Introduction
Colorectal cancer (CRC) is the third most common
type of cancer worldwide and is one of the leading causes of cancer
mortality (1). Mortality from CRC is
primarily due to metastatic progression (2) and treatment in the early stage of the
disease has been reported to have a high 5-year survival rate
(80–90%) compared with cases when the tumor has metastasized
(3). However, the majority of
patients are diagnosed when they are already in the advanced stage
of the disease. This is due to the fact that CRC may remain
asymptomatic until the disease has advanced. Furthermore,
diagnostic tests for CRC are invasive which may deter many patients
from undergoing screening.
The gold standards for screening and detection of
CRC are colonoscopy and sigmoidoscopy. These tests, apart from
being expensive and requiring skilled operators, are also invasive
and pose potential risks for complications particularly if
performed on the elderly or seriously ill patients. Therefore, the
non-invasive fecal occult blood test and fecal immunochemical test
are the more popular screening methods. However, these tests lack
sensitivity, particularly in detecting the early stage of the
disease. Therefore, the need for screening methods that are
non-invasive, specific and accurate for early identification of CRC
has spurred a number of researchers to turn to the use of molecular
techniques such as genomics, proteomics and, more recently,
metabolomics, to identify serum biomarkers.
Metabolomics is the comprehensive study of
low-molecular-mass metabolites in biological matrices. It is
downstream of genomics, transcriptomic and proteomics. Therefore,
alterations at the metabolomics level not only reflect the changes
at the genomics and proteomics levels, but also are influenced by
environmental factors. Differences in the levels of metabolites
between a diseased and the normal states are used to identify
altered metabolic pathways in that particular disease. In recent
years, metabolomics studies have been used successfully to identify
biomarkers and altered metabolic pathways in various cancer
systems, including gastric (4),
brain (5), breast (6) and lung (7) cancer.
Serum has been the sample of choice for the
identification of biomarkers as it reflects the metabolite profile
at the particular time when the sample is taken. Differences
observed in the metabolites from normal profiles may serve as
important indicators of the pathological states. Global serum
metabolomics has been used to identify early CRC biomarkers. Since
the altered metabolites may be influenced by biological and
environmental factors, it is important to determine the common
differentiating metabolites identified by the various studies which
may serve as potential common biomarkers for CRC. Therefore, in the
present systematic review, the results of the different studies on
global serum metabolomics on CRC were compared to identify any
common altered metabolites/biomarkers and the affected
pathways.
Search strategy
A literature search on metabolomics profiling of
colorectal cancer was conducted using EBSCO host, Web of Science
and PubMed electronic databases up to and including March 2018. The
search was conducted using the MeSH terms and Boolean operators:
Metabolomic* (OR) metabonomic* (OR) metabolite* (OR) metabolome
(OR) metabolic profiling in multiple combinations (AND) colorectal
(OR) colon (OR) bowel (OR) rectal (AND) cancer* (OR) tumor* (OR)
malignan* (OR) neoplas* (OR) benign* (OR) carcinoma* (OR) adenoma*.
The search was limited to the English language. Study titles and
abstracts were screened by four independent reviewers identified
through the electronic search. Full texts of potentially relevant
articles were then retrieved.
The inclusion criteria for the systematic review
included global metabolomics profiling studies on CRC using serum
or plasma. Exclusion criteria were studies on genomics,
transcriptomic and proteomics, studies on polyp colon disease,
animals and studies without a control group. Since the aim of the
systematic review was to identify common altered metabolites
reported, articles which did not include a report of the
metabolites identified were excluded. Sample types other than serum
such as tissue, urine and feces were excluded. Studies with
interventions including surgery or chemotherapy were also
excluded.
Study quality assessment
The Quality Assessment of Diagnostic Accuracy
Studies (QUADAS) tool (8) was used
to assess the quality of the included studies. It consists of 14
questions that evaluate spectrum, misclassification, disease
progression, partial verification, differential verification,
incorporation, review biases and bias associated with study
withdrawals and uninterpretable results. Each question was answered
with ‘yes’, ‘no’ or ‘unclear’. The answer ‘yes’ means that the risk
of bias is low, whereas the answer ‘no’ or ‘unclear’ means the risk
of bias is high.
Results
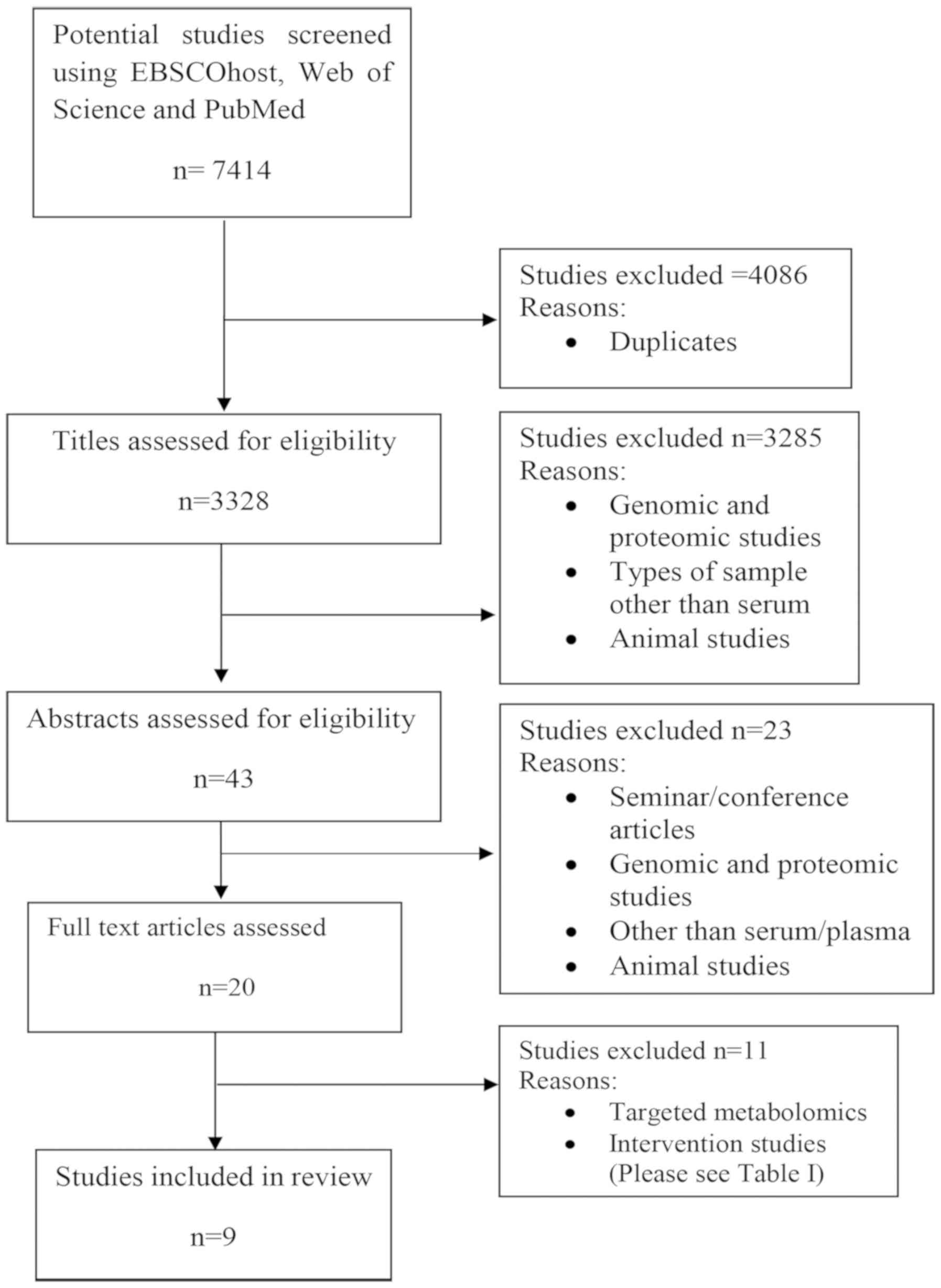
In total, 7,414 publications were identified during
the electronic database search. However, 4,086 were excluded
because they were duplicates. The remaining 3,328 titles were
screened by four independent reviewers who removed 3,285 studies
which did not meet the inclusion criteria. Abstracts of the
remaining 43 publications were then screened and 23 studies were
further excluded because they concerned genomics or proteomics, or
the index test was not serum or plasma. Abstracts presented in
seminars and conferences were also removed. This is because the
details on affected metabolites are needed for analysis in the
review. Only 20 publications were retrieved in full and reviewed in
detail (Fig. 1). A further 11 were
excluded for the reasons listed in Table
I. Ultimately, nine articles met the inclusion criteria and
were included in the present systematic review.
 | Table I.Excluded studies. |
Table I.
Excluded studies.
| No. | Study | Reason for
exclusion | (Refs.) |
|---|
| 1 | Ma et al,
2010 | The study used
subjects with surgical intervention | (9) |
| 2 | Bertini et
al, 2012 | Patients with CRC
with chemotherapy intervention | (10) |
| 3 | Zhu et al,
2014 | Targeted
metabolomics | (11) |
| 4 | Zhu et al,
2015 | Targeted
metabolomics | (2) |
| 5 | Guertin et
al, 2015 | The study
investigated the association between CRC and coffee
consumption | (12) |
| 6 | Dowling et
al, 2015 | Proteomic
studies | (13) |
| 7 | Crotti et
al, 2016 | Targeted
metabolomics; focus was on lipid metabolism | (14) |
| 8 | Farshidfar et
al, 2012 | Metabolite profile
was not reported | (15) |
| 9 | Farshidfar et
al, 2016 | Patients with CRC
undergoing chemotherapy | (16) |
| 10 | Vahabi et
al, 2017 | Comparing normal
and stage I CRC | (17) |
| 11 | Shu et al,
2018 | Sample collection
prior to cancer diagnosis | (18) |
Characteristics of studies
There were nine studies that met the inclusion
criteria in the present systematic review (19–27). All
nine studies presented the demographic data of their patients and
subjects. The index tests utilized for metabolomics analysis were
serum and plasma. The analytical platforms used for metabolite
detection included gas chromatography-mass spectrometry (GC-MS),
gas chromatography-triple-quadrupole mass spectrometry (GC-QqQ-MS),
gas chromatography-time-of-flight mass spectrometry (GC-TOF-MS),
high-resolution magic angle spinning-nuclear magnetic resonance
(1H-NMR), ultra-performance liquid chromatography-mass
spectrometry (UPLC-MS), ultra-performance liquid chromatography
quadrupole-time-of-flight mass spectrometry (UPLC-QTOF-MS) and
capillary electrophoresis-time-of-flight mass spectrometry
(CE-TOF-MS).
Summary of included studies
Table II presents a
brief summary of the characteristics of the included studies.
 | Table II.Characteristics of studies. |
Table II.
Characteristics of studies.
|
|
| Sample size |
|
|
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|---|
| Study | Country | Patients with
CRC | Healthy
controls | Polyps adenoma | Sample
extraction | Analytical
platform | Data analysis | Total metabolites
detected | No. of metabolites
significantly different | (Refs.) |
|---|
| Qiu et al,
2009 | China | 64 | 65 | – | Yes | GC-TOF-MS | MATLAB 7.0 | 22 | 21 | (19) |
|
|
|
|
|
|
| UPLC-TOF-MS | MarkerLynx 4.1 | 16 | 13 |
|
| Nishiumi et
al, 2012 | Japan | 60 | 60 | – | Yes | GC-MS | MetAlign | 126 | 54 | (20) |
| Tan et al,
2013 | China | 101 | 102 | – | Yes | GC-TOF-MS | ChromaTOF | 107 | 34 | (21) |
|
|
|
|
|
|
| UPLC-TOF-MS | MarkerLynx 4.1 | 147 | 44 |
|
| Cross et al,
2014 | USA | 254 | 254 | – | Yes | UPLC-GC-MS | SAS 9.1.3 and R
language 3.0.1 | 278 | 21 | (22) |
| Zamani et
al, 2014 | Iran | 33 | 33 | – | No | NMR | Chenomix 6.4 | 14 | 14 | (23) |
| Deng et al,
2016 | USA | 28 | 55 | 44 | No | NMR | Bruker TopSpin
3.5 | 70 | 5 | (24) |
| Uchiyama et
al, 2017 | Japan | 56 | 60 | 59 | Yes | CE-TOF-MS | PeakStat | 139 | 70 | (25) |
| Long et al,
2017 | USA | 30, 50 | 30, 50 | 30, 50 | Unknown | LC-MS | Stata version
10.1- | 404 | 50 | (26) |
| Nishiumi et
al, 2017 | Japan | 282 | 291 | – | Yes | GC-QqQ-MS | JMP12 | 64 | 41 | (27) |
Qiu et al, 2009 (19)
This study was conducted in China where the authors
analyzed serum metabolomics profiles using GC-TOF-MS and
UPLC-QTOF-MS. Fasting serum samples were collected from 64 patients
with CRC and 65 healthy subjects in the morning. Samples were
treated with methanol/chloroform (3:1) prior to metabolomics
analysis. The data were then analyzed using multivariate analysis
such as principal component analysis and orthogonal partial
least-squares-discriminant analysis (OPLS-DA) coupled with
univariate statistics. The authors were able to discriminate
altered metabolites between CRC and normal samples, but failed to
discriminate the different stages of the disease (stages I–IV).
There were 21 metabolites reported as being significantly different
between CRC and normal using GC-TOF-MS, and 13 metabolites
identified using UPLC-QTOF-MS. Of these metabolites, five were
detected by the two analytical platforms, including pyruvic acid,
lactic acid, tyrosine, uridine and tryptophan.
Nishiumi et al, 2012 (20)
This Japanese study aimed to identify novel early
biomarkers for CRC. Fasting blood samples were collected in the
early morning and the serum was treated with a
methanol/water/chloroform (2.5:1:1) mixture before analysis with
GC-MS. The study consisted of two sets of tests: Training and
validation sets. Serum samples from 60 patients with CRC and 60
healthy individuals were analyzed for the training set. In total,
54 metabolites were identified to be significantly different; four
metabolites, i.e. 2-hydroxybutyrate, aspartic acid, kynurenine and
cystamine, were subsequently used as their predictive model for CRC
and tested during the validation test. The protocol of the study
was well-described, including the stability studies of the
analytical platform using quality control samples.
Tan et al, 2013 (21)
These authors replicated their earlier study
(9) using the same analytical
platforms, i.e. GC-TOF-MS and UPLC-QTOF-MS, to analyze serum
samples from a new set of subjects which consisted of 62 patients
with CRC and 62 healthy controls. The authors reported 107 altered
metabolites using GC-TOF-MS and 147 metabolites when UPLC-TOF-MS
was used. Metabolomics profile data obtained from the two platforms
were then combined and analyzed using OPLS-DA; 249 differentiating
metabolites were identified. A prediction model was then developed
and validated on serum samples from 39 patients with CRC and 40
healthy controls. The authors provided a comprehensive protocol of
their methodologies including statistical analysis.
Cross et al, 2014 (22)
This study was conducted in the USA. Serum samples
were collected from 254 patients with CRC and 254 controls, and
were analyzed for global metabolomics using UPLC-MS and GC-MS.
Samples were first treated with methanol to precipitate the
proteins prior to vacuum-drying. The samples for UPLC-MS analysis
were reconstituted in 50 µl 0.1% formic acid in water, whereas for
GC-MS analysis, aliquots were derivatized using equal parts
bis(trimethylsilyl)trifluoroacetamide and solvent mixture of
acetonitrile/dichloromethane/cyclohexane (5:4:1, by vol.) with 5%
trimethylamine. The authors reported 278 altered metabolites, of
which only 21 metabolites were identified to be significantly
different between patients with CRC and normal controls. However,
following Bonferroni correction for multiple comparisons, no
association between the metabolites and CRC was identified.
Zamani et al, 2014 (23)
A total of 33 serum samples from Iranian patients
with CRC on a liquid diet and 33 healthy controls were analyzed
using 1H-NMR. The authors identified 14 differentiating
metabolites which were statistically significant between patients
with CRC and healthy individuals.
Deng et al, 2016 (24)
The authors performed global metabolomics on 28
patients with CRC, 44 patients with polyps and 55 healthy controls
in the USA, using NMR. The results were then validated using
targeted metabolomics with LC-tandem MS (MS/MS). In total, 70
differentiating metabolites were identified, of which five were
significantly different. The authors also reported that the altered
pathways in CRC were glycolysis, tricarboxylic acid (TCA) cycle,
fatty acid metabolism, amino acid metabolism and
glutaminolysis.
Uchiyama et al, 2017 (25)
Serum samples were obtained from 56 patients with
CRC, 60 healthy controls and 59 patients with colonic adenoma in
Japan. The samples were analyzed using CE-TOF-MS using the Advanced
Scan package (Human Metabolome Technologies, Yamagata, Japan). In
total, 139 metabolites were identified that were distinguishable
from controls, of which 70 were statistically significant; 16 of
these metabolites were reported to be correlated with CRC stages.
Benzoic acid was identified as the best candidate for CRC
biomarkers.
Long et al, 2017 (26)
This study was conducted in the USA and consisted of
two phases: Discovery phase and validation phase. Blood samples
were collected from 30 healthy controls, 30 patients with
colorectal adenoma polyps and 30 patients with CRC for global
metabolomics profile analysis using LC-MS. In the validation phase,
targeted metabolomics was performed to validate the biomarkers
identified earlier in the discovery phase using LC-MS/MS on a new
set of samples comprising 50 healthy controls, 50 patients with
polyps and 50 patients with CRC. Lower levels of xanthine and
hypoxanthine, and higher levels of D-mannose were identified in
polyps and CRC cases compared with controls.
Nishiumi et al, 2017 (27)
This study used GC-QqQ-MS to analyze plasma from 282
Japanese patients with CRC and 291 healthy volunteers. The study
differed from the other studies in that CRC samples were collected
from patients at stage I and II of the disease. Following
statistical analysis, eight metabolites were used in their
predictive model, i.e. pyruvic acid, glycolic acid, tryptophan,
palmitoleic acid, fumaric acid, ornithine, lysine and
3-hydroxyisovaleric acid.
Methodological quality of included
studies
The quality assessment results for the individual
studies are presented in Table
III. All studies described the demographic, clinical features
and the inclusion and exclusion criteria of their subjects clearly.
The diagnosis of study groups was confirmed by colonoscopy and
biopsy which was the reference standard for all studies. This
eliminated differential verification bias and partial verification
bias. However, the majority of the studies reviewed did not
indicate the duration of storage for samples before analyses.
Overall, the strength of these studies was in the technical aspects
of test description, but were limited in the amount of information
regarding blinded samples during the experiment.
 | Table III.Quality assessment of included
studies. |
Table III.
Quality assessment of included
studies.
|
|
| Study |
|---|
|
|
|
|
|---|
| No. | Question | Qiu et al,
2009 (19) | Nishiumi et
al, 2012 (20) | Tan et al,
2013 (21) | Cross et al,
2014 (22) | Zamani et
al, 2014 (23) | Deng et al,
2014 (24) | Uchiyama et
al, 2016 (25) | Long et al,
2017 (26) | Nishiumi et
al, 2017 (27) |
|---|
| 1 | Was the spectrum of
patients representative of the patients who will receive the test
in practice? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2 | Were selection
criteria clearly described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3 | Is the reference
standard likely to correctly classify the target condition? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4 | Is the period
between reference standard and index test short enough to be
reasonably sure that the target condition did not alter between the
two tests? | Unclear | Unclear | Unclear | Unclear | Unclear | Yes | Unclear | Unclear | Unclear |
| 5 | Did the whole
sample, or a random selection of the sample, receive verification
using a reference standard of diagnosis? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6 | Did patients
receive the same reference standard regardless of the index test
results? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7 | Was the reference
standard independent of the index test (i.e. the index text did not
form part of the reference standard)? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 8 | Was the execution
of the index test described in sufficient detail to permit
replication of the test? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9 | Was the execution
of the reference standard described in sufficient detail to permit
its replication? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10 | Were the index
tests results interpreted without knowledge of the results of the
reference standard? | No | No | No | No | No | No | No | No | No |
| 11 | Were the reference
standard results interpreted without knowledge of the results of
the index test? | No | No | No | No | No | No | No | No | No |
| 12 | Were the same
clinical data available when test results were interpreted as would
be available when the test is used in practice? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 13 | Were
uninterpretable/intermediate test results reported? | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| 14 | Were withdrawals
from the study explained? | No | No | No | No | No | No | No | No | No |
Altered metabolites
The numbers of differentiating metabolites that were
significantly different between patients with CRC and normal
controls identified by the studies differ. Furthermore, different
studies detected different affected metabolites. The suggested
biomarkers also differed in each study. However, there were some
common altered metabolites detected among the studies. For the
purpose of the present review, differentiating metabolites reported
by more than four studies are identified (Table IV) and discussed.
 | Table IV.Differentiating metabolites
identified by four or more studies. |
Table IV.
Differentiating metabolites
identified by four or more studies.
| Metabolite | GC-TOF-MS Qiu et
al, 2009 (19) | UPLC-TOF-MS | GC-MS Nishiumi
et al, 2012 (20) | GC-TOF-MS Tan et
al, 2013 (21) | UPLC-TOF-MS | UPLC-GC-MS Cross
et al, 2014 (22) | NMR Zamani et
al, 2014 (23) | NMR Deng et
al, 2016 (24) | CE-TOF-MS Uchiyama
et al, 2017 (25) | LC-MS Long et
al, 2017 (26) | GC-QqQ-MS Nishiumi
et al, 2017 (27) |
|---|
| Pyruvic acid | ↑ | ↑ | ↑ | ↑ |
|
|
|
|
| ↑ | ↑ |
| Glucose |
|
| ↓ |
|
|
|
| ↑ |
| ↑ | ↓ |
| Lactic acid | ↑ | ↑ | ↓ |
|
|
|
|
|
| ↓ | ↑ |
| Malic acid | ↑ |
| ↑ |
|
|
|
|
|
| ↓ | ↑ |
| Fumaric acid |
|
|
| ↓ |
| ↑ |
|
|
| ↓ | ↑ |
| 3-Hydroxybutyric
acid | ↑ |
| ↑ | ↑ |
|
| ↓ |
| ↑ |
|
|
| Ornithine | ↓ |
| ↑ | ↓ |
|
|
|
| ↓ | ↓ | ↑ |
| Tryptophan | ↓ |
|
| ↓ |
|
|
|
| ↓ |
| ↓ |
| Phenylalanine |
| ↓ | ↑ | ↓ | ↓ |
|
| ↑ | ↓ |
|
|
| Tyrosine | ↓ | ↓ | ↑ |
|
|
|
|
| ↓ |
| ↓ |
| Creatinine |
|
| ↓ | ↑ | ↑ |
|
| ↓ |
|
| ↑ |
There were 11 metabolites identified to be
significantly different between CRC and normal individuals by four
or more studies reviewed (Table
IV). These metabolites included pyruvic acid, glucose, lactic
acid, malic acid, fumaric acid, 3-hydroxybutyric acid, tryptophan,
phenylalanine, tyrosine, creatinine and ornithine.
The data in Table IV
indicate that three metabolites of the glycolytic pathway were
altered in CRC. Pyruvic acid was reported to be upregulated in five
studies (19–21,26,27).
Glucose was reported to be downregulated in two studies (20,26) and
upregulated in another two studies (24,26).
Similarly, two studies reported downregulation of lactic acid
(20,26), whereas two other studies identified
it to be upregulated (19,27). Among the metabolites of the TCA
cycle, upregulation of malic acid was reported by three studies
(19,20,27),
whereas one study reported it to be downregulated (26). Fumaric acid was reported to be
upregulated by two studies (22,27) and
downregulated in another two (21,26).
In general, there were fewer agreements in the
reported metabolites of lipid metabolism among the studies.
However, 3-hydroxybutyrate was reported by five studies to be
altered; four studies noted the upregulation of this lipid
(19–21,25),
whereas one study identified it to be downregulated (23).
There were five altered metabolites of protein/amino
acid metabolism reported by more than four studies: Ornithine,
tryptophan, phenylalanine, tyrosine, and creatinine (Table IV). In total, six studies identified
altered levels of ornithine; four of these studies reported
downregulation of ornithine (19,21,25,26),
whereas the other two noted its upregulation (20,26).
Tryptophan was identified to be downregulated in four studies in
CRC (19,21,25,27).
Downregulation of phenylalanine was reported in three studies
(19,21,25),
whereas two studies identified that it was upregulated in CRC
(20,24). With regard to tyrosine, three studies
reported downregulation (19,25,27),
whereas one study reported upregulation (20), in CRC. Creatinine was reported to be
downregulated in two studies (20,24) and
upregulated in two other studies (21,27).
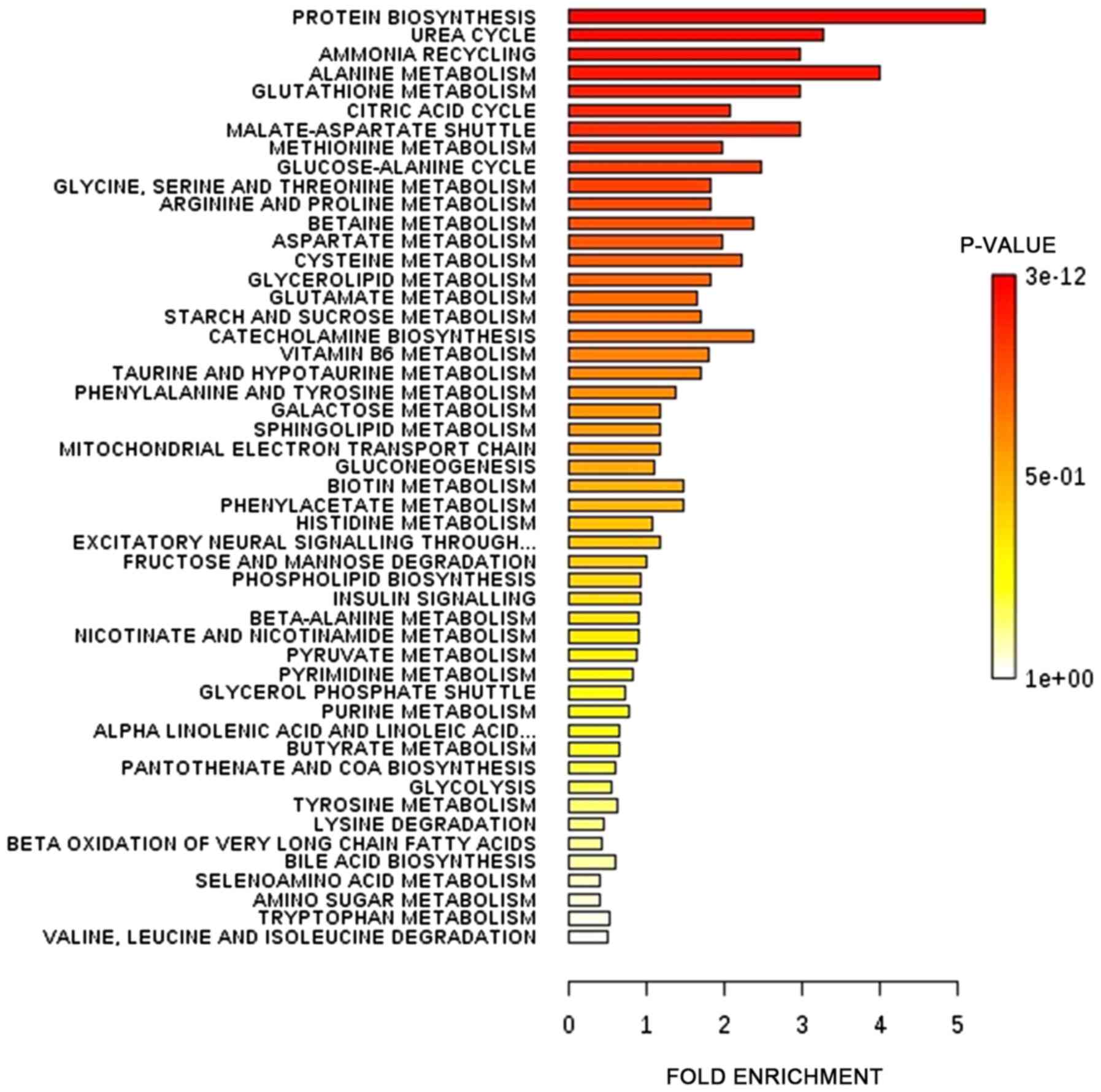
Metabolic pathways
The differential metabolites identified by all
studies under review were enriched into pathways. The enrichments
were performed using MetaboAnalyst software (version 4.0;
www.metaboanalyst.ca). Fig. 2 presents the affected pathways when
data from all the studies were enriched into pathways. The six most
affected pathways affected in CRC as presented in Fig. 2 were protein biosynthesis, urea
cycle, ammonia recycling, alanine metabolism, glutathione
metabolism and citric acid cycle.
Discussion
Serum metabolomics profiling has been aided by the
development of techniques which separate, detect, characterize and
quantify the metabolomes. The studies investigated in the present
systematic review used six different analytical platforms, which
were UPLC-QTOF-MS, LC-MS, GC-MS, GC-TOF-MS, CE-TOF-MS, GC-QqQ-MS
and NMR. The study populations were Chinese (19,21),
Japanese (20,25,27),
Iranian (23) and American (22,24,26). To
interpret the complex metabolomics data, each study used different
software as presented in Table II.
Qiu et al (19) and Tan et
al (21) analyzed their data
using ChromaTOF and MarkerLynx Application Manager software.
Nishiumi et al (20) used
MetAlign and SIMCA software, whereas Nishiumi et al
(27) used GCMS Solution Software
and JMP12 software for statistical analysis. Zamani et al
(23) used Chenomix 6.4 software.
Uchiyama et al (25) used HMT
Advanced Scan package for metabolome analysis and PeakStat for
statistical analysis. Long et al (26) used Stata software in their
statistical analysis.
The results of the present systematic review
confirmed an earlier review by Kim et al (28) that different analytical platforms
detect different altered metabolomes. The studies by Qiu et
al (19) and Tan et al
(21) on two different analytical
platforms illustrated this fact despite conducting the analysis on
the same samples. The differences in metabolites identified may be
due to differences in the techniques of separation and detection of
the different platforms. Furthermore, sample preparations were also
different. GC-MS detects low-molecular-mass (between 18 and 350 Da)
metabolites, including amino acids and organic acids, fatty acids,
carbohydrates and cholesterol (19),
whereas UPLC-MS detects higher-molecular-mass compounds of
medium-to-high lipophilicity, including lipids (29). Amino acids with a molecular mass
>147 Da can be detected by UPLC-MS. NMR has lower sensitivity
and therefore detects compounds that are present in high amounts.
Sample preparation also differs according to the analytical
platform used. Analysis using GC-MS involves sample derivatization,
whereas LC-MS requires the metabolites to be extracted from the
serum; however, little or no sample preparation is required for NMR
(30). In addition, there were also
differences in the study design. Certain authors reported the
metabolomics profiles following global analysis, whereas others
went on to validate their results using targeted metabolomics
analysis.
Another notable result is the difference in the
altered metabolomes detected in the different populations such as
Chinese (19,21), Japanese (20,25,27),
Iranian (23) and American (22,24,26).
This is not surprising as metabolomes have been identified to be
affected by genetics as well as environmental factors such as
nutrition and lifestyle (31).
Furthermore, the cancer screening policies and levels of medical
intervention differ in different countries. In certain countries,
there are more patients in the early stage, whereas others
diagnosed more patients at the metastatic stage. This may account
for the differing numbers of patients at each stage of the disease
and may affect the metabolomics profiles obtained. The same concern
can also be applied to the different time of the study conducted.
Since the present systematic review included only nine studies
which used five different analytical platforms on four different
populations, it is suggested that more studies are required to
confirm the effect of populations on the metabolomics profiles.
This is important as it may signify differences in the sensitivity
and specificity of biomarkers for the detection of CRC in different
populations.
For the purpose of the present review, the
metabolites whose levels were altered in CRC compared with normal
individuals identified by four or more studies are considered
common altered metabolites. Therefore, the present review
identified that the metabolites most affected in CRC are the
metabolites of energy pathways, protein/amino acid and lipid
metabolism (Table IV). However,
different studies reported different expression of the metabolites,
with the exception of pyruvic acid and tryptophan. The reason for
this difference is unclear. The CRC subjects included patients at
different stages of the disease and each study differed in the
percentage of subjects at the different stages. Since the
metabolism may differ at different stages of cancer progression,
this may account for the stated observation. Furthermore, serum
metabolomics profiling provides a snapshot of metabolism at that
instant within the cells.
Pyruvic acid, glucose and lactic acid were the most
commonly reported metabolites of glycolysis altered in CRC. Malic
acid and fumaric acid, intermediates of the TCA cycle, were also
commonly reported in the studies reviewed. High cellular glucose
metabolism in cancer has been suggested to provide energy and
precursors for the increased rate of anabolic processes in cancer
cells (32). This is achieved by
reprogramming of glucose metabolism which involves the activation
of phosphoinositide 3-kinase and its downstream protein kinase B
and mammalian target of rapamycin (mTOR) signaling pathways. The
events of glucose reprogramming in cancer has been well-reviewed by
Hay (33). The increased glycolysis
is not met with an increased rate of oxidative phosphorylation in
cancer cells because their proliferation rate often exceeds the
rate of angiogenesis (34).
Therefore, increased production of pyruvate from glycolysis leads
to lactic acid production. The metabolic adaptation to hypoxia is
coordinated by hypoxia-inducible factor 1 (35) through a variety of mechanisms,
including hyperactivation of mTOR complex 1, accumulation of
reactive oxygen species (ROS) and accumulation of the citric acid
cycle metabolites (36).
Amino acids are important as building materials and
as nutrient signals that regulate important signaling pathways
(37). The amino acids ornithine,
tryptophan, phenylalanine, tyrosine and creatinine were reported to
be altered in CRC by the majority of the studies reviewed (Table IV), suggesting the potential of
using these amino acids as biomarkers. Tryptophan metabolism is an
important mechanism exploited by cancer to evade immune
surveillance (38). Tryptophan is an
essential amino acid and 95% of dietary tryptophan is metabolized
along the kynurenine pathway (39).
Decrease tryptophan levels are associated with catabolism of
tryptophan into kynurenine via the kynurenine pathway (40). Mezrich et al (41) suggested that kynurenine binds to aryl
hydrocarbon receptor to promote the generation of
immune-suppressive T cells that support cancer development.
Tyrosine is phosphorylated by tyrosine kinases, and
phosphorylated tyrosine acts in signal transduction and the
regulation of enzyme activity. One such enzyme is pyruvate
dehydrogenase kinase 1 which has been suggested to be involved in
the promotion of the Warburg effect and cell proliferation
(42).
It is interesting to note that the ornithine level
was identified to be altered in CRC by six of the studies reviewed.
Ornithine is catabolized by ornithine decarboxylase (ODC) in the
pathway for polyamine synthesis. Polyamines are important molecules
for normal cell proliferation and are highly expressed in various
malignancies (43). Hoshino et
al (44) reported that the ODC
level is increased in CRC tumor cells compared with normal
tissues.
Increased levels of lipid metabolic intermediates
are primarily used for energy storage (45). Menendez and Lupu (46) suggested that lipid synthesis serves
an important function in tumor pathogenesis (46). In the present review, five studies
reported that 3-hydroxybutyric acid level was altered in CRC.
3-Hydroxybutyric acid is among the components of ketone bodies and
the altered levels may indicate increased protein catabolism
particularly involving the ketogenic branched-chain amino acids
(BCAAs) and increased fatty acid oxidation.
The significance of the altered metabolites is
reflected in the pathways affected (Fig.
2). Tumors are associated with increased protein synthesis
required for cell proliferation. The increase in urea cycle,
ammonia recycling and alanine metabolism may indicate increased
muscle proteolysis generating BCAAs which are subsequently oxidized
via the citric acid cycle, to meet the increased energy demand of a
tumor cell. The data in Fig. 2 also
indicated that glutathione metabolism is affected in CRC. The
increased metabolic activity of cancer cells leads to increase
production of ROS. ROS serve a significant function in the
pathogenesis of cancer by activating signaling pathways that
support cell proliferation, survival and metabolic adaptation.
However, high levels of ROS may cause cell damage. Therefore,
tumour cells react by producing glutathione, an antioxidant, to
prevent ROS from reaching toxic levels (47).
Limitations
The number of published papers on global serum
metabolomics that were included in the present systematic review is
small, indicating an inadequate amount of research in this area.
Different metabolite markers were identified by the different
studies which were influenced by the analytical platforms used, the
study design, stage of CRC, statistical analysis and the
populations studied. Although certain common metabolites were
identified, further studies are required to verify and identify
distinguishable metabolites in patients with CRC from those in
normal individuals in different populations, perhaps with
standardized sample preparation and measurement and analysis of
data.
Conclusion
Enrichment pathway analysis using data from all
studies included indicated that protein biosynthesis, urea cycle,
ammonia recycling, alanine metabolism, glutathione metabolism and
citric acid cycle were among the most affected pathways. However,
the altered metabolites in patients with CRC compared with in
healthy individuals were identified to be different among different
studies owing to differences in sample analysis and populations.
Tryptophan, phenylalanine, tyrosine, ornithine, creatinine, pyruvic
acid, glucose, lactic acid, malic acid, fumaric acid and
3-hydroxybutyrate were the altered metabolites identified by more
than four of the studies reviewed. Further studies are required to
determine whether metabolites can serve as common biomarkers for
CRC in different populations.
Acknowledgements
The authors would like to thank the Ministry of
Education Malaysia for providing the research grant. The authors
would also like to thank Professor Datuk Abdul Rahman A. Jamal who
secured funding for the present study.
Funding
The present study was funded by a Long Term Research
Grant of the Ministry of Higher Education, Malaysia (grant no.
LRGS/2014/UKM-UiTM/K/03).
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article [and its supplementary
information files].
Authors' contributions
NAAH searched for the published articles, performed
the analysis and wrote the manuscript. SAR, LSS, MSAS and MM were
involved in evaluating and reviewing the titles, abstracts and full
papers and determining the quality of papers (using QUADAS) and
that the papers included in the review fulfilled the inclusion and
exclusion criteria. They were also involved in generating ideas in
the content of the manuscript as well as editing the manuscript
prior to submission. MM conceptualized the idea for the review,
arranged for the writing and co-wrote and edited the manuscript
prior to submission.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhu J, Djukovic D, Deng L, Gu H, Himmati
F, Abu Zaid M, Chiorean EG and Raftery D: Targeted serum metabolite
profiling and sequential metabolite ratio analysis for colorectal
cancer progression monitoring. Anal Bioanal Chem. 407:7857–7863.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
American Cancer Society: Cancer facts and
figures 2013. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2013/cancer-facts-and-figures-2013.pdfAccessed
Month day, year.
|
|
4
|
Wang D, Li W, Zou Q, Yin L, Du Y, Gu J and
Suo J: Serum metabolomic profiling of human gastric cancer and its
relationship with the prognosis. Oncotarget. 8:110000–110015.
2017.PubMed/NCBI
|
|
5
|
Chinnaiyan P, Kensicki E, Bloom G, Prabhu
A, Sarcar B, Kahali S, Eschrich S, Qu X, Forsyth P and Gillies R:
The metabolomic signature of malignant glioma reflects accelerated
anabolic metabolism. Cancer Res. 72:5878–5888. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hadi NI, Jamal Q, Iqbal A, Shaikh F,
Somroo S and Musharraf SG: Serum metabolomic profiles for breast
cancer diagnosis, grading and staging by gas chromatography-mass
spectrometry. Sci Rep. 7:17152017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kumar N, Shahjaman M, Mollah MNH, Islam
SMS and Hoque MA: Serum and plasma metabolomic biomarkers for lung
cancer. Bioinformation. 13:202–208. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Whiting P, Rutjes AW, Reitsma JB, Bossuyt
PM and Kleijnen J: The development of QUADAS: A tool for the
quality assessment of studies of diagnostic accuracy included in
systematic reviews. BMC Med Res Methodol. 3:252003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ma Y, Liu W, Peng J, Huang L, Zhang P,
Zhao X, Cheng Y and Qin H: A pilot study of gas chromatograph/mass
spectrometry-based serum metabolic profiling of colorectal cancer
after operation. Mol Biol Rep. 37:1403–1411. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bertini I, Cacciatore S, Jensen BV, Schou
JV, Johansen JS, Kruhøffer M, Luchinat C, Nielsen DL and Turano P:
Metabolomic NMR fingerprinting to identify and predict survival of
patients with metastatic colorectal cancer. Cancer Res. 72:356–364.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhu J, Djukovic D, Deng L, Gu H, Himmati
F, Chiorean EG and Raftery D: Colorectal cancer detection using
targeted serum metabolic profiling. J Proteome Res. 13:4120–4130.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Guertin KA, Loftfield E, Boca SM, Sampson
JN, Moore SC, Xiao Q, Huang WY, Xiong X, Freedman ND, Cross AJ and
Sinha R: Serum biomarkers of habitual coffee consumption may
provide insight into the mechanism underlying the association
between coffee consumption and colorectal cancer. Am J Clin Nutr.
101:1000–1011. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dowling P, Hughes DJ, Larkin AM, Meiller
J, Henry M, Meleady P, Lynch V, Pardini B, Naccarati A, Levy M, et
al: Elevated levels of 14-3-3 proteins, serotonin, gamma enolase
and pyruvate kinase identified in clinical samples from patients
diagnosed with colorectal cancer. Clin Chim Acta. 441:133–141.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Crotti S, Agnoletto E, Cancemi G, Di Marco
V, Traldi P, Pucciarelli S, Nitti D and Agostini M: Altered plasma
levels of decanoic acid in colorectal cancer as a new diagnostic
biomarker. Anal Bioanal Chem. 408:6321–6328. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Farshidfar F, Weljie AM, Kopciuk K, Buie
WD, Maclean A, Dixon E, Sutherland FR, Molckovsky A, Vogel HJ and
Bathe OF: Serum metabolomic profile as a means to distinguish stage
of colorectal cancer. Genome Med. 4:422012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Farshidfar F, Weljie AM, Kopciuk KA,
Hilsden R, McGregor SE, Buie WD, MacLean A, Vogel HJ and Bathe OF:
A validated metabolomic signature for colorectal cancer:
Exploration of the clinical value of metabolomics. Br J Cancer.
115:848–857. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vahabi F, Sadeghi S, Arjmand M, Mirkhani
F, Hosseini E, Mehrabanfar M, Hajhosseini R, Iravani A, Bayat P and
Zamani Z: Staging of colorectal cancer using serum metabolomics
with 1HNMR Spectroscopy. Iran J Basic Med Sci.
20:835–840. 2017.PubMed/NCBI
|
|
18
|
Shu X, Xiang YB, Rothman N, Yu D, Li HL,
Yang G, Cai H, Ma X, Lan Q, Gao YT, et al: Prospective study of
blood metabolites associated with colorectal cancer risk. Int J
Cancer. 143:527–534. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qiu Y, Cai G, Su M, Chen T, Zheng X, Xu Y,
Ni Y, Zhao A, Xu LX, Cai S and Jia W: Serum metabolite profiling of
human colorectal cancer using GC-TOFMS and UPLC-QTOFMS. J Proteome
Res. 8:4844–4850. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nishiumi S, Kobayashi T, Ikeda A, Yoshie
T, Kibi M, Izumi Y, Okuno T, Hayashi N, Kawano S, Takenawa T, et
al: A novel serum metabolomics-based diagnostic approach for
colorectal cancer. PLoS One. 7:e404592012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tan B, Qiu Y, Zou X, Chen T, Xie G, Cheng
Y, Dong T, Zhao L, Feng B, Hu X, et al: Metabonomics identifies
serum metabolite markers of colorectal cancer. J Proteome Res.
12:3000–3009. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cross A, Moore SC, Boca S, Huang WY, Xiong
X, Stolzenberg-Solomon R, Sinha R and Sampson JN: A prospective
study of serum metabolites and colorectal cancer risk. Cancer.
120:3049–3057. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zamani Z, Arjmand M, Vahabi F, Eshaq
Hosseini SM, Fazeli SM, Iravani A, Bayat P, Oghalayee A,
Mehrabanfar M, Haj Hosseini R, et al: A metabolic study on colon
cancer using (1)h nuclear magnetic resonance spectroscopy. Biochem
Res Int. 2014:3487122014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Deng L, Gu H, Zhu J, Nagana Gowda GA,
Djukovic D, Chiorean EG and Raftery D: Combining NMR and LC/MS
using backward variable elimination: Metabolomics analysis of
colorectal cancer, polyps, and healthy controls. Anal Chem.
88:7975–7983. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Uchiyama K, Yagi N, Mizushima K,
Higashimura Y, Hirai Y, Okayama T, Yoshida N, Katada K, Kamada K,
Handa O, et al: Serum metabolomics analysis for early detection of
colorectal cancer. J Gastroenterol. 52:677–694. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Long Y, Sanchez-Espiridion B, Lin M, White
L, Mishra L, Raju GS, Kopetz S, Eng C, Hildebrandt MAT, Chang DW,
et al: Global and targeted serum metabolic profiling of colorectal
cancer progression. Cancer. 123:4066–4074. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nishiumi S, Kobayashi T, Kawana S, Unno Y,
Sakai T, Okamoto K, Yamada Y, Sudo K, Yamaji T, Saito Y, et al:
Investigations in the possibility of early detection of colorectal
cancer by gas chromatography/triple-quadrupole mass spectrometry.
Oncotarget. 8:17115–17126. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kim SJ, Kim SH, Kim JH, Hwang S and Yoo
HJ: Understanding metabolomics in biomedical research. Endocrinol
Metab (Seoul). 31:7–16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dunn WB, Broadhurst D, Begley P, Zelena E,
Francis-McIntyre S, Anderson N, Brown M, Knowles JD, Halsall A,
Haselden JN, et al: Procedures for large-scale metabolic profiling
of serum and plasma using gas chromatography and liquid
chromatography coupled to mass spectrometry. Nat Protoc.
6:1060–1083. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Serkova NJ, Standiford TJ and Stringer KA:
The emerging field of quantitative blood metabolomics for biomarker
discovery in critical illnesses. Am J Respir Crit Care Med.
184:647–655. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kastenmüller G, Raffler J, Gieger C and
Suhre K: Genetics of human metabolism: An update. Hum Mol Genet.
24:R93–R101. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ahn CS and Metallo CM: Mitochondria as
biosynthetic factories for cancer proliferation. Cancer Metab.
3:12015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Hay N: Reprogramming glucose metabolism in
cancer: Can it be exploited for cancer therapy? Nat Rev Cancer.
16:635–649. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jain RK, Munn LL and Fukumura D:
Dissecting tumour pathophysiology using intravital microscopy. Nat
Rev Cancer. 2:266–276. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
35
|
Semenza GL: Hypoxia-inducible factors in
physiology and medicine. Cell. 148:399–408. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kaelin WG Jr and Ratcliffe PJ: Oxygen
sensing by metazoans: The central role of the HIF hydroxylase
pathway. Mol Cell. 30:393–402. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ananieva E: Targeting amino acid
metabolism in cancer growth and anti-tumor immune response. World J
Biol Chem. 6:281–289. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Prendergast GC, Smith C, Thomas S,
Mandik-Nayak L, Laury-Kleintop L, Metz R and Muller AJ: Indoleamine
2,3-dioxygenase pathways of pathogenic inflammation and immune
escape in cancer. Cancer Immunol Immunother. 63:721–735. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Peters JC: Tryptophan nutrition and
metabolism: An overview. Adv Exp Med Biol. 294:345–358. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Grohmann U and Bronte V: Control of immune
response by amino acid metabolism. Immunol Rev. 236:243–264. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Mezrich JD, Fechner JH, Zhang X, Johnson
BP, Burlingham WJ and Bradfield CA: An interaction between
kynurenine and the aryl hydrocarbon receptor can generate
regulatory T cells. J Immunol. 185:3190–3198. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hitosugi T, Fan J, Chung TW, Lythgoe K,
Wang X, Xie J, Ge Q, Gu TL, Polakiewicz RD, Roesel JL, et al:
Tyrosine phosphorylation of mitochondrial pyruvate dehydrogenase
kinase 1 is important for cancer metabolism. Mol Cell. 44:864–877.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Pegg AE: Functions of polyamines in
mammals. J Biol Chem. 291:14904–14912. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Hoshino Y, Terashima S, Teranishi Y,
Terashima M, Kogure M, Saitoh T, Osuka F, Kashimura S, Saze Z and
Gotoh M: Ornithine decarboxylase activity as a prognostic marker
for colorectal cancer. Fukushima J Med Sci. 53:1–9. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Santos CR and Schulze A: Lipid metabolism
in cancer. FEBS J. 279:2610–2623. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Menendez JA and Lupu R: Fatty acid
synthase and the lipogenic phenotype in cancer pathogenesis. Nat
Rev Cancer. 7:763–777. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Benlloch M, Ortega A, Ferrer P, Segarra R,
Obrador E, Asensi M, Carretero J and Estrela JM: Acceleration of
glutathione efflux and inhibition of gamma-glutamyltranspeptidase
sensitize metastatic B16 melanoma cells to endothelium-induced
cytotoxicity. J Biol Chem. 280:6950–6959. 2005. View Article : Google Scholar : PubMed/NCBI
|