Introduction
Age is now widely accepted as the greatest single
risk factor for developing bladder cancer. Bladder cancer is
primarily considered a disease of the elderly due to the close link
between age and incidence of bladder cancer (1). Treatment decisions in elderly patients
may sometimes be challenging, as elderly patients are
physiologically, psychologically and socially different from
younger patients.
The main symptoms of invasive bladder cancer are
irritative voiding symptoms, lower abdominal pain, gross hematuria,
resulting in anemia and urinary retention. Locally advanced tumors
may be accompanied by several debilitating symptoms, including
bleeding, pain, dysuria and urinary obstruction (2,3).
Although radical cystectomy is the standard treatment for localized
muscle-invasive bladder cancer, chemotherapy is indicated for
patients with advanced or metastatic bladder cancer, who are not
candidates for surgery. However, the chemotherapy regimens are
toxic and difficult to administer to elderly patients with a World
Health Organization performance status 3 or 4, with or without
additional negative prognostic factors. The most appropriate
approach for such patients is best supportive care; they may also
be candidates for palliative treatment.
Occasionally, urinary diversion should be used,
depending on the clinical condition of the patient.
Ureterocutaneostomy is a urinary diverting procedure suitable for
obstructive uropathy in patients with advanced pelvic malignancy,
and is a less invasive approach for such poor-risk patients
requiring palliation (4,5). However, there have been fewer studies
on ureterocutaneostomy for elderly patients. The present study
reports a case of a very elderly patient with locally advanced
bladder cancer that was refractory to medical management of severe
irritative voiding symptoms, and was found be highly responsive to
palliative urinary diversion by retroperitoneoscopic
ureterocutaneostomy.
Case report
An 89-year-old male visited a local hospital with
the chief complaint of gross hematuria and voiding difficulty. The
patient had no past medical history and was not taking any
anticoagulants. Computed tomography of the abdomen and pelvis
showed a tumor on the right wall of the bladder and a right
hydronephrotic atrophic kidney caused by tumor obstruction. The
serum creatinine level was elevated to 1.44 mg/dl (normal range,
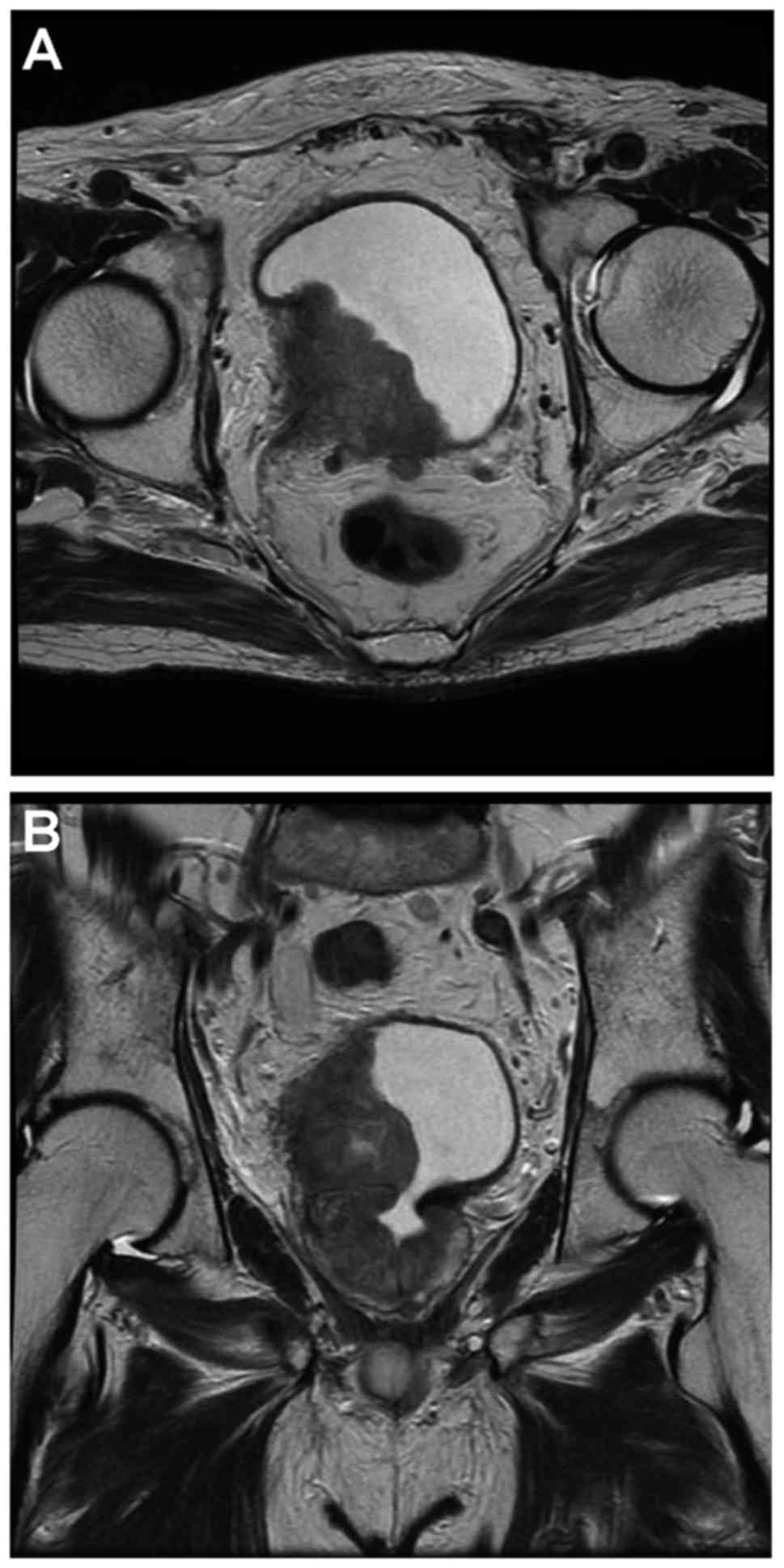
0.43–1.08 mg/dl) (Fig. 1). Magnetic
resonance imaging showed that the bladder tumor was invading the
perivesical tissue macroscopically (Fig.
2). The patient was referred to Saitama Medical University
International Medical Center (Saitama, Japan) for treatment.
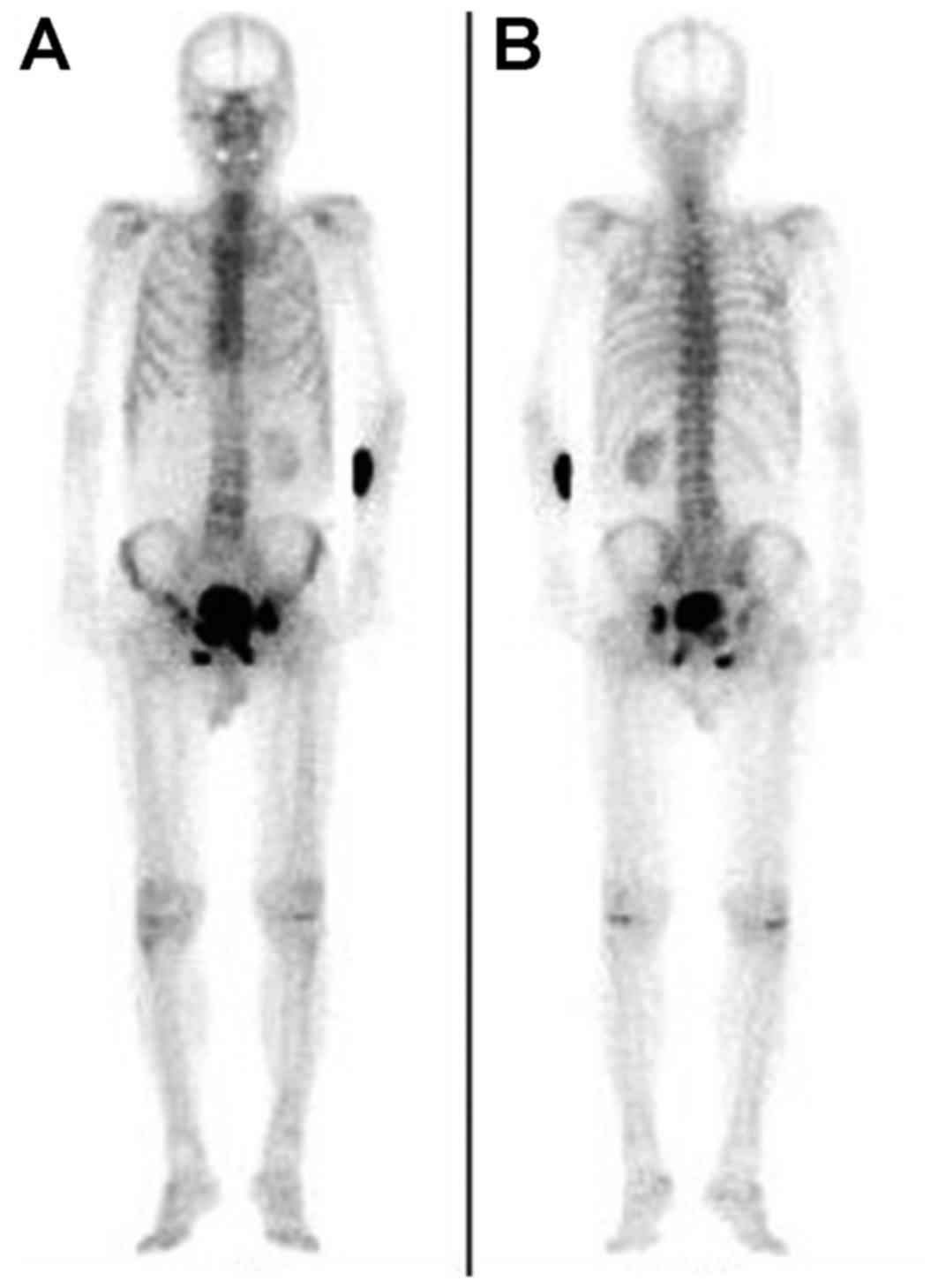
Bone scintigraphy revealed multiple bone metastases
in the ilium, pubis and ischium (Fig.
3). Curative radical cystectomy was not indicated in this case,
as distant metastases were present. The patient was elderly and did
not have a good performance status, therefore neither cystectomy
for palliation or chemotherapy was indicated. Palliative left
retroperitoneoscopic ureterocutaneostomy was performed to improve
renal function and relieve tumor bleeding without chemotherapy.
The surgery lasted 144 min and blood loss was kept
to a minimum; a drain was left in place for 72 h. A 7 FR ureteral
stent was placed to prevent an anastomotic stricture. The patient
started to walk and eat on the first postoperative day without
postoperative delirium. The serum creatinine level was 1.37 mg/dl
on the 7th postoperative day; it remained similar to the
preoperative level. The patient required a prescription for 12.5
µg/h fentanyl patches for severe pain in the right buttock and
thigh regions. Intensity-modulated radiotherapy of 30 Gy in 10
fractions was administered 9 days after the surgery, to control
tumor bleeding. After completing 8 days of radiotherapy, the
patient was discharged from hospital.
Following discharge, the patient was able to spend
the remainder of his life with no signs of either postrenal failure
or gross hematuria. The pain control was adequate with fentanyl
patches. The patient died due to progressive disease 7 months after
the operation.
Discussion
The present case illustrated that urinary diversion
by retroperitoneoscopic ureterocutaneostomy as a palliative
treatment for a very elderly patient with invasive bladder cancer
patient poor performance status was able to alleviate gross
hematuria and voiding difficulty and to avoid possible
complications due to progressive disease such as uncontrolled
hematuria, urinary retention and postrenal failure due to
obstructive uropathy. As a result, the patient maintained quality
of life until they died.
Severe localized problems may occur in patients with
invasive, inoperable bladder cancer and in those who have not
undergone cystectomy due to metastatic disease. These problems
include pain, bleeding, voiding problems and obstruction of the
upper urinary tract. Patients quality of life is markedly decreased
due to such problems (6,7). Salvage cystectomy is indicated for
palliation of such symptoms; however, elderly patients and certain
high-risk patients are not suitable for surgery. However,
particular patients are clinically unlikely to tolerate
chemotherapy, for example, those who have pre-existing comorbid
disease. These patients are candidates for palliative treatment
(8,9). Neither curative radical cystectomy nor
chemotherapy was indicated in the current case due to distant
metastases and a poor performance status, respectively.
Retroperitoneoscopic ureterocutaneostomy may relieve
severe symptoms and bleeding from tumors, preventing urinary
retention in the bladder. Furthermore, this procedure may avoid
postrenal failure due to bilateral lymph node metastasis or locally
advanced disease. It offers low morbidity with low-grade
postoperative pain, and low probability of postoperative ileus
compared with other urinary diversions using the intestinal tract,
due to the use of retroperitoneal manipulation (10,11). It
appears to be a reasonable alternative to percutaneous nephrostomy
for bilateral ureteral obstruction, provided that the clinical
condition of the patient allows general anesthesia (12,13). On
the other hand, as it is a permanent and irreversible procedure,
decisions regarding this option must be made following careful
consideration of the individuals condition and risk assessment.
Nakamura et al (14)
performed retroperitoneoscopic ureterocutaneostomy in a patient
with advanced bladder cancer who had a solitary kidney. Although
the patient died of progressive disease 3 months after the
operation, they did not present signs of postrenal failure nor did
he complain of macrohematuria after the operation (14). In the present case, urinary diversion
was performed only on the left side, as the right kidney was
hydronephrotic, atrophic and nonfunctional, due to tumor
obstruction. The left kidney functioned normally; therefore, the
serum creatinine level did not change markedly perioperatively.
In conclusion, surgery under general anesthesia is
typically avoided whenever possible in very elderly cases due to
increasing operative risk. In particular, retroperitoneoscopic
ureterocutaneostomy must be noted, as it is able to be performed in
elderly patients due to it being a minimally invasive surgery
without significant complications. Thus this surgery was able to be
performed for the very elderly patient in the present case without
postoperative delirium. Although its indication is limited to
select cases, retroperitoneoscopic ureterocutaneostomy for very
elderly patients of advanced bladder cancer with poor performance
status may be an important procedure for alleviating symptoms and
improving the quality of life.
References
|
1
|
Shariat SF, Sfakianos JP, Droller MJ,
Karakiewicz PI, Meryn S and Bochner BH: The effect of age and
gender on bladder cancer: a critical review of the literature. BJU
Int. 105:300–308. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
El-Tabey NA, Osman Y, Mosbah A, Mohsen T
and Abol-Enein H: Bladder cancer with obstructive uremia: oncologic
outcome after definitive surgical management. Urology. 66:531–535.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ok JH, Meyers FJ and Evans CP: Medical and
surgical palliative care of patients with urological malignancies.
J Urol. 174:1177–1182. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kearney GP, Docimo SG, Doyle CJ and
Mahoney EM: Cutaneous ureterostomy in adults. Urology. 40:1–6.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
MacGregor PS, Montie JE and Straffon RA:
Cutaneous ureterostomy as palliative diversion in adults with
malignancy. Urology. 30:31–34. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ubrig B, Lazica M, Waldner M and Roth S:
Extraperitoneal bilateral cutaneous ureterostomy with midline stoma
for palliation of pelvic cancer. Urology. 63:973–975. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gupta NP, Kolla SB, Seth A, Hemal AK,
Dogra PN and Kumar R: Oncological and functional outcome of radical
cystectomy in patients with bladder cancer and obstructive
uropathy. J Urol. 178:1206–1211, discussion 1211. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yi SK, Yoder M, Zaner K and Hirsch AE:
Palliative radiation therapy of symptomatic recurrent bladder
cancer. Pain Physician. 10:285–290. 2007.PubMed/NCBI
|
|
9
|
Witjes JA, Compérat E, Cowan NC, de Santis
M, Gakis G, Lebret T, Ribal MJ, Van der Heijden AG and Sherif A;
European Association of Urology, : EAU guidelines on
muscle-invasive and metastatic bladder cancer: summary of the 2013
guidelines. Eur Urol. 65:778–792. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yoshimura K, Ichioka K, Terada N, Matsuta
Y, Okubo K and Arai Y: Retroperitoneoscopic tubeless cutaneous
ureterostomy. BJU Int. 89:964–966. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Deliveliotis C, Papatsoris A, Chrisofos M,
Dellis A, Liakouras C and Skolarikos A: Urinary diversion in
high-risk elderly patients: modified cutaneous ureterostomy or
ileal conduit? Urology. 66:299–304. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Puppo P, Perachino M, Ricciotti G and
Bozzo W: Laparoscopic bilateral cutaneous ureterostomy for
palliation of ureteral obstruction caused by advanced pelvic
cancer. J Endourol. 8:425–428. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Puppo P, Ricciotti G, Bozzo W, Pezzica C,
Geddo D and Perachino M: Videoendoscopic cutaneous ureterostomy for
palliative urinary diversion in advanced pelvic cancer. Eur Urol.
28:328–333. 1995.PubMed/NCBI
|
|
14
|
Nakamura E, Terachi T, Kamoto T, Okuno H,
Terai A, Kakehi Y and Ogawa O: Retroperitoneoscopic
ureterocutaneostomy for obstructive uropathy with advanced bladder
cancer: a case report. Int J Urol. 9:60–62. 2002. View Article : Google Scholar : PubMed/NCBI
|