Introduction
Cutaneous angiosarcoma is a rare and aggressive
malignant tumor with poor prognosis and high risk of hematogenous
dissemination (1). It usually
develops on the scalp or face of elderly males (1). The scalp is a tumor site associated
with poor prognosis (2–4). Angiosarcoma of the scalp is often
treated with multimodality treatment, including surgery, radiation
therapy, chemotherapy, and immunotherapy (1–14).
Several studies have recently reported the efficacy
of taxane chemotherapy for cutaneous angiosarcomas of the scalp
(5–7,15–18). In
particular, concurrent chemoradiation (CCRT) with taxanes has been
reported to be one of the optimal treatment methods for this
malignancy (5,6). Moreover, patients receiving CCRT with
maintenance chemotherapy using taxanes showed a significant
improvement in overall survival (OS) than those receiving CCRT
alone (6). In 2006, we established
CCRT with maintenance chemotherapy using taxanes (paclitaxel or
docetaxel) as the standard treatment strategy for localized
angiosarcoma of the scalp without cervical lymph node metastasis.
Taxanes were administered as early as possible, followed by
maintenance chemotherapy also using taxanes. Maintenance
chemotherapy was repeated several times, when possible. Although
there were no criteria for administration of concurrent and
maintenance chemotherapy, we attempted to administer both
concurrent and maintenance chemotherapy, if feasible. Prior to the
establishment of this strategy, interleukin-2 (IL-2) was often used
in combination with radiation therapy.
This study aimed to retrospectively analyze the
efficacy of CCRT with maintenance chemotherapy using taxanes for
localized angiosarcomas of the scalp without cervical lymph node
metastases. To our knowledge, there have been no studies that have
analyzed the efficacy of CCRT and maintenance chemotherapy using
taxanes exclusively for localized angiosarcomas of the scalp
without cervical lymph node metastases.
Patients and methods
This retrospective study was approved by Okayama
University Hospital institutional review board (Approval no.
K1610-503), and the need for informed consent was waived owing to
the retrospective nature of the study.
Study population
This study included 19 patients with localized
angiosarcomas of the scalp without cervical lymph node metastases
who received radiation therapy between January 2000 and December
2017 at the Okayama University Hospital. All patients were
pathologically diagnosed with angiosarcoma of the scalp. The
patients received radiation therapy alone or in combination with
surgery, chemotherapy, or immunotherapy.
Radiation therapy
Radiation therapy was carried out using electron and
X-ray beams, 5 days per week for approximately 2 months. The
prescribed dose was 70 or 60 Gy in 2.0-Gy fractions. Up to 60 Gy,
the area of the initial irradiation field typically encompassed the
tumor with a 5-cm margin from the edges. In cases with residual
tumor, immediately before completion of 60 Gy, a 10-Gy boost dose
was delivered to the tumor mass. The boost irradiation field
typically covered a 2-cm margin from the edge of the tumor mass.
The extent of disease was determined by a dermatologist. In
post-surgical cases, the irradiation field was conjointly
determined by radiation oncologists and dermatologists. Computed
tomography (CT) simulation was used to determine the energy of the
electron beams and the thickness of bolus applied. The thickness of
the bolus was 5 or 10 mm.
Chemotherapy regimens
The weekly paclitaxel or docetaxel schedule
comprised 80 mg/m2 of paclitaxel or 30 mg/m2
of docetaxel, respectively, on days 1, 8, and 15 of a 28-day cycle.
The triweekly paclitaxel or docetaxel schedule comprised 210
mg/m2 of paclitaxel or 60 mg/m2 of docetaxel,
respectively, on day 1 of a 21-day cycle. Dose reduction and/or
extension of the treatment interval was based on the discretion of
the dermatologist. A weekly paclitaxel or docetaxel regimen was
used concurrently with radiation therapy. The type of chemotherapy
regimen depended on the discretion of the dermatologist.
Maintenance chemotherapy was defined as the repeated administration
of chemotherapy until tumor recurrence.
Other treatments
Prior to the establishment of this CCRT with
maintenance chemotherapy treatment strategy, immunotherapy (IL-2)
was used in combination with radiation therapy.
Surgery was performed in cases deemed completely
resectable by the dermatologist.
Patient and treatment
characteristics
The patient and treatment characteristics are shown
in Table I. The cohort comprised 14
men and 5 women with a median age of 78 years (range, 34–91 years).
Radiation therapy alone, radiation therapy + IL-2, surgery + CCRT
with maintenance chemotherapy, CCRT with maintenance chemotherapy,
and CCRT without maintenance chemotherapy were administered to 2,
4, 2, 9, and 2 patients, respectively. Data on tumor size was
missing for 1 patient, and 17 patients had tumors measuring ≥5
cm.
 | Table I.Patient and treatment
characteristics. |
Table I.
Patient and treatment
characteristics.
| Characteristic | No. of patients |
|---|
| Agea, years |
|
|
<75 | 8 |
| ≥75 | 11 |
| Sex |
|
| Male | 14 |
|
Female | 5 |
| Tumor size
(n=18)b, cm |
|
|
<5 | 1 |
| ≥5 | 17 |
| Radiation dose,
Gy |
|
| 60 | 3 |
| 70 | 16 |
| Surgery |
|
| Yes | 2 |
| No | 17 |
| IL-2 |
|
| Yes | 4 |
| No | 15 |
| Concurrent
chemotherapy |
|
| Yes | 13 |
| No | 6 |
| Concurrent and
maintenance chemotherapy |
|
|
Yes | 11 |
| No | 8 |
For radiation therapy, the median radiation dose was
70 Gy (range, 60–70 Gy). Only 1 patient was treated using electron
and X-ray beams. All other patients were treated using electron
beams only (3–12 MeV). Data on the bolus were missing for 3
patients, but the records indicated that all other patients were
treated using a bolus; a 5-mm and 10-mm bolus was applied in 14 and
2 patients, respectively. The planned radiation therapy could not
be completed in 1 patient owing to scalp infection. The radiation
dose in this patient was 60 Gy. The other patients completed the
planned radiation therapy schedule.
Among the 13 patients who received chemotherapy,
taxanes (paclitaxel or docetaxel) were concurrently administered
with radiation therapy. Weekly paclitaxel and docetaxel regimens
were used concurrently with radiation therapy in 11 and 2 patients,
respectively; these patients received 2 courses of the treatment.
Among the patients who received CCRT, 11 patients subsequently
received maintenance chemotherapy with a taxane. The weekly and
triweekly paclitaxel maintenance chemotherapy regimens were used in
5 and 3 patients, respectively. Weekly and triweekly maintenance
chemotherapy schedules of paclitaxel and docetaxel were used in 1
and 2 patients, respectively. Data regarding the total number of
chemotherapy courses were missing for 3 patients; excluding these
patients, the median number of courses was 11 (1–58). Among 13
patients treated with CCRT, taxane maintenance chemotherapy was not
administered in 2 patients, 1 of whom developed spontaneously
resolving elevated blood pressure and arrhythmia during the fourth
course of paclitaxel. After this event, we decided to discontinue
chemotherapy during and after radiation therapy for that patient.
In the other patient, chemotherapy was discontinued approximately 2
months after radiation therapy due to unknown reasons. Overall, 6
of the 19 patients were not administered taxanes. Among them, 4
patients were treated before our treatment strategy of CCRT with
maintenance chemotherapy using taxanes was established; the
remaining 2 patients were considerably aged (90 and 91 years).
Additionally, 4 patients received immunotherapy
using IL-2, and 2 patients underwent surgery before radiation
therapy. In 1 patient who underwent surgery, the lesion around the
postoperative site was clinically apparent before radiation
therapy.
Definition of recurrence
Local recurrence was defined as recurrence in the
scalp and face, while distant recurrence included the cervical
lymph nodes. Local control was evaluated using examination and
biopsy, whereas distant recurrence was evaluated using CT, magnetic
resonance imaging, and positron-emission tomography (PET)-CT. The
follow-up protocol was not clearly determined.
Adverse events
Adverse events were evaluated using the Common
Terminology Criteria for Adverse Events version 4.0. Adverse events
of grades >2 were investigated.
Statistical analyses
OS, progression-free survival (PFS), and local
control (LC) rates were calculated using Kaplan-Meier analysis. OS,
PFS, and LC were calculated from the initiation of treatment until
death, disease progression or death, and local recurrence,
respectively. Univariate analyses were performed for the various
potential prognostic factors for OS, PFS, and LC. Distant
metastasis-free survival (DMFS) was also analyzed in the same
manner. DMFS was calculated until distant recurrence or death.
Multivariate analysis was not performed owing to the small number
of patients. Kaplan-Meier analyses and log-rank tests were
performed using the JMP 12 statistical software package (SAS
Institute, Cary, NC, USA). P<0.05 was considered to indicate a
statistically significant difference.
Results
Follow-up and outcomes
The median follow-up period was 15 months (range,
3–102 months). During follow-up, local and distant recurrence
occurred in 6 and 13 patients, respectively. The first sites of
recurrence were only local, only distant, and both local and
distant in 5, 8, and 1 patients, respectively. In the 5 cases where
the first site of recurrence was only local, all the sites of the
first local recurrence were within the radiation field. In the 1
case where the first site of recurrence was local and distant, data
on the site of local recurrence was missing. A total of 10 patients
who died due to angiosarcoma had distant metastases at the time of
death, with the most common site of metastases being the lung
(n=7). In 6 patients, death was related to lung metastases. No
patient died of other diseases. The rates of 1- and 3-year OS, PFS,
and LC were 88 and 52%, 47 and 33%, and 74 and 56%,
respectively.
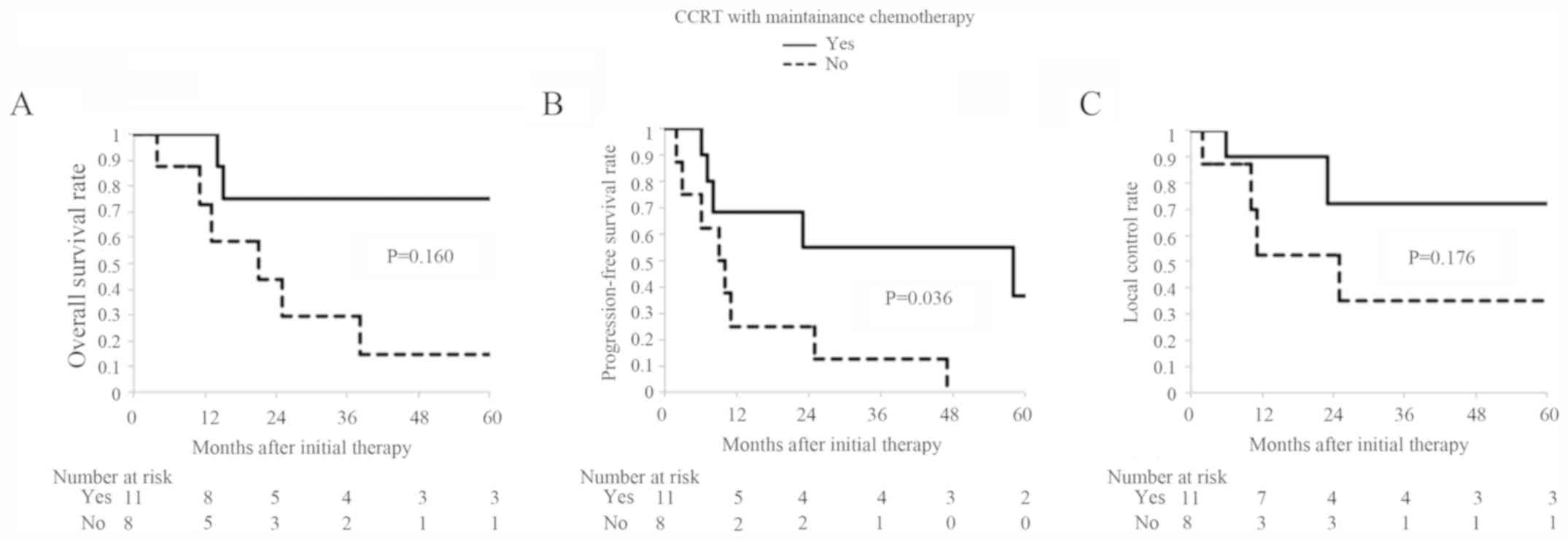
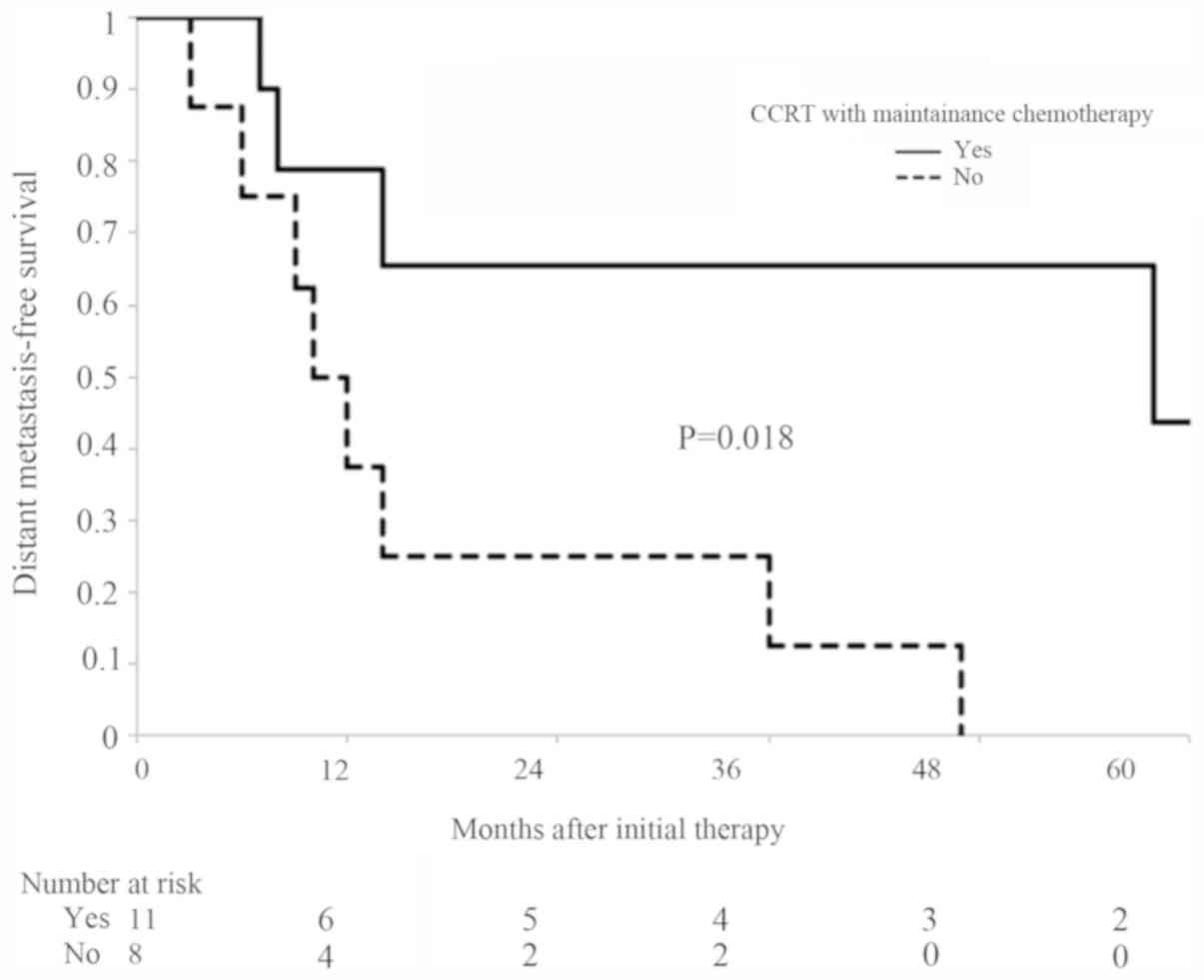
The results of the univariate analyses are shown in
Table II. CCRT with maintenance
chemotherapy and surgery were significant prognostic factors for
PFS (P=0.036, and 0.025, respectively) but not for OS and LC. The
results of CCRT with maintenance chemotherapy using taxanes
regarding OS, PFS, and LC are shown in Fig. 1. No significant prognostic factors
were found for OS and LC. In DMFS, CCRT with maintenance
chemotherapy using taxanes and surgery were significant prognostic
factors as well (P=0.018, and 0.029). The results of CCRT with
maintenance chemotherapy using taxanes with respect to DMFS is
shown in Fig. 2.
 | Table II.Results of univariate analysis. |
Table II.
Results of univariate analysis.
|
|
| aOverall survival rate | Progression-free
survival rate | Local control
rate |
|---|
|
|
|
|
|
|
|---|
| Variable | No. of
patients | 1-year | 3-years | P-value | 1-year | 3-years | P-value | 1-year | 3-years | P-value |
|---|
| Age (years) |
|
|
| 0.175 |
|
| 0.074 |
|
| 0.298 |
|
<75 | 8 | 100 | 71 |
| 75 | 60 |
| 88 | 70 |
|
|
≥75 | 11 | 77 | 34 |
| 24 | 12 |
| 59 | 40 |
|
| Sex |
|
|
| 0.192 |
|
| 0.670 |
|
| 0.751 |
|
Male | 14 | 82 | 49 |
| 41 | 31 |
| 72 | 54 |
|
|
Female | 5 | 100 | 60 |
| 60 | 40 |
| 80 | 60 |
|
| Radiation dose,
Gy |
|
|
| 0.051 |
|
| 0.171 |
|
| 0.224 |
| 60 | 3 | 100 | 100 |
| 100 | 100 |
| 100 | 100 |
|
| 70 | 16 | 86 | 45 |
| 39 | 23 |
| 70 | 46 |
|
| Surgery |
|
|
| 0.234 |
|
| 0.025 |
|
| 0.236 |
|
Yes | 2 | 100 | 100 |
| 100 | 100 |
| 100 | 100 |
|
| No | 17 | 86 | 45 |
| 39 | 23 |
| 70 | 47 |
|
| IL-2 |
|
|
| 0.919 |
|
| 0.270 |
|
| 0.425 |
|
Yes | 4 | 75 | 50 |
| 50 | 25 |
| 75 | 38 |
|
| No | 15 | 91 | 53 |
| 44 | 35 |
| 74 | 62 |
|
| CCRT |
|
|
| 0.351 |
|
| 0.080 |
|
| 0.370 |
|
Yes | 13 | 100 | 67 |
| 53 | 42 |
| 80 | 64 |
|
| No | 6 | 67 | 33 |
| 33 | 17 |
| 63 | 42 |
|
| CCRT with
maintenance chemotherapy |
|
|
| 0.160 |
|
| 0.036 |
|
| 0.176 |
|
Yes | 11 | 100 | 75 |
| 69 | 55 |
| 90 | 72 |
|
| No | 8 | 73 | 29 |
| 25 | 13 |
| 53 | 35 |
|
Adverse events
During radiation therapy, 4 patients treated with
CCRT developed hematotoxicity. Both grade 3 leukocytopenia and
neutropenia were noted in 2 patients; 1 patient developed both
grade 4 leukocytopenia and neutropenia; and 1 patient developed
grade 3 neutropenia. However, no patient discontinued chemotherapy
because of hematotoxicity. The 6 patients without CCRT did not
develop hematotoxicity. All patients developed radiation dermatitis
up to Grade 3, but radiation therapy was not suspended due to
hematotoxicity or dermatitis. A grade 3 scalp infection occurred in
1 patient that required intravenous antibiotic therapy. Only this
patient could not complete the planned radiation therapy schedule,
the dose of which was 60 Gy.
In terms of adverse events after radiation therapy,
4 patients treated with taxanes developed hematotoxicity. Grade 3
leukocytopenia and neutropenia, grade 3 neutropenia, and grade 4
neutropenia developed in 1 patient each. Grade 3 anemia was
observed in 1 patient. Grade 3 and 4 skin ulceration was noted in 1
patient each; 1 patient developed grade 3 cranial bone necrosis
with grade 4 skin ulceration. Grade 3 skin ulceration was noted in
1 patient who underwent CCRT (total dose of 60 Gy) with maintenance
chemotherapy using a weekly paclitaxel schedule after complete
resection. The patient with grade 4 skin ulceration received CCRT
(total dose of 70 Gy) with maintenance chemotherapy using a weekly
docetaxel schedule during radiation therapy and a triweekly
paclitaxel schedule after radiation therapy. Approximately 3 months
after radiation therapy, a residual lesion was suspected, and a
complete resection was performed. However, pathologically there was
no residual tumor. Approximately 7 months after the resection,
epidermization was performed for the ulcer at the postoperative
site. However, graft failure was observed after epidermization. The
patient with grade 3 cranial bone necrosis with grade 4 skin
ulceration underwent CCRT (total dose of 70 Gy) with maintenance
chemotherapy using a docetaxel schedule after resection and
epidermization. In this patient, the cranial bone necrosis was
removed, followed by reconstruction using an anterolateral thigh
flap and epidermization.
Discussion
In this study, we retrospectively evaluated the
efficacy of CCRT with maintenance chemotherapy using taxanes for
localized angiosarcomas of the scalp without cervical lymph node
metastases. On univariate analyses, CCRT with maintenance
chemotherapy using taxanes was a significant prognostic factor for
PFS and DMFS. All 10 patients who died had distant metastases at
the time of death, and 7 of them had lung metastases. Moreover, in
6 of these 10 patients, death was related to lung metastases. We
therefore speculated that CCRT with maintenance chemotherapy may
improve OS by preventing distant metastases. However, in this
study, CCRT with maintenance chemotherapy using taxanes was not a
significant prognostic factor for OS.
There are several reports on the importance of CCRT
with maintenance chemotherapy (5–7). Miki
et al (5) reported that
patients treated with docetaxel, including those with lymph node
metastasis, showed significantly better OS (P=0.0477) and distant
metastasis-free rates (P=0.0063) than those who did not receive
docetaxel. In their study, docetaxel was concurrently administered
with radiation therapy. Fujisawa et al (6) reported that the 5-year OS rate of
patients receiving CCRT with docetaxel or paclitaxel was
significantly higher than that of those receiving postoperative
radiation therapy (56 vs. 8%, respectively; P<0.01). Moreover,
patients who received CCRT followed by maintenance chemotherapy
showed a significant improvement in OS than those receiving CCRT
alone (P<0.01). Their study included patients with limb lesions
and with lymph node metastases. Regarding maintenance chemotherapy,
Ito et al (7) also reported
that maintenance chemotherapy with taxanes substantially affected
survival. Patients administered maintenance chemotherapy with
taxanes had prolonged disease-specific survival (DSS) and
event-free survival (EFS) compared with those who did not receive
it (3-year DSS: 77.0 vs. 39.2%, 5-year DSS: 57.0 vs. 19.6%, median
survival: 62.2 vs. 17.7 months, P=0.0049; 3-year EFS: 52.4 vs.
22.5%, 5-year EFS: 34.9 vs. 5.6%, median survival: 46.7 vs. 12.4
months, P=0.0024). Moreover, multivariate analysis revealed that
maintenance chemotherapy with taxanes was an independent prognostic
factor for DSS and EFS (P=0.046 for both). Their study included
patients with lymph node metastases and other distant metastases.
Treatments for primary lesions included radiation therapy, surgery,
and chemotherapy. Collectively, the findings of these studies
support our hypothesis that CCRT with maintenance chemotherapy
might improve OS. The retrospective design, small population, and
short follow-up period of our study may explain the lack of any
significant impact of CCRT with maintenance chemotherapy on OS.
Regarding adverse events, patients treated with CCRT
tended to develop severe hematotoxicity compared with those treated
without CCRT. In addition, 1 patient did not complete the planned
radiation therapy because of scalp infection. However, all the
other patients treated with CCRT completed the planned radiation
therapy and continued the chemotherapy. Therefore, the severity of
these acute adverse events during CCRT is acceptable. Similarly,
the toxicity associated with maintenance chemotherapy was also
acceptable. None of the patients were required to discontinue the
maintenance chemotherapy because of adverse events; the 3 patients
with skin ulceration also continued maintenance chemotherapy.
Regarding prognostic factors other than CCRT with
maintenance chemotherapy, surgery was a significant risk factor for
PFS and DMFS in this study. In their systematic review and
meta-analysis, Shin et al (4)
reported that surgery was the most effective treatment for
improving the survival rate. However, we believe that in our study,
the impact of surgery was unclear. This is because only 2 patients
underwent surgery; they also underwent CCRT with maintenance
chemotherapy, which may have affected the outcome. Age was not a
significant risk factor for OS in this study; this was similar to
the findings of previous studies (2,5,6,8–12). However, some other studies have
reported that age is a significant factor for survival (4,7,13,14). To
date, the association between age and survival remains unclear.
Tumor size has also been reported to be a prognostic factor for
survival (4,8,11,13),
with previous studies using a cut-off value of 5 cm. Conversely,
other previous studies have reported that tumor size is not a
significant factor affecting survival (2,3,5–7,9,10,12,14).
Tumor size was not included in our univariate analyses because data
on the tumor size of 1 patient were missing and only 1 patient had
a tumor measuring <5 cm. Therefore, the prognostic impact of
tumor size could not be determined in our study.
Regarding radiation therapy, the appropriate
prescribed doses, irradiation fields, and radiotherapy techniques
have not yet been determined. In previous reports, various
prescribed doses, irradiation fields, and radiotherapy techniques
were used. Bernstein et al (2) reported median preoperative,
postoperative, and definitive radiotherapy doses of 52, 53, and 56
Gy, respectively, delivered using megavoltage photons, electrons,
or intensity-modulated radiotherapy. The median dose per fraction
was 2 Gy. The radiation fields covered the primary site with
generous margins, and some patients received total scalp
radiotherapy. Ward et al (3)
reported doses that ranged from 45 to 75.6 Gy in once daily, twice
daily, and thrice daily fractions of 1.8, 1.2 to 1.5 Gy, and 1.0
Gy, respectively. Radiation therapy was administered to the primary
site with generous margins. Miki et al (5) reported a prescribed dose of 70 Gy for
all patients in 2.0–2.5 Gy fractions; docetaxel was administered
concurrently in some patients and extended local or whole-scalp
fields were used. For extended local fields, the gross tumor volume
was expanded with margins of ≥2.5 cm to form the clinical target
volume. The planning target volume contained the clinical target
volume with a margin of at least 0.5 cm. Radiation was delivered to
the primary lesion using 6–12 MeV electron beams. Fujisawa et
al (6) reported a typical
radiotherapy dose between 60 and 70 Gy, with a median dose of 70
Gy. Docetaxel or paclitaxel was administered concurrently in some
patients. The irradiation fields encompassed a 2–3 cm margin from
either the tumor or surgical margin. Ito et al (7) reported a radiotherapy dose of 45–85 Gy
(mean 67.5 Gy). Sasaki et al (8) reported a radiotherapy dose of 30–100 Gy
(median 68 Gy). The radiation fields were determined on the basis
of tumor extension, with a safety margin of ≥3 cm. Electron, X-ray,
or telecobalt beams were used. Ohguri et al (9) reported a median radiation dose of 70.3
Gy with fractions of 2 or 3 Gy. Radiation was delivered using 6–12
MeV electron beams. In most patients, a radiation dose of 50–60 Gy
was administered using various techniques to encompass the tumor
extension with a safety margin of >3 cm; a 10–20 Gy boost dose
was also delivered to the tumor. Ogawa et al (10) reported a total radiation dose of
26–71.6 Gy (median 60 Gy), with daily fractions of 1.8–2.0 or 3–4
Gy. The planning target volume included 3–5 cm margins for the
clinical target volume. Radiotherapy was delivered using 6–12-MeV
electron or 4-MV X-ray beams. None of the 14 patients who received
≥70 Gy had in-field recurrences. Perez et al (11) reported a strategy that administered
preoperative radiation doses of 50 Gy, postoperative doses of 60
Gy, and doses to bulky disease between 66 and 70 Gy. Patel et
al (12) reported doses of 40–70
Gy (median 60 Gy) in 10–35 fractions. Radiotherapy was delivered by
electrons or megavoltage photons. Pawlik et al (13) reported total scalp radiotherapy using
electron beams at a total dose of 60–72 Gy. Suzuki et al
(14) reported a total dose of
60–100 Gy (median 70 Gy) and a median dose per fraction of 2.0 Gy.
The primary tumor and all satellite lesions were included with a
3–5 cm margin. Radiotherapy was delivered using 5–9 MeV electron
beams. In our study, the prescribed dose was 60 or 70 Gy in 2.0-Gy
fractions. Although we cannot propose the optimal radiation dose,
we believe that doses of 60 to 70 Gy are acceptable and relatively
well tolerated by patients. Total scalp radiotherapy was sometimes
used in accordance with several previous reports (2,13).
Bernstein et al (2) reported
that total scalp radiotherapy was not a significant factor for
locoregional control, recurrence-free survival, and OS. Miki et
al (5) also reported that
whole-scalp fields were not a significant factor for OS. In our
study, in cases where the first site of recurrence was only local,
all the sites of the first local recurrence were within the
radiation field. We speculate that total scalp radiotherapy may be
unnecessary in cases where adequate margins are taken around the
tumor, and when dermatologists are able to clearly define the
extent of disease.
The present study has several limitations. First, it
was a retrospective study conducted in a single institution, and
the relatively short median follow-up period of 15 months may have
been inadequate to accurately detect local tumor progression and
late adverse events. Second, the number of patients was small.
Therefore, we could not perform a multivariate analysis. Moreover,
patients who received CCRT with maintenance chemotherapy may have
had better physical status than those who did not receive CCRT with
maintenance chemotherapy. This might have influenced the PFS, OS,
LC, and DMFS. Third, the heterogeneity of the treatment may have
influenced the generalizability of the results. Fourth, the effects
of surgery and IL-2 were not properly investigated because only a
small number of patients received them (only 2 patients underwent
surgery and 4 received IL-2). Finally, several new drugs such as
pazopanib and pembrolizumab have been recently developed (19,20); the
impact of these new drugs on angiosarcoma was not evaluated in our
study because only 1 patient received pazopanib. This patient was
initially treated with paclitaxel during and after the radiation
therapy, but was switched over to docetaxel after recurrence of
lung metastases. Subsequently, pazopanib was used because docetaxel
was ineffective. The patient died of angiosarcoma approximately 5
months after the initiation of pazopanib.
In conclusion, CCRT with maintenance chemotherapy
using taxanes may be effective in treating localized angiosarcomas
of the scalp without cervical lymph node metastases; this may be
particularly useful for preventing distant metastases. Further
prospective multicenter studies are required to validate our
findings and determine the optimal treatment modalities for
localized angiosarcomas of the scalp.
Acknowledgements
The abstract was presented at ESTRO 36 on May 5–9,
2017 in Vienna, Austria and published as abstract no. EP-1377 in
Radiother Oncol 123 (Suppl 1): S738, 2017.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
HI contributed to the study design, data collection,
analysis and interpretation, and writing the manuscript. HI, KK, TW
and NK were responsible for radiation therapy. TK, TM and OY
performed the patient follow-up and were responsible for conducting
the other treatments including chemotherapy scheduling. HM
contributed to the study design, and data analysis and
interpretation. MK, SM, and SK contributed to the study design and
reviewing the manuscript. All authors read and approved the
manuscript.
Ethics approval and consent to
participate
The present study was approved by Okayama University
Hospital Institutional Review Board (approval no. K1610-503), and
the requirement for informed consent was waived owing to the
retrospective nature of the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mendenhall WM, Mendenhall CM, Werning JW,
Reith JD and Mendenhall NP: Cutaneous angiosarcoma. Am J Clin
Oncol. 29:524–528. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bernstein JM, Irish JC, Brown DH,
Goldstein D, Chung P, Razak ARA, Catton C, Gilbert RW, Gullane PJ
and O'Sullivan B: Survival outcomes for cutaneous angiosarcoma of
the scalp versus face. Head Neck. 39:1205–1211. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ward JR, Feigenberg SJ, Mendenhall NP,
Marcus RB Jr and Mendenhall WM: Radiation therapy for angiosarcoma.
Head Neck. 25:873–878. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shin JY, Roh SG, Lee NH and Yang KM:
Predisposing factors for poor prognosis of angiosarcoma of the
scalp and face: Systematic review and meta-analysis. Head Neck.
39:380–386. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Miki Y, Tada T, Kamo R, Hosono MN, Tamiya
H, Shimatani Y, Tsutsumi S, Ogino R and MIKI Y: Single
institutional experience of the treatment of angiosarcoma of the
face and scalp. Br J Radiol. 86:201304392013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fujisawa Y, Yoshino K, Kadono T, Miyagawa
T, Nakamura Y and Fujimoto M: Chemoradiotherapy with taxane is
superior to conventional surgery and radiotherapy in the management
of cutaneous angiosarcoma: A multicentre, retrospective study. Br J
Dermatol. 171:1493–1500. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ito T, Uchi H, Nakahara T, Tsuji G, Oda Y,
Hagihara A and Furue M: Cutaneous angiosarcoma of the head and
face: A single-center analysis of treatment outcomes in 43 patients
in Japan. J Cancer Res Clin Oncol. 142:1387–1394. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sasaki R, Soejima T, Kishi K, Imajo Y,
Hirota S, Kamikonya N, Murakami M, Kawabe T, Ejima Y, Matsumoto A
and Sugimura K: Angiosarcoma treated with radiotherapy: Impact of
tumor type and size on outcome. Int J Radiat Oncol Biol Phys.
52:1032–1040. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ohguri T, Imada H, Nomoto S, Yahara K,
Hisaoka M, Hashimoto H, Tokura Y, Nakamura K, Shioyama Y, Honda H,
et al: Angiosarcoma of the scalp treated with curative radiotherapy
plus recombinant interleukin-2 immunotherapy. Int J Radiat Oncol
Biol Phys. 61:1446–1453. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ogawa K, Takahashi K, Asato Y, Yamamoto Y,
Taira K, Matori S, Iraha S, Yagi N, Yogi A, Haranaga S, et al:
Treatment and prognosis of angiosarcoma of the scalp and face: A
retrospective analysis of 48 patients. Br J Radiol. 85:e1127–e1133.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Perez MC, Padhya TA, Messina JL, Jackson
RS, Gonzalez RJ, Bui MM, Letson GD, Cruse CW, Lavey RS, Cheong D,
et al: Cutaneous angiosarcoma: A single-institution experience. Ann
Surg Oncol. 20:3391–3397. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Patel SH, Hayden RE, Hinni ML, Wong WW,
Foote RL, Milani S, Wu Q, Ko SJ and Halyard MY: Angiosarcoma of the
scalp and face: The Mayo Clinic experience. JAMA Otolaryngol Head
and Neck Surg. 141:335–340. 2015. View Article : Google Scholar
|
|
13
|
Pawlik TM, Paulino AF, Mcginn CJ, Baker
LH, Cohen DS, Morris JS, Rees R and Sondak VK: Cutaneous
angiosarcoma of the scalp: A multidisciplinary approach. Cancer.
98:1716–1726. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Suzuki G, Yamazaki H, Takenaka H, Aibe N,
Masui K, Kimoto T, Takekawa K, Nakashima A, Takenaka T, Asai J, et
al: Definitive radiation therapy for angiosarcoma of the face and
scalp. In Vivo. 30:921–926. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fata F, O'Reilly E, Ilson D, Pfister D,
Leffel D, Kelsen DP, Schwartz GK and Casper ES: Paclitaxel in the
treatment of patients with angiosarcoma of the scalp or face.
Cancer. 86:2034–2037. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Isogai R, Kawada A, Aragane Y and Tezuka
T: Successful treatment of pulmonary metastasis and local
recurrence of angiosarcoma with docetaxel. J Dermatol. 31:335–341.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nagano T, Yamada Y, Ikeda T, Kanki H, Kamo
T and Nishigori C: Docetaxel: A therapeutic option in the treatment
of cutaneous angiosarcoma: Report of 9 patients. Cancer.
110:648–651. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Penel N, Bui BN, Bay JO, Cupissol D,
Ray-Coquard I, Piperno-Neumann S, Kerbrat P, Fournier C, Taieb S,
Jimenez M, et al: Phase II trial of weekly paclitaxel for
unresectable angiosarcoma: The ANGIOTAX Study. J Clin Oncol.
26:5269–5274. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Van der Graaf WT, Blay JY, Chawla SP, Kim
DW, Bui-Nguyen B, Casali PG, Schöffski P, Aglietta M, Staddon AP,
Beppu Y, et al: Pazopanib for metastatic soft-tissue sarcoma
(PALETTE): A randomised, double-blind, placebo-controlled phase 3
trial. Lancet. 379:1879–1886. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sindhu S, Gimber LH, Cranmer L, McBride A
and Kraft AS: Angiosarcoma treated successfully with anti-PD-1
therapy-a case report. J Immunother Cancer. 5:582017. View Article : Google Scholar : PubMed/NCBI
|