Introduction
Unicameral bone cyst (UBC) or simple bone cyst (SBC)
is a benign cystic lesion commonly found in the humerus and femur
that is mainly encountered during childhood. UBCs typically remain
asymptomatic and represent ~3% of all primary bone lesions
(1). UBC is a serous or
serosanguineous fluid-filled cavity, which is typically inactive
and remains asymptomatic until a pathological fracture occurs. The
clinical presentation, location and radiographic features are
rather characteristic and the diagnosis may be readily established.
In 86% of the cases, UCB occurs within the first two decades of
life and the proximal humerus is the most common site, whereas it
is rarely observed in the hand. Very few cases of UBC have been
described in the hand to date, including the metacarpals,
phalanges, hamate and lunate bones. Men are twice as likely to be
affected compared with women (2).
The location of UBC may be classified as active
(immediately juxtaposed to the growth plate, not to be confused
with Enneking stage 2 tumors) or inactive (growth plate not
adjacent to the cyst) (3). On
clinical examination, the lesion appears as a well-defined
fluid-filled cyst in the metaphysis and diaphysis of the affected
bone that may cause pain and swelling. Radiological examination is
crucial for establishing the diagnosis, based on the following
characteristics: Well-demarcated osteolytic lesion without marked
marginal sclerosis, central location, thinning of the cortex and
intralesional fracture fragment (‘fallen leaf’ or ‘fallen fragment’
sign) (3). The treatment for UBC of
the hand commonly involves curettage, bone grafting, partial
resection with or without grafting, multiple drilling, fracture
immobilization and observation alone, and steroid injection
(4).
Case report
A 9-year-old right-handed female patient presented
in February 2017 to the Department of Orthopaedics and Traumatology
of Saiful Anwar Hospital (Malang, Indonesia) with a chief complaint
of a large, fast-growing lump over the first metacarpal of the left
hand. The swelling was first observed 6 months earlier. The pain
was described as dull and constant, with no diurnal variation.
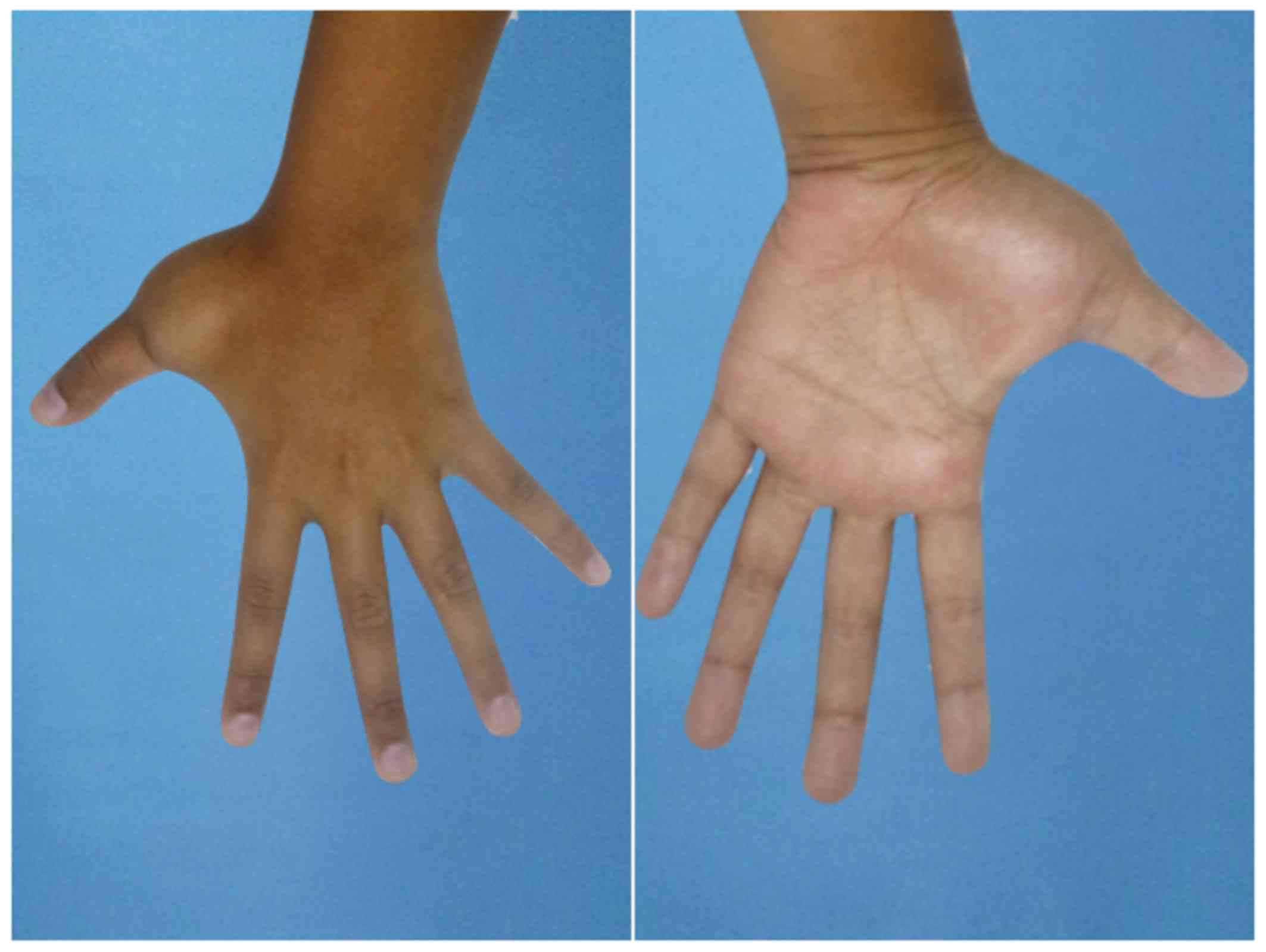
There was no history of trauma of infection. Physical examination
revealed a firm mass, ~3×4 cm in size, which was tender on
palpation, but with no local rise in temperature (Fig. 1). Flexion of the first
metacarpophalangeal joint was limited. There was minimal soft
tissue extension and no sensory-motor deficit; the distal
circulation was also normal. On imaging, plain radiographs of the
left hand revealed cystic enlargement of the first metacarpal that
included the base (Fig. 2).
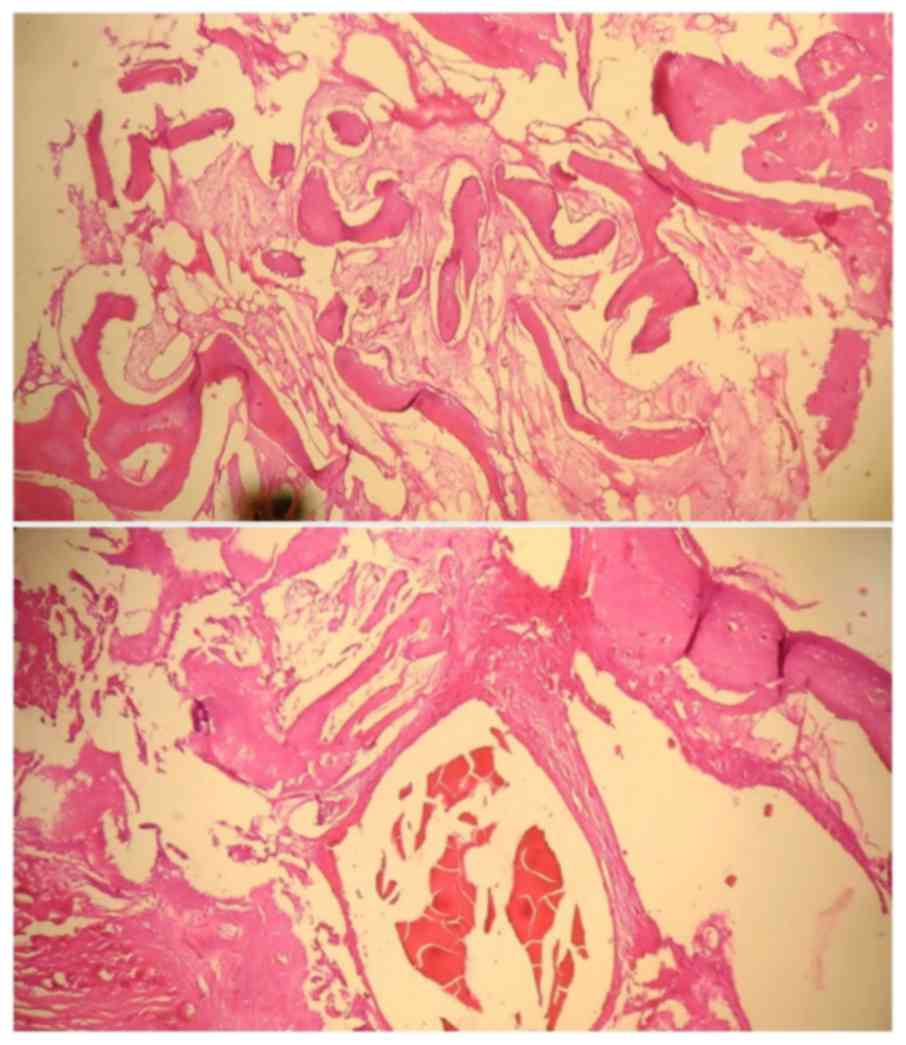
A biopsy was performed, which revealed that the cyst
was filled with serosanguinous fluid with a haemorrhagic tinge
(Fig. 3). After the diagnosis was
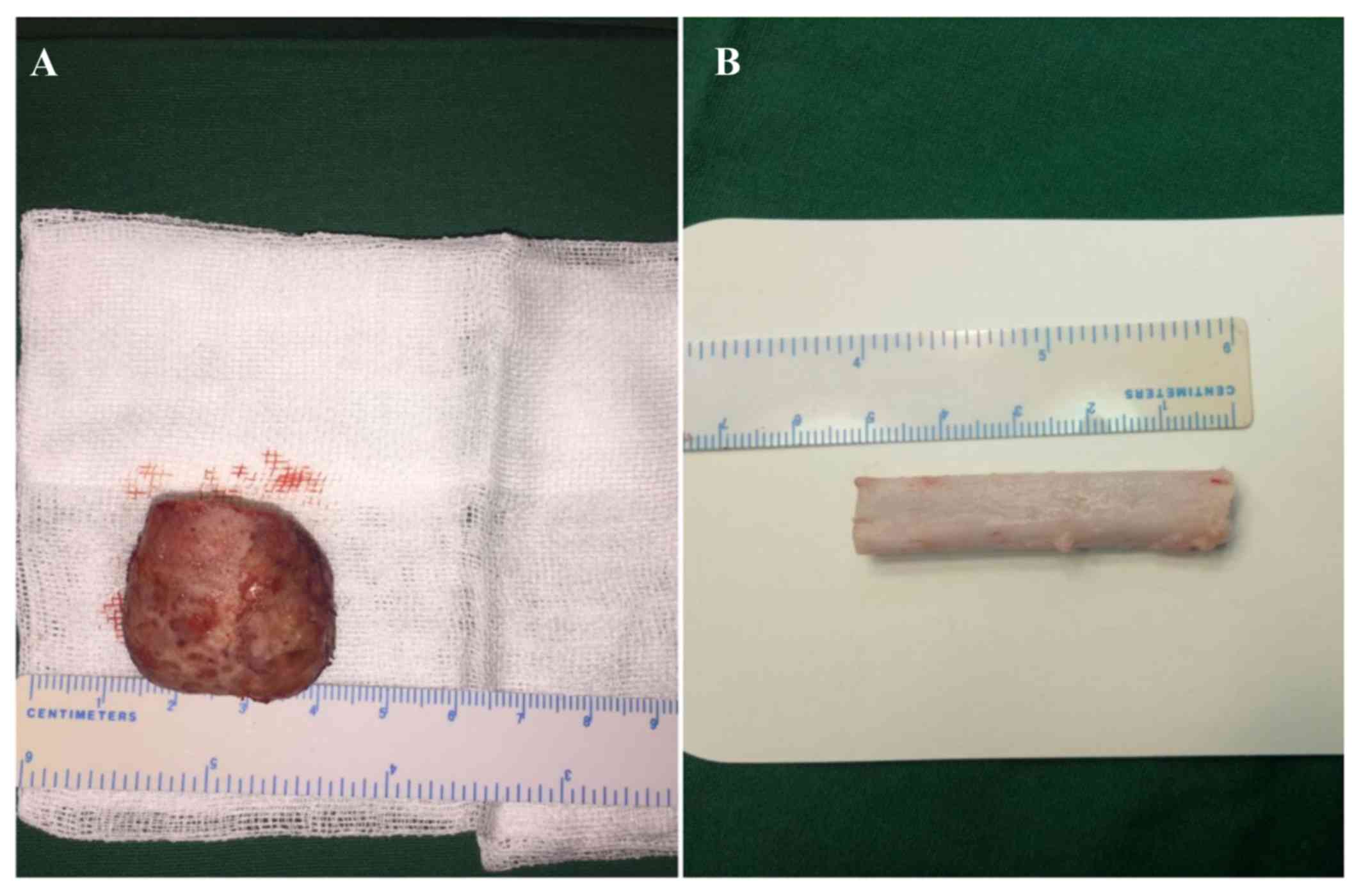
established, we decided to perform total resection of the cyst with
placement of a non-vascularized fibular graft. The cyst was
completely removed by resecting the shaft of the metacarpal with
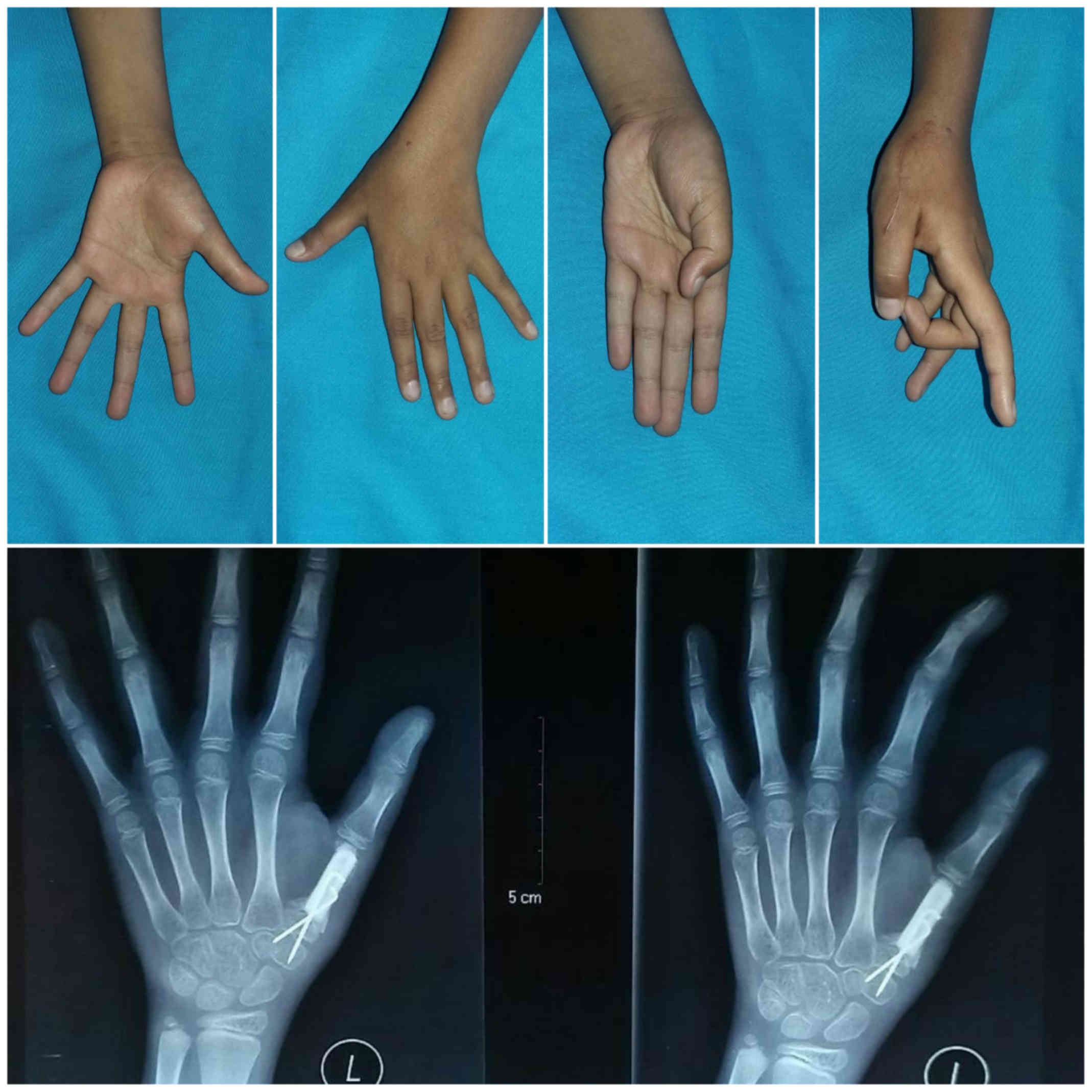
preservation of the epiphyseal plate (Fig. 4). A bone graft was obtained from the
fibula and inserted in the gap, distally attached to the epiphyseal
plate of the metacarpal and fixed with Kirshner wire proximally. A
radiograph revealed solid union of the bone graft to the epiphyseal
plate at the head after 7 weeks, with improving function of the
thumb. No recurrence has been reported after the last follow-up
appointment during January 2018 (Fig.
5).
Discussion
Simple bone cyst or UBC is a serous or
serosanguineous fluid-filled cavity that very rarely develops in
the metacarpal bone. The exact cause is unknown, but epiphyseal
plate defect or venous outflow obstruction have been suggested as
possible causes (3). Once diagnosed,
UBC poses a dilemma for clinicians, as its natural history and
management remain controversial. The recurrence rate of UBC ranges
from 20 to 50% after various treatments (5). The differential diagnosis includes
aneurysmal bone cyst and fibrous dysplasia. When additional
examinations are required, magnetic resonance imaging most
accurately delineates the central fluid collection. If a
pathological fracture has occurred, a fluid level may be observed,
mimicking the appearance of an aneurysmal bone cyst. There is no
convincing evidence, however, that a UBC may transform to an
aneurysmal bone cyst or other bone lesion (6). The gross pathology of UBC generally
includes a singular fluid-filled cavity, unlike an aneurysmal bone
cyst, which is composed of blood-filled cystic cavities that are
lined by a thick, fleshy membrane with an endothelial-like inner
layer. In some cases, multilocular lesions may be present. The bony
architecture surrounding the cyst is non-reactive and otherwise
unremarkable. Microscopic histological analysis shows a fibrous
tissue membrane, with occasional giant cells present. The fluid
within the cysts contains high levels of prostaglandins and enzymes
(7). Traditionally, plain
radiography has been used to diagnose and monitor UBCs, but
advanced imaging has become more popular as technology has
improved. On plain radiography, UBCs appear as lytic, expansile
lesions within the medullary cavity of long bones. The cortex is
thinned, but is not typically compromised structurally. Rarely, a
UBC may develop in the diaphyseal portion of long bones and is
known as a ‘latent’ cyst (8).
Among the various treatment methods mentioned above,
the choice of treatment may vary according to the patient's age,
the bone involved and the location of the cyst within the bone, and
proper treatment should be applied to decrease the risk of
recurrence (4,5). Several agents have been used for
intralesional injection of UBCs; Scaglietti et al first
described the use of methylprednisolone injections in patients with
UBCs. Recurrence rates of 15–88% have been reported after an
average of three injections (9).
A more aggressive approach, such as in the present
case, is occasionally necessary to treat UBC. The patient was
radically treated by complete excision and a fibular graft. Our
rationale was that, according to Jaffe (1), these cysts are active, as demonstrated
by complete destruction of the metacarpal bone; furthermore, the
patient was aged <10 years and was statistically more prone to
recurrence (10). This method may
also be used in other bone lesions, such as aneurysmal bone cyst,
as reported by Gundes et al (11), in 2005.
Before proceeding with treatment, a biopsy was
performed to confirm the diagnosis. We decided to perform total
resection of the cyst with preservation of the periosteum and
placement of a non-vascularized fibular graft. The proximal
epiphyseal plate was preserved and fixed with a Kirschner wire.
After 7 weeks, the function of the thumb was evaluated and union of
the graft was observed. There was no recurrence after 3 months of
follow-up, and the Kirschner wire was removed. The only known
predictor of treatment success is the age of the patient; patients
aged >10 years display higher rates of healing (90%) compared
with younger patients (60%), regardless of the treatment regimen
(8) due to the presence of the
active growth plate in younger patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
IGMOR and TECJH were involved in the drafting of the
manuscript and the revision of the manuscript for important
intellectual content. ARBS and SPPI made substantial contributions
to the design of the case report and were involved in the surgery.
III provided final approval of the version to be published. All the
authors have read and approved the final version of this
manuscript.
Ethics approval and consent to
participate
Ethics approval was obtained from the local Ethics
Committee of Saiful Anwar Hospital.
Patient consent for publication
The legal guardians of patients included in the
present study provided written, informed consent for the
publication of case details and associated photographs in this
manuscript.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jaffe HL: Tumors And Tumors Condition Of
The Bone And Joints. Lea & Febiger Publishing. (Philadelphia,
PA). 6291958.
|
|
2
|
Patwardhan S, Shah K, Shyam A and Sancheti
P: Simple bone cyst of metacarpal: Rare lesion with unique
treatment. J Orthop Case Rep. 4:63–65. 2014.PubMed/NCBI
|
|
3
|
Damron TA, Morris CD, Tornetta P and
Einhorn TA: Oncology and Basic Science. 7th. Lippincott Williams
& Wikins; pp. 1402008
|
|
4
|
McKay DW and Nasson SS: Treatment of
Unicameral bone cyst by subtotal resection without grafts. J Bone
Joint Surg. 55:59–68. 1943.
|
|
5
|
Neer CS II, Francis KC, Johnston AD and
Kiernan HA Jr: Current concepts on the treatment of solitary
unicameral bone cyst. Clin Orthop Relat Res. 97:40–51. 1973.
View Article : Google Scholar
|
|
6
|
Wilkins RM: Unicameral bone cysts. J Am
Acad Orthop Surg. 8:217–224. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Komiya S, Minamitani K, Sasaguri Y,
Hashimoto S, Morimatsu M and Inoue A: Simple bone cyst. Treatment
by trepanation and studies on bone resorptive factors in cyst fluid
with a theory of its pathogenesis. Clin Orthop Relat Res.
287:204–211. 1993.
|
|
8
|
Pretell-Mazzini J, Murphy RF, Kushare I
and Dormans JP: Unicameral bone cysts: General characteristics and
management controversies. J Am Acad Orthop Surg. 22:295–303. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scaglietti O, Marchetti PG and Bartolozzi
P: Final results obtained in the treatment of bone cysts with
methylprednisolone acetate (depo-medrol) and a discussion of
results achieved in other bone lesions. Clin Orthop Relat Res.
165:33–42. 1982.
|
|
10
|
Baruch A, Haas A, Lifschitz-Mercer B and
Zeligowsky A: Simple bone cyst of the metacarpal. J Hand Surg Am.
12:1103–1106. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gundes H, Tosun B, Muezzinoglu B and Tosun
A: Total destruction of the fourth metacarpal bone by aneurysmal
bone cyst: Reconstruction with strut fibular graft - a case report.
Hand Surg. 10:265–269. 2005. View Article : Google Scholar : PubMed/NCBI
|