Introduction
Malignant psoas syndrome (MPS) was first described
by Stevens and Gonet in 1990 and is a unique cancer-related
syndrome characterized by ipsilateral proximal lumbosacral
plexopathy and painful hip flexion caused by radiographically or
pathologically evident malignant involvement of the psoas major
muscle (1,2). MPS is a rare entity, and its incidence
has been reported to be less than 1% among patients with high-risk
cancer, although this value may reflect under-recognition of the
disease (3,4).
As the pain in MPS involves a combination of
nociceptive and neuropathic pain, it is often intractable and
refractory to multiple drug treatment. In addition, MPS usually
occurs in patients with advanced and recurrent cancer; thus, it is
difficult to control the symptoms, resulting in remarkable
deterioration in the quality of life of patients. Although several
studies have reported different treatment approaches for MPS, the
effectiveness appears to be limited and an evidence-based effective
protocol remains to be established.
In the present paper, we report three cases of MPS
associated with gynecological malignancies, which showed symptom
improvement with particular medical interventions. We also discuss
the clinical features and practical treatment of MPS with a review
of the literature.
Case reports
Written and verbal informed consent was obtained
from all participating individuals.
Case 1
A 31-year-old woman was diagnosed with stage IB
poorly differentiated squamous cervical cancer and was treated with
radical hysterectomy and bilateral salpingo-oophorectomy followed
by adjuvant chemotherapy with paclitaxel plus carboplatin (TC). Six
months after the completion of the initial treatment, a recurrent
tumor was detected in the lower abdominal wall on follow-up
computed tomography (CT) scan. Abdominal wall resection and pedicle
flap reconstruction using the right tensor fascia lata were
performed. However, 3 months after the surgery, pelvic lymph node
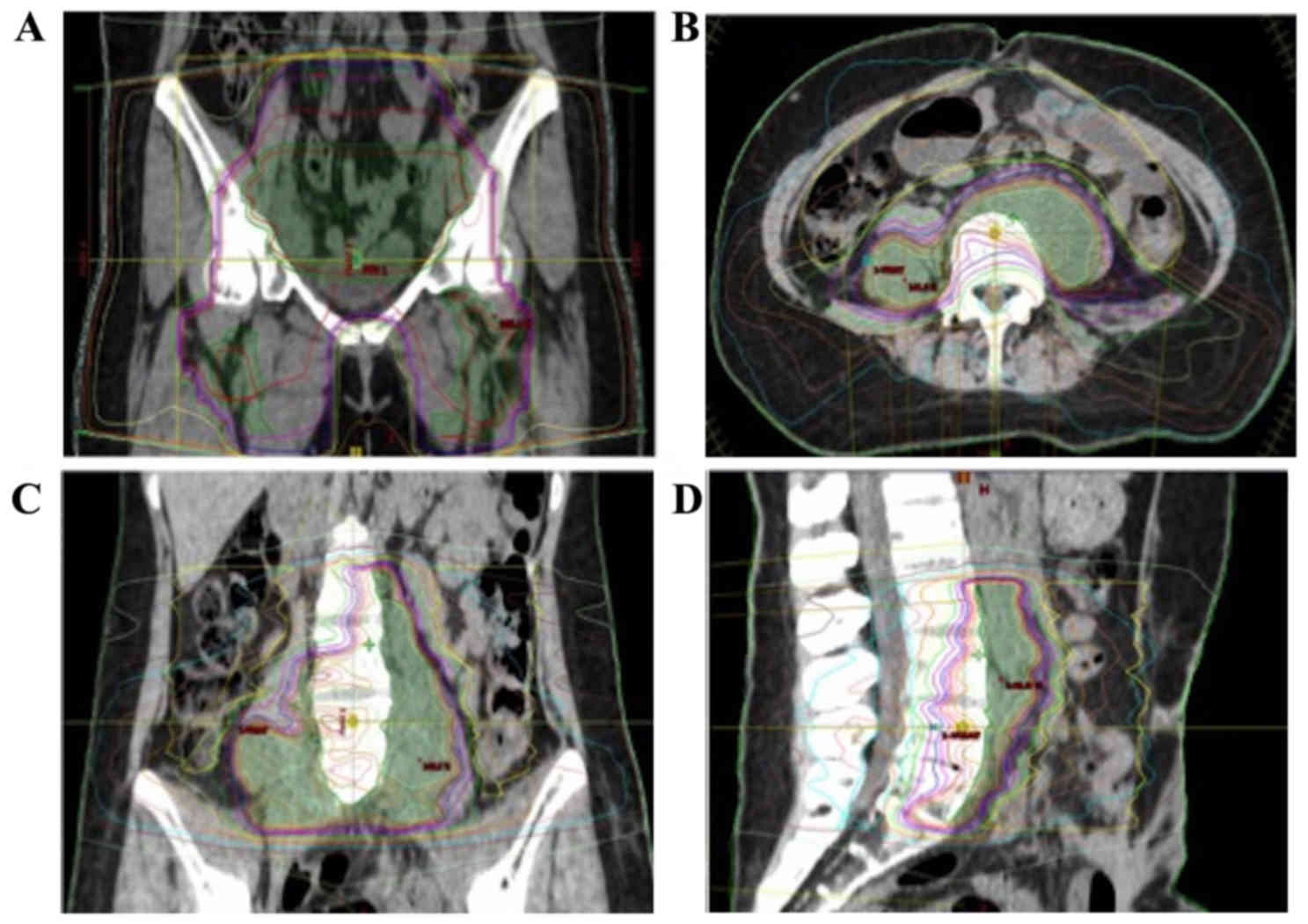
metastases were identified. External beam radiation therapy (EBRT)
to the whole pelvis (46 Gy in 23 fractions) and bilateral inguinal
region (20 Gy in 10 fractions) was performed with a total dose of
66 Gy in 33 fractions (Fig. 1A) and
partial tumor regression was observed. Although adjuvant
chemotherapy was considered, the patient was hospitalized again
because of small bowel obstruction. She eventually discontinued the
additional therapy.
Thirty months after the last radiation therapy, she
presented with a complaint of severe low back pain. The pain was
left-sided, extending from the lower back through the hip and thigh
to inside the knee, and it worsened in the last 1 month. Physical
examination identified painful flexion of her left hip and gait
abnormality.
The patient had been administered tramadol 200
mg/day and loxoprofen 180 mg/day for pain control in outpatient
settings, although this did not work well. After hospital
admission, the medications were changed to oral long-acting
oxycodone 20 mg/day plus a rescue dose of short-acting oxycodone 5
mg, naproxen 300 mg/day, acetaminophen 4 g/day, and pregabalin 75
mg/day. Subsequently, betamethasone 4 mg/day was added, and the
dose of oxycodone was increased to 60 mg/day. However, her pain
remained uncontrollable and was associated with an unpleasant
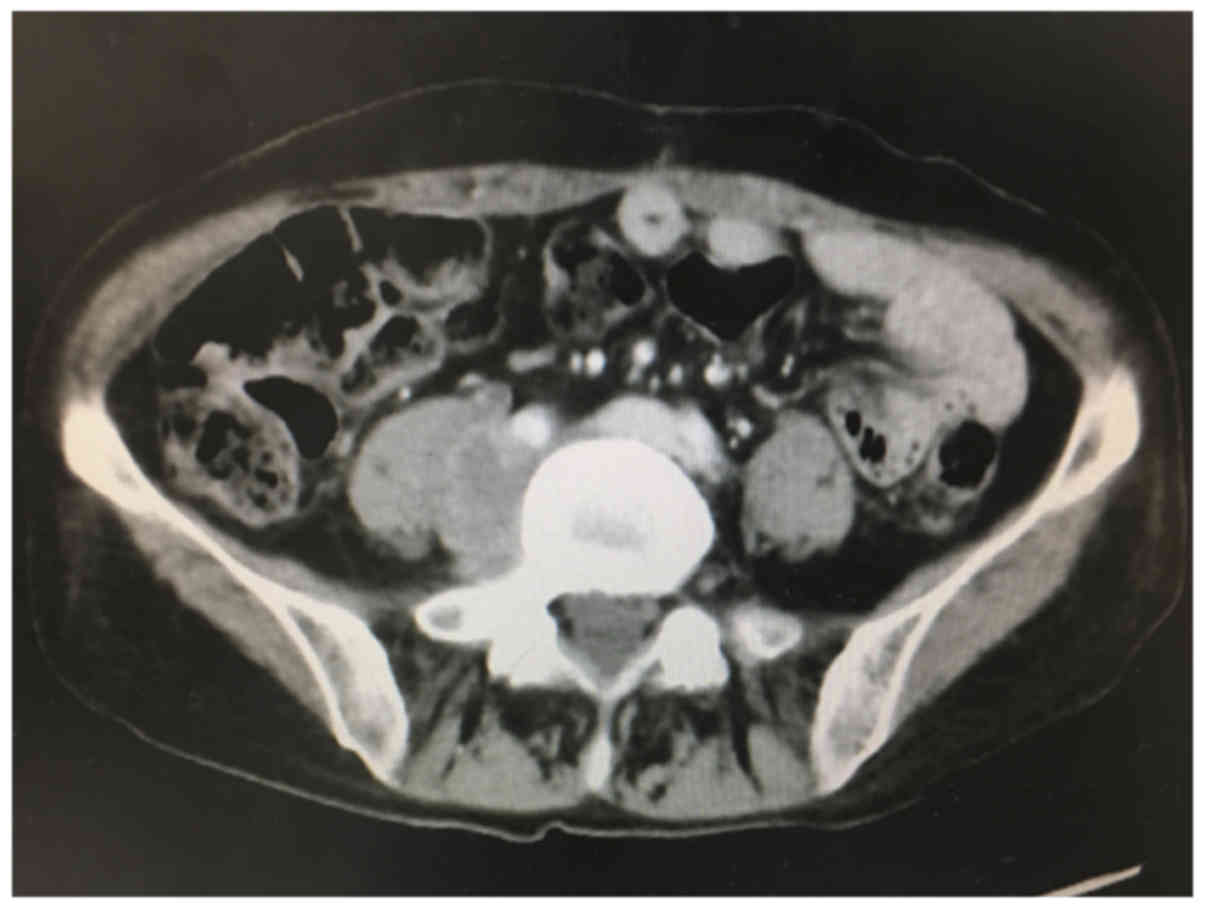
sleepiness. Magnetic resonance imaging revealed bilateral
metastatic para-aortic lymphadenopathy (Fig. 2). The left nodes were apparently
invading laterally into the left psoas muscle and almost replacing
it. Although the culprit lesion was very close to the previous
radiation field, intensity modulated radiation therapy (IMRT)
targeting the area was proposed by the radiologist (Fig. 1B-D).
After IMRT, with a total dose of 45 Gy in 25
fractions, her pain gradually reduced. Finally, she recovered
normal gait and was discharged from the hospital to a local clinic
for terminal care. Her pain relapsed 4 months after discharge but
was well controlled with administration of opioids. The patient
died due to the disease 8 months after symptom onset of MPS.
Case 2
A 63-year-old woman underwent initial surgery
involving total hysterectomy, bilateral salpingo-oophorectomy, and
pelvic lymph adenectomy for stage IB uterine endometrial serous
adenocarcinoma, followed by adjuvant chemotherapy with TC. Although
follow-up studies for the next 4 years showed no evidence of
recurrent disease, CT detected multiple para-aortic lymph node
metastases. The nodes were sensitive to salvage chemotherapy with
TC and were resected by the following surgery. However, soon after
the completion of the additional chemotherapy with the same
regimen, multiple metastatic lesions in bilateral lung fields and
supraclavicular lymph nodes were observed. Subsequently, she
received intermittent chemotherapy with a regimen of docetaxel and
carboplatin; however, there was limited tumor response.
After 5 cycles of the chemotherapy, she gradually
complained of worsening muscle weakness, edema, and severe pain
with a burning sensation in the right leg. On hospital admission
for treatment, her right hip was fixed in the flex position with
walking difficulty.
Analgesics including oral long-acting oxycodone 10
mg/day, loxoprofen 180 mg/day, and acetaminophen 3 g/day were
initially administered. The dose of oxycodone was increased to 40
mg/day, and a variety of adjuvant drugs were administered, such as
pregabalin 50 mg/day, olanzapine 2.5 mg at night, and betamethasone
4 mg/day. However, her condition did not show significant
improvement. Subsequent CT revealed para-aortic lymph node
metastases invading into the right psoas muscle (Fig. 3). She refused chemotherapy because of
the possible adverse effects and was referred to radiologists for
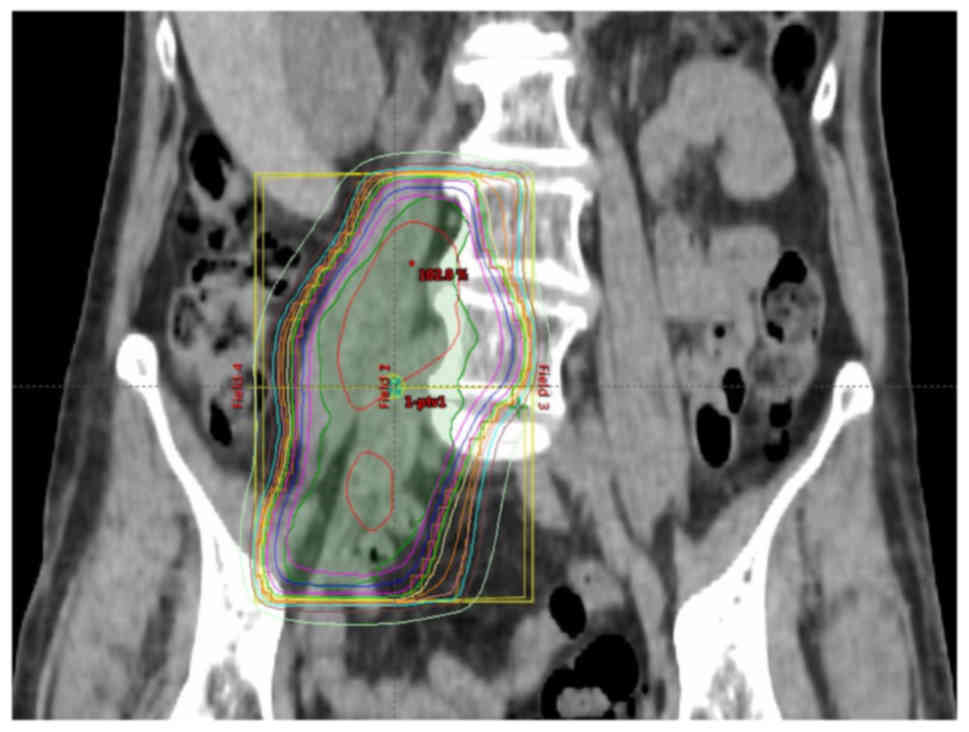
palliative radiotherapy. EBRT to the culprit lesion was planned,
with a dose of 40 Gy in 16 fractions (Fig. 4). Two weeks after the initiation of
radiation, her pain significantly improved, and analgesics were
stopped. Subsequently, she could walk independently and was
discharged from the hospital to home. The symptoms of MPS did not
recur; however, she died due to the disease, 7 months after symptom
onset.
Case 3
A 50-year-old woman with an initial diagnosis of
stage IVB fallopian tube cancer was referred to our hospital for
treatment. She presented with abdominal distension and severe pain
radiating from her left lower back to the lower leg. The pain was
associated with an inability to extend the left hip, and thus, the
patient was forced to rest with the hip in flexion.
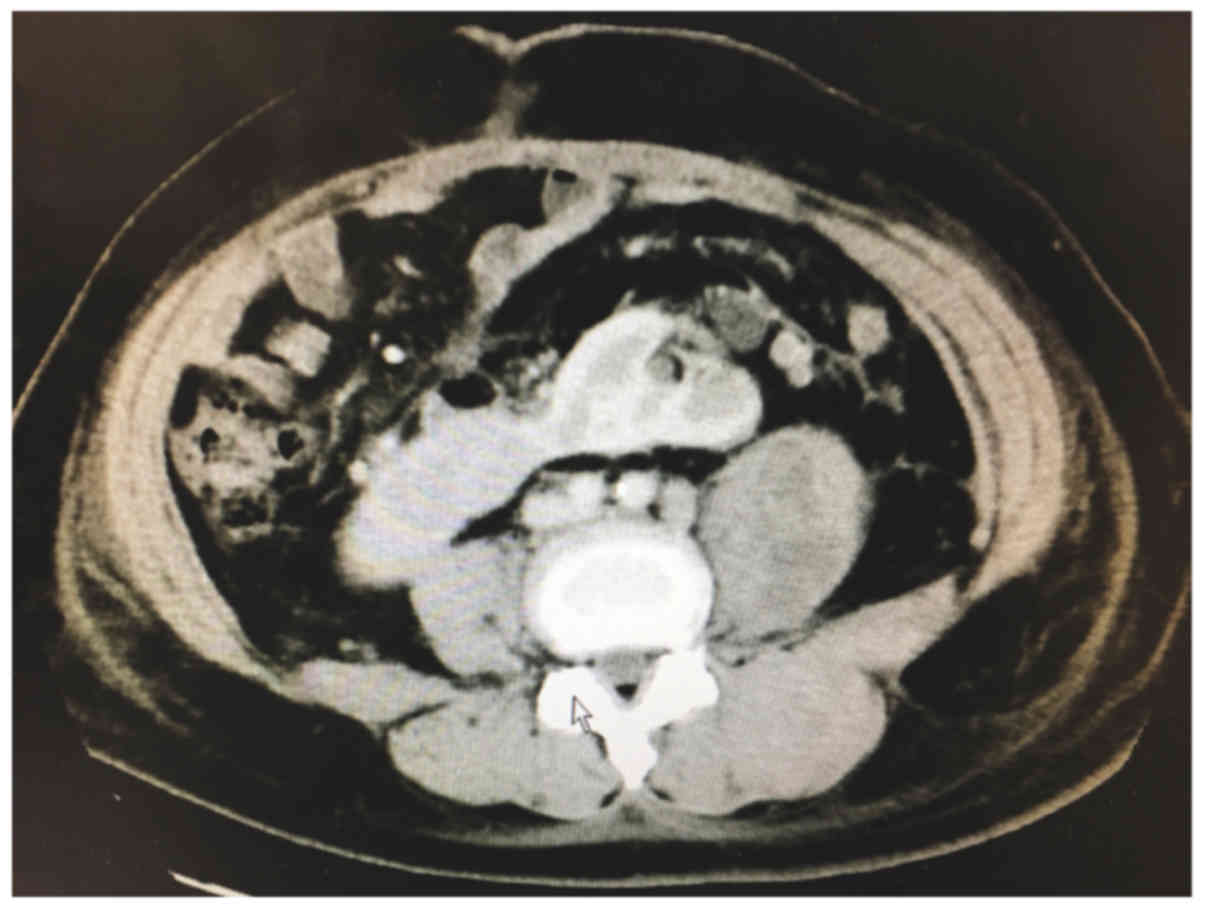
CT revealed cancerous ascites, multiple abdominal
disseminations, systematic lymphadenopathy, and multiple
intramuscular space-occupying lesions at the left psoas major and
quadratus lumborum muscles (Fig. 5).
Pain control medication was initiated, including oral long-acting
oxycodone 20 mg/day, naproxen 300 mg/day, and acetaminophen 4
g/day, with a rescue dose of short-acting oxycodone 5 mg. However,
the required dose of oxycodone continuously increased every day,
and opioid-induced side effects, including nausea, vomiting,
drowsiness, and delirium, progressively became intolerable. Opioid
switching to intravenous fentanyl was initiated, but it was not
effective. The pain worsened and became agonizing. After diagnostic
laparotomy, the patient was enrolled in a phase 3 clinical trial
with conventional TC chemotherapy plus an investigational drug or
placebo.
As the treatment advanced, her symptoms improved.
Finally, when the 6-course treatment was completed, radiographic
complete tumor remission was achieved, and her symptoms almost
disappeared.
At 7 months after the completion of chemotherapy,
recurrence was observed at the para-aortic lymph nodes and intra
psoas major muscle with no subjective symptoms. Salvage
chemotherapy with TC plus bevacizumab was undertaken, and the
recurrent tumors disappeared. The patient is currently alive with
no evidence of the disease.
Literature review and discussion
MPS is considered to be a rare entity. The frequency
of lumbosacral plexopathy in patients with cancer, which is not
specific to MPS, has been reported as 0.71% (4). However, such a low frequency may
reflect significant under-recognition of MPS (3,4). In
fact, we encountered our three patients over a period of 1 year in
our hospital. Similar cases may have been previously
overlooked.
On reviewing the English literature, we identified
39 cases of MPS in which the primary cancer site was identified
(1–3,5–19) (Table
I). It should be noted that among the different primary
cancers, female genital tract malignancies, accounting for 27%
(10/39) of the cases, were the most common diseases causing MPS,
followed by gastrointestinal (20%, 8/39) and urinary tract (20%,
8/39) malignancies. Psoas muscle involvement in MPS is considered
to result from either direct intramuscular metastasis or
extra-nodal extension from regional lymph nodes (2,3).
Considering this mechanism, it is reasonable that cancers with a
propensity to lymphatically metastasize to the retroperitoneal
nodes and/or hematogenously to the psoas major muscle, such as that
observed in genitourinary and colorectal malignancies, are likely
to cause MPS.
 | Table I.Sites of primary cancer causing
malignant psoas syndrome reported in the literature. |
Table I.
Sites of primary cancer causing
malignant psoas syndrome reported in the literature.
| Authors, year | Site of primary
cancer female genital tract | Number of cases
(n) | (Refs.) |
|---|
| Agar et al,
2004; Stevens et al, 2010; | Uterine cervix | 7 | (2,3,6,8,11,14,19) |
| Takase et al,
2015; Basu et al, 2014; |
|
|
|
| Ampil et al,
2001; Bar-Dayan et al, 1997; |
|
|
|
| Yamaguchi et
al, 2017 |
|
|
|
| Agar et al,
2004 | Ovary | 2 | (2) |
| Yang et al,
1999 | Uterine
endometrium | 1 | (10) |
|
| Gastrointestinal
tract |
|
|
| Yang et al,
1999; Ampil et al, 2001; | Colon | 5 | (10,11,13) |
| Avery et al,
1988 |
|
|
|
| Yang et al,
1999 | Rectum | 1 | (10) |
| Ota et al,
2017 | Stomach | 1 | (9) |
| Ampil et al,
2001 | Pancreas | 1 | (11) |
|
| Urinary tract |
|
|
| Stevens et al,
1990; Yamaguchi et al, 2017 | Bladder | 3 | (1,19) |
| Stevens et
al, 1990; Takase et al, 2015 | Prostate | 2 | (1,6) |
| Ampil et al,
2001; Linn et al, 1996 | Kidney | 2 | (11,15) |
| Takase et
al, 2015 | Urachus | 1 | (6) |
|
| Hematological
cancer |
|
|
| Agar et al,
2004; Kounami et al, 2012 | Lymphoma
Lymphoma | 4 | (2,7,12,17) |
|
| Others |
|
|
| Ampil et al,
2001; Nash et al, 1996 | Lung | 2 | (11,18) |
| Elkowitz et
al, 1991 | Tongue | 1 | (16) |
| Elkowitz et
al, 1991 | Nasopharynx | 1 | (16) |
| Ampil et al,
2001; Yamaguchi et al, 2017 | Skin | 2 | (11,19) |
| McKay et al,
2017 | Psoas muscle | 1 | (5) |
The pain associated with MPS is usually difficult to
treat. This could be explained by the complex pathogenesis of this
condition, with malignant involvement of the psoas major muscle
producing not only deep somatic nociceptive pain but also
neuropathic pain, owing to lumbosacral plexopathy (2,3).
Furthermore, patients presenting with MPS usually have advanced and
recurrent cancers. In the case of initially diagnosed cancer,
cancer-directed therapy can be the most effective option; however,
in most cases, the tumor is already refractory to standard therapy.
Consequently, only palliative treatments could be adapted in such
cases. Among our cases, the patient with primary fallopian tube
cancer showed symptom improvement concordant with the
chemotherapeutic effect.
Several reports have proposed approaches for the
management of MPS, but no single, crucial protocol has been
established. A simple analgesic agent is often ineffective, and
multimodal pharmacotherapy, including opioids, non-opioid
analgesics, and adjuvant drugs (antiepileptics, antidepressants,
and muscle relaxants), is required, although its effectiveness has
been shown to be limited (2,3). Recent studies have shown that rotation
switching of opioids to methadone was effective for refractory
neuropathic pain (6,20). Other studies reported the efficacy of
intervention strategies, including epidural analgesia (9,19),
injection from a psoas sheath catheter (21) or intrathecal catheter (19,22), and
dorsal rhizotomy (23). Radiotherapy
is occasionally adapted for both cancer-directed and palliative
therapy, although its efficacy remains to be clarified (1,2,4,5). In two
of our cases with progressive recurrent uterine cancer, palliative
radiation therapy resulted in significant symptom improvement. It
should be noted that in the cervical cancer case, IMRT targeted to
the lesion close to the post-radiated area was effective without
serious adverse events. In recent decades, high-precision radiation
therapy, including IMRT, has been developed. As this therapy can
deliver a highly conformal dose to the target with minimal exposure
to adjacent normal tissues, it can significantly reduce toxicity
and improve disease control (24,25). It
could be emphasized that radiotherapy is a considerable treatment
option for MPS.
The survival of patients with MPS is considered to
be very short, as demonstrated by many previous studies, and the
reported median survival duration was 5.5–10.7 months after
diagnosis (2,4,19,23). In
the present study, patients in cases 1 and 2 died at 8 and 7 months
from the time of diagnosis, respectively. Considering such a
significant mortality rate and remarkable impact on the patient's
quality of life, the recognition and diagnosis of this syndrome are
clinically important to allow patients to receive all possible
therapies.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
ST designed the study and prepared the manuscript
draft and substantively participated in revising the manuscript. NM
contributed in analyzing the patients' data and revised the
manuscript. KM, HT, TT, and HN collected and interpreted the
clinical data and conducted a comprehensive literature review
related to this project. AS and MM helped revise the manuscript for
important intellectual content. All authors thoroughly reviewed the
manuscript. All authors read and approved the final version of this
manuscript.
Ethics approval and consent to
participate
The present study was conducted in accordance with
the ethical principles of the Declaration of Helsinki. Written and
verbal informed consent was obtained from all participating
individuals.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
CT
|
computed tomography
|
|
EBRT
|
external beam radiation therapy
|
|
IMRT
|
intensity modulated radiation
therapy
|
|
MPS
|
malignant psoas syndrome
|
|
TC
|
paclitaxel plus carboplatin
|
References
|
1
|
Stevens MJ and Gonet YM: Malignant psoas
syndrome: Recognition of an oncologic entity. Australas Radiol.
34:150–154. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Agar M, Broadbent A and Chye R: The
management of malignant psoas syndrome: Case reports and literature
review. J Pain Symptom Manage. 28:282–293. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stevens MJ, Atkinson C and Broadbent AM:
The malignant psoas syndrome revisited: Case report, mechanisms,
and current therapeutic options. J Palliat Med. 13:211–216. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jaeckle KA: Neurological manifestations of
neoplastic and radiation-induced plexopathies. Semin Neurol.
24:385–393. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
McKay TA, Bishop S and McKay MJ: Primary
psoas sarcoma causing malignant psoas syndrome: Favourable response
to radiotherapy. Ann Transl Med. 5:1052017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Takase N, Ikegaki J, Nishimura H, Yuasa S,
Ito Y and Kizawa Y: Methadone for patients with malignant psoas
syndrome: Case series of three patients. J Palliat Med. 18:645–652.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kounami S, Shibuta K, Yoshiyama M, Mitani
Y, Watanabe T, Takifuji K and Yoshikawa N: Primary anaplastic large
cell lymphoma of the psoas muscle: A case report and literature
review. Acta Haematol. 127:186–188. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Basu S and Mahajan A: Psoas muscle
metastasis from cervical carcinoma: Correlation and comparison of
diagnostic features on FDG-PET/CT and diffusion-weighted MRI. World
J Radiol. 6:125–129. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ota T, Makihara M, Tsukuda H, Kajikawa R,
Inamori M, Miyatake N, Tanaka N, Tokunaga M, Hasegawa Y, Tada T and
Fukuoka M: Pain management of malignant psoas syndrome under
epidural analgesia during palliative radiotherapy. J Pain Palliat
Care Pharmacother. 31:154–157. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang WT, Yeo W and Metreweli C: Imaging of
iliopsoas metastasis. Clin Radiol. 54:85–89. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ampil FL, Lall C and Datta R: Palliative
management of metastatic tumors involving the psoas muscle: Case
reports and review of the literature. Am J Clin Oncol. 24:313–314.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Connor SE, Chavda SV and West R:
Recurrence of non-Hodgkin's lymphoma isolated to the right
masticator and left psoas muscles. Eur Radiol. 10:841–843. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Avery GR: Metastatic adenocarcinoma
masquerading as a psoas abscess. Clin Radiol. 39:319–320. 1988.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bar-Dayan Y, Fishman A, Levi Z and
Rachmani R: Squamous cell carcinoma of the cervix with psoas
abscess-like metastasis in an HIV-negative patient. Isr J Med Sci.
33:674–676. 1997.PubMed/NCBI
|
|
15
|
Linn JF, Fichtner J, Voges G, Schweden F,
Störkel S and Hohenfellner R: Solitary contralateral psoas
metastasis 14 years after radical nephrectomy for organ confined
renal cell carcinoma. J Urol. 156:1731996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Elkowitz SS, Patel M and Hirschfield LS:
Paravertebral muscle metastases from primary tongue and
nasopharyngeal carcinomas. Clin Radiol. 43:400–401. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cortés-Blanco A and Martínez-Lázaro R:
Lymphoma mimicking a psoas abscess on Ga-67 scintigraphy. Clin Nucl
Med. 25:567–568. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nash S, Rubenstein J, Chaiton A and
Morava-Protzner I: Adenocarcinoma of the lung metastatic to the
psoas muscle. Skeletal Radiol. 25:585–587. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yamaguchi T, Katayama K, Matsumoto M, Sato
Y, Nakayama N and Hisahara K: Successful control of pain from
malignant psoas syndrome by spinal opioid with local anesthetic
agents. Pain Pract: 23 Sep 2017 (Epub ahead of print).
|
|
20
|
Porta-Sales J, Garzón-Rodríguez C,
Villavicencio-Chávez C, Llorens-Torromé S and González-Barboteo J:
Efficacy and safety of methadone as a second-line opioid for cancer
pain in an outpatient clinic: A prospective open-label study.
Oncologist. 21:981–987. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Douglas I and Bush D: The use of
patient-controlled boluses of local anaesthetic via a psoas sheath
catheter in the management of malignant pain. Pain. 82:105–107.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Becker R, Jakob D, Uhle EI, Riegel T and
Bertalanffy H: The significance of intrathecal opioid therapy for
the treatment of neuropathic cancer pain conditions. Stereotact
Funct Neurosurg. 75:16–26. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Son BC, Yoon JH, Kim DR and Lee SW: Dorsal
rhizotomy for pain from neoplastic lumbosacral plexopathy in
advanced pelvic cancer. Stereotact Funct Neurosurg. 92:109–116.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nakamura K, Sasaki T, Ohga S, Yoshitake T,
Terashima K, Asai K, Matsumoto K, Shioyama Y and Honda H: Recent
advances in radiation oncology: Intensity-modulated radiotherapy, a
clinical perspective. Int J Clin Oncol. 19:564–569. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhang MX, Li J, Shen GP, Zou X, Xu JJ,
Jiang R, You R, Hua YJ, Sun Y, Ma J, et al: Intensity-modulated
radiotherapy prolongs the survival of patients with nasopharyngeal
carcinoma compared with conventional two-dimensional radiotherapy:
A 10-year experience with a large cohort and long follow-up. Eur J
Cancer. 51:2587–2595. 2015. View Article : Google Scholar : PubMed/NCBI
|