Introduction
Bladder cancer is one of the 10 predominant
malignancies globally, with an estimated 573,278 new cases and
212,536 deaths recorded in 2020(1). It can be divided into muscle-invasive
bladder cancer (MIBC) and non-MIBC. MIBC accounts for ~25% of
bladder cancer cases at the time of initial diagnosis (2). Radical cystectomy with extended
pelvic lymphadenectomy remains the guideline-recommended treatment
for MIBC and may provide optimal cancer control (3). Vascular complications, such as
intraoperative injury to blood vessels, which results in massive
bleeding, are commonly reported complications of radical
cystectomy, which is a catastrophic event and may potentially have
an unfavorable effect on surgical mortality rates (4,5).
Iliac artery pseudoaneurysm and arterioureteral fistula are rare
complications following radical cystectomy (6,7). The
present study described another rare case of delayed right external
iliac artery disruption that occurred one month after laparoscopic
radical cystectomy, without any obvious evidence of iliac artery
pseudoaneurysm or arterioureteral fistula.
Case report
A 60-year-old male patient was admitted to the
emergency department of the Second Affiliated Hospital of Zhejiang
University (Hangzhou, China) in May 2019 with a 2-day history of
acute anaemia and fever. The patient had a medical history of
poorly controlled diabetes mellitus. Furthermore, the patient had
been subjected to a successful laparoscopic radical cystectomy with
bilateral pelvic lymph node dissection and urinary diversion and
was discharged one month prior. The patient presented with septic
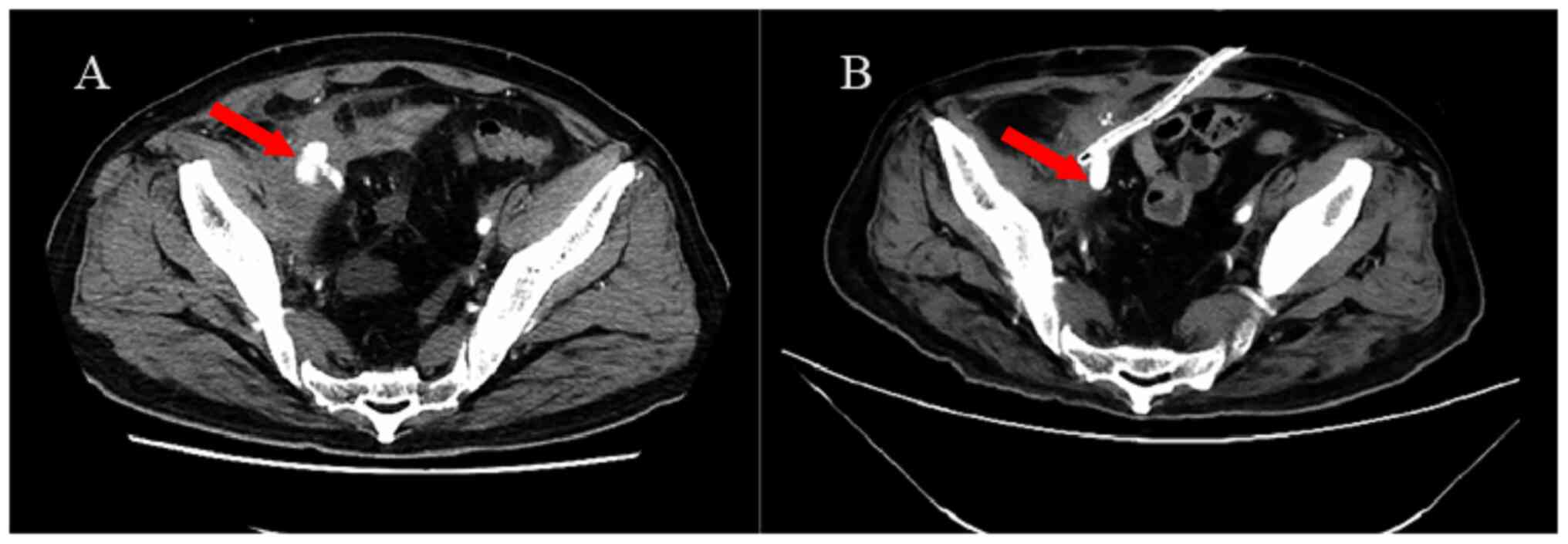
and haemorrhagic shock on admission. Enhanced abdominal CT showed
diffuse extravasation of the contrast medium from the right
external iliac artery, without any evidence of iliac artery
pseudoaneurysm or arterioureteral fistula (Fig. 1A). Based on these findings, a
diagnosis of right external iliac artery disruption was made.
Broad-spectrum antibiotics (imipenem) were started
empirically and then, an open, exploratory operation was undertaken
immediately, during which extensive adhesion formation and
inflammation around the ileal bladder and external iliac artery
were found. More importantly, a vessel split of the right external
iliac artery was found after removing the visible blood clots and
hematoma around it. Therefore, the diagnosis of disruption and
bleeding of the right external iliac artery was confirmed. A
vascular stent was inserted to cover the artery split by a vascular
surgeon. The patient was then transferred to the intensive care
unit for further resuscitation.
Klebsiella pneumoniae subsp.
Pneumoniae (KPSP) was isolated in blood culture which was
performed according to standard protocols three days later. The
standard drug susceptibility test determined that KPSP was more
sensitive to tigecycline and imipenem. Appropriate antibiotics
(tigecycline plus imipenem) were then administered based on the
above results of bacterial culture and drug sensitivities. The
vital signs and corresponding blood tests of the patient became
normal within three weeks. Furthermore, repeat enhanced CT
indicated no effusion of the contrast medium one month later
(Fig. 1B). The patient was
discharged one week after the repeat CT scan. Follow-up was carried
out every 3 months in the first year and every 6 months thereafter.
To date, the patient has been followed up for nearly 4 years with
no relapse.
Discussion
KP is a common pathogen that causes infections
involving the urinary tract, lungs, surgical sites, abdominal
cavity, intravascular devices, soft tissues and subsequent
bacteremia, particularly in alcoholics and diabetic patients
(8,9). For the patient of the present study,
diabetes mellitus and immunosuppression due to a major operation
were possible risk factors for KP infection in the blood.
Previous studies indicated that KP entry through an
overt or occult break in the skin resulted in initial bacteremia
(10). The subsequent spread of
bacteremia may lead to various complications, such as
endophthalmitis, meningitis and aneurysm (11-13).
As a gram-negative encapsulated rod, KP has a higher tendency to
expand and rupture the vessel wall where it colonizes (14). It was thus speculated that KPSP,
which belongs to the KP family, was seeded from the initial
bacteremia and then colonized into the right external iliac artery,
causing uncontrollable sepsis and arteritis. KPSP infection
eventually leads to such catastrophic vessel rupture. The
corresponding antibiotics for KPSP were subsequently changed based
on the drug sensitivity test to control the bacterial infection and
the vessel wall exhibited no evidence of split recurrence at the
time of writing the present report.
As interventions, endovascular treatments such as
vascular stent grafts are now suggested to be a better choice than
conventional surgical vessel repair because severe vessel injuries
destabilize the haemodynamic status of the patient and preclude
open repair of the lesion (8). In
the present case, vascular stent insertion but not vessel suturing
was carried out. Both antibiotics and endovascular operation had an
important role in the quick recovery of the patient.
In conclusion, timely detection, adequate antibiotic
treatment and emergency vascular stent insertion are important
strategies for physicians to manage this rare but life-threatening
condition. However, large-scale, prospective, controlled trials are
in high demand to comprehensively evaluate the effectiveness and
feasibility of these antibiotic and surgical treatments.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the Natural Science
Foundation of Zhejiang Province (grant no. LQ20H1 60032) and the
Natural Science Foundation of Fujian Province (grant no.
2018J05124).
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
LD contributed to the conception and design of the
study, obtained the raw data of the patient, such as laboratory
data and imaging examinations, and wrote the manuscript. LD and ZW
participated in the diagnosis and treatment of the patient. LD and
ZW checked and confirmed the authenticity of all the raw data. Both
authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the Second Affiliated Hospital of Zhejiang University
(Hangzhou, China).
Patient consent for publication
The patient provided written consent for the
publication of the case details and any associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global Cancer Statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Comperat E, Larre S, Roupret M, Neuzillet
Y, Pignot G, Quintens H, Houede N, Roy C, Durand X, Varinot J, et
al: Clinicopathological characteristics of urothelial bladder
cancer in patients less than 40 years old. Virchows Arch.
466:589–594. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Russell B, Liedberg F, Khan MS, Nair R,
Thurairaja R, Malde S, Kumar P, Bryan RT and Van Hemelrijck M: A
systematic review and Meta-analysis of delay in radical cystectomy
and the effect on survival in bladder cancer patients. Eur Urol
Oncol. 3:239–249. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Konety BR, Allareddy V and Herr H:
Complications after radical cystectomy: Analysis of
population-based data. Urology. 68:58–64. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lazzeri M, Benaim G, Turini D, Beneforti P
and Turini F: Iatrogenic external iliac artery disruption during
open pelvic lymph node dissection: Successful repair with
hypogastric artery transposition. Scand J Urol Nephrol. 31:205–207.
1997.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Laddha A, Pooleri GK and Thomas A:
External iliac artery pseudoaneurysm following radical cystectomy:
A report of two cases. Indian J Urol. 36:56–58. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jiang Z, Wang J, Cui J, Chen S, Qu S, Wang
W, Guo H, Shi B and Zhu Y: Arterioureteral fistula after radical
cystectomy and ureterocutaneostomy: Two case reports and a
systematic literature review. BMC Urol. 22(117)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wu CY, Hung YN, Liu YH and Ko PJ:
Endovascular treatment of iatrogenic iliac artery disruption in
lumbar disc surgery. Ann Vasc Surg. 23:255.e7–11. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Lin YT, Wang FD, Wu PF and Fung CP:
Klebsiella pneumoniae liver abscess in diabetic patients:
Association of glycemic control with the clinical characteristics.
BMC Infect Dis. 13(56)2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shon AS, Bajwa RP and Russo TA:
Hypervirulent (hypermucoviscous) Klebsiella pneumoniae: A
new and dangerous breed. Virulence. 4:107–118. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Namikawa H, Yamada K, Fujimoto H, Oinuma
KI, Tochino Y, Takemoto Y, Kaneko Y, Shuto T and Kakeya H: Two
unusual cases of successful treatment of hypermucoviscous
Klebsiella pneumoniae invasive syndrome. BMC Infect Dis.
16(680)2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wu KM, Li LH, Yan JJ, Tsao N, Liao TL,
Tsai HC, Fung CP, Chen HJ, Liu YM, Wang JT, et al: Genome
sequencing and comparative analysis of Klebsiella pneumoniae
NTUH-K2044, a strain causing liver abscess and meningitis. J
Bacteriol. 191:4492–4501. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Maruno T, Ooiwa Y, Takahashi K, Kodama Y,
Takakura S, Ichiyama S and Chiba T: A liver abscess deprived a
healthy adult of eyesight: Endogenous endophthalmitis associated
with a pyogenic liver abscess caused by serotype K1 Klebsiella
pneumonia. Intern Med. 52:919–922. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Molacek J, Treska V, Baxa J, Certik B and
Houdek K: Acute conditions caused by infectious aortitis. Aorta
(Stamford). 2:93–99. 2014.PubMed/NCBI View Article : Google Scholar
|