Introduction
Meningiomas are the most common primary tumours of
the central nervous system (CNS) constituting more than one-third
(1). Their probable origin is the
arachnoid cap cells of the meningeal layers. These cells have both
mesenchymal and epithelial features and are morphologically,
ultrastructurally, and functionally similar to meningioma cells,
giving rise to the great heterogeneity in histopathology,
recurrence rates, aggressivity, symptoms, and prognoses (2-4).
The incidence of meningiomas increases with age, so in an ageing
population they will become more prevalent. Meningiomas are rare in
children, and there is a more than a twofold higher incidence among
females (5,6).
Most meningiomas are benign and slow growing, but
they have an intrinsic tendency to recur despite benign histology
(3,4,7).
Prognostication of meningiomas has primarily been based on
histopathology, and according to criteria given by the World Health
Organization (WHO) these tumours are divided into three malignancy
grades and distinct subtypes. The 2021 WHO classification endorses
use of molecular biomarkers to support classification and grading
of these tumours (8,9).
Observation may be sufficient management; however,
when indicated, the main treatment mostly involves surgery
(10). The surgical gold standard
is complete resection, as subtotal resection is strongly associated
with high risk of recurrence (10). Radiation therapy may be indicated
in case of incomplete resection, difficult location for surgery
(i.e., skull-base meningiomas), recurrences, and high-grade tumours
(10). In any case, all these
treatment options have troublesome complications and side effects
(10-12).
Furthermore, as the incidence of meningioma increases with age,
these patients also have an increased risk of various adverse
events and prolonged hospitalization (13). Systemic therapy is still at the
experimental stage (10,11). All in all, these aspects underline
the crucial need for more objective biomarkers with which to
stratify meningioma patients according to risk of recurrence and
optimal treatment and follow-up regimes.
In this regard, the EGFR (epidermal growth factor
receptor) family is pertinent as these receptor proteins are known
to be crucial drivers of the growth and progression of many human
tumours (14-17).
This receptor family comprises four transmembrane tyrosine kinases:
ErbB1/EGFR, ErbB2/HER2, ErbB3/HER3, and ErbB4/HER4 (14,15,18).
These receptor proteins have an external ligand-binding domain, a
transmembrane domain, and an intracellular kinase domain. Upon
ligand binding, the receptor protein undergoes conformational
changes leading to homo- and heterodimerisation, and subsequently
active tyrosine kinase activity. Since ErbB2/HER2 lacks
ligand-binding sites, and ErbB3/HER3 lacks an internal kinase
domain, heterodimerisation is therefore important for their mutual
activation. Activated ErbB receptors trigger a cascade of
fundamental downstream signalling pathways, such as the Ras-ERK,
P13K-Akt, PLC-γ1, STAT1, and Src pathways (14,17,18),
which are involved in many essential cellular processes, including
survival, differentiation, proliferation, metabolism, adhesion,
motility, and angiogenesis (14,15,17,18).
Hence, aberrant ErbB expression is implicated in many human
malignancies and has shown diagnostic, prognostic, and therapeutic
significance (14,16,17,19),
whereas in human meningiomas the clinical significance is more
ambiguous (20-26).
We have recently published three papers on the
expression of each member of the EGFR family in human meningiomas,
and we found abundant co-expression of these receptor proteins
(20-22).
To our knowledge, there are no larger studies that have
investigated the clinicopathological significance of this
co-expression in these tumours. Here we give an overview of the
status of the EGFR receptor family in human meningiomas and discuss
clinical and histopathological aspects of this concurrent
overexpression.
Materials and methods
Patients and samples
The patient data, histopathological examination,
tissue microarray (TMA) construction, and immunohistochemical
analyses have been published earlier (20-22,27,28).
Briefly, all patients consecutively operated for meningiomas at St.
Olavs Hospital, Trondheim, Norway, in the time frame January
1991-January 2000 were evaluated for inclusion (only primary
tumours). Tumour tissue was fixed in formalin and embedded in
paraffin, and after microscopy the tumours were classified and
graded according to WHO 2016 guidelines (29). Exclusion criteria were patient age
<18 years and spinal localization. Anaplastic WHO grade 3
meningiomas were omitted due to few cases. Finally, 185 cases were
included. Follow-up time was a maximum of 18 years.
Immunohistochemistry
There was sufficient tumour tissue to construct TMAs
in 163 cases. Each tumour was represented by three
paraffin-embedded tissue cylinders. The remaining 22 cases not
suitable for TMA construction were processed as whole-tissue
sections. Standard immunohistochemistry was performed using a Dako
Autostainer Plus (Dako, Glostrup, DK). For ErbB1/EGFR and
ErbB2/HER2 staining, antibodies reactive against internal and
external domains and phosphorylated/activated receptor were used.
Antibodies targeting the internal domain were used for ErbB3/HER3
and ErbB4/HER4. A list of the primary antibodies used is shown in
Table I. After incubation with the
primary antibodies, the sections were incubated in a Dako EnVision
system. Each immunostaining was semiquantitatively assessed and
recorded as a staining index (SI) calculated as the product of the
intensity and the distribution of immunoreactive tumour cells.
Intensity was scored as 0 (no reaction), 1 (weak), 2 (moderate), or
3 (strong). Fraction of positive tumour cells was recorded as 0 (no
positivity), 1 (<10% positive cells), 2 (10-50% positive cells),
or 3 (>50% positive cells).
 | Table IList of antibodies. |
Table I
List of antibodies.
| Antibody | Supplier | Cat. no. | Clonality | Clone/epitope | Dilution |
|---|
| ErbB1/EGFR | | | | | |
|
Internal
domain (ErbB1/EGFR-int) | Novocastra, Leica
Biosystems | NCL-L-EGFR-384 | Moab | EGFR.25 | 1:100 |
|
External
domain (ErbB1/EGFR-ext) | Novocastra, Leica
Biosystems | NCL-EGFR | Moab | EGFR.113 | 1:10 |
|
Phosphorylated
(ErbB1/EGFR-ph) | EMD Millipore | 04-341 | Moab | Anti-phospho-EGFR
(Tyr1173) | 1:45 |
| ErbB2/HER2 | | | | | |
|
Internal
domain (ErbB2/HER2-int) | Novocastra, Leica
Biosystems | NCL-L-CB11 | Moab | CB11 | 1:40 |
|
External
domain (ErbB2/HER2-ext) | Thermo Fisher
Scientific | MA5-16348 | Moab | SP3 | 1:10 |
|
Phosphorylated
(ErbB2/HER2-ph) | Cell Signaling
Technology | 2243 | Moab | 6B12 | 1:10 |
| ErbB3/HER3 | | | | | |
|
Internal
domain (ErbB3/HER3-int) | Novocastra, Leica
Biosystems | NCL-c-erbB-3 | Moab | RTJ-1 IgM | 1:10 |
| ErbB4/HER4 | | | | | |
|
Internal
domain (ErbB4/HER4-int) | Thermo Fisher
Scientific | MA1-861 | Moab | HFR1 IgG2b | 1:50 |
Statistical analyses
The survival analyses have been described earlier
(20-22,27).
Briefly, associations between SIs and tumour grades were assessed
by Mann-Whitney U-test, and Kruskal-Wallis and Dunn tests were used
to test for associations between SIs and variables with more than
two groups (tumour subtypes and localization). Cox regression
analyses were used in both uni- and multivariate survival analyses
based on continuous SIs. Simpson resection grade (1/2 vs. 3/4), WHO
performance status (0 and 1 vs. 2, 3, 4, and 5), histological
malignancy grade (grade 1 vs. grade 2), and age (continuous values)
were used as covariates in the multivariate analyses. Statistical
significance was defined as P<0.05. SPSS version 24.0 (IBM
Corp.) was used in the statistical analyses.
Results
A total number of 185 cases were enrolled: 129 CNS
WHO grade 1 meningiomas (70%) and 56 atypical CNS WHO grade 2
meningiomas (30%), with a female:male ratio of 2.9. Most patients
were radically operated and had a good performance status.
Convexity meningiomas (falx and convexities) comprised 109 cases
(59%), and skull base meningiomas (skull base, posterior fossa,
tentoria and intraventricular) 76 cases (41%). Most tumours showed
positive immunoreactivity for epithelial membrane antigen (EMA)
(98.3%). Patient data are shown in Table II.
 | Table IIPatient data. |
Table II
Patient data.
| Parameter | Grade 1 | Grade 2 | Total |
|---|
| Number of
cases | 129 (69.7%) | 56 (30.2%) | 185 |
| Median age at
operation, years (range) | 58 (27-84) | 62 (25-86) | 59 (25-86) |
| Sex,
male/female | 29/100 | 18/38 | 47/138 |
| Simpson grade,
I/II/III/IV | 33/53/18/25 | 11/27/11/7 | 44/80/29/32 |
| WHO Performance
Status, 0/1/2/3/4 | 18/89/20/2/0 | 6/41/7/1/1 | 25/130/27/3/1 |
| Localization,
convexity (including falcine)/skull base (including posterior
fossa, tentorial and intraventricular) | 64/65 | 45/11 | 109/76 |
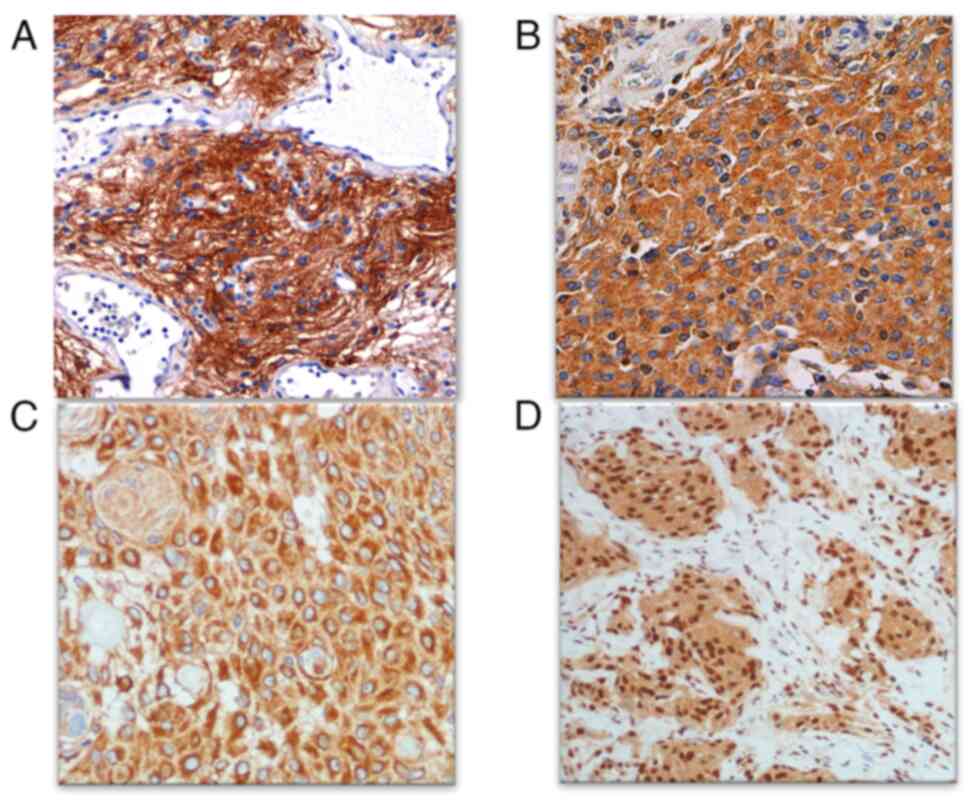
All tumours were immunoreactive for the ErbB
receptors, most tumours showed high expression levels. Both
cytoplasmic and membranous immunoreactivity were observed. For
ErbB4/HER4, nuclear immunoreactivity was found as well. Normal
meninges adjacent to the tumour tissue did not display detectable
immunoreactivity. A survey of the immunohistochemical analyses is
presented in Table III, and
examples of typical immunostaining images of internal domains are
shown in Fig. 1.
 | Table IIIImmunohistochemical results. |
Table III
Immunohistochemical results.
| ErbB receptor | Benign (n=129),
number immunoreactive (%) | Atypical (n=56),
number immunoreactive (%) |
|---|
| ErbB1/EGFR-internal
domain | 129 (100%) | 56 (100%) |
| ErbB1/EGFR-external
domain | 128 (99.2%) | 56 (100%) |
|
ErbB1/EGFR-phosphorylated | 128 (99.2%) | 56 (100%) |
| ErbB2/HER2-internal
domain | 129 (100%) | 56 (100%) |
| ErbB2/HER2-external
domain | 67 (51.9%) | 23 (41.1%) |
|
ErbB2/HER2-phosphorylated | 15 (11.6%) | 5 (9.1%) |
| ErbB3/HER3-internal
domain | 126 (97.7%) | 56 (100%) |
| ErbB4/HER4-internal
domain | 129 (100%) | 56 (100%) |
Table IV shows the
clinical data. The expression pattern was generally poorly
associated with tumour localization, subtypes, tumour grade, and
prognosis. Among significant results, ErbB1/EGFR showed higher SIs
in transitional (P=0.028) and meningothelial (P=0.044) subtypes
compared with fibrous ones. The SIs of ErbB1/EGFR-ph were lower in
skull-base compared with convexity meningiomas (P=0.001) and were
higher in grade 2 tumours than in grade 1 (P=0.018). Further,
ErbB4/HER4 SIs were higher in convexity meningiomas compared with
those in the skull base (P=0.040).
 | Table IVSurvey of ErbB receptor expression
and clinical associations. |
Table IV
Survey of ErbB receptor expression
and clinical associations.
| ErbB receptor | Localization
(convexity vs. skull base) | Association with
subtypes | Association with
histological malignancy grade | Association with to
TTR | Association with
OS |
|---|
| ErbB1/EGFR-int | NS | NS | NS | NS | NS |
| ErbB1/EGFR-ext | NS | Sc | NS | Se | NS |
| ErbB1/EGFR-ph | Sa | NS | Sd | NS | NS |
| ErbB2/HER2-int | NS | NS | NS | NS | NS |
| ErbB2/HER2-ext | NS | NS | NS | NS | NS |
| ErbB2/HER2-ph | NS | NS | NS | Sf | Sg |
| ErbB3/HER3-int | NS | NS | NS | NS | NS |
| ErbB4/HER4-int | Sb | NS | NS | NS | Sh |
Concerning prognosis, ErbB1/EGFR-ext and
ErbB4/HER4-int were correlated with TTR (HR=1.099, 95% CI
0.987-1.222, P=0.084) and OS (HR=1.223, 95% CI 1.023-1.461,
P=0.027) in univariate analyses, respectively. ErbB2/HER2-ph was
significantly associated with TTR and OS in both univariate (TTR:
HR=1.512, 95% CI 1.132-2.019, P=0.005; OS: HR=1.397, 95% CI
1.027-1.900, P=0.033) and multivariate (TTR: HR=1.512, 95% CR
1.132-2.019, P=0.005; OS: HR=1.679, 95% CI 1.213-2.323, P=0.002)
analyses. Among clinical factors, high Simpson grade was associated
with poorer prognosis in multivariate analysis (HR=0.36, 95% CI
0.21-0.60, P<0.001).
Discussion
By means of immunohistochemistry we have shown
concurrent overexpression of all members of the EGFR family in our
series of meningiomas, whereas the clinical significance was
limited where only ErbB2/HER2-ph was significantly associated with
prognosis in multivariate analyses.
Malignant transformation of normal cells involves
accumulation of several genetic changes, whereas subsequent steps
in tumour progression, such as clonal growth, invasion, and
angiogenesis, are in high degree mediated by growth factors and
their receptors (19). Common
genetic changes in human meningiomas are loss of chromosome 22q
(60-70% in sporadic meningiomas) and mutations in NF2,
TRAF7, SMO, AKT1, KLF4, SMARCB1, BAP1, TERT promoter,
homozygous deletions of CDKN2A/B, and H3K27me loss (5,30,31).
These genetic events are linked to and affect intracellular
signalling pathways, including those mediated by the EGFR family,
and play important roles in tumour growth and progression (14,17,19,30).
Thus, concurrent overexpression of the ErbB receptors together with
the reported molecular genetic events, constitutes a strong
synchronous driving force on intracellular pathways fundamental to
the tumourigenesis of human meningiomas. This is in accordance with
the study of Hilton et al, who reported the activation of
many growth factor receptors and their signalling pathways
(32). This overexpression of the
ErbB receptors was poorly associated with proliferative activity
(i.e., mitotic activity), atypical histological features, and
tumour grade (apart from ErbB1/EGFR-ph), suggesting that the
receptor proteins are more involved in aspects of tumour biology,
such as cell survival (including apoptosis), angiogenesis, cell
motility and metabolism (14,19,33),
than in tumour progression.
Various growth factors bind to and activate ErbB
receptors (14,17,19),
such as epidermal growth factor and transforming growth
factor-alpha, which also have been detected in meningioma cells
(22,34). Their release/shedding is proposed
to be a rate-limiting step determining levels of ligands in the
tissue (35,36). These ligands bind to their specific
ErbB receptor with various affinities and with formation of homo-
and heterodimers (14,15). The various combinations of ligands
and dimers also stand out as important regulatory mechanisms
(14,35). These findings support the existence
of local autocrine and paracrine growth loops in the meningioma
tissue, but non-neoplastic cells, such as fibroblasts, endothelial
cells, and macrophages, are also involved. This cross talk is
essential for tumour biology with regard to infiltration,
migration, angiogenesis, local inflammatory responses, and
establishment and maintenance of the tumour microenvironment
(14,19,36,37).
These aspects may be reflected by the infiltrative growth of
meningioma in dura, bone, and brain tissue (the latter typical for
aggressive meningiomas), vascularization, and inflammatory response
(4,14,15,38).
In this regard, ErbB receptors have been shown to induce an
immunosuppressive tumour microenvironment by regulating the immune
system, and in this manner enable tumour escape from antitumour
immune responses (38). This may
be important in the observed acquired resistance to multitargeted
therapies as well as to immune checkpoint inhibitors (38).
Activation of ErbB receptors trigger various
intracellular signalling pathways, such as the phosphatidylinositol
3-kinase/Akt (PKB) pathway, the Ras/Raf/MEK/ERK1/2 pathway, and the
phospholipase C (PLCγ) pathway (14,15,17,18).
This complex ErbB network is regarded as a robust cellular
signalling system in tumours, as many receptors activate common
pathways (14,38,39).
This may also partly explain why ErbB1/EGFR alone has not worked as
a valuable therapeutic target (14,33,38)
and thus constitutes a rationale for application of multi-tyrosine
kinase inhibitors (10,40-42).
Both membranous and cytoplasmic immunoreactivity
were observed in agreement with their transmembrane localization
and their fate after activation, including endocytosis,
ubiquitylation, and degradation as well as recycling (14). The clinical relevance of either the
membranous or the cytoplasmic immunoreactivity was not
investigated, as the mesenchymal features of meningioma tumour
tissue make such a distinction difficult. However, this issue is of
relevance in other tumour types, such as breast and lung cancer
where only membranous ErbB2/HER2 is accepted (43,44).
Nuclear ErbB receptor immunoreactivity has been reported in various
human malignancies as well, but to our knowledge not in human
meningiomas (14,17,45,46).
We found; however nuclear immunoreactivity for ErbB4/HER4(20) that may be involved in
transcriptional regulation, signal transmission, cell
proliferation, and DNA repair and replication. They have also been
linked to genomic instability, chemo- and radio-resistance, and
various clinicopathological states (14,17,45,46).
Overexpression of ErbB1/EGFR has been commonly found
in human meningiomas (22-25,47,48)
and may be due to ligand overproduction, increased transcription or
translation, or endocytic pathway regulation as EGFR gene
amplification has not been found in these tumours (33). Actually, EGFR mutations have
recently been detected, but the clinical significance of this is
uncertain (49). Activation of the
ErbB receptors leads to conformational changes and
autophosphorylation. Both represent important regulatory steps
(14,15). We therefore wanted to study the
expression level of ErbB1/EGFR-ph. Most of our meningiomas were
immunoreactive indicating a constitutively active receptor. The
positive correlation with malignancy grade may be related to tumour
progression; however, no prognostic value was found. The higher
immunoreactivity in convexity compared with skull-base meningiomas
but not any relation to subtypes, may be due to the embryonic
origin of the meninges (50).
ErbB1/EGFR-ext displayed weak immunostaining. We have no obvious
explanation for this, but we have observed this in glioblastomas as
well (51). One may speculate
whether this is related to proteolytic shedding or conformational
changes during ligand binding and resultant epitope availability
(15,52). ErbB1/EGFR-ext was also
significantly associated with decreased TTR, but only in univariate
analyses. Accordingly, our findings are in agreement with the
literature that ErbB1/EGFR has limited prognostic value in human
meningiomas.
ErbB2/HER2 was also widely expressed in accordance
with most others (21,53-57).
This overexpression may be due to factors previously mentioned, but
gene amplification has been found in a few tumours (55). We have; however, not found this
genetic event in our studies (21,58).
The expression levels between females and males have not been
checked, but it has been reported not to differ (56). ErbB2/HER2 lacks extracellular
ligand binding sites, so this receptor protein becomes activated
because it is a favoured dimerization partner for the other ErbB
receptor proteins (14,59). In contrast to the abundant
expression of ErbB1/HER-ph, few cases were ErbB2/HER2-ph
immunoreactive, and the labelling was weak as well. Nevertheless,
it achieved statistical significance regarding prognosis in
multivariate analyses. This is also in line with findings in breast
and lung cancer (60,61). Thus, ErbB2/HER2-ph may be
considered as a prognostic biomarker in human meningiomas, a
drawback is the weak labelling, so both the immunostaining and
prognostic power must be further validated.
ErbB3/HER3 and ErbB4/HER4 were highly expressed in
all of our meningiomas (20), but
the clinicopathologic value is scarcely described (20,23,25,62).
Since ErbB3/HER3 lacks intrinsic kinase activity, its activation
depends on ligand binding and/or heterodimerisation with other ErbB
members, and especially ErbB2/HER2 is a prioritized partner
(14,59,63).
Overexpressed and activated ErbB3/HER3 has been linked to tumour
progression and poor prognosis in many human cancers (17,63),
whereas we do not find any such association (20). ErbB4/HER4 has been shown to have
various clinical roles in human cancers (17,64).
We find it to have prognostic value but only in univariate
analyses, so this needs to be further investigated. ErbB4/HER4 was
the only EGFR family member with nuclear expression. Studies have
shown clinical relevance of this immunoreactivity (17,64).
As most of our tumours displayed nuclear expression, no
clinicopathological significance could be established. As for
ErbB1/EGFR-ph, ErbB4/HER4 displayed higher labelling in convexity
meningiomas compared with basal ones, which may be related to the
meninges' embryology and NF2 gene status (8,30,50).
Primary treatment for most meningiomas is surgery,
alternatively radiotherapy (10).
In case of inoperable, subtotally resected or recurrent aggressive
meningiomas, chemotherapy or targeted therapy may be ventilated,
but their roles in the clinical management of meningiomas are still
not well established (10,41,42).
Nevertheless, future therapeutic approaches may be based on
identification of potential unique molecular targets. As most
growth factor receptors and tyrosine kinases are expressed in human
meningiomas with subsequent activation of several intracellular
signalling pathways (26,31), molecular targeted therapies
including tyrosine kinase inhibitors have emerged (26,31,38,42).
In this regard, pilot studies with ErbB tyrosine kinase inhibitors
have largely been ineffective, mostly due to acquired resistance
(38). This may be related to
upregulation of downstream signalling pathways, activation of
by-pass pathways, upregulated autophagy, and secondary mutations,
as well as the induction of an immunosuppressive tumour
microenvironment (33,38). That said, multitargeted tyrosine
kinase inhibitors, anti-angiogenetic therapy (VEGF inhibitors), and
mTOR inhibitors have revealed promising results (41,42).
In addition, other antineoplastic drugs are under investigations as
potential candidates for systemic therapy and immunotherapy of
especially more aggressive meningiomas (42,65,66).
The strength of our studies is the rather large
number of patients operated at a single neurosurgical centre with
population-based referral and long follow-up. Limitations are the
retrospective aspects, the inherent challenges of
immunohistochemistry, and the subjective assessment of the
immunostaining.
In conclusion, we have shown abundant co-expression
of all ErbB receptors in human meningiomas, supporting their
fundamental role in their tumourigenesis, and this overexpression
may be of value in any targeted clinical strategies for these
tumours.
Acknowledgements
Not applicable.
Funding
Funding: This project was funded by the Norwegian University of
Science and Technology, Trondheim, Norway (project no. 81850106)
and the Department of Pathology, St. Olavs Hospital, Trondheim,
Norway.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SHT, DS, and MBA were involved in conceptualization
of the study. SHT and MBA confirm the authenticity of all the raw
data. MBA performed analyses. MBA, DS and SHT wrote the manuscript.
SHT performed project administration and supervision. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of The Declaration of Helsinki and was approved by the
Regional Committee for Medical Research Ethics Central Norway,
Faculty of Medicine and Health Sciences, Norwegian University of
Science and Technology, Trondheim, Norway with approved waiver of
consent (project number 4.2006.947).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ostrom QT, Price M, Ryan K, Edelson J,
Neff C, Cioffi G, Waite KA, Kruchko C and Barnholtz-Sloan JS:
CBTRUS statistical report: Pediatric brain tumor foundation
childhood and adolescent primary brain and other central nervous
system tumors diagnosed in the United States in 2014-2018. Neuro
Oncol. 24(Suppl 3):iii1–iii38. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Perry A, Gutmann DH and Reifenberger G:
Molecular pathogenesis of meningiomas. J Neurooncol. 70:183–202.
2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Harter PN, Braun Y and Plate KH:
Classification of meningiomas-advances and controversies. Chin Clin
Oncol. 6(Suppl 1)(S2)2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mawrin C and Perry A: Pathological
classification and molecular genetics of meningiomas. J Neurooncol.
99:379–391. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Suppiah S, Nassiri F, Bi WL, Dunn IF,
Hanemann CO, Horbinski CM, Hashizume R, James CD, Mawrin C,
Noushmehr H, et al: Molecular and translational advances in
meningiomas. Neuro Oncol. 21(Suppl 1):i4–i17. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wiemels J, Wrensch M and Claus EB:
Epidemiology and etiology of meningioma. J Neurooncol. 99:307–314.
2010.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Buerki RA, Horbinski CM, Kruser T,
Horowitz PM, James CD and Lukas RV: An overview of meningiomas.
Future Oncol. 14:2161–2177. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gritsch S, Batchelor TT and Gonzalez
Castro LN: Diagnostic, therapeutic, and prognostic implications of
the 2021 World Health Organization classification of tumors of the
central nervous system. Cancer. 128:47–58. 2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Louis DN, Perry A, Wesseling P, Brat DJ,
Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM,
Reifenberger G, et al: The 2021 WHO Classification of tumors of the
central nervous system: A summary. Neuro Oncol. 23:1231–1251.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Goldbrunner R, Stavrinou P, Jenkinson MD,
Sahm F, Mawrin C, Weber DC, Preusser M, Minniti G, Lund-Johansen M,
Lefranc F, et al: EANO guideline on the diagnosis and management of
meningiomas. Neuro Oncol. 23:1821–1834. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Brastianos PK, Galanis E, Butowski N, Chan
JW, Dunn IF, Goldbrunner R, Herold-Mende C, Ippen FM, Mawrin C,
McDermott MW, et al: Advances in multidisciplinary therapy for
meningiomas. Neuro Oncol. 21(Suppl 1):i18–i31. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lacy J, Saadati H and Yu JB: Complications
of brain tumors and their treatment. Hematol Oncol Clin North Am.
26:779–796. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nia AM, Branch DW, Maynard K, Frank T,
Yowtak-Guillet J, Patterson JT and Lall RR: How the elderly fare
after brain tumor surgery compared to younger patients within a
30-day follow-up: A National surgical Quality Improvement Program
analysis of 30,183 cases. J Clin Neurosci. 78:114–120.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Roskoski R Jr: The ErbB/HER family of
protein-tyrosine kinases and cancer. Pharmacol Res. 79:34–74.
2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lemmon MA, Schlessinger J and Ferguson KM:
The EGFR family: Not so prototypical receptor tyrosine kinases.
Cold Spring Harb Perspect Biol. 6(a020768)2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Uberall I, Kolar Z, Trojanec R, Berkovcova
J and Hajduch M: The status and role of ErbB receptors in human
cancer. Exp Mol Pathol. 84:79–89. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wang Z: ErbB receptors and cancer. Methods
Mol Biol. 1652:3–35. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yarden Y: The EGFR family and its ligands
in human cancer. Signalling mechanisms and therapeutic
opportunities. Eur J Cancer. 37 (Suppl 4):S3–S8. 2001.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Witsch E, Sela M and Yarden Y: Roles for
growth factors in cancer progression. Physiology (Bethesda).
25:85–101. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Arnli MB, Meta R, Lydersen S and Torp SH:
HER3 and HER4 are highly expressed in human meningiomas. Pathol Res
Pract. 215(152551)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Arnli MB, Winther TL, Lydersen S and Torp
SH: Prognostic value of ErbB2/HER2 in human meningiomas. PLoS One.
13(e0205846)2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Arnli MB, Backer-Grondahl T, Ytterhus B,
Granli US, Lydersen S, Gulati S and Torp SH: Expression and
clinical value of EGFR in human meningiomas. PeerJ.
5(e3140)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Andersson U, Guo D, Malmer B, Bergenheim
AT, Brännström T, Hedman H and Henriksson R: Epidermal growth
factor receptor family (EGFR, ErbB2-4) in gliomas and meningiomas.
Acta Neuropathol. 108:135–142. 2004.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wickremesekera A, Hovens CM and Kaye AH:
Expression of ErbB-1 and ErbB-2 in meningioma. J Clin Neurosci.
17:1155–1158. 2010.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Laurendeau I, Ferrer M, Garrido D, D'Haene
N, Ciavarelli P, Basso A, Vidaud M, Bieche I, Salmon I and Szijan
I: Gene expression profiling of ErbB receptors and ligands in human
meningiomas. Cancer Invest. 27:691–698. 2009.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Roesler R, Souza BK and Isolan GR:
Receptor tyrosine kinases as candidate prognostic biomarkers and
therapeutic targets in meningioma. Int J Mol Sci.
22(11352)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Backer-Grondahl T, Moen BH, Sundstrom SH
and Torp SH: Histopathology and prognosis in human meningiomas.
APMIS. 122:856–866. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Backer-Grondahl T, Moen BH and Torp SH:
The histopathological spectrum of human meningiomas. Int J Clin Exp
Pathol. 5:231–242. 2012.PubMed/NCBI
|
|
29
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 World Health Organization
classification of tumors of the central nervous system: A summary.
Acta Neuropathol. 131:803–820. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Birzu C, Peyre M and Sahm F: Molecular
alterations in meningioma: Prognostic and therapeutic perspectives.
Curr Opin Oncol. 32:613–622. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Preusser M, Brastianos PK and Mawrin C:
Advances in meningioma genetics: Novel therapeutic opportunities.
Nat Rev Neurol. 14:106–115. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Hilton DA, Shivane A, Kirk L, Bassiri K,
Enki DG and Hanemann CO: Activation of multiple growth factor
signalling pathways is frequent in meningiomas. Neuropathology.
36:250–261. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Sigismund S, Avanzato D and Lanzetti L:
Emerging functions of the EGFR in cancer. Mol Oncol. 12:3–20.
2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Carroll RS, Black PM, Zhang J, Kirsch M,
Percec I, Lau N and Guha A: Expression and activation of epidermal
growth factor receptors in meningiomas. J Neurosurg. 87:315–323.
1997.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Singh B, Carpenter G and Coffey RJ: EGF
receptor ligands: Recent advances. F1000Res. 5(F1000 Faculty
Rev-2270)2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Sanderson MP, Dempsey PJ and Dunbar AJ:
Control of ErbB signaling through metalloprotease mediated
ectodomain shedding of EGF-like factors. Growth Factors.
24:121–136. 2006.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Wilson KJ, Mill C, Lambert S, Buchman J,
Wilson TR, Hernandez-Gordillo V, Gallo RM, Ades LM, Settleman J and
Riese DJ II: EGFR ligands exhibit functional differences in models
of paracrine and autocrine signaling. Growth Factors. 30:107–116.
2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Kumagai S, Koyama S and Nishikawa H:
Antitumour immunity regulated by aberrant ERBB family signalling.
Nat Rev Cancer. 21:181–197. 2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Citri A and Yarden Y: EGF-ERBB signalling:
Towards the systems level. Nat Rev Mol Cell Biol. 7:505–516.
2006.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Zhao L, Zhao W, Hou Y, Wen C, Wang J, Wu P
and Guo Z: An overview of managements in meningiomas. Front Oncol.
10(1523)2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Patel B, Desai R, Pugazenthi S, Butt OH,
Huang J and Kim AH: Identification and management of aggressive
meningiomas. Front Oncol. 12(851758)2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Kim L: A narrative review of targeted
therapies in meningioma. Chin Clin Oncol. 9(76)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Moelans CB, de Weger RA, Van der Wall E
and van Diest PJ: Current technologies for HER2 testing in breast
cancer. Crit Rev Oncol Hematol. 80:380–392. 2011.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Petersen I, Dietel M, Geilenkeuser WJ,
Mireskandari M, Weichert W, Steiger K, Scheel AH, Büttner R,
Schirmacher P, Warth A, et al: EGFR immunohistochemistry as
biomarker for antibody-based therapy of squamous NSCLC-Experience
from the first ring trial of the German Quality Assurance
Initiative for Pathology (QuIP®). Pathol Res Pract. 213:1530–1535.
2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Carpenter G and Liao HJ: Trafficking of
receptor tyrosine kinases to the nucleus. Exp Cell Res.
315:1556–1566. 2009.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Wang YN and Hung MC: Nuclear functions and
subcellular trafficking mechanisms of the epidermal growth factor
receptor family. Cell Biosci. 2(13)2012.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Caltabiano R, Barbagallo GM, Castaing M,
Cassenti A, Senetta R, Cassoni P, Albanese V and Lanzafame S:
Prognostic value of EGFR expression in de novo and progressed
atypical and anaplastic meningiomas: An immunohistochemical and
fluorescence in situ hybridization pilot study. J Neurosurg Sci.
57:139–151. 2013.PubMed/NCBI
|
|
48
|
Torp SH, Helseth E, Dalen A and Unsgaard
G: Expression of epidermal growth factor receptor in human
meningiomas and meningeal tissue. APMIS. 100:797–802.
1992.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Pepe F, Pisapia P, Del Basso de Caro ML,
Conticelli F, Malapelle U, Troncone G and Martinez JC: Next
generation sequencing identifies novel potential actionable
mutations for grade I meningioma treatment. Histol Histopathol.
35:741–749. 2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Catala M: Embryonic and fetal development
of structures associated with the cerebro-spinal fluid in man and
other species. Part I: The ventricular system, meninges and choroid
plexuses. Arch Anat Cytol Pathol. 46:153–169. 1998.PubMed/NCBI
|
|
51
|
Torp SH, Gulati S, Johannessen E and Dalen
A: Coexpression of c-erbB 1-4 receptor proteins in human
glioblastomas. An immunohistochemical study. J Exp Clin Cancer Res.
26:353–359. 2007.PubMed/NCBI
|
|
52
|
Perez-Torres M, Valle BL, Maihle NJ,
Negron-Vega L, Nieves-Alicea R and Cora EM: Shedding of epidermal
growth factor receptor is a regulated process that occurs with
overexpression in malignant cells. Exp Cell Res. 314:2907–2918.
2008.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Torp SH, Helseth E, Unsgaard G and Dalen
A: C-erbB-2/HER-2 protein in human intracranial tumours. Eur J
Cancer. 29A:1604–1606. 1993.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Potti A, Forseen SE, Koka VK, Pervez H,
Koch M, Fraiman G, Mehdi SA and Levitt R: Determination of
HER-2/neu overexpression and clinical predictors of survival in a
cohort of 347 patients with primary malignant brain tumors. Cancer
Invest. 22:537–544. 2004.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Loussouarn D, Brunon J, Avet-Loiseau H,
Campone M and Mosnier JF: Prognostic value of HER2 expression in
meningiomas: An immunohistochemical and fluorescence in situ
hybridization study. Hum Pathol. 37:415–421. 2006.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Telugu RB, Chowhan AK, Rukmangadha N,
Patnayak R, Phaneendra BV, Prasad BC and Reddy MK: Human epidermal
growth factor receptor 2/neu protein expression in meningiomas: An
immunohistochemical study. J Neurosci Rural Pract. 7:526–531.
2016.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Schlegel J, Ullrich B, Stumm G, Gass P,
Harwerth IM, Hynes NE and Kiessling M: Expression of the
c-erbB-2-encoded oncoprotein and progesterone receptor in human
meningiomas. Acta Neuropathol. 86:473–479. 1993.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Helseth E, Unsgaard G, Dalen A, Fure H,
Skandsen T, Odegaard A and Vik R: Amplification of the epidermal
growth factor receptor gene in biopsy specimens from human
intracranial tumours. Br J Neurosurg. 2:217–225. 1988.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Yarden Y and Pines G: The ERBB network: At
last, cancer therapy meets systems biology. Nat Rev Cancer.
12:553–563. 2012.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Kurebayashi J, Kanomata N, Yamashita T,
Shimo T, Mizutoh A, Moriya T and Sonoo H: Prognostic value of
phosphorylated HER2 in HER2-positive breast cancer patients treated
with adjuvant trastuzumab. Breast Cancer. 22:292–299.
2015.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Suzuki M, Shiraishi K, Yoshida A, Shimada
Y, Suzuki K, Asamura H, Furuta K, Kohno T and Tsuta K: HER2 gene
mutations in non-small cell lung carcinomas: Concurrence with Her2
gene amplification and Her2 protein expression and phosphorylation.
Lung Cancer. 87:14–22. 2015.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Cimino PJ, Yoda RA, Wirsching HG, Warrick
JI, Dorschner MO and Ferreira M: Genomic profiling of anaplastic
meningioma identifies recurrent genetic alterations with relevance
to lower-grade meningioma. Neuropathol Appl Neurobiol. 45:179–182.
2019.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Haikala HM and Jänne PA: Thirty years of
HER3: From basic biology to therapeutic interventions. Clin Cancer
Res. 27:3528–3539. 2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
El-Gamal MI, Mewafi NH, Abdelmotteleb NE,
Emara MA, Tarazi H, Sbenati RM, Madkour MM, Zaraei SO, Shahin AI
and Anbar HS: A Review of HER4 (ErbB4) kinase, its impact on
cancer, and its inhibitors. Molecules. 26(7376)2021.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Jungwirth G, Yu T, Liu F, Cao J, Alaa
Eddine M, Moustafa M, Abdollahi A, Warta R, Unterberg A and
Herold-Mende C: Pharmacological landscape of FDA-Approved
anticancer drugs reveals sensitivities to ixabepilone, romidepsin,
omacetaxine, and carfilzomib in aggressive meningiomas. Clin Cancer
Res. 29:233–243. 2023.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Falzone L, Bordonaro R and Libra M:
SnapShot: Cancer chemotherapy. Cell. 186:1816–1816.el. 2023.
|