Introduction
Surgical liver resection is the most effective
treatment for colorectal liver metastases (CRLM) and is currently
the only potentially curative therapeutic option (1,2).
Previously, preoperative chemotherapy was demonstrated to improve
prognosis and increase conversion to resectability in patients with
CRLM (3–5). However, preoperative chemotherapy is
not always effective and the disease may progress (6). Therefore, it may be beneficial to
personalize treatment based on the individual molecular
characteristics of the tumor. Identification of predictive markers
for the response to preoperative chemotherapy may help to ensure
prompt selection of effective drugs for each patient and to avoid
unnecessary administration of ineffective or even harmful drugs.
Furthermore, the reduction in treatment costs would have economic
benefits.
There are currently no molecular markers of
chemosensitivity to predict the response of CRLM to 5-fluorouracil
(5-FU)- and oxaliplatin-based treatment regimens, such as FOLFOX
(5-FU, folinic acid and oxaliplatin) and XELOX (capecitabine and
oxaliplatin). Thymidylate synthase (TS) and excision repair
cross-complementation group 1 (ERCC1) have been shown to be useful
predictors of the response to 5-FU- and oxaliplatin-based
chemotherapy in colorectal cancer (CRC) (7–12).
However, little is known on the direct association between TS and
ERCC1 expression as detected by immunohistochemistry (IHC) of tumor
tissues and the response to 5-FU- and oxaliplatin-based
preoperative chemotherapy for CRLM. Furthermore, it is not known
whether TS and ERCC1 expression levels in the primary lesions and
CRLM are associated.
The aim of the present study was to evaluate TS and
ERCC1 expression in primary lesions and CRLM as predictive markers
for the response to preoperative chemotherapy according to both
histological [tumor regression grade (TRG)] and radiological
[Response Evaluation Criteria in Solid Tumors (RECIST)]
assessments. Identification of predictive markers for response to
chemotherapy may help identify the CRLM patients who would most
benefit from preoperative chemotherapy.
Patients and methods
Patients
The present study included 24 consecutive patients
with CRLM who were treated with 5-FU- and oxaliplatin-based
preoperative chemotherapy between January 2007 and February 2016.
Selection of the chemotherapy regimen was not randomized, but
rather determined by the clinician's preference. Medical records
were reviewed and clinical data were retrospectively obtained. This
study was conducted in compliance with the Declaration of Helsinki
and in accordance with guidelines approved by the Institutional
Research Board of Kindai University Nara Hospital (no. 364).
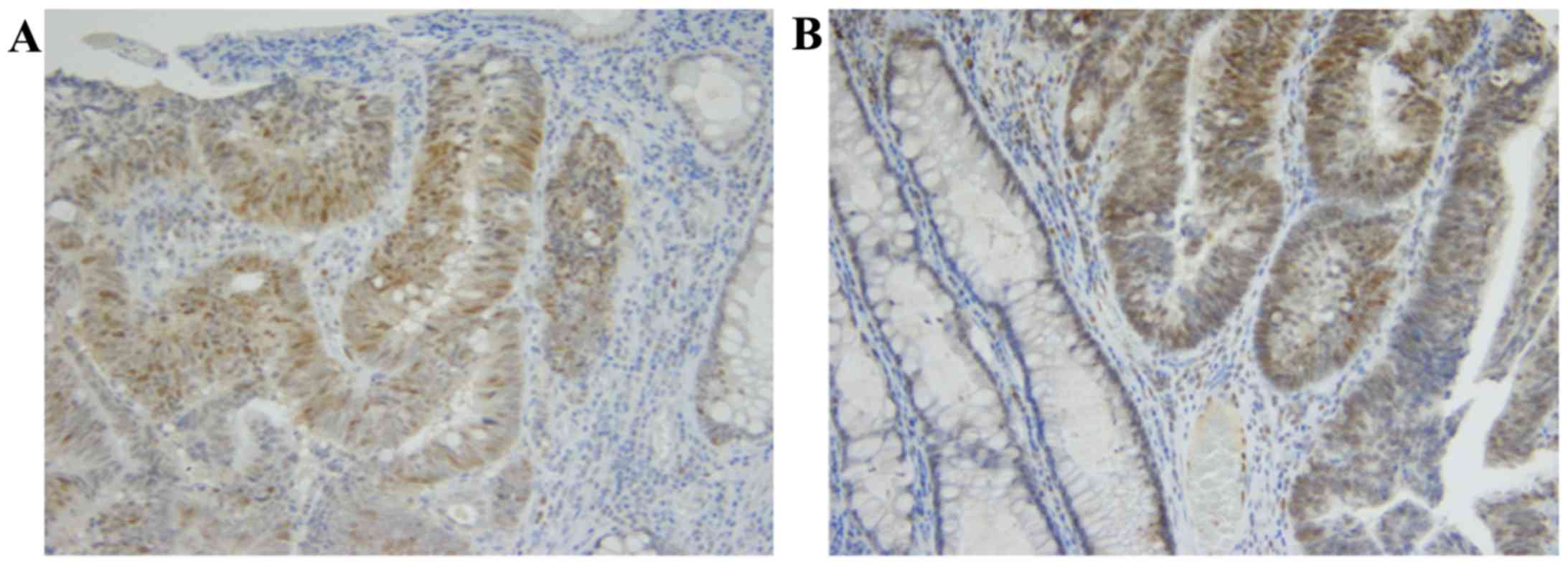
Immunohistochemistry
A total of 23 paired samples of formalin-fixed,
paraffin-embedded sections from primary tumors and CRLM and 1
unpaired CRLM section were deparaffinized with xylene, rehydrated
with a graded series of aqueous ethanol solutions, and then stained
as briefly described herein. For antigen retrieval, the sections
were placed in citrate buffer (pH 6.0) and autoclaved at 121°C for
10 min. Endogenous peroxidase activity was blocked by incubation of
sections with a 3% hydrogen peroxide solution at room temperature
for 15 min, followed by rinsing with 0.05 M phosphate-buffered
saline (PBS) and blocking with Blocking One solution (Nacalai
Tesque, Kyoto, Japan) at room temperature for 10 min. The sections
were then incubated with rabbit anti-TS monoclonal antibody (1:500,
clone TS106, Dako, Tokyo, Japan) or mouse anti-ERCC1 monoclonal
antibody (1:250, clone 8F1, Abcam, Cambridge, UK) overnight at 4°C.
Following washing with PBS, the sections were incubated with
universal immuno-peroxidase polymer (N-Histofine Simple Stain MAX,
Nichirei Co., Tokyo, Japan) at room temperature for 30 min. After
washing again with PBS, peroxidase activity was detected by
incubation with 3,3′-diaminobenzidine tetrahydrochloride (DAB;
Merck KGaA, Darmstadt, Germany) at room temperature for 5 min. The
sections were washed again with PBS, and cell nuclei were stained
with Mayer's hematoxylin at room temperature for 1 min. IHC
qualitative scoring was performed using the ASCO/CAP criteria
(13), i.e., 10% of cells with
nuclear staining was considered as a positive staining reaction for
TS and ERCC1 (Fig. 1). The slides
were examined independently by two pathologists blinded to the
clinical data.
Imaging assessment
RECIST 1.1-based evaluation of the effect of
preoperative chemotherapy was assessed by experienced
gastroenterological surgeons using computed tomography or magnetic
resonance imaging (14,15). The criteria of the Japanese Society
for Cancer of the Colon and Rectum (JSCCR) were used for grading
liver metastasis. This JSCCR staging system is based on the number
of liver metastases as follows: H1, ≤4 metastatic tumors and the
largest hepatic tumor sized ≤5 cm; H2, except H1 and H3; H3, ≥5
metastatic tumors and the largest hepatic tumor sized >5 cm
(16).
Histological assessment
Two pathologists blinded to the patient's clinical
information reviewed all histological specimens. Tumor and node
staging for all resected specimens was conducted according to the
7th American Joint Committee on Cancer TNM staging manual (17). The TRG method was used to
characterize the tumor response (18) based on tumor viability and the extent
of fibrosis and inflammation, and TRG classes were defined as
follows: TRG 1, complete regression with no residual tumor; TRG 2,
presence of rare residual cancer cells; TRG 3, presence of larger
numbers of residual cancer cells with predominant fibrosis; TRG 4,
residual cancer outgrowing the fibrosis; and TRG 5, absence of
regressive changes.
Statistical analysis
Statistical analysis was performed using JMP
Pro® software, version 11 (SAS Institute, Cary, NC,
USA). Continuous data are reported as median and range unless
otherwise specified. Categorical data are presented as frequency
and percentage. Comparison of continuous variables was performed
using the Wilcoxon's rank-sum test. The Fisher's exact test was
used for comparison of categorical variables as appropriate.
Statistical significance was defined as P<0.05.
Results
Patient characteristics
The patient characteristics are summarized in
Table I. A total of 24 patients (8
women and 16 men) aged 39–78 years (median, 64 years) were analyzed
in this study. A primary lesion specimen was missing for 1 patient
who underwent surgery at another hospital. A total of 9 patients
had rectal cancer and 15 patients had colon cancer. The
chemotherapy regimens included modified FOLFOX6 (21 cases) and
XELOX (3 cases). The median number of chemotherapy cycles was 6
(range, 3–56). Molecular-targeted drugs were administered to 20
patients: 8 patients received panitumumab, 1 received cetuximab,
and 11 received bevacizumab. As regards the response to
preoperative chemotherapy evaluated according to TRG, 2 patients
were classified as TRG1, 13 as TRG2, 4 as TRG3, 4 as TRG4 and 1 as
TRG5. As regards the response evaluated according to RECIST, 2
patients had progressive disease (PD), 5 had stable disease (SD),
and 17 exhibited a partial response (PR). No patients achieved
complete response (CR). Other clinical and histological data are
provided in Table I.
 | Table I.Patient characteristics (n=24). |
Table I.
Patient characteristics (n=24).
| Characteristics | No. |
|---|
| Age, years (median,
range) | 64 (39–78) |
| Sex, male/female | 16/8 |
| Tumor classification
of the primary lesion |
|
|
T2/T3/T4 | 1/14/9 |
| Node
classification |
|
|
N0/N1/N2/N3 | 7/8/6/3 |
| Differentiation |
|
|
Tub1/Tub2/muc | 7/16/1 |
| Location |
|
|
Colon/rectum | 15/9 |
| Number of
metastases |
|
|
Multiple/solitary | 19/5 |
| Grade of liver
metastases |
|
|
H1/H2/H3 | 8/11/5 |
| Size of largest
metastasis prior to | 51.4
(7.8–130.9) |
| chemotherapy, mm
(median, range) |
|
| Size of largest
metastasis after | 34.2 (9–91.8) |
| chemotherapy, mm
(median, range) |
|
| No. of chemotherapy
cycles (median, range) | 6 (3–56) |
| Chemotherapy
regimen |
|
|
FOLFOX/XELOX | 21/3 |
| Molecular targeted
drug |
|
|
P-mab/C-mab/Bev | 8/1/11 |
| Response Evaluation
Criteria in Solid |
|
| Tumors
(RECIST) |
|
|
CR/PR/SD/PD | 0/17/5/2 |
| Tumor Regression
Grade (TRG) |
|
|
1/2/3/4/5 | 2/13/4/4/1 |
| ERCC1 expression in
primary lesion |
|
|
Negative/positive | 9/14 |
| ERCC1 expression in
liver metastasis |
|
|
Negative/positive | 15/9 |
| TS expression in
primary lesion |
|
|
Negative/positive | 12/11 |
| TS expression in
liver metastasis |
|
|
Negative/positive | 18/6 |
Correlation between TRG and RECIST
assessments
We analyzed the association between the response
assessed by TRG and RECIST. Patients classified as TRG1-3 were
considered to be responders, while those classified as TRG4-5 were
considered to be non-responders (18–21).
Based on this classification, 19 patients were assigned to the
responder group (TRG 1–3) and 5 to the non-responder group (TRG
4–5). Similarly, patients were assigned to two groups based on
RECIST criteria: responders (PR, n=17) and non-responders (SD and
PD, n=7) (22). The analysis
identified a significant association between the response of CRLM
patients to preoperative chemotherapy assessed by TRG and RECIST
(P=0.0005; Table II).
 | Table II.Correlation between response based on
TRG and RECIST. |
Table II.
Correlation between response based on
TRG and RECIST.
|
| Response according
to RECIST |
|
|---|
|
|
|
|
|---|
| TRG class | PR (n=17) | SD + PD (n=7) | P-value |
|---|
| TRG1-3 (n=19) | 17 | 2 | 0.0005 |
| TRG4-5 (n=5) | 0 | 5 |
|
Response to preoperative chemotherapy
based on RECIST
The clinicopathological data for patients in the
RECIST responder (PR) and non-responder (SD + PD) groups are
summarized in Table III. The
response based on RECIST was significantly associated with TS
expression in the primary tumor and with the size of metastases
prior to chemotherapy (P=0.0272 and P=0.0454, respectively). Other
factors were not found to be significantly associated with
RESICT.
 | Table III.Response to preoperative chemotherapy
based on RECIST. |
Table III.
Response to preoperative chemotherapy
based on RECIST.
| Variables | PR (n=17) | SD + PD (n=7) | P-value |
|---|
| Age, years (median,
range) | 63 (39–78) | 71 (41–75) | 0.2151 |
| Sex |
|
|
|
|
Male | 13 | 3 | 0.1670 |
|
Female | 4 | 4 |
| Tumor
classification of the primary lesion |
|
|
|
| T1,
T2 | 1 | 0 | 1.000 |
| T3,
T4 | 16 | 7 |
|
| Node
classification |
|
|
|
| N0 | 4 | 3 | 0.3742 |
| N1,
N2 | 13 | 4 |
|
| Location |
|
|
|
|
Colon | 11 | 4 | 1.000 |
|
Rectum | 6 | 3 |
|
| Number of
metastases |
|
|
|
|
Solitary | 2 | 3 | 0.1265 |
|
Multiple | 15 | 4 |
|
| Size of metastases
prior to chemotherapy, mm (median, range) | 63.2
(17.2–130.9) | 33.6
(7.8–87.8) | 0.0454 |
| Molecular targeted
drug |
|
|
|
| P-mab,
C-mab | 8 | 1 | 0.0847 |
|
Bev | 8 | 3 |
|
|
None | 1 | 3 |
|
| TS expression in
primary lesion |
|
|
|
|
Negative | 11 | 1 | 0.0272 |
|
Positive | 5 | 6 |
| TS expression in
liver metastasis |
|
|
|
|
Negative | 13 | 5 | 1.000 |
|
Positive | 4 | 2 |
|
| ERCC1 expression in
primary lesion |
|
|
|
|
Negative | 6 | 3 | 1.000 |
|
Positive | 10 | 4 |
|
| ERCC1 expression in
liver metastasis |
|
|
|
|
Negative | 11 | 4 | 1.000 |
|
Positive | 6 | 3 |
|
Response to preoperative chemotherapy
based on TRG
The clinicopathological data for patients in the TRG
responder (TRG-3) and non-responder (TRG4-5) groups are summarized
in Table IV. The response based on
TRG was significantly associated with TS expression in the primary
tumor (P=0.0137). Other factors were not found to be significantly
associated with TRG class.
 | Table IV.Response to preoperative chemotherapy
based on TRG. |
Table IV.
Response to preoperative chemotherapy
based on TRG.
| Variables | TRG1-3 (n=19) | TRG4-5 (n=5) | P-value |
|---|
| Age, years (median,
range) | 63 (39–78) | 71 (42–74) | 0.4339 |
| Sex |
|
|
|
|
Male | 14 | 2 | 0.2885 |
|
Female | 5 | 3 |
|
| Tumor
classification of the primary lesion |
|
|
|
| T1,
T2 | 1 | 0 | 1.000 |
| T3,
T4 | 18 | 5 |
|
| Node
classification |
|
|
|
| N0 | 5 | 2 | 0.6080 |
| N1,
N2 | 14 | 3 |
|
| Location |
|
|
|
|
Colon | 11 | 4 | 0.6146 |
|
Rectum | 8 | 1 |
|
| Number of
metastases |
|
|
|
|
Solitary | 4 | 1 | 1.000 |
|
Multiple | 15 | 4 |
|
| Size of metastases
before chemotherapy, mm (median, range) | 56.2
(17.2–30.9) | 18.4
(7.8–87.8) | 0.0699 |
| Molecular targeted
drug |
|
|
|
| P-mab,
C-mab | 8 | 1 | 0.3385 |
|
Bev | 9 | 2 |
|
|
None | 2 | 2 |
|
| TS expression in
primary lesion |
|
|
|
|
Negative | 12 | 0 | 0.0137 |
|
Positive | 6 | 5 |
|
| TS expression in
liver metastasis |
|
|
|
|
Negative | 12 | 3 | 1.000 |
|
Positive | 7 | 2 |
|
| ERCC1 expression in
primary lesion |
|
|
|
|
Negative | 8 | 1 | 0.6106 |
|
Positive | 10 | 4 |
|
| ERCC1 expression in
liver metastasis |
|
|
|
|
Negative | 14 | 4 | 1.000 |
|
Positive | 5 | 1 |
|
Correlation between TS and ERCC1
expression in the primary lesion and CRCLM
As shown in Table V,
no correlation was detected between TS expression in the primary
lesion and that in the matched liver metastases (P=0.371). There
was also no correlation detected between ERCC1 expression in the
primary lesion and that in the matched liver metastasis
(P=1.00).
 | Table V.Correlation between TS and ERCC1
expression in matched pairs of primary lesions and CRLM. |
Table V.
Correlation between TS and ERCC1
expression in matched pairs of primary lesions and CRLM.
|
| TS expression in
CRLM |
|
|---|
|
|
|
|
|---|
|
| Negative | Positive | P-value |
|---|
| TS expression in
primary lesion |
|
| 0.371 |
|
Negative | 10 | 2 |
|
|
Positive | 7 | 4 |
|
|
|
|
|
|
| ERCC1 expression in
CRLM |
|
|
|
|
|
| Negative | Positive | P-value |
|
|
|
|
| ERCC1 expression in
primary lesion |
|
| 1.00 |
|
Negative | 6 | 3 |
|
|
Positive | 8 | 6 |
|
Discussion
The main methods used to assess the response of CRLM
to chemotherapy include radiological and pathological grading
systems (19,23). In radiological assessment, the effect
of chemotherapy is usually evaluated on radiographic scans
according to the RECIST scoring system. Recently, Rubbia et
al published a novel grading system, TRG, which assesses
prognosis based on the pathological response to chemotherapy
(18). In the present study, we
evaluated the expression of TS and ERCC1 in the primary colorectal
lesion and CRLM to determine their potential as predictive markers
of the response of CRLM to preoperative chemotherapy as assessed by
both the TRG and RECIST methods.
The correlation between the TRG and RECIST results
were first evaluated for the 24-patient cohort in the present study
and observed a significant association between the two assessment
tools. A previous study demonstrated that RECIST was significantly
associated with the percentage of residual tumor cells in patients
treated with preoperative chemotherapy for CRLM (24). In that study, the authors scored the
pathological response semi-quantitatively (percentage of residual
tumor cells relative to the total tumor surface area) and, although
our study used a slightly different method of pathological
assessment, our results are consistent with the findings of Chun
et al, confirming that radiological assessment based on
RECIST was significantly associated with the pathological
assessment (24).
Fluoropyrimidines, particularly 5-FU, have been the
mainstay of systemic treatment of metastatic CRC for >50 years.
The major mechanism of action of 5-FU is inhibition of TS, which
catalyzes a crucial rate-limiting step in DNA synthesis (25).
Several studies on metastatic CRC have demonstrated
that high intratumoral TS levels are correlated with resistance to
fluoropyrimidine treatment (26–28).
Other studies have demonstrated that TS is a prognostic marker for
patients with CRC (29) and
metastatic CRC (30). Similar to the
present study, Arienti et al demonstrated that TS expression
is a marker of chemosensitivity of peritoneal carcinomatosis from
colon cancer to 5-FU- and oxaliplatin-based chemotherapy (31). However, despite these promising
results, TS has not been recommended for routine clinical practice
as a predictor of response to 5-FU-based chemotherapy (32). Thus, the aim of the present study was
to determine whether TS expression is a direct marker of the CRLM
response to preoperative chemotherapy.
In this study, TS expression in the primary lesion,
but not in CRLM, was identified as a predictive marker for the
response to preoperative chemotherapy, as assessed by both TRG and
RECIST. No significant difference in TS expression was found
between the primary lesion and CRLM. Therefore, it appears that
other molecular characteristics of the primary tumor must have been
altered during the metastatic process (33). Chemotherapy may also have modified
the tumor characteristics (34). We
hypothesized that such factors may explain why TS expression in
liver metastases was not a predictive marker of response.
ERCC1 expression was not found to be a predictive
marker of response to preoperative chemotherapy. It was previously
suggested that ERCC1 is a good predictive chemosensitivity marker
for oxaliplatin-based chemotherapy (11); however, other studies have
demonstrated that TS expression is a better predictive
chemosensitivity marker compared with ERCC1 for 5-FU- and
oxaliplatin-based chemotherapy (28,31,35,36). In
agreement with the latter reports, we found that TS expression is a
more useful predictor of chemosensitivity to 5-FU- and
oxaliplatin-based chemotherapy compared with ERCC1 expression.
Although ERCC1 was a good predictive marker for oxaliplatin-based
chemotherapy, previous reports included several factors, such as
inclusion criteria, outcome and stage, and it remains controversial
whether it is also a direct good predictive marker for response to
5-FU- and oxaliplatin-based chemotherapy.
There were certain limitations to the present study.
First, this was a small, retrospective, non-randomized study, and
the results may have been affected by its retrospective design. The
inclusion or exclusion criteria for preoperative chemotherapy were
not strictly defined. We included only patients who proceeded to
receive surgery, whereas patients with CRLM who failed to convert
to resectability were excluded. Thus, the patients with the lowest
responses may have been excluded from this study.
Ideally, these problems could be overcome by
performing liver biopsies before and after chemotherapy. However,
liver biopsy is not practically recommended due to the risk of
tumor spillage, which may be the cause of peritoneal carcinomatosis
(37). For this reason, only
specimens resected by surgery were evaluated. Second, we did not
analyze prognosis in terms of disease-free survival and overall
survival, mainly because prognosis was significantly affected by
the postoperative treatment. Therefore, we considered that the
chemotherapy response based on pathological and radiological
assessments would allow for direct analysis of the association
between protein expression and the tumor response to therapy.
In summary, the results of the present study
demonstrated a significant association between TS expression in the
primary colorectal tumor and response to preoperative chemotherapy
as assessed by both TRG and RECIST. Although investigations of
larger patient cohorts are required to confirm our results, the
data of the present study suggest that TS expression in the primary
lesion may be a predictive marker for the response of CRLM to 5-FU-
and oxaliplatin-based preoperative chemotherapy.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HT designed the study and analyzed the data. HT, KK,
KI, MT, MY and MI performed the surgery. TW, TO, and YO performed
the histological experiments. HT, MY, and MI wrote the
manuscript.
Ethics approval and consent to
participate
Appropriate ethical approval was obtained from the
Institutional Review Board of Kindai University Nara Hospital
(Nara, Japan; no. 364). Patient consent was not required for the
present study, as it was conducted retrospectively.
Consent for publication
Not applicable.
Competing interests
The authors confirm that they have no competing
interests.
References
|
1
|
Rees M, Tekkis PP, Welsh FK, O'Rourke T
and John TG: Evaluation of long-term survival after hepatic
resection for metastatic colorectal cancer: A multifactorial model
of 929 patients. Ann Surg. 247:125–135. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
van der Pool AE, de Wilt JH, Lalmahomed
ZS, Eggermont AM, Ijzermans JN and Verhoef C: Optimizing the
outcome of surgery in patients with rectal cancer and synchronous
liver metastases. Br J Surg. 97:383–390. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Goéré D, Deshaies I, de Baere T, Boige V,
Malka D, Dumont F, Dromain C, Ducreux M and Elias D: Prolonged
survival of initially unresectable hepatic colorectal cancer
patients treated with hepatic arterial infusion of oxaliplatin
followed by radical surgery of metastases. Ann Surg. 251:686–691.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Giacchetti S, Itzhaki M, Gruia G, Adam R,
Zidani R, Kunstlinger F, Brienza S, Alafaci E, Bertheault-Cvitkvoic
F, Jasmin C, et al: Long-term survival of patients with
unresectable colorectal cancer liver metastases following
infusional chemotherapy with 5-fluorouracil, leucovorin,
oxaliplatin and surgery. Ann Oncol. 10:663–669. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tanaka K, Adam R, Shimada H, Azoulay D,
Lévi F and Bismuth H: Role of neoadjuvant chemotherapy in the
treatment of multiple colorectal metastases to the liver. Br J
Surg. 90:963–969. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Adam R, Pascal G, Castaing D, Azoulay D,
Delvart V, Paule B, Levi F and Bismuth H: Tumor progression while
on chemotherapy: A contraindication to liver resection for multiple
colorectal metastases? Ann Surg. 240:1052–1064. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Johnston PG, Lenz HJ, Leichman CG,
Danenberg KD, Allegra CJ, Danenberg PV and Leichman L: Thymidylate
synthase gene and protein expression correlate and are associated
with response to 5-fluorouracil in human colorectal and gastric
tumors. Cancer Res. 55:1407–1412. 1995.PubMed/NCBI
|
|
8
|
Li S, Zhu L, Yao L, Xia L and Pan L:
Association between ERCC1 and TS mRNA levels and disease free
survival in colorectal cancer patients receiving oxaliplatin and
fluorouracil (5-FU) adjuvant chemotherapy. BMC Gastroenterol.
14:1542014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Choueiri MB, Shen JP, Gross AM, Huang JK,
Ideker T and Fanta P: ERCC1 and TS expression as prognostic and
predictive biomarkers in metastatic colon cancer. PLoS One.
10:e01268982015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Noda E, Maeda K, Inoue T, Fukunaga S,
Nagahara H, Shibutani M, Amano R, Nakata B, Tanaka H, Muguruma K,
et al: Predictive value of expression of ERCC 1 and GST-p for
5-fluorouracil/oxaliplatin chemotherapy in advanced colorectal
cancer. Hepatogastroenterology. 59:130–133. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Geva R, Shamai S, Brazowsky E, Paoulas M,
Ben-Haim M, Johnstone E, Alex B and Shacham-Shmueli E: The
predictive role of ERCC1 status in oxaliplatin based neoadjuvant
therapy for metastatic colorectal cancer (mCRC) to the liver.
Cancer Invest. 33:89–97. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Han JJ, Baek SK, Lee JJ, Kim GY, Kim SY
and Lee SH: Combination of TRAP1 and ERCC1 expression predicts
clinical outcomes in metastatic colorectal cancer treated with
Oxaliplatin/5-fluorouracil. Cancer Res Treat. 46:55–64. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wolff AC, Hammond ME, Hicks DG, Dowsett M,
McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M,
Fitzgibbons P, et al: Recommendations for human epidermal growth
factor receptor 2 testing in breast cancer: American society of
clinical oncology/college of american pathologists clinical
practice guideline update. J Clin Oncol. 31:3997–4013. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Trillet-Lenoir V, Freyer G, Kaemmerlen P,
Fond A, Pellet O, Lombard-Bohas C, Gaudin JL, Lledo G, Mackiewicz
R, Gouttebel MC, et al: Assessment of tumour response to
chemotherapy for metastatic colorectal cancer: Accuracy of the
RECIST criteria. Br J Radiol. 75:903–908. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Japanese Society for Cancer of the Colon
and RectumGeneral Rules for Clinical and Pathological Studies on
Cancer of the Colon, Rectum and Anus. 7th edition. Tokyo: Japanese
Society for Cancer of the Colon and Rectum; 2006
|
|
17
|
Edge SB, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: AJCC cancer staging manual. 7th edition.
Springer NY; New York: 2010
|
|
18
|
Rubbia-Brandt L, Giostra E, Brezault C,
Roth AD, Andres A, Audard V, Sartoretti P, Dousset B, Manjo PE,
Soubrane O, et al: Importance of histological tumor response
assessment in predicting the outcome in patients with colorectal
liver metastases treated with neo-adjuvant chemotherapy followed by
liver surgery. Ann Oncol. 18:299–304. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dede K, Salamon F, Landherr L, Jakab F and
Bursics A: Pathologic assessment of response to chemotherapy in
colorectal cancer liver metastases after hepatic resection: which
method to use? Pathol Oncol Res. 21:173–179. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Noble F, Hopkins J, Curtis N, Kelly JJ,
Bailey IS, Byrne JP, Bateman AC, Bateman AR and Underwood TJ: The
role of systemic inflammatory and nutritional blood-borne markers
in predicting response to neoadjuvant chemotherapy and survival in
oesophagogastric cancer. Med Oncol. 30:5962013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Fareed KR, Al-Attar A, Soomro IN, Kaye PV,
Patel J, Lobo DN, Parsons SL and Madhusudan S: Tumour regression
and ERCC1 nuclear protein expression predict clinical outcome in
patients with gastro-oesophageal cancer treated with neoadjuvant
chemotherapy. Br J Cancer. 102:1600–1607. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Valtorta E, Misale S, Sartore-Bianchi A,
Nagtegaal ID, Paraf F, Lauricella C, Dimartino V, Hobor S, Jacobs
B, Ercolani C, et al: KRAS gene amplification in colorectal cancer
and impact on response to EGFR-targeted therapy. Int J Cancer.
133:1259–1265. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nishioka Y, Shindoh J, Yoshioka R, Gonoi
W, Abe H, Okura N, Yoshida S, Oba M, Hashimoto M, Watanabe G, et
al: Radiological morphology of colorectal liver metastases after
preoperative chemotherapy predicts tumor viability and
postoperative outcomes. J Gastrointest Surg. 19:1653–1661. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chun YS, Vauthey JN, Boonsirikamchai P,
Maru DM, Kopetz S, Palavecino M, Curley SA, Abdalla EK, Kaur H,
Charnsangavej C and Loyer EM: Association of computed tomography
morphologic criteria with pathologic response and survival in
patients treated with bevacizumab for colorectal liver metastases.
JAMA. 302:2338–2344. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Van Triest B, Pinedo HM, Giaccone G and
Peters GJ: Downstream molecular determinants of response to
5-fluorouracil and antifolate thymidylate synthase inhibitors. Ann
Oncol. 11:385–391. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bertino JR and Banerjee D: Is the
measurement of thymidylate synthase to determine suitability for
treatment with 5-fluoropyrimidines ready for prime time? Clin
Cancer Res. 9:1235–1239. 2003.PubMed/NCBI
|
|
27
|
Popat S, Matakidou A and Houlston RS:
Thymidylate synthase expression and prognosis in colorectal cancer:
A systematic review and meta-analysis. J Clin Oncol. 22:529–536.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Leichman CG, Lenz HJ, Leichman L,
Danenberg K, Baranda J, Groshen S, Boswell W, Metzger R, Tan M and
Danenberg PV: Quantitation of intratumoral thymidylate synthase
expression predicts for disseminated colorectal cancer response and
resistance to protracted-infusion fluorouracil and weekly
leucovorin. J Clin Oncol. 15:3223–3229. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shirota Y, Stoehlmacher J, Brabender J,
Xiong YP, Uetake H, Danenberg KD, Groshen S, Tsao-Wei DD, Danenberg
PV and Lenz HJ: ERCC1 and thymidylate synthase mRNA levels predict
survival for colorectal cancer patients receiving combination
oxaliplatin and fluorouracil chemotherapy. J Clin Oncol.
19:4298–4304. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Silvestris N, Simone G, Partipilo G,
Scarpi E, Lorusso V, Brunetti AE, Maiello E, Paradiso A and Mangia
A: CES2, ABCG2, TS and Topo-I primary and synchronous metastasis
expression and clinical outcome in metastatic colorectal cancer
patients treated with first-line FOLFIRI regimen. Int J Mol Sci.
15:15767–15777. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Arienti C, Tesei A, Verdecchia GM,
Framarini M, Virzi S, Grassi A, Scarpi E, Turci L, Silverstrini R,
Amadori D and Zoli W: Role of conventional chemosensitivity test
and tissue biomarker expression in predicting response to treatment
of peritoneal carcinomatosis from colon cancer. Clin Colorectal
Cancer. 12:122–127. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Locker GY, Hamilton S, Harris J, Jessup
JM, Kemeny N, Macdonald JS, Somerfield MR, Hayes DF and Bast RC Jr:
ASCO: ASCO 2006 update of recommendations for the use of tumor
markers in gastrointestinal cancer. J Clin Oncol. 24:5313–5327.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lim B, Mun J, Kim JH, Kim CW, Roh SA, Cho
DH, Kim YS and Kim JC: Genome-wide mutation profiles of colorectal
tumors and associated liver metastases at the exome and
transcriptome levels. Oncotarget. 6:22179–22190. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Baba H, Baba Y, Uemoto S, Yoshida K,
Saiura A, Watanabe M, Maehara Y, Oki E, Ikeda Y, Matsuda H, et al:
Changes in expression levels of ERCC1, DPYD, and VEGFA mRNA after
first-line chemotherapy of metastatic colorectal cancer: Results of
a multicenter study. Oncotarget. 6:34004–34013. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
López-Gómez M, Moreno-Rubio J,
Suárez-García I, Cejas P, Madero R, Casado E, Jiménez A, Sereno M,
Gómez-Raposo C, Zambrana F, et al: SMAD4 and TS expression might
predict the risk of recurrence after resection of colorectal liver
metastases. Clin Trans Oncol. 17:133–138. 2015. View Article : Google Scholar
|
|
36
|
Kumamoto K, Kuwabara K, Tajima Y, Amano K,
Hatano S, Ohsawa T, Okada N, Ishibashi K, Haga N and Ishida H:
Thymidylate synthase and thymidine phosphorylase mRNA expression in
primary lesions using laser capture microdissection is useful for
prediction of the efficacy of FOLFOX treatment in colorectal cancer
patients with liver metastasis. Oncol Lett. 3:983–989. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Jones OM, Rees M, John TG, Bygrave S and
Plant G: Biopsy of resectable colorectal liver metastases causes
tumour dissemination and adversely affects survival after liver
resection. Br J Surg. 92:1165–1168. 2005. View Article : Google Scholar : PubMed/NCBI
|