Introduction
Vascular neoplasms of the testis and its adnexa are
uncommon. Testicular cavernous hemangioma is a benign vascular
neoplasm that may arise either within the testicular parenchyma
(intratesticular) or from adnexal structures of the testis
(extratesticular) (1,2). In addition, testicular cavernous
hemangiomas originating from the spermatic cord (3) and scrotum (4) have been reported. Overall, cavernous
hemangiomas developing in the external genitalia are an infrequent
occurrence, and cavernous hemangioma of the testis is extremely
rare (5). This type of tumor may be
encountered at any age, from fetuses of 17 weeks to patients aged
77 years (6), and its progression is
slow (7). The aim of the present
study was to report a rare case of a testicular cavernous
hemangioma in an adult manifesting with an acute onset.
Case report
A 23-year-old male patient presented with a tender
right scrotal swelling for 7 days in June 2018. The patient had
been seen by local physician and treated for epididymitis with
antibiotics and scrotal support. However, the testicular pain
persisted and the patient was referred to the andrology clinic of
the First Hospital of Jilin University. The patient's medical
history was unremarkable, and he had no previous history of trauma
or infection. However, he reported an accidental blunt trauma to
the scrotum 2 weeks earlier, with transient scrotal pain. On
physical examination, a solid, tender, edematous mass was
identified, measuring 20x20 mm, without transillumination. The
tumor presented as a soft, spongy, non-pulsatile, painless,
irregularly lobulated mass, not involving the ipsilateral
epididymis or spermatic cord.
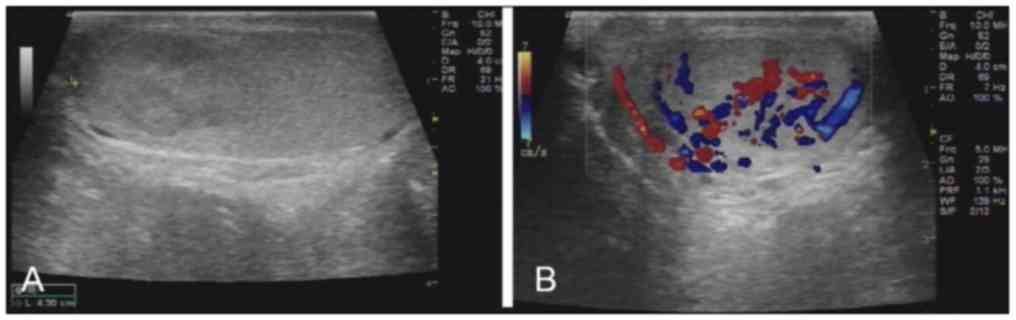
With clinical suspicion of testicular torsion, the
patient was subjected to ultrasound examination, which demonstrated
a hypoechoic lesion in the upper pole of the right testicle, with
poorly demarcated margins and abundant blood flow (Fig. 1). No calcifications, fibrosis or
necrotic foci were found in the area of the lesion. There was no
extension to the perineum or groin, and no regional
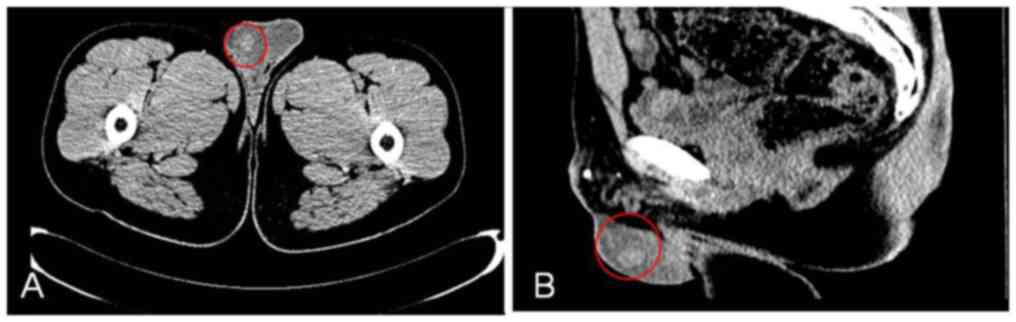
lymphadenopathy. Computed tomography examination clearly
demonstrated a solitary tumor of the right testis (Fig. 2). The laboratory examinations,
including relevant tumor markers, particularly α-fetoprotein (2.31
ng/ml; normal range, <20 ng/ml), β-human chorionic gonadotropin
(0.11 ng/ml; normal range, <4 ng/ml) and serum lactate
dehydrogenase (171 U/l; normal range, 120-150 U/l) were normal.
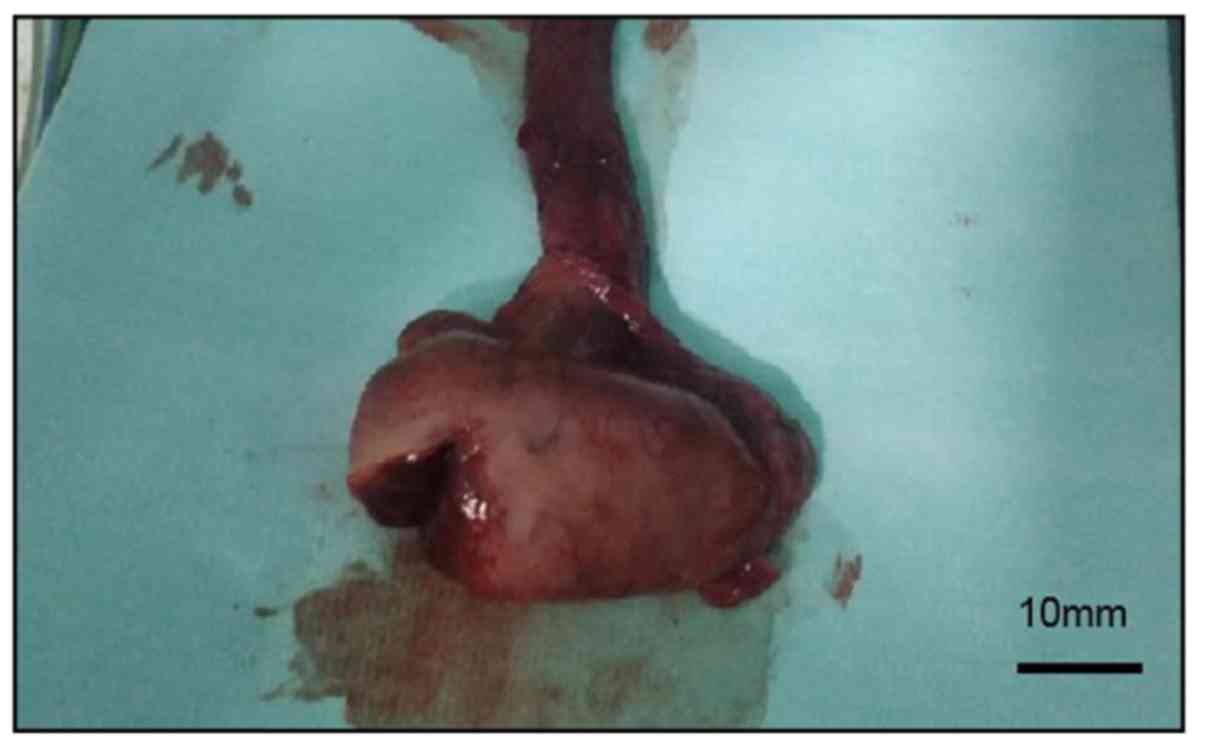
The patient was diagnosed with a testicular tumor
and a right inguinal incision was performed to access the spermatic
cord and separate the right testis, together with the tunica
vaginalis, from the scrotum. Intraoperatively, a solid, richly
vascular tumor, sized 30x20x20 mm, was identified on the upper pole
of right testis (Fig. 3). The
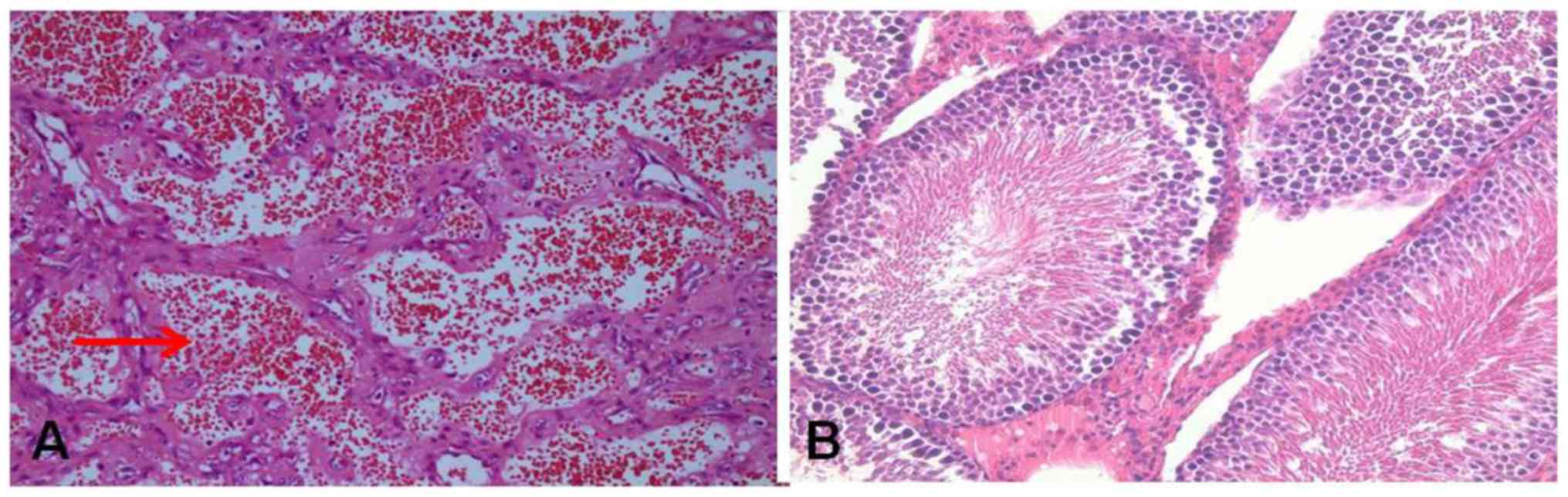
histopathological examination confirmed that the tumor was mainly
composed of vascular lumina and thromboses, consistent with the
diagnosis of testicular cavernous hemangioma (Fig. 4). The patient was discharged 1 week
later, and remained free of complications and recurrence at the
1-year flow-up.
Discussion
Hemangioma is a type of the benign vascular tumor
that may develop in any part of the body. In the pediatric
population, hemangiomas located in the head and neck account for
60%, with 25% found in the truck and 15% in the extremities,
whereas only 2% of hemangiomas develop in the genitalia (4,8). After
Kleiman first reported a case of testicular hemangioma in
1944(9), ~50 cases of hemangiomas of
the testis have been reported. Four histological types of
hemangioma of the testis have been reported to date: Cavernous
hemangiomas, capillary hemangiomas, histiocytoid and papillary
endothelial hyperplasia. These occur in diverse age groups, but are
most commonly encountered in children and adolescents. The youngest
reported patient was a 1-month-old infant (10) and the oldest case was a 77 year-old
man (7). Cavernous hemangiomas of
the testis primarily present during childhood. Their clinical
presentation varies from a painless testicular enlargement to
painful testicular infarction (8,11). Thus,
the diagnosis is usually established only following inguinal
orchiectomy. We herein describe the case of an adult patient
presenting with acute onset of testicular enlargement and pain,
which may be due to intratesticular bleeding caused by blunt
testicular injury.
The differential diagnosis must include germ cell
tumors (e.g., seminoma and teratoma), adenomatoid tumor and
sex-cord stromal tumors, such as Sertoli cell tumor. Sonography is
the primary modality used for imaging scrotal lesions. On
sonographic examination, these tumors may present as hypoechoic,
hyperechoic, or mixed echogenic masses, which may be either well or
poorly defined. Color Doppler patterns may vary among different
types of hemangiomas (capillary, cavernous or venous), as some
hemangiomas display slower flow or a lesser degree of vascular
pooling. Extensive hypervascularity and areas of low-resistance
velocity on spectral Doppler imaging are considered to be
suggestive of hemangioma (12).
Furthermore, a testicular mass with various-sized calcifications is
a characteristic presentation of testicular hemangioma (3). The calcifications may be phleboliths
that frequently form in the dilated venous spaces of a cavernous
hemangioma, or represent stromal calcifications (13). In the present case, there was no
evidence of intratesticular calcification, and no thrombosis or
calcification were detected on pathological examination. Thus, it
may be difficult to distinguish this tumor from testicular
carcinoma preoperatively using only these modalities. In addition,
contrast-enhanced ultrasound (CEUS) has been suggested as an
adjunctive tool for testicular imaging. CEUS is characterized by
nodular enhancement around the arterial phase, progressive
centripetal filling, and hyperechoic/isoechoic changes in the
portal and delayed phases in CEUS images.
The available treatment options for testicular
hemangioma include surgical excision, vessel ligation,
intralesional sclerotherapy, radiation, intravascular steroid,
laser fulguration, cryotherapy and orchiectomy (14,15). The
complications of testicular cavernous hemangioma include further
enlargement, rupture, hemorrhage, infection, torsion, infarction
and infertility. Intraoperative frozen section examination should
be performed, as it is helpful for performing testicle-sparing
surgery. All reported vascular testicular tumors have exhibited
benign clinical behavior, without local recurrence or
metastasis.
In conclusion, testicular cavernous hemangioma is an
extremely rare disease, and its clinical presentation and findings
on examination are similar with those of malignant testicular
tumors, which may lead to diagnostic difficulties. Scrotal injury
may trigger the onset of testicular swelling or pain. When dealing
with a testicular mass in a patient without serum elevations of
β-human chorionic gonadotropin or α-fetoprotein, and ultrasound
examination showing a mass with vascular proliferation, with or
without calcifications, testicular cavernous hemangioma should be
considered in the differential diagnosis.
Acknowledgements
Not applicable.
Funding
The present study was partially supported by the
Jilin Finance Science Foundation (grant. no. JLSCZD2019-001)..
Availability of data and materials
All data generated or analyzed during the present
study are included in the published article.
Authors' contributions
FL and SX performed the surgery. LL, ZL, DC and HW
provided medical care for the patients and collected the data. SH
collected the data and revised the manuscript. KG wrote this
manuscript ansd analyzed all of the data. LL, ZL and DC provided
medical care for the patients and collected the data. All the
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics Review
Committee of The First Hospital of Jilin University.
Patient consent for publication
The patient provided written informed consent for
the publication of the case details and associated images.
Competing interests
All the authors declare that they have no competing
interests.
References
|
1
|
Erdag G, Kwon EO, Lizza EF and Shevchuk M:
Cavernous hemangioma of tunica albuginea testis manifesting as
testicular pain. Urology. 68:673.e13–5. 2006.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chetty R, Bandid S and Freedman D:
Cavernous haemangioma of the epididymis mimicking a testicular
malignancy. Aust N Z J Surg. 63:235–237. 1993.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Jeon YS, Cho SG, Kim WH and Choi SJ:
Cavernous haemangioma of the spermatic cord in a child. Pediatr
Radiol. 36:1323–1325. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ergün O, Ceylan BG, Armagan A, Kapucuoglu
N, Ceyhan AM and Perk H: A giant scrotal cavernous hemangioma
extending to the penis and perineum: A case report. Kaohsiung J Med
Sci. 25:559–561. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Liu B, Chen J, Luo J, Zhou F, Wang C and
Xie L: Cavernous hemangioma of the testis mimicking a testicular
teratoma. Exp Ther Med. 6:91–92. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Suriawinata A, Talerman A, Vapnek JM and
Unger P: Hemangioma of the testis: Report of unusual occurrences of
cavernous hemangioma in a fetus and capillary hemangioma in an
older man. Ann Diagn Pathol. 5:80–83. 2001.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Frank RG, Lowry P and Ongcapin EH: Images
in clinical urology. Venous cavernous hemangioma of the testis.
Urology. 52:709–710. 1998.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tepeneu NF, Krafka K, Meglic S, Rogatsch H
and Fasching G: Testicular cavernous hemangioma associated with
testicular torsion-case report and review of literature. Int J Surg
Case Rep. 49:247–250. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kleiman AH: Hemangioma of the testis. J
Urol. 51:548–550. 1944.
|
|
10
|
Manoney MT: Cavernous hemangioma of the
scrotal septum. J Pediatr. 49:744–745. 1956.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fossum BD, Woods JC and Blight EM Jr:
Cavernous hemangioma of testis causing acute testicular infarction.
Urology. 18:277–278. 1981.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ricci Z, Koenigsberg M and Whitney K:
Sonography of an arteriovenous-type hemangioma of the testis. AJR
Am J Roentgenol. 174:1581–1582. 2000.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Venkatanarasimha N, McCormick F and
Freeman SJ: Cavernous hemangioma of the testis. J Ultrasound Med.
29:859–860. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ray B and Clark SS: Hemangioma of scrotum.
Urology. 8:502–505. 1976.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Naveed S, Quari H and Sharma H: Cavernous
haemangioma of the testis mimicking testicular malignancy in an
adolescent. Scott Med J. 58:e5–e7. 2013.PubMed/NCBI View Article : Google Scholar
|