Introduction
Giant cell tumor (GCT) of the bone represents ~5% of
primary bone tumor types and 20% of benign bone tumor types
(1). The disease often occurs in
adults between the ages of 20- and 40-years-old, with a higher
incidence in females (2,3). GCTs are generally composed of
mononuclear histiocytic cells, multinucleated giant cells
resembling osteoclasts and neoplastic stromal cells that are the
predominant proliferating cell population (4,5). The
disease is generally recognized as a border or low-grade, with a
certain degree of invasive characteristics, demonstrated by
biological behavior (6,7). The predominant problem in the
management of GCT is local recurrence following surgical treatment:
27–65% following isolated curettage; 12–27% following curettage
with adjuvants such as high-speed burr, phenol, liquid nitrogen, or
polymethylmethacrylate; and 0–12% after en bloc resection
(6).
The distal radius and ulna is the fourth most common
location for GCT of the bone, after the distal femur, proximal
tibia and proximal femur, accounting for ~9% of cases (8,9).
Numerous previous studies have identified the distal radius and
ulna as being particularly prone to recurrence. To date, the ideal
treatment methods for GCTs of the distal ulna and radius remain
controversial (10–12). En bloc resection of GCT
provides lower rates of recurrences, which also sacrifices the
joint, results in a major reconstruction, and the functional
outcomes are questionable. Intralesional excision (curettage)
preserves the joint; however, has a reasonably high risk of local
recurrence even if used in combination with surgical adjuvants,
including liquid nitrogen, phenol or cement (8,10,13).
Therefore, the effect of different surgical modalities on tumor
recurrence and postoperative wrist function remains unclear. The
aim of the present study was to assess the clinical effects of
three surgical approaches for GCT of the distal radius and ulna,
including curettage plus inactivated tumor bed plus allogeneic bone
graft/bone cement augmentation, simple en bloc resection,
and en bloc resection and reconstruction with
non-vascularized fibular autograft/allogeneic bone graft
segment.
Materials and methods
Patients
The present study was approved by the Ethics
Committee of the Tumor Hospital of Yunnan Province and was
performed in accordance with the declaration of Helsinki. Informed
consent was obtained from all patients. The present study
retrospectively collected the clinical data of patients with a GCT
of the distal radius and ulna between January 2000 and December
2013. The inclusion criteria were patients who were diagnosed with
GCT by biopsy examination in The Third Affiliated Hospital of
Kunming Medical University, Tumor Hospital of Yunnan Province and
confirmed the location as the distal radius and ulna by X-ray and
computed tomography. The exclusion criteria were as follows: i)
Patients with a previous history of surgery; ii) patients receiving
surgical treatment other than the three surgical methods being
assessed; iii) patients who received non-surgical treatment.
Surgical points
Individual therapeutic regimens were selected
according to the Campanacci's grade (14) and the location of distal ulna and
radius (Table I). The key points
included: Following curettage, a Stryker drill (Stryker, Kalamazoo,
MI, USA) was used to grind lesions along each direction. Then, 95%
ethanol was used to inactivate the tumor bed. For en bloc
resection, the scope of the osteotomy was determined by the
preoperative imaging results. It is usually no less than 2 cm
distance to the focus, including soft tissue reaction zone or soft
tissue focus. The present study used autologous fibular graft or
allogeneic bone graft segment (contained distal articular surface)
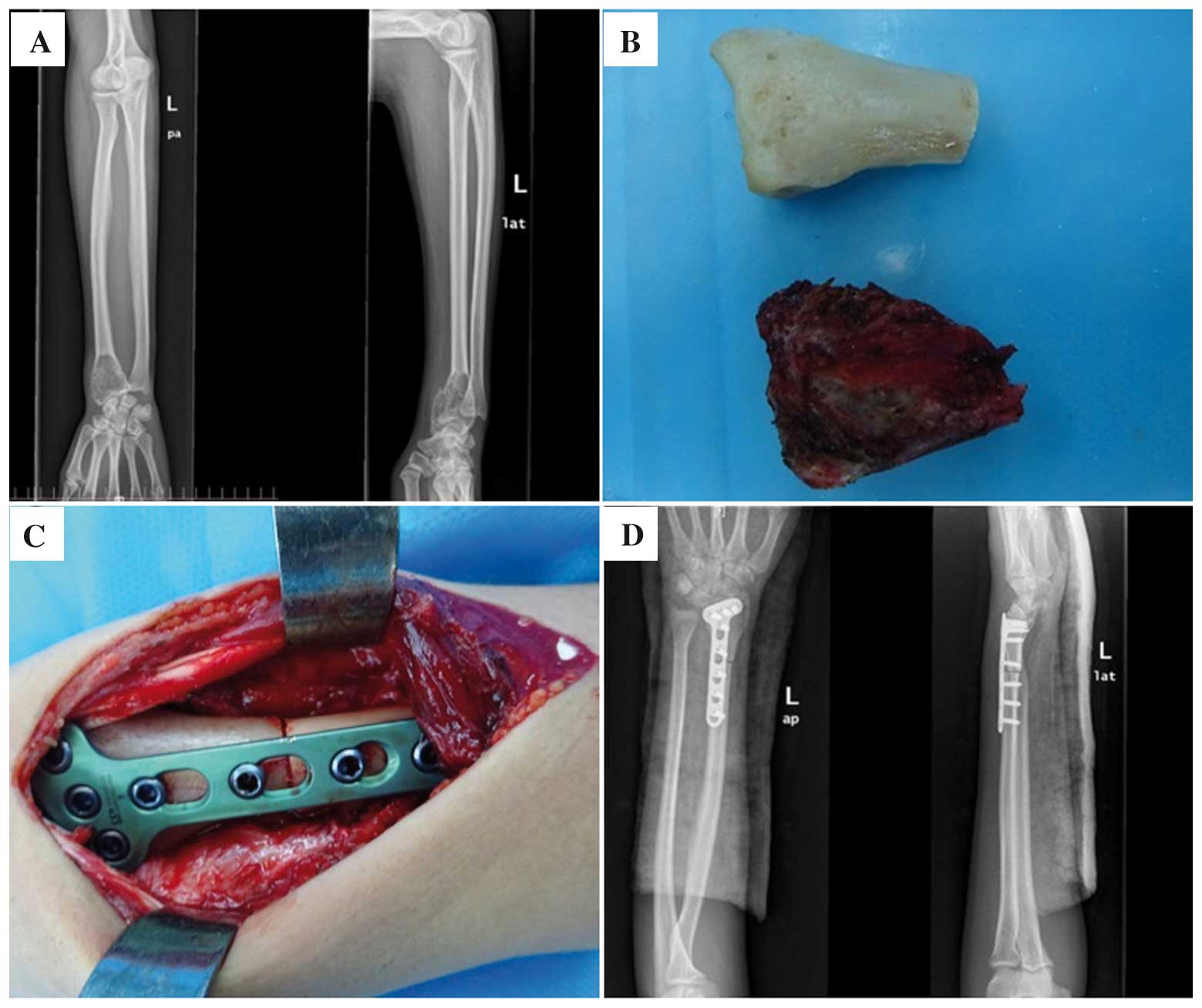
to reconstruct the radiocarpal joint (Fig. 1).
 | Table I.Baseline characteristics of 27
patients with a giant cell tumor on the distal radius and ulna. |
Table I.
Baseline characteristics of 27
patients with a giant cell tumor on the distal radius and ulna.
| Characteristic | No. patients |
|---|
| Mean age, years
(range) | 34.8
(21–72-years-old) |
| Gender
(male/female) | 10/17 |
| Location (distal
ulna/distal radius) | 7/20 |
| Campanacci's
Grade |
|
| Grade
I | 4 |
| Grade
II | 16 |
| Grade
III | 7 |
| MSTS scores
(range) | 20 (11–28) |
| Surgical
regimens |
|
| Group
A | 4 |
| Group
B | 5 |
| Group
C | 18 |
| Preoperative
soft-tissue invasion | 7 |
| Preoperative
pathological fracture | 5 |
| Tumor size |
|
| ≥3
cm | 22 |
| <3
cm | 5 |
| Follow-up time,
months (range) | 25 (9–125
months) |
Functional assessment
The Musculoskeletal Tumor Society Score (MTSS) was
used to assess limb function (15).
The system consisted of six items, including pain, overall
function, psychological level, gesture, sensitivity and muscle
strength. The functional result was assessed as excellent (30–24
scores), good (23–18 scores), fair (17–12 scores) or poor (<12
scores) using the grading scheme.
Statistical analysis
The mean follow-up time of the 27 patients was 25
months (range, 9–125 months). All data were analyzed using SPSS
19.0 software (IBM SPSS, Chicago, IL, USA). Continuous variables
were expressed in terms of means ± standard deviation and were
compared using a one-way analysis of variance. Categorical
variables were expressed in terms of percentage and frequency, and
were compared using the χ2 test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Preoperative patients'
characteristics
From January 2000 to December 2013, a total of 27
patients with GCT of the distal radius and ulna were included. The
patients consisted of 10 male and 17 female. The mean age was
34.8-years-old (range, 21–72-years-old). The tumor location was the
distal ulna in 10 cases and the distal radius in the remaining 17
cases. The GCT was graded radiologically according to Campanacci
et al (14). According to
Campanacci's grading system, 4 cases were in stage I, 16 cases in
stage II and 7 cases in stage III. The clinical data of the
patients are shown in Table II.
 | Table II.Individualized surgical methods
according to Campanacci's grade of giant cell tumor of the distal
ulna and radius. |
Table II.
Individualized surgical methods
according to Campanacci's grade of giant cell tumor of the distal
ulna and radius.
|
| Campanacci's
classification |
|---|
|
|
|
|---|
| Tumor location | Grade I | Grade II | Grade III |
|---|
| Distal ulna | Curettage,
inactivated tumor bed and allogeneic bone graft/bone cement
augmentation (Group A) | Simple en bloc
resection (Group B) | Simple en bloc
resection (Group B) |
| Distal radius | Curettage,
inactivated tumor bed and allogeneic bone graft/bone cement
augmentation (Group A) | En bloc
resection and autologous fibular graft/llogeneic bone graft segment
(Group C) | En bloc
resection and autologous fibular graft/llogeneic bone graft segment
(Group C) |
Postoperative recurrence
A total of 3 patients (11.1%) exhibited tumor
recurrence at 9, 11 and 15 months after surgery. The case with
Campanacci's grade I GCT of the distal radius exhibited tumor
recurrence 9 months after curettage plus inactivated tumor bed plus
bone cement augmentation. The case with Campanacci's grade I GCT of
distal ulna exhibited recurrance 11 months after curettage plus
inactivated tumor bed plus bone cement augmentation. The two
patients were treated with en bloc resection and
reconstruction with allogeneic bone graft segment after
pathological examination and developed no recurrence after the
aforementioned secondary surgery. The remaining case with
Campanacci's grade III GCT of distal radius exhibited tumor
recurrence 15 months after en bloc resection and
reconstruction with allogeneic bone graft segment. The patient was
further treated with en bloc resection and reconstruction
with autologous fibular graft. At 6 months postoperatively, the
patient developed pulmonary metastasis and succumbed to respiratory
failure after chemotherapy and supportive therapy for 6 months.
Overall, the incidence of the postoperative recurrence of the GCT
of the distal ulna and radius was 14.3 (1/7) and 10% (2/20),
respectively, with a statistical P-value of 0.762. The incidence of
the postoperative recurrence were 50% (2/4) in Group A, 0% (0/5) in
Group B and 5.6% (1/18) in Group C, with a statistical P-value of
0.069. However, statistical significance was noted when the
incidence of the postoperative recurrence of curettage (Group A)
was compared with that of en bloc resection (Groups B and C)
(50 vs. 4.3%; P=0.024).
Postoperative complications
Of the patients, 4/27 (14.8%) with GCT of the distal
radius developed postoperative complications, including 1 case of
postoperative infection, 2 cases of implant breakage and
postoperative fractures, and 1 case of nonunion (Table III). No statistically significant
difference was observed regarding the incidence of the
postoperative complications among the three surgical approaches for
the GCT on the distal ulna and radius (P>0.05). The patient who
developed postoperative infection healed following anti-infection
drug therapy. The remaining 3 patients underwent secondary
fibulo-scapholunate arthrodesis, and no postoperative infection or
nonunion was noted. None of the patients developed neurovascular
complications.
 | Table III.Postoperative outcomes in the three
groups. |
Table III.
Postoperative outcomes in the three
groups.
| Outcome | Group A (n=4) | Group B (n=5) | Group C (n=18) | P-value |
|---|
| Recurrence | 2
(50%) | 0 (0%) | 1 (5.6%) | 0.024a |
| Infection | 0 (0%) | 0 (0%) | 1 (5.6%) | 0.660 |
| Internal fixation
fracture | 0 (0%) | 0 (0%) | 2
(11.1%) | 0.427 |
| Nonunion | 0 (0%) | 0 (0%) | 1 (5.6%) | 0.660 |
| Functional
assessment |
|
|
Excellent | 2
(50%) | 2
(40%) | 3
(16.7%) | 0.397 |
|
Good | 0 (0%) | 2
(40%) | 10 (55.5%) |
|
|
Fair | 1
(25%) | 1
(20%) | 3
(16.7%) |
|
|
Poor | 1
(25%) | 0 (0%) | 2
(11.1%) |
|
Function outcomes
The mean follow-up time of the 27 patients was 25
months (range, 9–125 months). Functional MTSS results were
excellent in 7 cases (25.9%), good in 12 cases (44.5%), fair in 5
cases (18.5%) and poor in 3 cases (11.1%). The overall excellent
and good rate was 70.4% (Table
III). No statistically significant difference was observed
regarding the postoperative MTSS results among the three surgical
approaches for the GCT on the distal ulna and radius.
Discussion
Currently, no consensus has been reached regarding
the optimal treatment approach for GCTs that occur in the distal
radius. Although almost 100% local control can be achieved with
en bloc resection (16), limb
function is usually offset (17).
Intralesional excision with curettage is the standard method of
treatment; however, it is associated with the rates of local
recurrence ranging between 10 and 40% (18–21). As
a result, topical adjuvant agents, including hydrogen peroxide,
phenol and alcohol, have been used to decrease the recurrence rates
(9). Liu et al (10) reported that patients in the
intralesional excision group exhibited a higher recurrence rate,
particularly for Campanacci's III Grade GCT compared with the en
bloc resection group (10).
Pazionis et al (11) reported
that the odds of local recurrence were three times less in the
en bloc resection group (n=60) compared with the
intralesional excision group (n=81). Considering the high local
recurrence risk of curettage, the 23 patients with Campanacci's
grade II and III GCT of the distal radius and ulna were all treated
with en bloc resection, and only one patient (1/23; 4.3%)
relapsed. However, 6 months after secondary surgery, the patient
developed pulmonary metastasis, which may be associated with the
high invasiveness. Considering the limited lesions of Campanacci's
grade I GCT, the present study selected the curettage plus
inactivated tumor bed and allogeneic bone graft (1 case)/bone
cement augmentation (3 cases) for Campanacci's grade I GCT of the
distal radius and ulna, which can theoretically guarantee the
safety boundary. However, the incidence of the postoperative
recurrence of patients was 50% (2/4), which is higher compared with
that reported previously, which may be due to limited sample size.
It can also partially reflect that the application of bone cement
augmentation cannot reduce the risk of the recurrence of GCT
(9). A previous report suggested
that wrist joint can still reach 75% grasp strength and 80% range
of motion following distal ulnar resection (22). Therefore, in the present study, en
bloc resection without reconstruction for Campanacci's grade II
and III GCT of the distal ulna was selected. Following surgery, no
statistically significant difference was revealed regarding the
incidence of the postoperative recurrence of the GCT in distal ulna
and radius (14.3 vs. 10%). Although no statistically significant
difference was found in the present study regarding the incidence
of the postoperative recurrence among the three surgical approaches
for the GCT on distal ulna and radius, a >10-fold higher
difference was revealed regarding the incidence of the
postoperative recurrence of curettage when compared with that of
en bloc resection. Further studies with a larger number of
samples are warranted.
Various surgical approaches for GCT of the distal
radius and ulna can produce different rates of postoperative
complications. Previous reports suggested that en bloc
resection was associated with a relatively high rate of major
complications (range, 29–100%) (23–27).
These complications included nonunion at the graft-radius junction
(12–38%) (26–28), fracture of graft (13–29%) (26,27),
subluxation (12–67%) (23,26), arthritis (13–50%) (23,28) and
postsurgical pneumonia (24).
Notably, in the present study, 1 case (5.6%) experienced
postoperative infection, which may be associated with rich blood
supply and rapid tissue healing. Additionally, 2 cases of internal
fixation fracture (11.2%) and 1 case of nonunion (5.6%) occurred.
These patients received reconstruction with allogeneic bone graft.
This may be associated with the slow creeping substitution of
allografts and premature functional exercise. These 3 patients
underwent with fibulo-scapholunate arthrodesis and thereafter no
postoperative infection or nonunion was noted. Overall, the
postoperative complications observed in the present study were
lower compared with that in the aforementioned reports.
Patients with GCT of the distal radius and ulna can
have long-term survival, unless the incidence of pulmonary
metastasis occurs; therefore, functional recovery of the wrist is
extremely important. In the present study, patients undergoing
allogeneic bone graft were all treated with individual customized
allografts with the preservation of the articular aspect of the
distal radius. The overall excellent and good rate of en
bloc resection and reconstruction was 70.4%, which is not
statistically different compared with that of curettage. The
present study suggested that en bloc resection and
reconstruction can be used as the standard initial treatment method
for Campanacci's grade II and III GCT. Wysocki et al
(12) suggested that curettage can
be considered for the initial treatment for Campanacci's grade II
and III GCT of the distal radius, since en bloc resection
can be performed if tumor recurrence occurred. However, secondary
surgery not only increases the expense of the patients, it also
increases the risk of postoperative complications. Therefore, the
present study suggested that en bloc resection can be used
as the standard initial treatment method for Campanacci's grade II
and III GCT, whereas curettage can be used for Campanacci's I Grade
GCT.
In conclusion, in order to achieve the best clinical
effects for patients with GCT on distal radius and ulna,
individualized treatment regimens must be designed according to the
different Campanacci's grades and tumor locations.
Acknowledgements
The present study was supported in part by the
National Natural Science Foundation of China (grant no. 81302343),
the Joint Special Funds for the Department of Science and
Technology of Yunnan Province-Kunming Medical University (grant no.
2014FB067), and the Doctor Funds Project of Tumor Hospital of
Yunnan province (grant no. BSJJ201501).
References
|
1
|
Vanni D, Pantalone A, Andreoli E, Caldora
P and Salini V: Giant cell tumor of the distal ulna: A case report.
J Med Case Rep. 6:1432012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Raskin KA, Schwab JH, Mankin HJ,
Springfield DS and Hornicek FJ: Giant cell tumor of bone. J Am Acad
Orthop Surg. 21:118–126. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Padwa BL: Giant cell tumorPediatric Head
and Neck Tumors. Rahbar R, Rodriguez-Galindo C, Meara JG, Smith ER
and Perez-Atayde AR: Springer-Verlag; New York, NY: pp. 165–170.
2014, View Article : Google Scholar
|
|
4
|
Werner M: Giant cell tumour of bone:
Morphological, biological and histogenetical aspects. Int Orthop.
30:484–489. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Klenke FM, Wenger DE, Inwards CY, Rose PS
and Sim FH: Giant cell tumor of bone: Risk factors for recurrence.
Clin Orthop Relat Res. 469:591–599. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chakarun CJ, Forrester DM, Gottsegen CJ,
Patel DB, White EA and Matcuk GR Jr: Giant cell tumor of bone:
Review, mimics, and new developments in treatment. Radiographics.
33:197–211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Balke M, Schremper L, Gebert C, Ahrens H,
Streitbuerger A, Koehler G, Hardes J and Gosheger G: Giant cell
tumor of bone: Treatment and outcome of 214 cases. J Cancer Res
Clin Oncol. 134:969–978. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Errani C, Ruggieri P, Asenzio MA, Toscano
A, Colangeli S, Rimondi E, Rossi G, Longhi A and Mercuri M: Giant
cell tumor of the extremity: A review of 349 cases from a single
institution. Cancer Treat Rev. 36:1–7. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Niu X, Zhang Q, Hao L, Ding Y, Li Y, Xu H
and Liu W: Giant cell tumor of the extremity: retrospective
analysis of 621 Chinese patients from one institution. J Bone Joint
Surg Am. 94:461–467. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Liu YP, Li KH and Sun BH: Which treatment
is the best for giant cell tumors of the distal radius? A
meta-analysis. Clin Orthop Relat Res. 470:2886–2894. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pazionis TJ, Alradwan H, Deheshi BM,
Turcotte R, Farrokhyar F and Ghert M: A Systematic review and
meta-analysis of En-Bloc vs intralesional resection for giant cell
tumor of bone of the distal radius. Open Orthop J. 7:103–108. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wysocki RW, Soni E, Virkus WW, Scarborough
MT, Leurgans SE and Gitelis S: Is intralesional treatment of giant
cell tumor of the distal radius comparable to resection with
respect to local control and functional outcome? Clin Orthop Relat
Res. 473:706–715. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Prosser GH, Baloch KG, Tillman RM, Carter
SR and Grimer RJ: Does curettage without adjuvant therapy provide
low recurrence rates in giant-cell tumors of bone? Clin Orthop
Relat Res. 211–218. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Campanacci M: Bone and Soft Tissue Tumors:
Clinical Features, Imaging, Pathology and Treatment.
Springer-Verlag; Vienna, Austria: 1999, View Article : Google Scholar
|
|
15
|
Enneking WF, Dunham W, Gebhardt MC,
Malawar M and Pritchard DJ: A system for the functional evaluation
of reconstructive procedures after surgical treatment of tumors of
the musculoskeletal system. Clin Orthop Relat Res. 241–246.
1993.PubMed/NCBI
|
|
16
|
Su YP, Chen WM and Chen TH: Giant-cell
tumors of bone: An analysis of 87 cases. Int Orthop. 28:239–243.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gitelis S, Mallin BA, Piasecki P and
Turner F: Intralesional excision compared with en bloc resection
for giant-cell tumors of bone. J Bone Joint Surg Am. 75:1648–1655.
1993.PubMed/NCBI
|
|
18
|
Blackley HR, Wunder JS, Davis AM, White
LM, Kandel R and Bell RS: Treatment of giant-cell tumors of long
bones with curettage and bone-grafting. J Bone Joint Surg Am.
81:811–820. 1999.PubMed/NCBI
|
|
19
|
Lausten GS, Jensen PK, Schiødt T and Lund
B: Local recurrences in giant cell tumour of bone. Local-term
follow up of 31 cases. Int Orthop. 20:172–176. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Malek F, Krueger P, Hatmi ZN, Malayeri AA,
Faezipour H and O'Donnell RJ: Local control of long bone giant cell
tumour using curettage, burring and bone grafting without adjuvant
therapy. Int Orthop. 30:495–498. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kivioja AH, Blomqvist C, Hietaniemi K,
Trovik C, Walloe A, Bauer HC, Jorgensen PH, Bergh P and Follerås G:
Cement is recommended in intralesional surgery of giant cell
tumors: A Scandinavian Sarcoma Group study of 294 patients followed
for a median time of 5 years. Acta Orthop. 79:86–93. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wolfe SW, Mih AD, Hotchkiss RN, Culp RW,
Kiefhaber TR and Nagle DJ: Wide excision of the distal ulna: A
multicenter case study. J Hand Surg Am. 23:222–228. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cheng CY, Shih HN, Hsu KY and Hsu RW:
Treatment of giant cell tumor of the distal radius. Clin Orthop
Relat Res. 221–228. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kang L, Manoso MW, Boland PJ, Healey JH
and Athanasian EA: Features of grade 3 giant cell tumors of the
distal radius associated with successful intralesional treatment. J
Hand Surg Am. 35:1850–1857. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Panchwagh Y, Puri A, Agarwal M, Anchan C
and Shah M: Giant cell tumor-distal end radius: Do we know the
answer? Indian J Orthop. 41:139–145. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Griend RA Vander and Funderburk CH: The
treatment of giant-cell tumors of the distal part of the radius. J
Bone Joint Surg Am. 75:899–908. 1993.PubMed/NCBI
|
|
27
|
Sheth DS, Healey JH, Sobel M, Lane JM and
Marcove RC: Giant cell tumor of the distal radius. J Hand Surg Am.
20:432–440. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Harness NG and Mankin HJ: Giant-cell tumor
of the distal forearm. J Hand Surg Am. 29:188–193. 2004. View Article : Google Scholar : PubMed/NCBI
|