Introduction
Testicular cancer represents 5% of all urological
tumors worldwide. According to the GLOBOCAN 2018 database, the
global age-standardized incidence rate (ASIR) of testicular cancer
is 1.7 cases per 100,000 individuals, with the highest ASIRs in
Europe (6.2 in 100,000) and Oceania (5.4 in 100,000) and the lowest
in the Africa (0.35 in 100,000) (1).
Recent increases in the availability of effective treatments have
subsequently led to a rise in the likelihood of patients being
successfully cured from testicular cancer. Although the incident
rates of testicular cancer appear to be low, effective treatment
for patients is nonetheless important. Research aimedtime
consolidating the data from different treatments may help to pave
the way for more efficient treatments and higher cure success
rates.
Patients diagnosed with stage I and II testicular
cancer are typically informed of all the available treatments.
These include surveillance, adjuvant chemotherapy and radiotherapy
after orchiectomy. Orchiectomy is the default treatment
administered to low stage patients. Chemotherapy, however, is
recommended to patients with stage Ⅲ testicular cancer.
Records from the Surveillance, Epidemiology &
End Results (SEER) database reveal that approximately 11.6% of
testicular cancer patients during the years 2000 to 2015 were
reported to have stage III of the disease with distant metastasis
as their initial diagnosis. Although some studies identify
preclinical and clinical factors as markers for treatment outcomes
(2-4); no
prior study has been conducted to evaluate the effectiveness of
surgical treatment to the primary lesion of patients with stage Ⅲ
testicular cancer, but the effectiveness of locoregional surgery
has been reported in other types of cancer, such as breast cancer
(5). For further insight into the
effects of removing a primary tumor, we conducted a
population-based study using data from the National Cancer
Institute's SEER program database.
Patients and methods
Data acquisition and population
study
The SEER database used in this study contains data
that represents approximately 28% of the population of the United
States of America. The database was used to obtain comprehensive
data on 54,944 men diagnosed with testicular cancer between 1973
and 2015. Patients staged at M1 (M1a and M1b) based on the 7th AJCC
staging system were included in this study. The final cohort
included 1,577 primary metastatic testicular cancer (pMTC) patients
diagnosed from 2010 to 2015. And we held a retrospective analysis
on them. These data were obtained from SEER datasets on 16th May,
2019 by SEER Statistics Software.
Patient records were then categorized into two
groups viz; surgery and non-surgery, based on whether the patient
had undergone locoregional surgery after their diagnosis. The data
was then further sub-categorized according to the patients' age,
race, marital status, T stage, lymph node status, histological
type, molecular subtypes, distant metastasis status, radiation and
chemotherapy recode.
The demographic sub-categories included: i)
Fourty-five and older than 45 and younger than 45 ; ii) white and
non-white and iii) married and others.
Based on the 7th AJCC staging system, the T stage
categories used were T1+T2, T3+T4 and TX+T0.
In addition to the patients at a N stage, patients
staged at N0 were categorized as lymph node negative with the
remaining records as lymph node positive.
Pathological type was divided into two groups,
seminoma and non-seminoma.
Molecular subtypes (AFP, HCG and LDH) were divided
based on the whether the value was normal or not.
Distant metastasis was divided into the metastatic
organs that were identified in the SEER database.
Lastly, the radiation therapy and chemotherapy
categories were divided into groups that had received the treatment
and those that did not.
Statistical analysis
The distribution differences between locoregional
surgery and demographic information were analyzed using the
Chi-square test. Kaplan-Meier survival curves were used to describe
differences in predicting the probability of testicular cancer
specific survival (TCSS) and overall survival (OS) whilst log-rank
tests were used to determine statistical significance.
Univariate analysis was conducted using the log-rank
test and 95% confidence intervals (95% CIs) were calculated. For
variables that emerged as statistically significant in the
univariate analysis; multivariate Cox's proportion hazard
regression analysis was employed to evaluate the statistical
significance for the survival probability of each substage. To
further compensate for potential baseline bias, 1:2 propensity
score matching (PSM) was performed by R package. All statistical
analyses were performed using SPSS 22 (IBM Corp.) software.
P<0.05, was considered to be statistically significant.
Results
Characteristics of the patients
Of the 1,577 patients who were diagnosed with pMTC
between 2010 and 2015, 1,285 (81.5%) of them underwent testicular
surgery, while 292 (18.5%) did not. As can be seen from Table I, the median age of patients in the
sample diagnosed with testicular cancer is 59, indicating diagnosis
at neither a young nor very senior age. Analysis on race and
marital status reveals non-white and married groups as the
minority.
 | Table ICharacteristics of patients diagnosed
with primary metastatic testis cancer included in SEER database
between 2010 with 2015. |
Table I
Characteristics of patients diagnosed
with primary metastatic testis cancer included in SEER database
between 2010 with 2015.
| | Before PSM | After PSM |
|---|
| Characteristics | All, n | No surgery, n | Surgery, n | P-value | All, n | No surgery, n | Surgery, n | P-value |
|---|
| Age, years | | | | | | | | |
|
<45 | 1,263 | 198 | 1,065 | <0.001 | 631 | 198 | 433 | 0.055 |
|
≥45 | 314 | 94 | 220 | | 245 | 94 | 151 | |
| Ethnicity | | | | | | | | |
|
White | 1,427 | 255 | 1,172 | 0.047 | 779 | 255 | 524 | 0.305 |
|
Others | 150 | 37 | 113 | | 97 | 37 | 60 | |
| Marital status | | | | | | | | |
|
Others | 1,129 | 192 | 937 | 0.018 | 628 | 192 | 436 | 0.007 |
|
Married | 448 | 100 | 348 | | 248 | 100 | 148 | |
| T stage | | | | | | | | |
|
T1+T2 | 914 | 0 | 914 | <0.001 | 213 | 0 | 213 | <0.001 |
|
T3+T4 | 298 | 18 | 280 | | 298 | 18 | 280 | |
|
TX+T0 | 365 | 274 | 91 | | 365 | 274 | 91 | |
| Lymph node
status | | | | | | | | |
|
Negative | 446 | 88 | 358 | 0.430 | 247 | 88 | 159 | 0.381 |
|
Positive | 1,131 | 204 | 927 | | 629 | 204 | 425 | |
| Histological
type | | | | | | | | |
|
Seminoma | 493 | 145 | 348 | <0.001 | 306 | 145 | 161 | <0.001 |
|
Non-seminoma | 1,084 | 147 | 937 | | 570 | 147 | 423 | |
| AFP | | | | | | | | |
|
Normal | 428 | 59 | 369 | <0.001 | 190 | 59 | 131 | 0.003 |
|
Unnormal | 401 | 41 | 360 | | 173 | 41 | 132 | |
|
Unknown | 748 | 192 | 556 | | 513 | 192 | 321 | |
| HCG | | | | | | | | |
|
Normal | 357 | 26 | 331 | <0.001 | 137 | 26 | 111 | <0.001 |
|
Unnormal | 460 | 67 | 393 | | 205 | 67 | 138 | |
|
Unknown | 760 | 199 | 561 | | 534 | 199 | 335 | |
| LDH | | | | | | | | |
|
Normal | 258 | 14 | 244 | <0.001 | 96 | 14 | 82 | <0.001 |
|
Unnormal | 435 | 64 | 371 | | 195 | 64 | 131 | |
|
Unknown | 884 | 214 | 670 | | 585 | 214 | 371 | |
| Distant
metastasis | | | | | | | | |
|
Multiple
sites | 292 | 82 | 210 | <0.001 | 199 | 82 | 117 | <0.001 |
|
Bone
only | 37 | 12 | 25 | | 26 | 12 | 14 | |
|
Liver
only | 61 | 21 | 40 | | 41 | 21 | 20 | |
|
Lung
only | 676 | 67 | 609 | | 318 | 67 | 251 | |
|
Brain
only | 6 | 3 | 3 | | 5 | 3 | 2 | |
| Radiation | | | | | | | | |
|
No | 1,487 | 281 | 1,206 | 0.125 | 836 | 281 | 555 | 0.495 |
|
Yes | 90 | 11 | 79 | | 40 | 11 | 29 | |
| Chemotherapy | | | | | | | | |
|
No | 139 | 49 | 90 | <0.001 | 128 | 49 | 79 | 0.223 |
|
Yes | 1,438 | 243 | 1,195 | | 748 | 243 | 505 | |
Based on 7th AJCC staging records, the number of
patients assigned to the T1+T2 group is > the number assigned to
the T3+T4 group. Most patients in both T1+T2 and T3+T4 groups,
however, were recorded as having had surgery. Compared with the
group of patients who received surgery, the non-surgery group had
fewer patients that were lymph node negative.
A greater proportion of non-seminoma pathological
type patients appear to have had surgery compared to those in the
seminoma group. Although molecular subtypes for about half of the
data are unknown, there is an equal number of normal and abnormal
subtypes among the known cases.
Most patients did not undergo the radiation therapy,
while nearly 90% of them had chemotherapy. Although, PSM was
conducted to reduce the potential bias of the baseline, the
statistically significant differences could not be completely
eliminated with baseline characteristics due to the limited number
of cases available.
Analysis of TCSS and OS
The 5-year OS of testicular cancer is 76.68% for the
surgery group and 62.36% for the non-surgery group. The 5-year TCSS
is 82.35% for the surgery group and 72.13% for the non-surgery
group. The survival trends of the two groups are the same in OS and
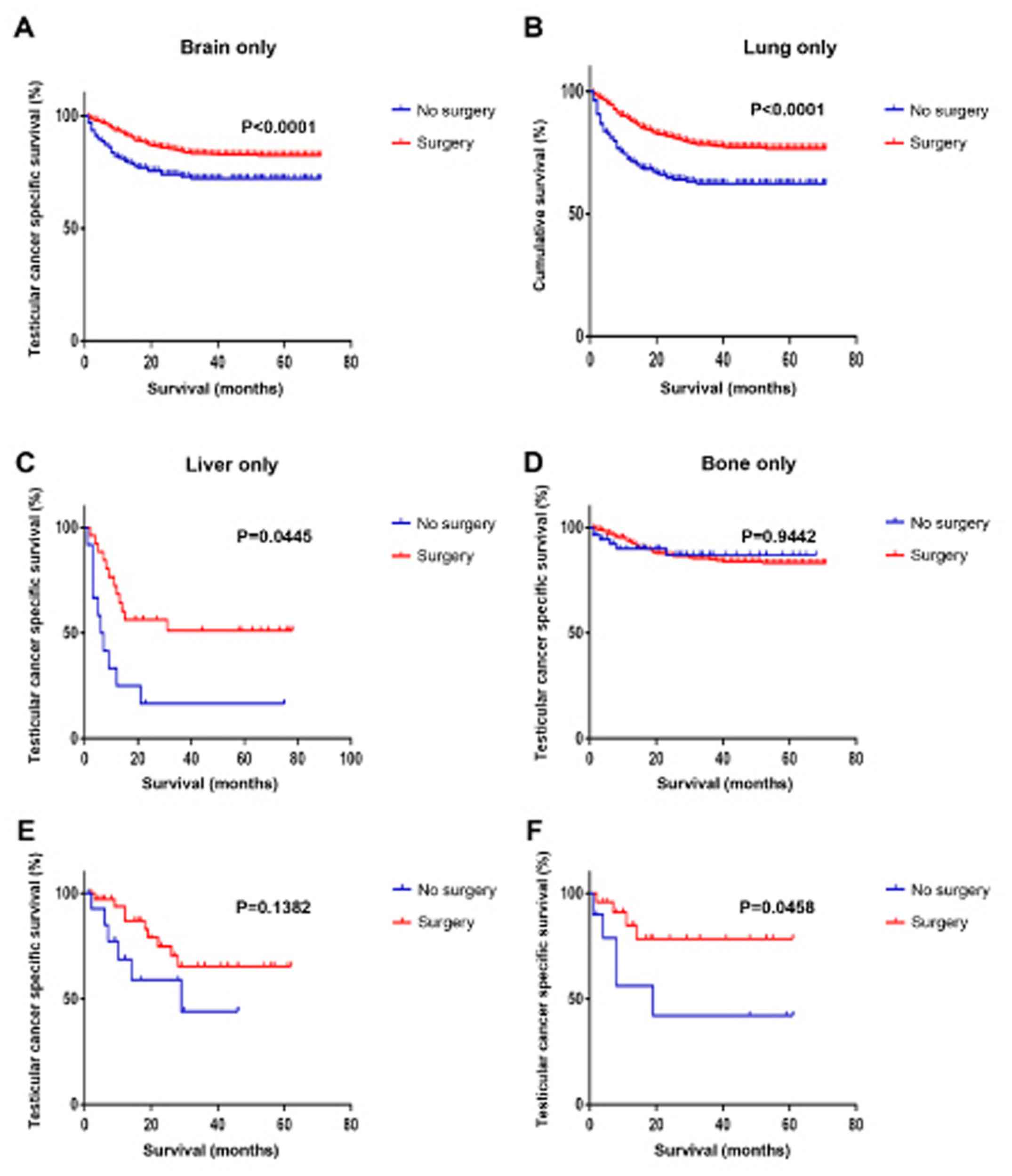
TCSS (Fig. 1A and B).
Data were divided based on the distant organs
involved (bone, liver, lung and brain) in order to decrease the
bias of the site-specific metastasis on survival analysis. Local
orchiectomy of pMTC patients with bone and brain metastasis is
found to prolong the TCSS (P=0.0458; P<0.0001) (Fig. 1C and F). The survival outcome of patients with
lung and liver metastasis, however, is not affected by surgery
(Fig. 1D and E).
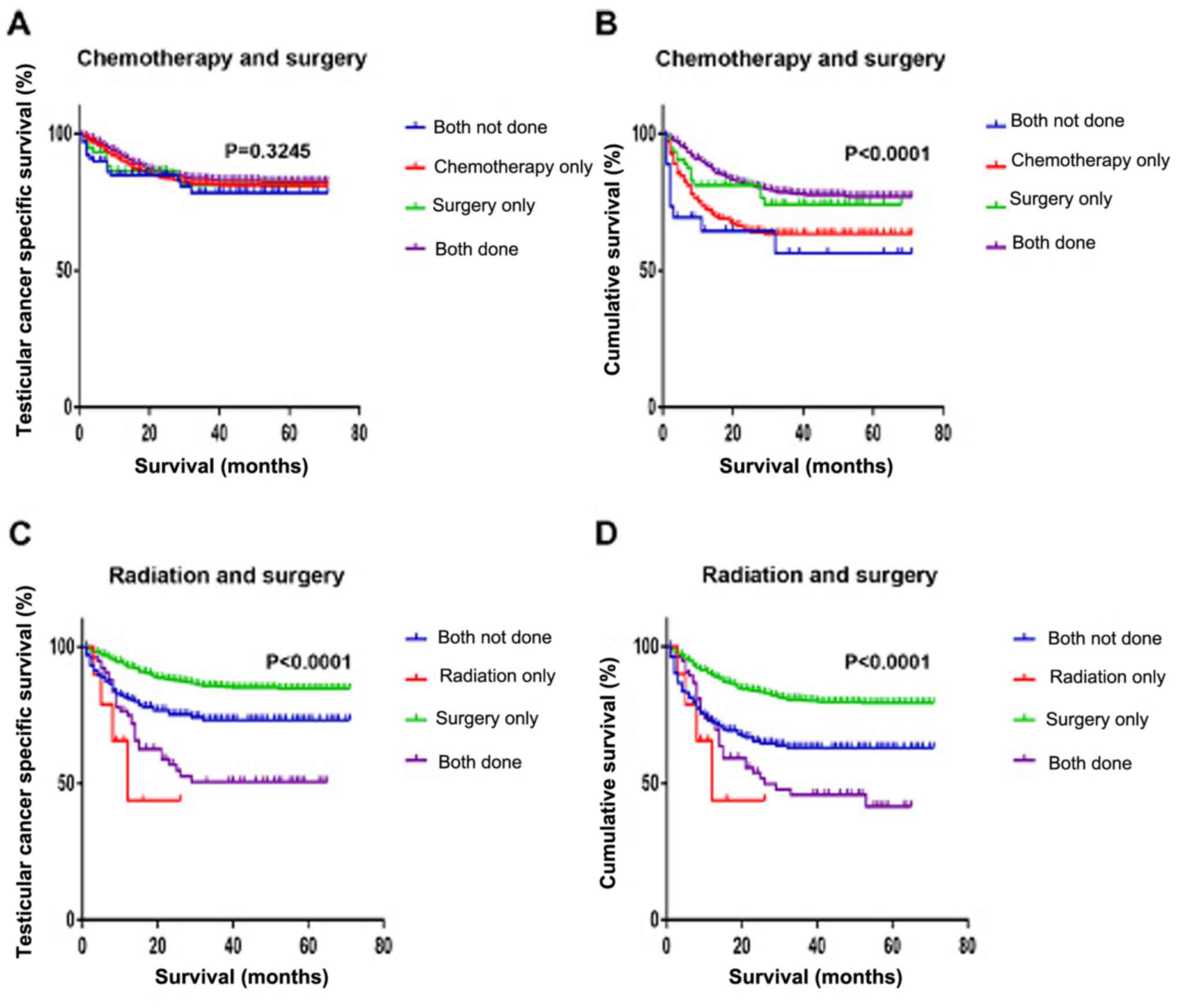
We next analyzed the effects of radiotherapy or
chemotherapy together with local surgery on the survival of
patients with pMTC (Fig. 2).
Expectedly, TCSS appears to be prolonged for patients who receive
surgery as well chemotherapy (P<0.0001) (Fig. 2A and B). Receiving surgery alone, however, seems
to be more favorable to the survival outcomes of patients as
opposed to radiotherapy or radiotherapy in addition to surgery
(Fig. 2C and D).
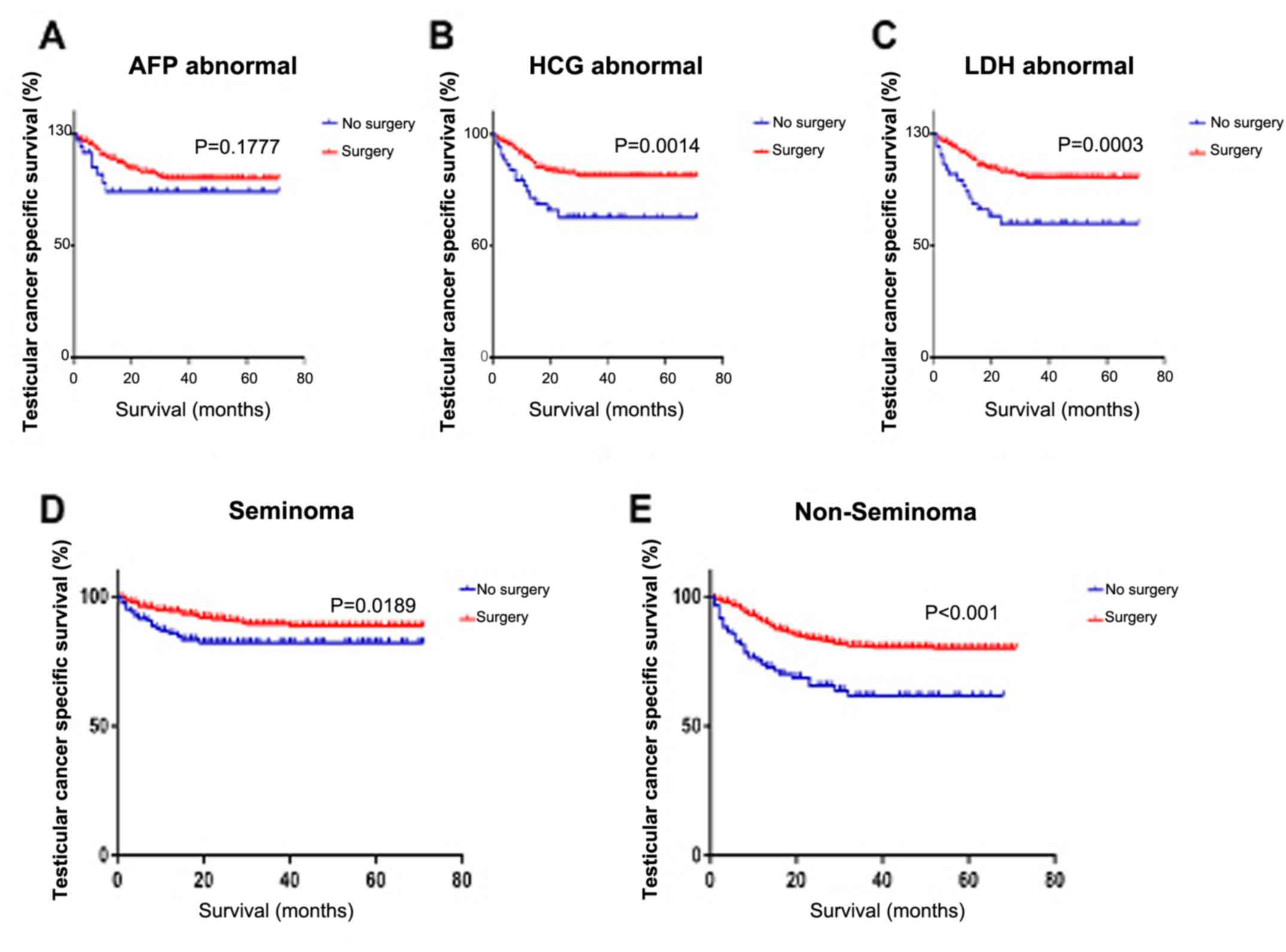
Data stratified on the basis of molecular subtypes
shows that when the values of HCG and LDH are in the abnormal
range, surgery can help to prolong the survival of a patient
(P=0.0014; P=0.0003) (Fig. 3B and
C). Unfortunately, the value of AFP
does not have any significance when it comes to the metastatic
testicular cancer disease (Fig.
3A).
When it comes to pathological type, we have found
that surgery may be beneficial to the survival outcome of patients
with non-seminoma pMTC (Fig. 3E).
For patients with seminoma pMTC, however, surgery may not prolong
the survival (Fig. 3D).
Univariate and multivariate
analysis
In order to reduce the potential confounding and
selection bias, 1:2 PSM procedure was performed, and 872 patients
were enrolled into the propensity model with 292 non-surgery cases
and 584 surgery cases. We then carried out univariate and
multivariate analyses to evaluate the effects of the subdivided
factors on TCSS (Table II). It can
be seen that the risk of pMTC-related death increased with age
(P<0.001).
 | Table IIUnivariate and multivariate analysis
of clinicopathological characteristics and TCSS of patients with
testis cancer. |
Table II
Univariate and multivariate analysis
of clinicopathological characteristics and TCSS of patients with
testis cancer.
| | Before PSM | After PSM |
|---|
| | Univariate
analysis | Multivariate
analysis | Univariate
analysis | Multivariate
analysis |
|---|
|
Characteristics | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age, years | | | | | | | | |
|
<45 | Reference | - | Reference | - | Reference | - | Reference | - |
|
≥45 | 1.699
(1.297-2.227) | <0.001 | 1.718
(1.283-2.302) | <0.001 | 1.342
(0.979-1.841) | 0.068 | - | - |
| Ethnicity | | | | | | | | |
|
White | Reference | - | Reference | - | Reference | - | Reference | - |
|
Others | 1.065
(0.710-1.596) | 0.762 | - | - | 0.711
(0.418-1.207) | 0.206 | - | - |
| Marital status | | | | | | | | |
|
Others | Reference | - | Reference | - | Reference | - | Reference | - |
|
Married | 0.865
(0.656-1.140) | 0.302 | - | - | 0.817
(0.579-1.154) | 0.252 | - | - |
| T stage | | | | | | | | |
|
T1+T2 | Reference | - | Reference | - | Reference | - | Reference | - |
|
T3+T4 | 1.335
(0.968-1.842) | 0.078 | - | - | 1.000
(0.655-1.528) | 0.999 | - | - |
|
TX+T0 | 2.018
(1.530-2.663) | <0.001 | 0.806
(0.450-1.446) | 0.469 | 1.488
(1.007-2.199) | 0.046 | 0.840
(0.428-1.650) | 0.612 |
| Lymph node
status | | | | | | | | |
|
No
metastasis | Reference | - | Reference | - | Reference | - | Reference | - |
|
Metastasis | 1.028
(0.783-1.348) | 0.844 | - | - | 1.011
(0.723-1.414) | 0.949 | - | - |
| Histological
type | | | | | | | | |
|
Seminoma | Reference | - | Reference | - | Reference | - | Reference | - |
|
Non-seminoma | 1.516
(1.140-2.016) | 0.004 | 1.370
(0.994-1.888) | 0.055 | 1.592
(1.131-2.242) | 0.008 | 1.286
(0.881-1.877) | 0.193 |
| AFP | | | | | | | | |
|
Normal | Reference | - | Reference | - | Reference | - | Reference | - |
|
Abnormal | 1.139
(0.927-1.878) | 0.124 | - | - | 1.381
(0.871-2.190) | 0.169 | - | - |
|
Unknown | 1.405
(1.032-1.914) | 0.031 | 0.809
(0.501-1.308) | 0.388 | 1.141
(0.770-1.691) | 0.511 | - | - |
| HCG | | | | | | | | |
|
Normal | Reference | - | Reference | - | Reference | - | Reference | - |
|
Abnormal | 2.312
(1.530-3.493) | <0.001 | 1.845
(1.198-2.843) | 0.005 | 2.104
(1.210-3.659) | 0.008 | 1.622
(0.903-2.916) | 0.106 |
|
Unknown | 2.351
(1.596-3.463) | <0.001 | 2.433
(1.408-4.205) | 0.001 | 1.731
(1.038-2.887) | 0.035 | 1.348
(0.712-2.551) | 0.360 |
| LDH | | | | | | | | |
|
Normal | Reference | - | Reference | - | Reference | - | Reference | - |
|
Abnormal | 1.706
(1.112-2.616) | 0.014 | 1.024
(0.646-1.623) | 0.920 | 2.030
(1.072-3.844) | 0.030 | 1.297
(0.663-2.535) | 0.448 |
|
Unknown | 1.594
(1.072-2.370) | 0.021 | 0.812
(0.489-1.347) | 0.419 | 1.686
(0.931-3.054) | 0.085 | - | - |
| Distant
metastasis | | | | | | | | |
|
Multiple
sites | Reference | - | Reference | - | Reference | - | Reference | - |
|
Bone
only | 0.786
(0.422-1.461) | 0.446 | - | - | 0.902
(0.452-1.801) | 0.771 | - | - |
|
Liver
only | 0.752
(0.456-1.239) | 0.263 | - | - | 0.716
(0.380-1.347) | 0.300 | - | - |
|
Lung
only | 0.264
(0.198-0.352) | <0.001 | 0.344
(0.253-0.467) | <0.001 | 0.339
(0.237-0.485) | <0.001 | 0.382
(0.261-0.559) | <0.001 |
|
Brain
only | 0.529
(0.074-3.793) | 0.527 | - | - | 0.557
(0.077-4.006) | 0.561 | - | - |
| Radiation | | | | | | | | |
|
No | Reference | - | Reference | - | Reference | - | Reference | - |
|
Yes | 2.873
(2.020-4.086) | <0.001 | 2.142
(1.468-3.126) | <0.001 | 2.280
(1.362-3.817) | 0.002 | 1.853
(1.083-3.172) | 0.024 |
| Chemotherapy | | | | | | | | |
|
No | Reference | - | Reference | - | Reference | - | Reference | - |
|
Yes | 0.393
(0.279-0.552) | <0.001 | 0.393
(0.273-0.565) | <0.001 | 0.439
(0.306-0.631) | <0.001 | 0.320
(0.215-0.476) | <0.001 |
| Primary
surgery | | | | | | | | |
|
No | Reference | - | Reference | - | Reference | - | Reference | - |
|
Yes | 0.390
(0.300-0.507) | <0.001 | 0.363
(0.204-0.645) | 0.001 | 0.461
(0.342-0.622) | <0.001 | 0.338
(0.186-0.611) | <0.001 |
Based on the molecular subtype, compared to the
normal range of HCG, the abnormal group showed a higher mortality
risk (P=0.005). Interestingly, compared to multiple distant
metastasis, patients are at a lower mortality risk when the
metastatic organ is only the lung (P<0.001).
Chemotherapy and local surgery can reduce mortality
risk (P<0.001, P<0.001). Only radiotherapy, however, may
accelerate mortality (P<0.001). After PSM, lung metastasis,
chemotherapy and local surgery are still the independent predictive
factors of pMTC. Local testicular surgery dramatically improved the
survival of patients, reducing the MTC-related mortality rate by
about 64%. After PSM, the rate of MTC-related mortality is reduced
by nearly 66% with local surgery. Meanwhile, chemotherapy seems to
be as effective as surgery.
Discussion
Patients diagnosed with metastatic testicular cancer
have a poorer survival rate than those with a localized disease.
This difference, however, disappears for patients after having
survived 3 years from diagnosis (6).
The age-adjusted five-year survival has been calculated to be 97.3%
in Europe (7). The International
Germ Cell Cancer Collaborative Group (IGCCCG) classified the
metastatic testicular cancer into good, intermediate and poor-risk
groups. The five-year survival rates of these groups were reported
as 90, 75 and 45%, respectively (8).
In our study, the five-year TCSS rate is 82.35% in the surgery
group and 72.13% in the non-surgery group.
There are well-established risk factors for
testicular cancer, including a history of cryptorchidism, personal
or family history of testicular cancer disease, age and ethnicity
(9). Based on our findings however,
ethnicity seems to not be a risk factor in contracting metastatic
testicular cancer. In addition, infertility and infection with the
human immunodeficiency virus/AIDS increases the risk of testicular
cancer (9,10). In the present study, only lung
metastasis, chemotherapy and local surgery are predictive factors
for cancer specific survival. Compared to multiple metastasis,
patients with only lung metastasis showed better prognosis.
Obvious symptoms allow for testicular cancer to be
diagnosed at an early stage. Chest radiography and abdominal/pelvic
computed tomography (CT) should however, be performed to check for
metastasis. Experienced physicians always take metastasis into
consideration.
Chemotherapy is generally the first treatment choice
of physicians when dealing with metastatic patients. Appropriate
treatment is defined as three cycles of bleomycin, etoposide, and
cisplatin (BEP), four cycles of etoposide and cisplatin (EP), or
three cycles of etoposide, ifosfamide, and cisplatin (VIP)
chemotherapy for men with good IGCCC risk classification, and four
cycles of either BEP or VIP chemotherapy for intermediate or poor
IGCCC risk classification (11,12).
Chemotoxicity, however, is an inevitable
complication. This may manifest as cardiovascular disease,
pulmonary toxicity, nephrotoxicity, ototoxicity or peripheral
neuropathy (13). Fung et al
(14) found a five-fold increase in
the risk of cardiovascular mortality within the first year after
chemotherapy compared with orchiectomy alone.
Radiotherapy has been recognized as a risk factor
for secondary cancers. There is a reported three-fold increase in
the risk of leukemia among patients with testicular cancer after
radiotherapy (14). In this study,
radiotherapy appears as a risk factor for mortality among
metastatic testicular cancer patients. To our knowledge, the
accelerated mortality may either be linked to a second primary
cancer or it may be that radiotherapy is not effective in
controlling the tumor growth. In this study, local resection was
found to be a better choice for metastatic patients.
Surgery was found to prolong the survival of
patients better than chemotherapy alone. Although the difference is
not very apparent, the combination of surgery and chemotherapy
provided better results compared to surgery alone. Taking into
consideration patients with brain and bone and metastasis, surgery
can be conducted.
Based on the IGCCCC criteria, the long-term survival
among brain metastatic patients is 30-40%, and chemotherapy and
radiotherapy are recommended (15).
However, we considered whether local resection combined with brain
radiotherapy would provide a better prognosis for brain metastatic
patients. Spine metastasis is common in bone metastatic patients.
Previous studies have shown that the management method for bone
metastatic disease can be chosen based on the pathological type of
the testicular cancer (16,17). Resection of bone metastases seem to
be conducted if there is a significant histology with teratoma and
vital carcinoma. In the case of seminomatous histology, however,
radiotherapy on bone is an option that has shown positive results
(15). Patients with liver and lung
metastatic disease may not benefit from orchiectomy. To our
knowledge, the combination of the resection of local and metastatic
lesions may be helpful in improving the treatment outcomes for
liver and lung metastatic testicular cancer patients.
We compared the surgical outcome based on molecular
subtypes and pathological types. Although AFP, HCG and LDH are the
cornerstones of clinical management for testicular cancer; based on
this study, only HCG and LDH may be considered in the decision of
treatment for patients with metastatic testicular cancer. Serum
levels of microRNA miR-371a-3p is found to be more sensitive and
specific than classical ones, expressing by 88.7% (18). Limited by the SEER database, we
cannot obtain the data of miR-371a-3p needed to assess the
prognosis with metastatic disease. To our knowledge, surgery plays
a large role in the management of non-seminoma, and its role in the
management of seminoma is much more limited. Although physicians
have demonstrated the significant role of surgery during stage II
seminoma testicular cancer, it is remains to be seen whether
surgery is an effective treatment for metastatic seminoma
testicular cancer. Most clinicians suggest chemotherapy after
orchiectomy during stage II. It is assumed that the same route of
treatment may be effective for patients diagnosed at a higher
stage. In our study, we divided our pathological type into two
groups, however, in non-seminoma group, there is mixed-cell tumors,
which has a worse outcome.
As discussed above, the effect of locoregional
surgery has been neglected in pMTC patients. Although orchiectomy
is the preferred first choice treatment for patients at a lower
stage, it is also good for selected patients at a higher stage.
Based on our study, orchiectomy has some positive effects on
metastatic testicular cancer. Although the data was acquired from a
large sample size, further investigation needs to be conducted on
this topic. Furthermore, we believe that an RCT consisting of
patients with solo distant metastasis, except lung and liver
metastasis, should be initiated to compare the difference between
surgery and non-surgery. And we hope more research will be held to
answer why locoregional treatment can benefit metastasis and why
chemotherapy or radiotherapy can affect, and what are the underling
mechanisms.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant nos. 81472377, 81502192
and 81672544).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
MA and DWY designed the study and prepared the
manuscript draft and substantively participated in revising the
manuscript. YZ contributed by analyzing the patients' data and
revised the manuscript. DWY supervised the study and critically
reviewed the manuscript, and gave final approval of the version to
be published. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
International Agency for Research on
Cancer (IARC): Estimated number of new cases in 2018, testis,
males, all ages. https://gco.iarc.fr/today/online-analysis-table?v=2018&mode=population&mode_population=continents&population=900&populations=900&key=asr&sex=1&cancer=28&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&include_nmsc=1&include_nmsc_other=1.
Accessed September 20, 2019.
|
|
2
|
Spiekermann M, Dieckmann KP, Balks T,
Bullerdiek J and Belge G: Is relative quantification dispensable
for the measurement of microRNAs as serum biomarkers in germ cell
tumors? Anticancer Res. 35:117–121. 2015.PubMed/NCBI
|
|
3
|
Hjelle LV, Gundersen PO, Oldenburg J,
Brydøy M, Tandstad T, Wilsgaard T, Fosså SD, Bremnes RM and Haugnes
HS: Long-term platinum retention after platinum-based chemotherapy
in testicular cancer survivors: A 20-year follow-up study.
Anticancer Res. 35:1619–1625. 2015.PubMed/NCBI
|
|
4
|
Burczynska BB, Kobrouly L, Butler SA,
Naase M and Iles RK: Novel insights into the expression of CGB1
& 2 genes by epithelial cancer cell lines secreting ectopic
free hCGβ. Anticancer Res. 34:2239–2248. 2014.PubMed/NCBI
|
|
5
|
Li X, Huang R, Ma L, Liu S and Zong X:
Locoregional surgical treatment improves the prognosis in primary
metastatic breast cancer patients with a single distant metastasis
except for brain metastasis. Breast. 45:104–112. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Janssen-Heijnen ML, Gondos A, Bray F,
Hakulinen T, Brewster DH, Brenner H and Coebergh JW: Clinical
relevance of conditional survival of cancer patients in europe:
Age-specific analyses of 13 cancers. J Clin Oncol. 28:2520–2528.
2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Verdecchia A, Francisci S, Brenner H,
Gatta G, Micheli A, Mangone L and Kunkler I: EUROCARE-4 Working
Group. Recent cancer survival in Europe: A 2000-02 period analysis
of EUROCARE-4 data. Lancet Oncol. 8:784–796. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
International Germ Cell Consensus
Classification. A prognostic factor-based staging system for
metastatic germ cell cancers. International Germ Cell Cancer
Collaborative Group. J Clin Oncol. 15:594–603. 1997.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Baird DC, Meyers GJ and Hu JS: Testicular
cancer: Diagnosis and treatment. Am Fam Physician. 97:261–268.
2018.PubMed/NCBI
|
|
10
|
Goedert JJ, Purdue MP, McNeel TS, McGlynn
KA and Engels EA: Risk of germ cell tumors among men with
HIV/acquired immunodeficiency syndrome. Cancer Epidemiol Biomarkers
Prev. 16:1266–1269. 2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Culine S, Kerbrat P, Kramar A, Théodore C,
Chevreau C, Geoffrois L, Bui NB, Pény J, Caty A, Delva R, et al:
Refining the optimal chemotherapy regimen for good-risk metastatic
nonseminomatous germ-cell tumors: A randomized trial of the
genito-urinary group of the french federation of cancer centers
(GETUG T93BP). Ann Oncol. 18:917–924. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
de Wit R, Roberts JT, Wilkinson PM, de
Mulder PH, Mead GM, Fosså SD, Cook P, de Prijck L, Stenning S and
Collette L: Equivalence of three or four cycles of bleomycin,
etoposide, and cisplatin chemotherapy and of a 3- or 5-day schedule
in good-prognosis germ cell cancer: A randomized study of the
European organization for research and treatment of cancer
genitourinary tract cancer cooperative group and the medical
research council. J Clin Oncol. 19:1629–1640. 2001.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fung C, Fossa SD, Milano MT, Sahasrabudhe
DM, Peterson DR and Travis LB: Cardiovascular disease mortality
after chemotherapy or surgery for testicular nonseminoma: A
population-based study. J Clin Oncol. 33:3105–3115. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fung C, Fossa SD, Williams A and Travis
LB: Long-term morbidity of testicular cancer treatment. Urol Clin
North Am. 42:393–408. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pfister D, Haidl F, Paffenholz P and
Heidenreich A: Metastatic surgery in testis cancer. Curr Opin Urol.
26:590–595. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Paffenholz P, Pfister D and Heidenreich A:
Postchemotherapy residual tumour resection in complex metastatic
sites of advanced testicular germ cell tumours. Urologe A.
55:632–640. 2016.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
17
|
Collis CH and Eckert H: Seminoma of the
testis with bone involvement: A report of three cases. Clin Radiol.
36:467–468. 1985.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dieckmann KP, Radtke A, Spiekermann M,
Balks T, Matthies C, Becker P, Ruf C, Oing C, Oechsle K, Bokemeyer
C, et al: Serum levels of microRNA miR-371a-3p: A sensitive and
specific new biomarker for germ cell tumours. Eur Urol. 71:213–220.
2017.PubMed/NCBI View Article : Google Scholar
|