Introduction
Infection with Mycobacterium tuberculosis may
lead to the development of masses in the lungs (1) or musculoskeletal sites, which are often
referred to as tuberculomas (2).
When tuberculoma develops in the wrist, it often induces an
inflammatory reaction, such as tenosynovitis, due to the related
friction (3). Cases of wrist
tuberculoma with tenosynovitis are relatively uncommon, but are
becoming more frequent due to the increasing incidence of
tuberculosis worldwide (3–5). However, to the best of our knowledge,
no case reports to date have described tuberculomas with
phlegmon-like symptoms. Therefore, we herein report an uncommon
case of wrist tuberculoma with phlegmon-like symptoms and review
the related literature.
Case report
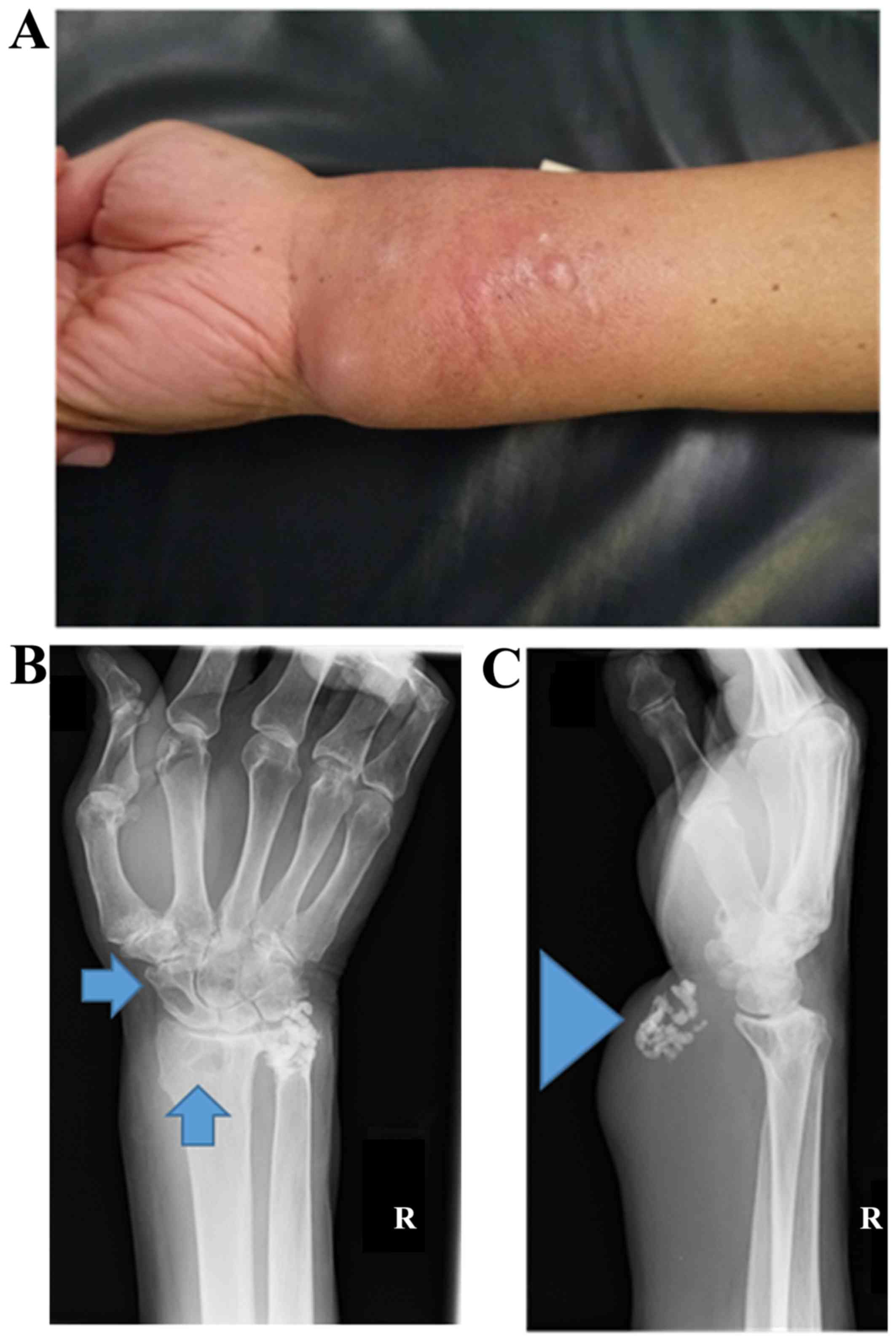
A 79-year old man noticed a swelling in his left
wrist and forearm 3 months before he visited the Kindai University
Hospital (Osaka-Sayama, Japan), although he did not report
experiencing wrist pain. The patient did not have any significant
medical history and had never had tuberculosis. A physical
examination revealed that his left wrist was erythematous and felt
warm to the touch (Fig. 1A),
although the range of motion of the wrist was normal, there was no
numbness of the hand or fingers, and the muscle strength was also
normal. The blood testing results were normal, with no evidence of
an inflammatory reaction (Table I).
The C-reactive protein concentration was 0.21 mg/dl, with a white
blood cell count of 8,500/µl and an erythrocyte sedimentation rate
of 4 mm/h.
 | Table I.Blood test results. |
Table I.
Blood test results.
| Tests | Normal value | Preoperative
values |
|---|
| C-reactive protein
(mg/dl) | 0.0–0.1 | 0.21 |
| Aspartate
transaminase (U/l) | 13.0–30.0 | 23 |
| Alanine transaminase
(U/l) | 7.0–23.0 | 22 |
| White blood cells
(×103 µl) | 3.3–8.6 | 8.5 |
| Hemoglobin
(g/dl) | 11.6–14.8 | 14.8 |
| Platelets
(×104 µl) | 15.8–34.8 | 30.1 |
| Blood urea nitrogen
(mg/dl) | 8.0–20.0 | 14 |
| Creatinine
(mg/dl) | 0.5–0.8 | 0.65 |
| Sodium (mEq/l) | 138.0–145.0 | 139 |
| Potassium
(mEq/l) | 3.6–4.8 | 4.3 |
| Chlorine (mEq/l) | 101.0–108.0 | 104 |
| Total protein
(g/dl) | 6.6–8.1 | 5.9 |
| Albumin (g/dl) | 4.1–5.1 | 3.3 |
Radiography revealed lytic regions at the radius and
scaphoid, as well as calcification in the volar side of the wrist
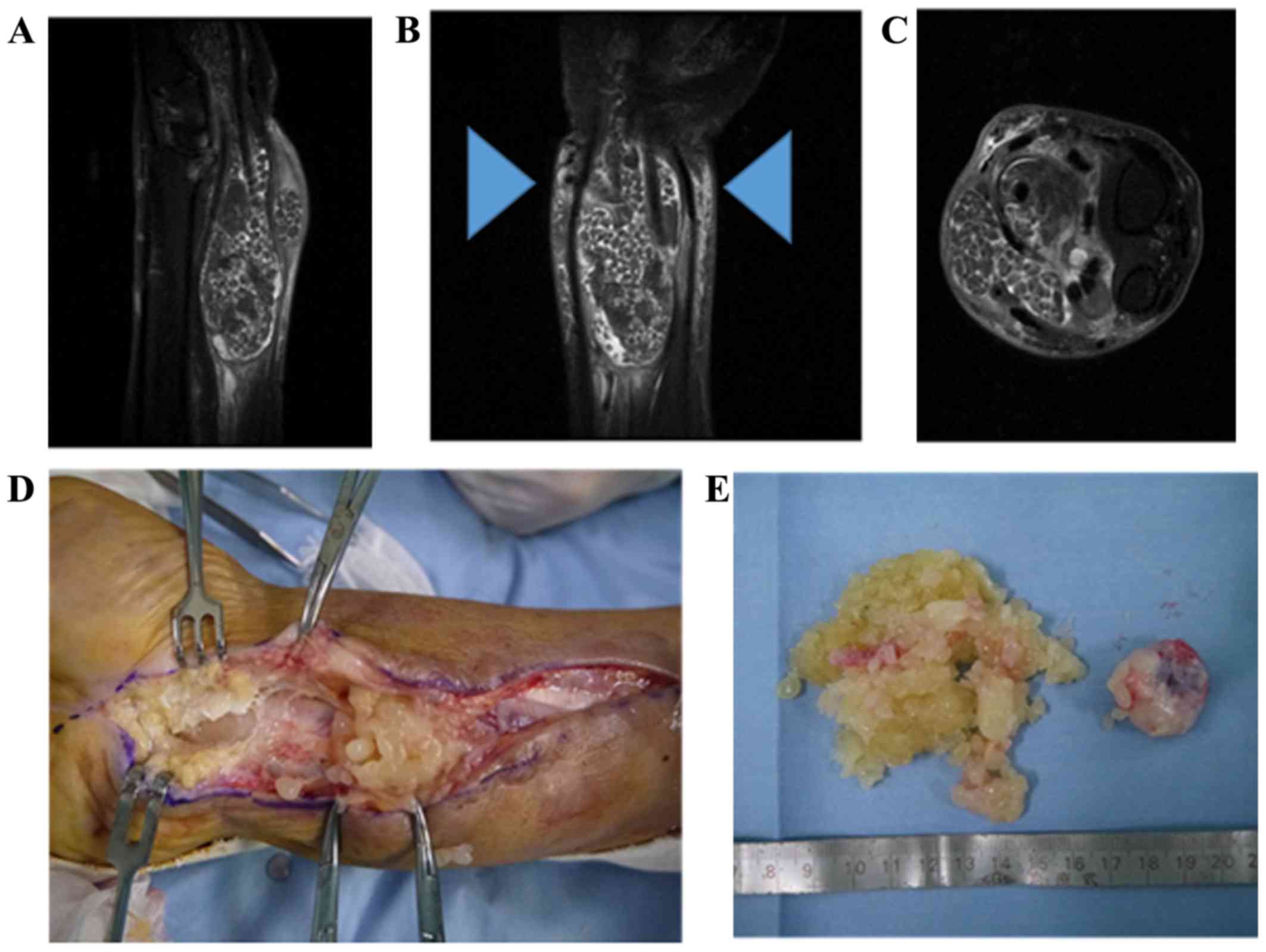
(Fig. 1B and C). Magnetic resonance
imaging revealed a mosaic mass that involved the flexor tendons in
the T1-weighted and T2-weighed images (Fig. 2A-C), with a high-intensity area in
the T2-weighed image (Fig. 2B).
Incisional biopsy was performed and numerous rice bodies were
discovered in the wrist (Fig. 2D). A
rapid pathological evaluation revealed necrosis, and as many rice
bodies as possible were removed (Fig.
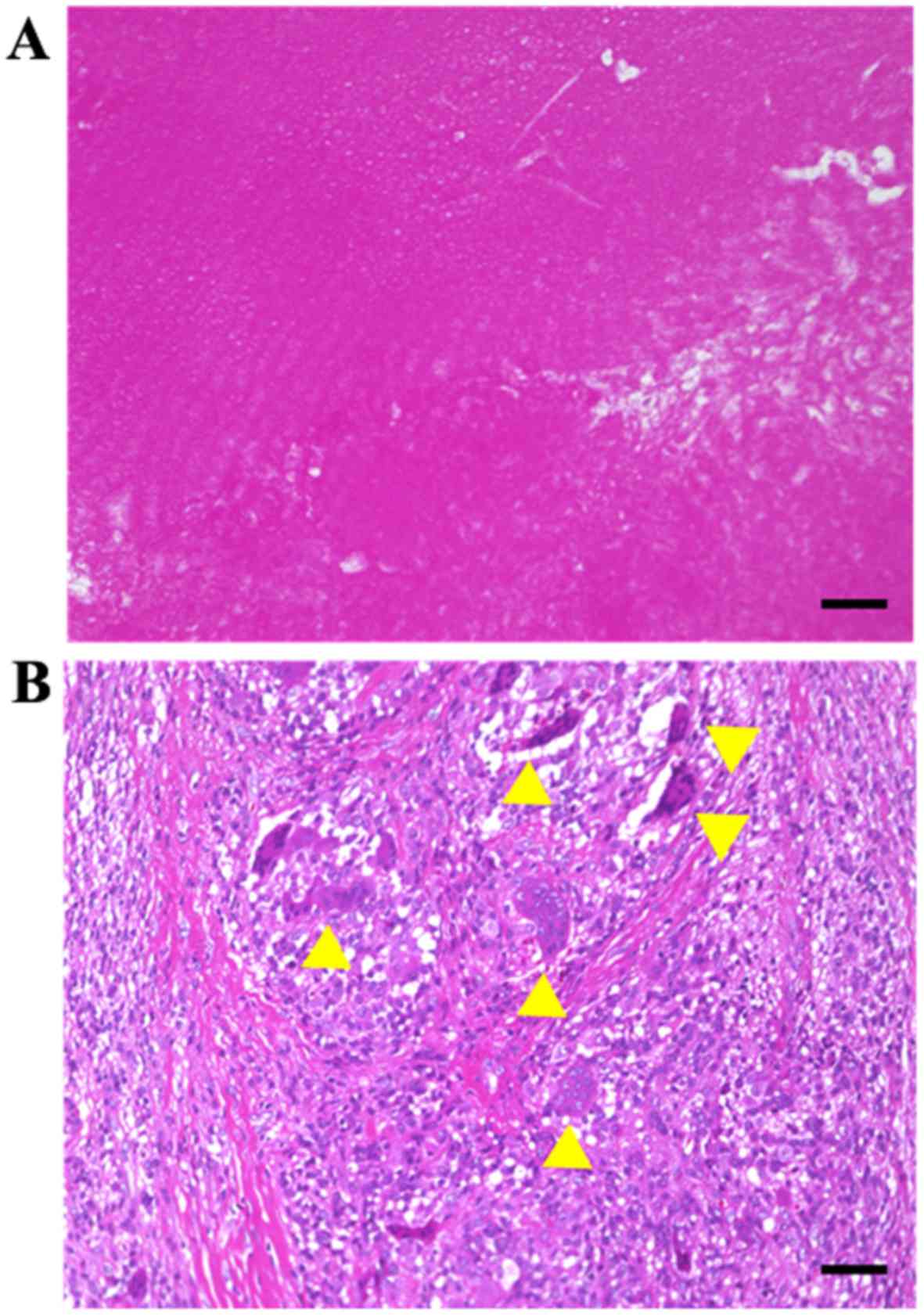
2E). A histological evaluation of the resected specimens
revealed caseous necrosis and Langhans giant cells (Fig. 3A and B). After consulting the
Infection Prevention and Control Team, the patient received
postoperative antibiotic treatment (pyrazinamide 1,100 mg/day,
isoniazid 200 mg/day, rifampicin 450 mg/day and ethambutol 1,000
mg/day). The treatment was scheduled for a 2-month period, although
it was discontinued as the patient developed hepatic insufficiency
after 2 weeks of treatment (aspartate transaminase level 1,038 U/l
and alanine transaminase level 1,506 U/l). After the treatment was
stopped, the patient's hepatic function normalized (aspartate
transaminase 19 U/l and alanine transaminase 21 U/l), and no
recurrence was detected at 1 year after treatment.
Discussion
Musculoskeletal tuberculoma is relatively uncommon
(6), although it may result in the
formation of rice bodies and the development of tenosynovitis in
the wrists (3–6). However, there are no reports describing
phlegmon-like symptoms (redness and heat), which were observed in
the present case. Previous studies have indicated that wrist
tuberculoma predominantly affects men and predominantly involves
the right wrist (7), with overuse of
the dominant hand potentially inducing tuberculoma with
tenosynovitis (8). However, our
patient reported that he had a dominant right hand, while the
lesion developed in his left wrist. In general, redness and heat
are not common signs of tuberculoma, which typically involves a
cold abscess (9). In the present
case, the phlegmon-like symptoms were likely caused by the friction
between the flexor tendons and the lesion, as a subcutaneous
infection was excluded based on the absence of inflammatory markers
in the blood test results. Therefore, it is important for
physicians to be aware that a wrist tuberculoma may manifest with
phlegmon-like symptoms.
The route of infection may involve direct invasion
or a hematogenous spread from a distant primary site, such as the
lungs, lymph nodes, bones, soft tissues, or genitourinary tract
(10). This condition should be
suspected in cases that involve trauma, overuse of the joint, older
age, malnutrition, and decreased immune function (11). Although the mechanism of infection in
this patient was not elucidated, he was an older man with decreased
immune function, and it is possible that the infection involved the
lymph nodes.
Rice bodies were first described by Reise in 1895
(12) and are observed in ~50% of
wrist tuberculomas (7). These
objects macroscopically resemble shiny white rice grains, whereas
microscopically they consist of an inner amorphous core of
acidophilic material surrounded by fibrin and collagen (5). Their pathogenesis is unclear, although
they may originate from microinfarcted synovium and induce synovial
shedding with subsequent encasement by fibrin derived from the
synovial fluid. It is also possible that early rice bodies form
de novo and independently of synovial elements, with
progressive enlargement that is driven by fibrin aggregation
(5,13). In this context, the disease
progresses through distinct histopathological stages that are
dependent on the status, the patient's immune function, and the
virulence of the infecting pathogen (7,11). The
first stage involves replacement of the tendon by granulation
tissue, which is followed by the sheath being obliterated by
fibrous tissue, and finally caseation leading to the appearance of
rice bodies. At this point, the tendons may only consist of a few
strands of tissue and are prone to spontaneous rupture (7,11). Our
patient was likely between the third and final stages. Previous
studies have indicated that surgical intervention should be
avoided, as rice bodies per se can be harmless (4,7);
however, surgical treatment was performed in the present case due
to the phlegmon-like symptoms and the absence of a definitive
diagnosis.
The diagnosis of tuberculous tenosynovitis is often
delayed, as the symptoms may mimic those of atypical mycobacterial
infections, tuberculosis, systemic lupus erythematosus,
brucellosis, foreign body tendonitis, osteoarthritis and rheumatoid
arthritis (5,7). Thus, the diagnosis must be confirmed by
biopsy and culture of the histopathological specimens, although
these steps require a significant length of time and may delay
diagnosis and treatment. Therefore, when the tentative diagnosis is
tuberculous tenosynovitis, antibiotic treatment should be started
while waiting for the results (7,14).
However, anti-tuberculosis drugs often induce hepatic dysfunction
(15,16), with elevation of biliary or hepatic
enzymes (e.g., aspartate transaminase and alanine transaminase)
being common in elderly patients (16). Thus, careful observation is necessary
when using anti-tuberculosis drugs to treat elderly patients, as in
the present case.
The recommended surgical technique involves
decompression of the median nerve when this condition is associated
with clinical symptoms of carpal tunnel syndrome (17). Local recurrence is possible, and ~50%
of the cases develop recurrence within 1 year (18). However, our patient did not
experience recurrence within the first year, which may be
attributed to the rapid diagnosis and treatment.
In conclusion, we encountered a case of tuberculoma
with phlegmon-like symptoms in an elderly patient. Therefore,
tuberculoma should be considered in the differential diagnosis of
patients with an erythematous, warm and swollen wrist. Rapid
diagnosis and treatment are required to ensure good outcomes in
such cases.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data presented in this study are available from
the corresponding author upon reasonable request.
Authors' contributions
Data acquisition: KH, SN, NO and RK. Data analysis:
KH, SN NO and MA. Manuscript preparation: KH and MA. All authors
have read and approved the final version of this manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided informed consent for the
publication of the case details and associated images.
Competing interests
The authors declare that they have no competing
interests to disclose.
References
|
1
|
Li CR, Li YZ, Li YM and Zheng YS: Dynamic
and contrast enhanced CT imaging of lung carcinoma, pulmonary
tuberculoma and inflammatory pseudotumor. Eur Rev Med Pharmacol
Sci. 21:1588–1592. 2017.PubMed/NCBI
|
|
2
|
Ju HB, Guo DM and Chen FF: Intramedullary
cervical tuberculoma: A case report with note on surgical
management. Int Surg. 100:133–136. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Anoumou MN, Kouame M, Daix T and Yepie A:
Tuberculosis tenosynovitis of the flexor tendons in the wrist: A
case report. Acta Orthop Traumatol Turc. 48:690–692. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Woon CY, Phoon ES, Lee JY, Puhaindran ME,
Peng YP and Teoh LC: Rice bodies, millet seeds and melon seeds in
tuberculous tenosynovitis of the hand and wrist. Ann Plast Surg.
66:610–617. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ergun T, Lakadamyali H and Aydin O:
Multiple rice body formation accompanying the chronic nonspecific
tenosynovitis of flexor tendons of the wrist. Radiat Med.
26:545–548. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sbai MA, Benzarti S, Bouzaidi K, Sbei F
and Maalla R: A rare localization of tuberculosis of the wrist: The
scapholunate joint. Int J Mycobacteriol. 4:161–164. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Baidoo PK, Baddoo D, Ocloo A, Agbley D,
Lartey S and Baddoo NA: Tuberculous tenosynovitis of the flexor
tendons of the wrist: A case report. BMC Res Notes. 11:2382018.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hoffman KL, Bergman AG, Hoffman DK and
Harris DP: Tuberculous tenosynovitis of the flexor tendons of the
wrist: MR imaging with pathologic correlation. Skeletal Radiol.
25:186–188. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kouassi KJ, Yao LB, Sery BJLN, M'bra KI,
Krah KL, Lohourou GF and Kodo M: Dorsolumbar cold abscess revealing
Pott's disease. Pan Afr Med J. 27:22017.PubMed/NCBI
|
|
10
|
Higuchi S, Ishihara S, Kobayashi H and
Arai T: A mass lesion of the wrist: A rare manifestation of
tuberculosis. Intern Med. 47:313–316. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lall H, Nag SK, Jain VK, Khare R and
Mittal D: Tuberculous extensor tenosynovitis of the wrist with
extensor pollicis longus rupture: A case report. J Med Case
Reports. 3:1422009. View Article : Google Scholar
|
|
12
|
Reise H: Die Reiskorpschen in
tuberculserkrankensynovalsacken. Dtsch Z Chir. 42:11895.(In
German).
|
|
13
|
Popert AJ, Scott DL, Wainwright AC, Walton
KW, Williamson N and Chapman JH: Frequency of occurrence, mode of
development and significance or rice bodies in rheumatoid joints.
Ann Rheum Dis. 41:109–117. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wali H, Al-Khuwaitir S and Hafeez MA:
Compound palmar ganglion: A case report and literature review. Ann
Saudi Med. 6:55–59. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cao J, Mi Y, Shi C, Bian Y, Huang C, Ye Z,
Liu L and Miao L: First-line anti-tuberculosis drugs induce
hepatotoxicity: A novel mechanism based on a urinary metabolomics
platform. Biochem Biophys Res Commun. 497:485–491. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chang LY, Lee CH, Chang CH, Lee MC, Lee
MR, Wang JY and Lee LN: Acute biliary events during
anti-tuberculosis treatment: Hospital case series and a nationwide
cohort study. BMC Infect Dis. 18:642018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Jaovisidha S, Chen C, Ryu KN,
Siriwongpairat P, Pekanan P, Sartoris DJ and Resnick D: Tuberculous
tenosynovitis and bursitis: Imaging findings in 21 cases.
Radiology. 201:507–513. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Regnard PJ, Barry P and Isselin J:
Mycobacterial tenosynovitis of the flexor tendons of the hand. A
report of five cases: J Hand Surg. 21:351–354. 1996.
|