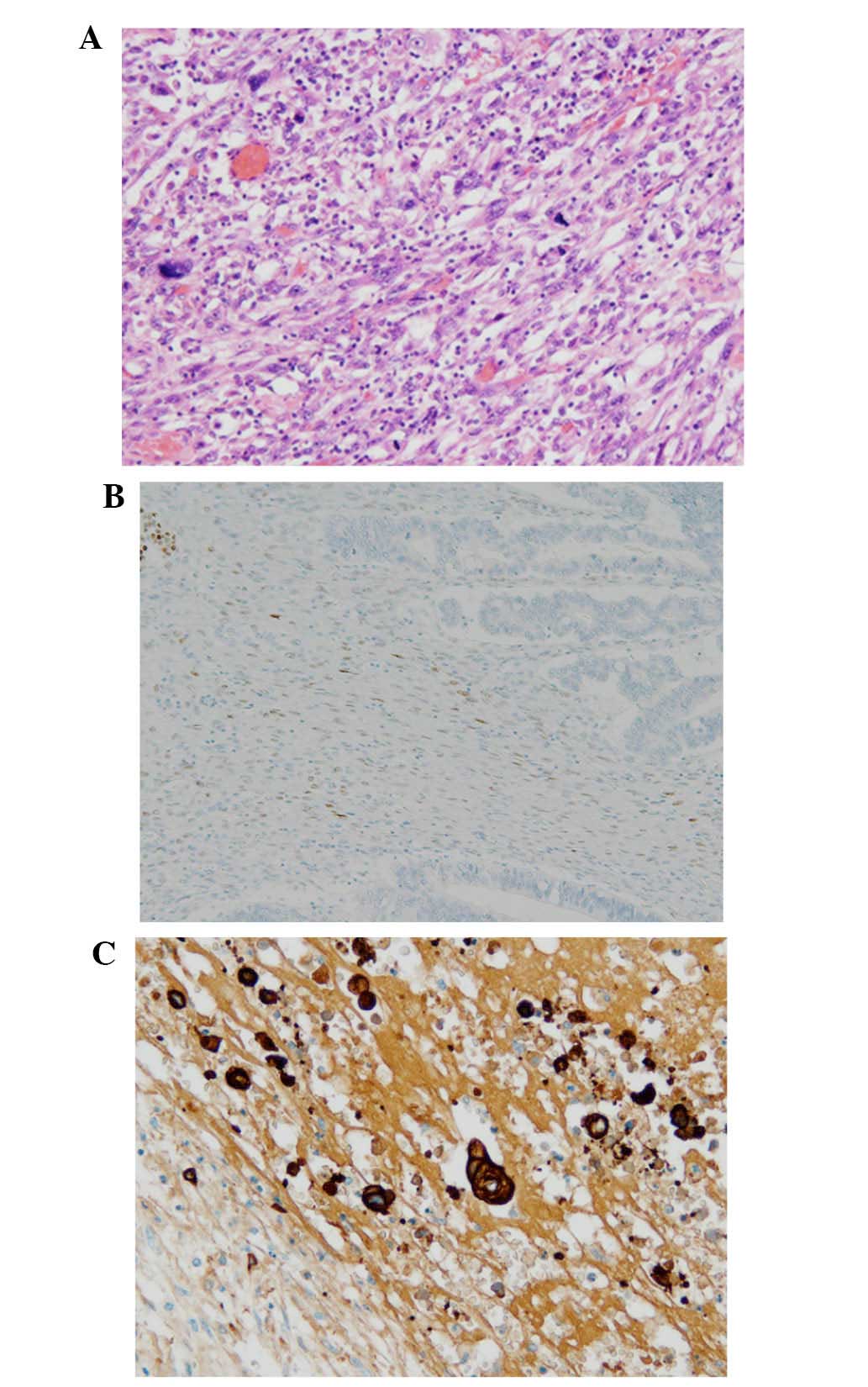
component (Fig. 4). Histopathological
analysis revealed MCN compatible with ovarian-type stromal tissue
(Fig. 5A). Immunohistochemical
analysis revealed positive staining for progesterone receptor in
stromal cell nuclei (Fig. 5B). In
addition, anaplastic carcinoma was suggested since the spindle and
pleomorphic tumor cells stained positive for cytokeratin AE1/AE3
and vimentin in the solid area of the tumor (Fig. 5C). The pathological diagnosis was
mucinous cystadenocarcinoma of the pancreas with anaplastic
carcinoma, which penetrated the serosa without lymphovenous and
retroperitoneal invasion. The mass was pT3N0M0 Stage III, according
to the General Rules for the Study of Pancreatic Cancer edited by
the Japan Pancreas Society (10).
The postoperative course was uneventful and the
patient was discharged ~1 month following surgery. Following
discharge, the patient underwent postoperative chemotherapy
consisting of gemcitabine (1,000 mg/m2) + TS-1 (100
mg/m2). During chemotherapy, the patient was performing
well, enjoying life, and was able to undertake light sports and
trips without any trouble. Unfortunately, recurrence (peritoneal
dissemination) was detected by follow-up CT 20 months following
surgery. Following detection of the recurrence, the patient was
treated with chemoradiotherapy and subsequently palliative care at
the hospital in her home town. The patient succumbed to pancreatic
cancer 32 months following the surgery.
Discussion
Reports of MCN with anaplastic carcinoma of the
pancreas are rare. To the best of our knowledge, only six cases
(3–7)
have been reported to date, including the present case (Table I). No previous patients have been a
Jehovah's Witness. The prognosis for MCN is reasonably good, with a
postoperative 5-year survival rate of almost 100% for adenoma,
non-invasive and in situ carcinoma, and 30–60% for invasive
carcinoma (2). A multi-institute
study in Japan reported a 5-year survival rate for MCN following
resection of 100% in the case of adenoma to minimally invasive
carcinoma, and 37.5% in the case of invasive carcinoma (1). By contrast, anaplastic carcinoma of the
pancreas is a rare, aggressive tumor. It accounts for 2–7% of all
pancreatic cancer types and has a male preponderance (2).
 | Table I.Previous reports of mucinous
cystadenocarcinoma with anaplastic carcinoma of the pancreas. |
Table I.
Previous reports of mucinous
cystadenocarcinoma with anaplastic carcinoma of the pancreas.
| Author | Year | Age/gender | Tumor location | Size (cm) | Spindle cell | Giant cell | Direct invasion | Lymphatic
invasion | Distant
metastasis | Surgery | Outcome |
|---|
| Logan et al
(5) | 1982 | 35/F | Body-tail | 17 | + | ND | Stomach | ND | Liver | DP + Splenectomy,
Gastric resection | Dead (1–2
months) |
| Marinoho et al
(6) | 1995 | 70/F | Body-tail | 4.5 | ND | ND | Capsule | − | − | DP + Splenectomy | ND |
| Lane et al
(7) | 1997 | 25/F | Tail, liver, lymph
node | 15 | + | − | − | + | Liver | DP + Splenectomy,
Segmental liver resection, retroperitoneal LN resection | ND |
| Pan et al
(4) | 2007 | 70/F | Body-tail | 10.4 | + | + | − | ND | − | DP + Splenectomy | ND |
| Hakamada et al
(3) | 2008 | 39/F | Tail | 5 | + | + | − | − | − | Partial
Pancreatectomy, Partial Gastrectomy, Left adrenalectomy | Alive (4 years) |
| Present case | 2015 | 25/F | Tail | 12.5 | + | − | Transverse colon | − | − | DP + Splenectomy,
Transvers colectomy | Dead (2 years 8
months) |
It is difficult to determine any differences in
imaging modalities between MCN and MCN with anaplastic carcinoma,
since this diagnosis was confirmed by the immunohistochemical
features of epithelial components pathologically (3,4). However,
it is important to recognize this distinct entity, which is an
aggressive neoplasm with a poorer prognosis compared with poorly
differentiated ductal adenocarcinoma of the pancreas (4). The prognosis of pancreatic anaplastic
carcinoma is extremely poor since, in most cases, the tumor not
only has areas of adenocarcinoma, but also mesenchymal components,
including spindle-shaped cells and osteoclastoid giant cells,
reminiscent of sarcomatous differentiation (3,4). Notably,
no previous reports demonstrates any patients surviving >5 years
following surgery, including the present case (Table I). Until now, the longest reported
survival following surgery was 4 years (3).
Konstantinidis et al (9) reported a median estimated blood loss of
400 ml for 10 pancreatic resections (six pancreaticoduodenectomy,
four distal pancreatectomy/splenectomy; range 250–1,800 ml). In the
present case, the estimated blood loss was 400 ml, which is
comparable with previous reports. Generally, if Jehovah's Witness
patients undergoing pancreatectomy experience massive blood loss,
they are administered erythropoietin and iron hydroxide sucrose
complex. Fortunately, the present patient did not require treatment
for anemia since no change in postoperative hemoglobin and
hematocrit was observed compared with the preoperative levels.
Previously, the Liga Sure™ (COVIDIEN) vessel-sealing system was
used to reduce intraoperative blood loss during proximal and/or
distal pancreatectomy (11), and this
system was used in the present patient. Regardless, in the case of
Jehovah's Witness patients undergoing pancreatic resection,
surgical outcome can be enhanced by good interdepartmental
cooperation, careful patient selection and appropriate preoperative
management.
A previous report suggested that lymph node
metastasis occurred in 58% of surgical patients with invasive MCN
(2). Therefore, pancreatic resection
and standard lymphadenectomy (D1 or D2) against invasive MCN of the
pancreas may be required. In addition, this entity is observed
predominantly in younger female patients and is located in the body
and/or tail of pancreas (1,2), as observed in the current patient. The
present case was further treated not only with intraoperative
radiotherapy, but also postoperative chemotherapy for 20 months
until recurrence was detected, and subsequently with
chemoradiotherapy. The chemotherapy regimen in the present case was
a combination chemotherapy with gemcitabine and S-1, one of the
standard chemotherapeutic regimens for advanced pancreatic cancer
(12).
The present case highlighted the management of MCN
with anaplastic carcinoma of the pancreas in a Jehovah's Witness
patient undergoing pancreatic surgery. Additional reports of this
entity are required to optimize the standard management for this
uncommon disease.
References
|
1
|
Suzuki Y, Atomi Y, Sugiyama M, Isaji S,
Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J,
et al: Cystic neoplasm of the pancreas: A Japanes
multi-institutional study of intraductal papillary mucinous tumor
and mucinous cystic tumor. Pancreas. 28:241–246. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sugiyama M, Suzuki Y, Abe N and Atomi Y:
Surgical treatment of pancreatic cystic neoplasms. Nihon Shokakibyo
Gakkai Zasshi. 101:865–871. 2004.(In Japanese). PubMed/NCBI
|
|
3
|
Hakamada K, Miura T, Kimura A, Nara M,
Toyoki Y, Narumi S and Sasak M: Anaplastic carcinoma associated
with a mucinous cystic neoplasm of the pancreas during pregnancy:
Report of a case and a review of the literature. World J
Gastroenterol. 14:132–135. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pan Z and Wang B: Anaplastic carcinoma of
the pancreas associated with a mucinous cystic adenocarcinoma. A
case report and review of the literature. JOP. 8:775–782.
2007.PubMed/NCBI
|
|
5
|
Logan SE, Voet RL and Tompkins RK: The
malignant potential of mucinous cysts of the pancreas. West J Med.
136:157–162. 1982.PubMed/NCBI
|
|
6
|
Marinho A, Nogueira R, Schmitt F and
Sobrinho-Simoes M: Pancreatic mucinous cystadenocarcinoma with a
mural nodule of anaplastic carcinoma. Hispathology. 26:284–287.
1995.
|
|
7
|
Lane RB Jr and Sangüeza OP: Anaplastic
carcinoma occurring in association with a mucinous cystic neoplasm
of the pancreas. Arch Pathol Lab Med. 121:533–535. 1997.PubMed/NCBI
|
|
8
|
Jeon YB, Yun S and Choi D: Transfusion
free radical antegrade modular pancreaticoduodenectomy of
metastatic neuroendocrine tumor of the pancreas in Jehovah's
Witness patient. Ann Surg Treat Res. 88:106–110. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Konstantinidis IT, Allen PJ, D'Angelica
MI, DeMatteo RP, Fischer ME, Grant F, Fong Y, Kingham TP and
Jarnagin WR: Pancreas and liver resection in Jehovah's Witness
patient: Feasible and safe. J Am Coll Surg. 217:1101–1107. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Japan Pancreas Society (eds):
Classification of Pancreatic Carcinoma (3rd). Tokyo: Kanehara &
Co., Ltd. 2011.
|
|
11
|
Piccini G, Pasculli A, D'Ambrosio E,
Gurrado A, Lissidini G and Testini M: Retrospective comparison of
traditional vs. Liga Sure impact dissection during
pancreatoduodenectomy: How to save money by using an expensive
device. Surg Technol Int. 23:88–93. 2013.PubMed/NCBI
|
|
12
|
Li Y, Jiang Z, Zhang L and Liu G:
Gemcitabine and S-1 combination therapy versus gemcitabine alone
for locally advanced and metastatic pancreatic cancer: A
meta-analysis of randomized controlled trials in Asia. J Chemother.
27:227–234. 2015. View Article : Google Scholar : PubMed/NCBI
|