Introduction
Numerous previous studies have investigated the
clinicopathological characteristics of early colorectal cancer
types. As a result, a consensus is forming in regards to the
clinical treatment of T1 cancer types (1–3). According
to the Colorectal Cancer Treatment guidelines, T1 colorectal cancer
types are recommended for endoscopic treatment if they are
papillary adenocarcinoma or tubular adenocarcinoma with a vertical
invasion of ≤1,000 µm and without any lymphovascular invasion
(3).
T2 cancer types, which invade deeper layers as
compared with T1 cancer types, are considered an early stage of
advanced cancer. T2 cancer types are considered to be the
developmental transition from early to advanced cancer. Although
several retrospective studies on the association between morphology
and tumor characteristics of T2 colorectal cancer types have been
performed in Japan, there remains no consensus on the subject
(4–8).
This may be due to advanced cancer types exhibiting highly modified
morphologies as compared with early cancer types.
Nevertheless, numerous lesions are thought to
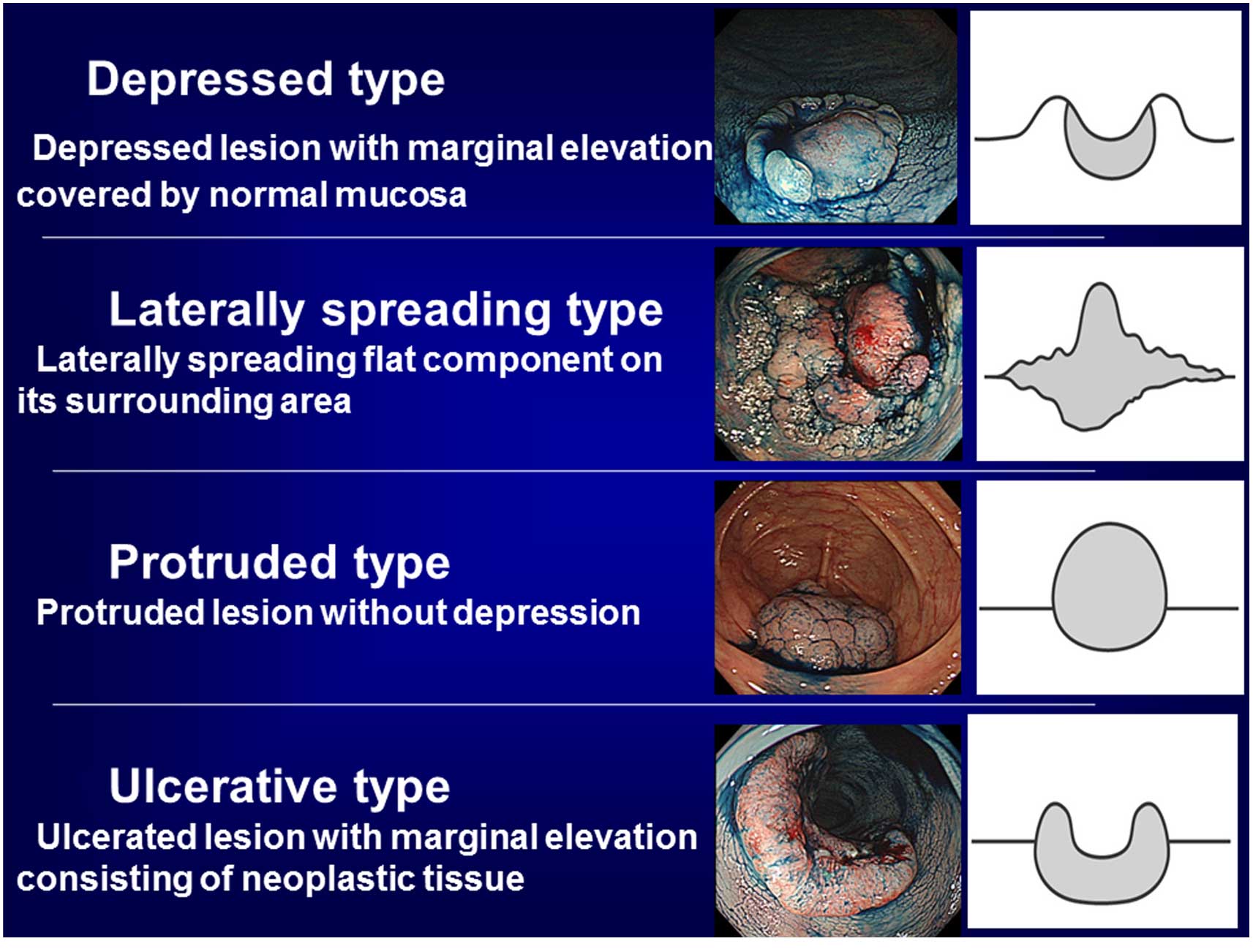
clearly derive from depressed type early cancer (Fig. 1). The present study proposed novel
morphological categories for T2 colorectal cancer types, based on
the growth and development route. The primary aim of the present
study was to clarify the association between morphology and
malignant potential of T2 colorectal cancer types.
Patients and methods
Patients
The present study included 195 patients (195
lesions) with T2 colorectal cancer who underwent surgical resection
at Showa University Northern Yokohama Hospital (Yokohama, Japan)
between April 2001 and April 2009. The present study
retrospectively analyzed the association between morphology and
clinicopathological factors. The present study was approved by the
Ethics Committee of Showa University Northern Yokohama Hospital
(Yokohama, Japan).
Groups and assessments
Preliminary categories were created for T2 cancer
morphology, based on growth and development route. These were as
follows: group A, depressed type; group B, laterally spreading
type; group C, protruded type; group D, ulcerative type (Fig. 1). The morphologies containing
depressed areas on the surfaces were divided into two groups
(groups A and D). In other words, those lesions with some normal
mucosa remaining in the margins of the depression were assigned to
the group A, which was considered to be derived from depressed-type
T1 cancer. Those with neoplastic mucosa around the entire
circumference of the depression were assigned to the group D).
Group B included laterally spreading flat component on its
surrounding area, which was considered to be derived from laterally
spreading type early T1 cancer. Group C included protruded type
lesions that had purely protruded morphology without depression.
The present study retrospectively investigated the association
between these morphological classifications and tumor size,
lymphovascular invasion, lymph node metastasis and distant
metastasis.
Statistical analysis
The data were statistically analyzed using the
χ2 test as a test of independence and the Mann-Whitney
test for comparing the mean values of the two groups. R software
(version 2.10.0; https://www.r-project.org/) was used for statistical
analyses. In consideration of effects induced by multiple
comparison, P<0.0125 was considered to indicate a statistically
significant difference by using Bonferroni's correction.
Results
Detailed description of the cases
Of the 195 patients, 48 exhibited lymph node
metastasis and 4 were positive for distal metastasis at the time of
resection, accounting for 24.6 and 2.1% of the total number of
cases, respectively. The number of cases in each classification
included: Group A, 73 (37.4%); group B, 26 (13.3%); group C, 24
(12.3%); group D, 72 (36.9%) (Table
I).
 | Table I.Number of patient lesions and tumor
diameter of each morphological type. |
Table I.
Number of patient lesions and tumor
diameter of each morphological type.
| Morphology | No. patients (%) | Tumor diameter |
|---|
| Depressed type | 73 (37.5) |
22.7±9.5
mm |
| Laterally spreading
type | 26 (13.3) |
51.2±22.6
mm |
| Protruded type | 24 (12.3) |
29.9±8.7
mm |
| Ulcerative type | 72 (36.9) |
36.3±11.3
mm |
Association between T2 cancer
morphology and tumor size
The mean tumor sizes were as follows: Group A,
22.7±9.5; group B, 51.2±22.6; group C, 29.9±8.7; group D, 36.3±11.3
mm (Table I). Depressed type T2
cancers were of a significantly smaller tumor size compared with
the other types (P<0.01).
Association between T2 cancer
morphology and vascular invasion
The positive rates for lymphatic invasion were as
follows: Group A 68.5; group B, 53.8; group C 58.3; group D, 48.6%
(Table II). Depressed type T2
cancers exhibited higher positive rates for lymphatic invasion
compared with the other types (P=0.0333).
 | Table II.Lymphatic invasion and venous invasion
of each morphological type. |
Table II.
Lymphatic invasion and venous invasion
of each morphological type.
|
| No. patients (%) |
|---|
|
|
|
|---|
| Morphology | Lymphatic
invasion | Venous invasion |
|---|
| Depressed type
(n=73) | 50 (68.5) | 54 (74.0) |
| Laterally spreading
type (n=26) | 14 (53.8) | 12 (46.2) |
| Protruded type
(n=24) | 14 (58.3) | 8
(33.3) |
| Ulcerative type
(n=72) | 35 (48.6) | 41 (56.9) |
The positive rates for venous invasion were as
follows: Group A 74.0; group B 46.2; group C, 33.3; group D, 56.9%
(Table II). Depressed type T2
cancers had significantly higher positive rates for venous invasion
compared with the other types (P=0.0019).
Association between T2 cancer
morphology and lymph node metastasis/distant metastasis
The positive rates for lymph node metastasis were as
follows: Group A, 26.0; group B, 30.8; group C, 25.0; group D,
22.2% (Table III). No significant
differences were observed between the four morphological
classifications.
 | Table III.Lymph node metastasis and distant
metastasis of each morphological type. |
Table III.
Lymph node metastasis and distant
metastasis of each morphological type.
|
| No. patients (%) |
|---|
|
|
|
|---|
| Morphology | Lymph node
metastasis | Distant
metastasis |
|---|
| Depressed type
(n=73) | 19 (26.0) | 1 (1.4) |
| Laterally spreading
type (n=26) | 8
(30.8) | 0 (0.0) |
| Protruded type
(n=24) | 6
(25.0) | 0 (0.0) |
| Ulcerative type
(n=72) | 16 (22.2) | 3 (4.2) |
The positive rates for synchronous distant
metastasis were as follows: Group A, 1.4; group B, 0; group C, 0;
group D, 4.2% (Table III). No
significant differences were observed between the groups for
distant metastasis.
Discussion
The present study proposed novel morphological
classifications of T2 colorectal cancer with reference to growth
and development route, and subsequently investigated their
respective features.
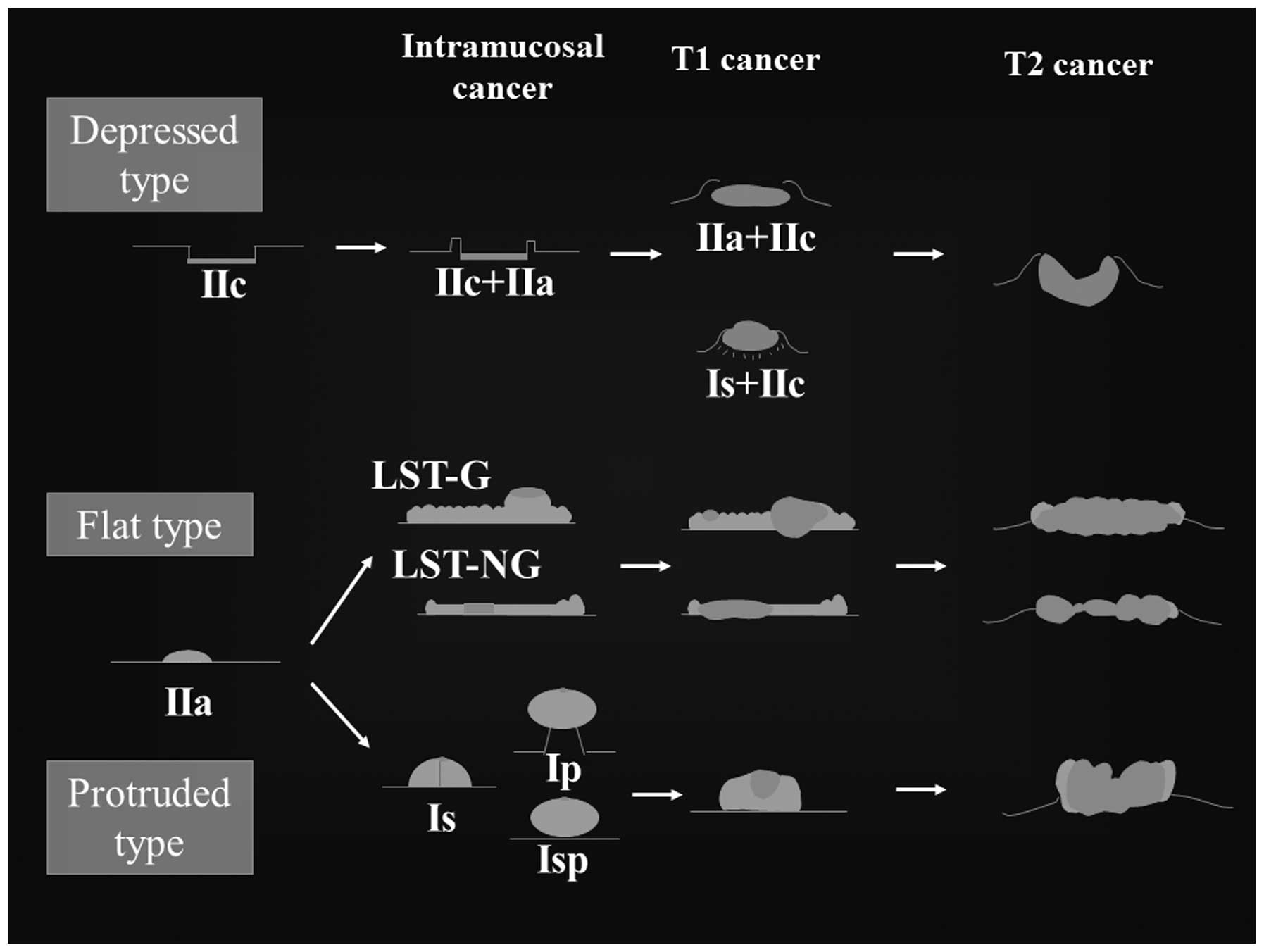
Since numerous previous studies have investigated
the growth and development route of T1 stage cancer, a consensus is
forming on this issue (1,2,9,10). Growth and development classifications
for depressed, flat and protruded types were constructed based on
their various morphologies (Fig. 2).
By acontrast, several previous studies on T2 cancer types have been
previously performed (4–8); however, limited debate on this topic has
occurred compared with that of T1 cancer types.
The morphologies containing depressed areas on tumor
surfaces were dominant among T2-T4 cancer types, thus in the
clinical setting they were conventionally treated as an identical
morphology, often termed ‘Bormann type 2’ cancers in Japan.
However, biological difference among the ‘Bormann type 2’ cancers
were considered to exist, thus, several morphological
classifications were proposed by Japan and the west. George et
al (5) classified T2 cancers into
polypoid and non-polypoid types based on whether the marginal
mucosa is elevated or not. This resulted in 45% of tumors being
classified as polypoid, half of which included adenomatous
components within the lesions, and 48% were classified as
non-polypoid, which rarely included adenomatous components. The
remaining 7% included morphologies that exhibited both polypoid and
non-polypoid characteristics. Non-polypoid tumor types often
exhibited wild-type K-ras and had a significantly higher rate of
postoperative recurrence compared with polypoid tumors, which
suggested that non-polypoid tumors were more malignant. In a
previous study of T2 colorectal cancer tumor types ≤2 cm, Goi et
al (6) reported that 63% of
small, advanced colorectal cancer types were non-polypoid, while
~25% of normal advanced tumors of ≥2 cm were non-polypoid tumors.
The non-polypoid vs. polypoid classifications used by these
researchers assumed that non-polypoid lesions were associated with
the de novo cancer route (10)
and that polypoid lesions were associated with the carcinogenic
route that followed the adenoma-carcinoma sequence (9). Nevertheless, since these classification
systems were focused on remnant intramucosal lesions, certain
researchers may feel they should be restricted to use on
early-stage cancer types. Another problem is that these
non-polypoid vs. polypoid classifications were based on resected
pathological specimens, thus, it cannot be used for treatment
determination.
In consideration of these problems, the present
study classified tumor types focusing on growth and development
route based on preoperative endoscopic findings. Specifically, the
laterally spreading and protruded types of lesions were firstly
classified as groups B and C, respectively, because each were
clearly derived from laterally spreading type and protruded type
early lesions. The remaining depressed and ulcerative types of
lesions were classified based on whether the margins have normal
mucosal tissue or not. Depressed type lesions, which are thought to
be de novo cancer-derived, were placed into their own
category.
Of all the types in the present classification
system, depressed type T2 cancer showed characteristic
clinicopathological features. They exhibited a significantly
smaller tumor size and higher incidence of lymphovascular invasion.
These features have extremely strong resemblance to the
clinicopathological features of depressed type T1 cancer (1,2). However,
no significant differences were observed in terms of lymph node
metastasis and distant metastasis. This may be a result of the fact
that positive rates for T2 cancer lymph node metastasis and distant
metastasis were relatively low at 25.0 and 3.2%, respectively.
Therefore, this issue requires further study with a larger number
of cases for analysis.
In conclusion, compared with the other types,
depressed type T2 cancer exhibited a smaller tumor size, higher
rate of lymphatic involvement and venous involvement, which
suggested a more malignant nature of these lesions.
References
|
1
|
Kudo SE, Takemura O and Ohtsuka K: Flat
and depressed types of early colorectal cancers: From East to West.
Gastrointest Endosc Clin N Am. 18:581–593. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kudo Se, Lambert R, Allen JI, Fujii H,
Fujii T, Kashida H, Matsuda T, Mori M, Saito H, Shimoda T, et al:
Nonpolypoid neoplastic lesions of the colorectal mucosa.
Gastrointest Endosc. 68(4 Suppl): S3–S47. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Watanabe T, Itabashi M, Shimada Y, Tanaka
S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, et
al: Japanese society for cancer of the colon and rectum (JSCCR)
guidelines 2014 for treatment of colorectal cancer. Int J Clin
Oncol. 20:207–239. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Adachi, Yasuda, Kakisako, Sato, Shiraishi
and Kitano: Histopathologic characteristics of advanced colorectal
cancer smaller than 2 cm in size. Colorectal Dis. 1:19–22. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
George SM, Mäkinen MJ, Jernvall P, Mäkelä
J, Vihko P and Karttunen TJ: Classification of advanced colorectal
carcinomas by tumor edge morphology: Evidence for different
pathogenesis and significance of polypoid and nonpolypoid tumors.
Cancer. 89:1901–1909. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Goi T, Kawasaki M, Hirono Y, Katayama K
and Yamaguchi A: Clinicopathological analysis of invading
muscularis propria (T2) cancers < or=20 mm in diameter. Int
Surg. 93:1–5. 2008.PubMed/NCBI
|
|
7
|
Miyamoto S, Boku N, Fujii T, Ohtsu A,
Matsumoto S, Tajiri H, Yoshida S, Arai T, Ono M, Hasebe T and
Ochiai A: Macroscopic typing with wall stricture sign may reflect
tumor behaviors of advanced colorectal cancers. J Gastroenterol.
36:158–165. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhang H, Chen CS, Cong JC, Qiao L,
Hasegawa T and Takashima S: Clinicopathological characteristics of
advanced colorectal cancer 30 mm or smaller in diameter. Chin Med
Sci J. 22:98–103. 2007.PubMed/NCBI
|
|
9
|
Morson BC: Precancerous and early
malignant lesions of the large intestine. Br J Surg. 55:725–731.
1968. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shimoda T, Ikegami M, Fujisaki J, Matsui
T, Aizawa S and Ishikawa E: Early colorectal carcinoma with special
reference to its development de novo. Cancer. 64:1138–1146. 1989.
View Article : Google Scholar : PubMed/NCBI
|