Introduction
Cleft lip with or without cleft palate (CL/P) is the
most frequent congenital abnormality in the maxillofacial region.
The prevalence of cleft lip with or without cleft palate in Japan
is 1.73 per 1,000 individuals (1).
As a disease model for CL/P, a multi-factorial threshold model
involving several genetic and environmental factors has been
proposed to explain the development of CL/P, but it is difficult to
identify key factors (2).
Modifications in various genes have been proposed to be related to
the development of CL/P, including IRF6, VAX1, 8q24
locus, ABCA4, MAFB, and 17q22 locus (which were
identified mainly by genome-wide association studies), and BMP4,
FGFR2, FOXE1, MSX1, MYH9, CHIRSPLD2 FGF8, GSTT1, MTHFR, PDGFC,
PVRL1, SUMO1, TGFα, and TGFβ3 (which were revealed
mainly by candidate gene association or mutation detection studies)
(3,4). Smoking, alcohol consumption, drug use,
and viral infection during pregnancy have been proposed to be
associated with the development of CL/P as environmental factors
(2).
It has been known for decades that vitamin
deficiencies during pregnancy can cause congenital abnormalities.
Folic acid deficiency is well known to affect neural tube closure
and the development of orofacial clefts, and supplementation with
folic acid was demonstrated to reduce the frequencies of congenital
abnormalities (2,5-7). In
A/J mice, folic acid administered before and during pregnancy
reduced the onset of naturally developed CL/P (8,9).
Tolarova and Harris and Shaw et al reported a decrease in
the prevalence of CL/P when mothers took vitamin supplements
including folic acid before and during pregnancy until the
organogenesis stage (10,11).
Regarding the metabolism of folic acid, the enzyme
activity of 5,10-methylenetetrahydrofolate reductase (MTHFR)
was proposed to be a rate-determining step influencing serum folic
acid levels (12). Polymorphisms of
the MTHFR gene at base pair 677 and 1298 (C677T; rs1801133,
A1298C; rs1801131) were demonstrated to decrease the enzyme
activity (13). These polymorphisms
were also suggested to be correlated with CL/P (11,14). We
conducted the present study to investigate the relationship between
MTHFR gene polymorphisms and the development of CL/P in a
Japanese population.
Patients and methods
Patients
The patient series included Japanese individuals
with non-syndromic CL/P treated at the Department of Oral and
Maxillofacial Surgery, Dokkyo Medical University Hospital or the
Cleft Lip and Palate Center, Aichi-Gakuin University Dental
Hospital. The patients, parents and guardians of the patients and
control subjects provided informed consent for the investigation of
gene polymorphisms for MTHFR by polymerase chain reaction
(PCR) amplification of their DNA fragment. The study was approved
by the Clinical Research Ethics Committee of Dokkyo University
Hospital (approval no. R-33-22J), and the Research Ethics Committee
of Aichi-Gakuin University School of Dentistry (approval no. 55).
The samples were collected from April 2004 to March 2007 at
Aichi-Gakuin University Dental Hospital and from June 2007 to May
2008 at Dokkyo Medical University Hospital. We were able to analyze
240 patients as well as 103 fathers and 153 mothers of these
patients. As controls, 68 volunteers with no congenital
abnormalities (including cleft lip and palate) and no family
history of congenital abnormality were also enrolled (Table I).
 | Table IDemographic data of the study cohort
(n=240), parents and controls. |
Table I
Demographic data of the study cohort
(n=240), parents and controls.
| Sex | | | Total no. of
cases |
|---|
| Male | | | 129 |
| Female | | | 111 |
| Demographic data
labeled by type of abnormality |
| Type of
abnormality | Sex | | No. of cases |
| CLA | | | 73 |
|
Right
cleft | Male | | 16 |
| | | Incomplete | 12 |
| | | Complete | 3 |
| | | Unknown | 1 |
| | Female | | 5 |
| | | Incomplete | 3 |
| | | Complete | 2 |
| | | Unknown | 0 |
|
Left
cleft | Male | | 18 |
| | | Incomplete | 13 |
| | | Complete | 4 |
| | | Unknown | 1 |
| | Female | | 21 |
| | | Incomplete | 10 |
| | | Complete | 10 |
| | | Unknown | 1 |
|
Bilateral
cleft | Male | | 8 |
| | | Incomplete | 3 |
| | | Complete | 4 |
| | | Unknown | 1 |
| | Female | | 4 |
| | | Incomplete | 3 |
| | | Complete | 1 |
| | | Unknown | 0 |
| Unidentified | | | 1 |
|
CLP | | | 124 |
|
Right
cleft | Male | | 23 |
| | | Incomplete | 6 |
| | | Complete | 15 |
| | | Unknown | 2 |
| | Female | | 22 |
| | | Incomplete | 3 |
| | | Complete | 17 |
| | | Unknown | 2 |
|
Left
cleft | Male | | 32 |
| | | Incomplete | 9 |
| | | Complete | 21 |
| | | Unknown | 2 |
| | Female | | 22 |
| | | Incomplete | 3 |
| | | Complete | 18 |
| | | Unknown | 1 |
|
Bilateral
cleft | Male | | 20 |
| | | Incomplete | 2 |
| | | Complete | 17 |
| | | Unknown | 1 |
| | Female | | 5 |
| | | Incomplete | 1 |
| | | Complete | 2 |
| | | Unknown | 2 |
| CP | | | 43 |
| Demographic data
labeled by family members, and controls |
| Family members | Type of
abnormality | | No of cases |
| Fathers: | | | 103 |
| | of CLA | | 32 |
| | of CP | | 17 |
| | of CLP | | 54 |
| Mothers: | | | 153 |
| | of CLA | | 51 |
| | of CP | | 34 |
| | of CLP | | 68 |
| Controls: | | | 68 |
| | Male | | 29 |
| | Female | | 39 |
PCR amplification and detection of the
restriction fragment length polymorphisms (RFLPs)
DNA was extracted from all of the subject peripheral
blood samples with the use of the DNA Blood Mini kit (Qiagen GmbH)
following the manufacturer's instructions. The extracted DNA was
dissolved in Tris-EDTA buffer and stored at -80˚C until analysis.
For the detection of the C677T polymorphism, the following primers
were used: Forward primer, 5'-TGAAGGAGAAGGTGTCTGCGGGA-3' and
reverse primer, 5'-AGGACGGTGCGGTGAGAGTG-3' (15). DNA (200 ng) was used as a template,
and each primer set (0.2 µM final concentration) was treated in 10
µl of reaction solution containing 0.25 U Takara Ex Taq®
(Takara Bio), dNTPs (0.4 mM each), and reaction buffer containing 4
mM Mg2+. After preheating for 5 min at 94˚C, the samples
were denatured for 1 min at 94˚C followed by amplification at 64˚C
for 1 min and extension at 72˚C for 1 min; the reaction was
operated for 30 cycles following extension at 72˚C for 5 min.
For the detection of the A1298C polymorphism, the
following primers were used: Forward primer,
5'-CTTTGGGGAGCTGAAGGACTACTAC-3' and reverse primer:
5'-CACTTTGTGACCATTCCGGTTTG-3' (16).
We used 200 ng of DNA as a template, and each primer set (0.2 µM
final concentration) was treated in 10 µl of reaction solution
containing 0.25 U Takara Ex Taq®, dNTPs (0.4 mM each),
and reaction buffer containing 4 mM Mg2+. After
preheating at 94˚C for 5 min, the samples were denatured at 94˚C
for 1 min followed by amplification at 57˚C for 1 min and extension
at 72˚C for 1 min; the reaction was repeated for 30 cycles
following extension at 72˚C.
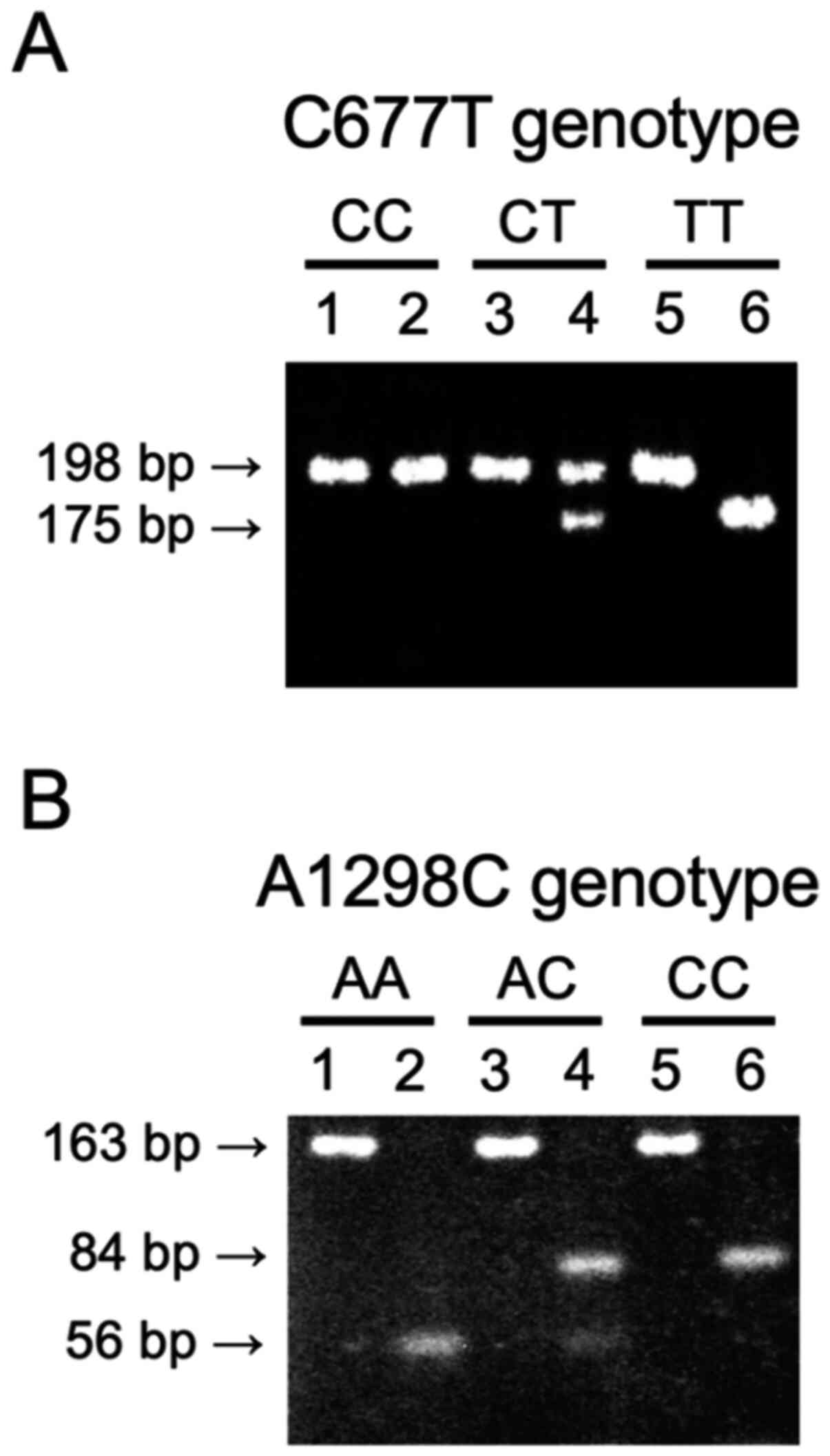
The PCR products amplified by the two primer sets
were digested by restriction enzymes for the detection of
polymorphisms. For C677T detection, the PCR products were a 198-bp
fragment. Conversion of C to T creates an HinfI restriction site,
the 198 bp fragment was digested into 175-bp and 23-bp fragments
(Fig. 1A). For the A1298C detection,
the PCR products were 163 bp and MboII digested the fragment into
56-bp, 31-bp, 30-bp, 28-bp and 18-bp fragments. Conversion of A to
C abolishes the MboII restriction site, it digests into 84, 31, 30,
18 bp fragments (Fig. 1B). All the
subject genotypes were determined by PCR-RFLP and the allele and
genotype frequencies were determined. With regard to the C677T
polymorphism, the wild-type 677th base of the MTHFR gene is
referred to as CC (677CC), the heterozygous type as CT (677CT), and
the recessive type as TT (677TT). With regard to the A1298C
polymorphism, the wild-type is referred to as AA (1298AA), the
heterozygous type as AC (1298AC), and the recessive type as CC
(1298CC).
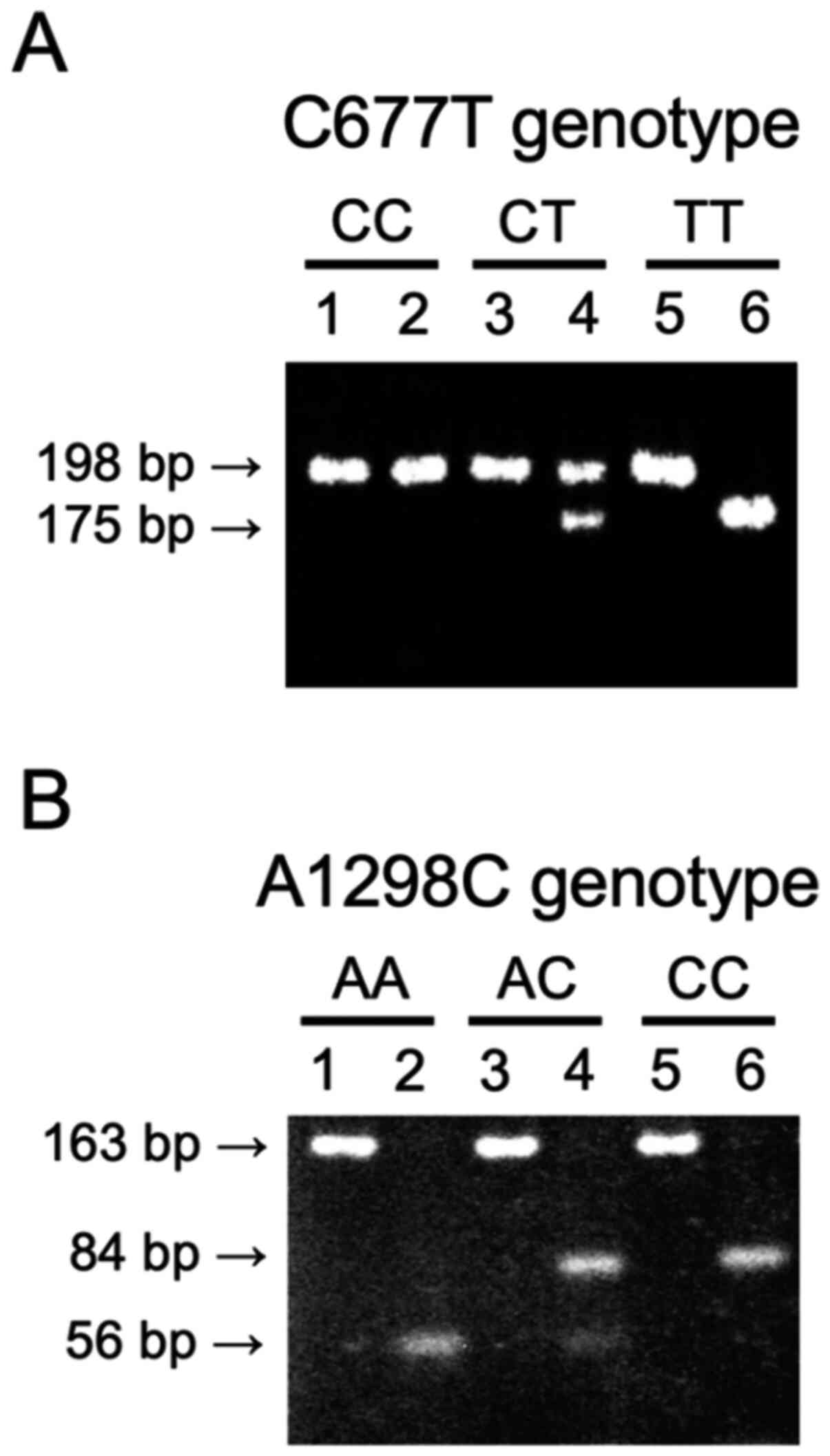 | Figure 1Representative data of PCR-RFLP. (A)
MTHFR C677T polymorphism. The 198 fragment represents the C
allele and the 175 bp fragment represents the T allele. Lane 1, PCR
product of genotype CC; lane 2, PCR products of genotype CC
digested with HinfI; lane 3, PCR product of genotype CT; lane 4,
PCR products of genotype CT digested with HinfI; lane 5, PCR
products of genotype TT; lane 6, PCR products of genotype TT
digested with HinfI. (B) MTHFR A1298C polymorphism. The
fragment of 163 bp is the total length of PCR products, the 56 bp
fragment represents the A allele, the fragment of 84 bp represents
the C allele, respectively. Lane 1, PCR product of genotype AA;
lane 2, PCR products of genotype AA digested with MboII; lane 3,
PCR product of genotype AC; lane 4, PCR products of genotype AC
digested with MboII; lane 5, PCR products of genotype CC; lane 6,
PCR products of genotype CC digested with MboII. PCR, polymerase
chain reaction; RFLP, restriction fragment length polymorphisms;
MTHFR, 5,10-methylentetrahydrofolate reductase. |
Transmission disequilibrium test
(TDT)
We examined the over-transmission of C677T and
A1298C from heterozygous parents to their children with CL/P
(patients) by conducting a transmission disequilibrium test (TDT).
The family-based association test (FBAT) developed by Laird and
Lange was conducted as previously described (17).
Haplotype analysis
Since the transmission of an allele from parents to
their children is known to differ from family to family, we
investigated the linkage disequilibrium of the subjects'
haplotypes. In linkage disequilibrium test, D, D' and r,
coefficient of linkage disequilibrium, were calculated. D indicates
the coefficient of linkage disequilibrium, D' is the normalized
coefficient of linkage disequilibrium, r is the coefficient of
correlation. SNPstats, a web tool for SNP analysis, (https://snpstats.net) was used to estimate the
haplotypes from genotype frequencies and to further analyze the
linkage disequilibrium and haplotype association with CL/P
(18).
Statistical analysis
We tested the Hardy-Weinberg equilibrium (HWE) for
each patient, the patient's father and mother, and the controls
with the use of the R package ‘HardyWeinberg’ (19,20).
Fisher's exact test was used for the statistical analyses. The
results of the TDT were analyzed using McNemar's test, and
haplotypes were analyzed with the use of SNPstats software. We
calculated the odds ratios (ORs) with confidence intervals (CIs) to
assess the associations of genotypes. The strength of the
association was tested under genetic models comparing the allele,
genotype, and dominant (TT+CT vs. CC for C677T; CC+AC vs. AA for
A1298C) or recessive (CC+CT vs. TT for C677T; AA+AC vs. CC for
A1298C) models, respectively. A P-value <0.05 was indicative of
a statistically significant difference.
Results
Polymorphism at base pair (bp) 677 of
the MTHFR gene
The genotype frequency of the MTHFR C677T
polymorphism of the patients, patients' fathers and mothers, and
controls were in agreement with the HWE: P=0.89, P=0.55, P=0.17,
and P=0.60, respectively. There were no significant differences in
the allele frequencies of C and T at bp 677 of the MTHFR
gene between the patients and controls. The genotype frequencies
also showed no significant differences between the patients and
controls (Table II). The dominant
or recessive genetic model for C677T was tested to investigate the
association of genotypes and CL/P, although the results revealed no
association (Table II).
 | Table IIPolymorphisms of MTHFR
C677T. |
Table II
Polymorphisms of MTHFR
C677T.
| | Odds ratio |
|---|
| Group | Polymorphism | Cases (n=240) n
(%) | Controls (n=68) n
(%) | OR | 95% CI | P-value |
|---|
| Patient | Genotype | | | | | |
| |
CC | 89 (37.1) | 27 (39.7) | 1.000 | | |
| |
CT | 116 (48.3) | 34 (50.0) | 1.035 | 0.582-1.841 | 0.907 |
| |
TT | 35 (14.6) | 7 (10.3) | 1.517 | 0.605-3.801 | 0.372 |
| | Allele | | | | | |
| |
C | 294 (61.3) | 88 (64.7) | 1.000 | | |
| |
T | 186 (38.8) | 48 (35.3) | 1.160 | 0.780-1.725 | 0.464 |
| | Genetic model | | | | | |
| |
Dominant | 151 (62.9) | 41 (60.3) | 1.117 | 0.643-1.940 | 0.694 |
| |
Recessive | 205 (85.4) | 61 (89.7) | 0.672 | 0.284-1.589 | 0.363 |
| Type of cleft | | | | | | |
|
CLA | Genotype | | | | | |
| |
CC | 32 (43.8) | 27 (39.7) | 1.000 | | |
| |
CT | 32 (43.8) | 34 (50.0) | 0.794 | 0.393-1.605 | 0.521 |
| |
TT | 9 (12.4) | 7 (10.3) | 1.085 | 0.357-3.300 | 0.886 |
| | Allele | | | | | |
| |
C | 95 (66.0) | 88 (64.7) | 1.000 | | |
| |
T | 49 (34.0) | 48 (35.3) | 0.946 | 0.578-1.547 | 0.824 |
| | Genetic model | | | | | |
| |
Dominant | 41 (56.2) | 41 (60.3) | 0.844 | 0.431-1.650 | 0.619 |
| |
Recessive | 64 (87.7) | 25 (78.1) | 1.991 | 0.669-5.925 | 0.210 |
|
CLP | Genotype | | | | | |
| |
CC | 41 (33.1) | 27 (39.7) | 1.000 | | |
| |
CT | 61 (49.2) | 34 (50.0) | 1.181 | 0.622-2.245 | 0.610 |
| |
TT | 22 (17.7) | 7 (10.3) | 2.070 | 0.777-5.512 | 0.141 |
| | Allele | | | | | |
| |
C | 143 (57.7) | 88 (64.7) | 1.000 | | |
| |
T | 105 (42.3) | 48 (35.3) | 1.346 | 0.873-2.075 | 0.177 |
| | Genetic model | | | | | |
| |
Dominant | 83 (66.9) | 41 (60.3) | 1.333 | 0.722-2.461 | 0.357 |
| |
Recessive | 102 (82.3) | 61 (89.7) | 0.532 | 0.215-1.319 | 0.168 |
|
CLA+CLP | Genotype | | | | | |
| |
CC | 73 (37.1) | 27 (39.7) | 1.000 | | |
| |
CT | 93 (47.2) | 34 (50.0) | 1.012 | 0.560-1.827 | 0.969 |
| |
TT | 31 (15.7) | 7 (10.3) | 1.638 | 0.645-4.158 | 0.296 |
| | Allele | | | | | |
| |
C | 239 (60.7) | 88 (64.7) | 1.000 | | |
| |
T | 155 (39.3) | 48 (35.3) | 1.189 | 0.793-1.784 | 0.403 |
| | Genetic model | | | | | |
| |
Dominant | 124 (62.9) | 41 (60.3) | 1.119 | 0.636-1.969 | 0.697 |
| |
Recessive | 166 (84.3) | 61 (89.7) | 0.614 | 0.257-1.468 | 0.270 |
|
CP | Genotype | | | | | |
| |
CC | 16 (37.2) | 27 (39.7) | 1.000 | | |
| |
CT | 23 (53.5) | 34 (50.0) | 1.142 | 0.506-2.576 | 0.750 |
| |
TT | 4 (9.30) | 7 (10.3) | 0.964 | 0.244-3.815 | 0.959 |
| | Allele | | | | | |
| |
C | 55 (64.0) | 88 (64.7) | 1.000 | | |
| |
T | 31 (36.0) | 48 (35.3) | 1.033 | 0.588-1.815 | 0.909 |
| | Genetic model | | | | | |
| |
Dominant | 27 (62.8) | 41 (60.3) | 1.111 | 0.506-2.440 | 0.793 |
| |
Recessive | 39 (90.7) | 61 (89.7) | 1.119 | 0.307-4.075 | 0.865 |
| Parents | | | | | | |
|
Father | Genotype | | | | | |
| |
CC | 31 (30.1) | 10 (34.5) | 1.000 | | |
| |
CT | 54 (52.4) | 15 (51.7) | 1.161 | 0.466-2.896 | 0.748 |
| |
TT | 18 (17.5) | 4 (13.8) | 1.452 | 0.397-5.31 | 0.572 |
| | Allele | | | | | |
| |
C | 116 (56.3) | 35 (60.3) | 1.000 | | |
| |
T | 90 (43.7) | 23 (39.7) | 1.181 | 0.652-2.138 | 0.583 |
| | Genetic model | | | | | |
| |
Dominant | 72 (69.9) | 19 (65.5) | 1.222 | 0.51-2.929 | 0.652 |
| |
Recessive | 85 (82.5) | 25 (86.2) | 0.756 | 0.234-2.438 | 0.638 |
|
Mother | Genotype | | | | | |
| |
CC | 56 (36.6) | 17 (43.6) | 1.000 | | |
| |
CT | 80 (52.3) | 19 (48.7) | 1.278 | 0.611-2.674 | 0.514 |
| |
TT | 17 (11.1) | 3 (7.70) | 1.720 | 0.45-6.583 | 0.424 |
| | Allele | | | | | |
| |
C | 192 (62.7) | 53 (67.9) | 1.000 | | |
| |
T | 114 (37.3) | 25 (32.1) | 1.259 | 0.742-2.136 | 0.393 |
| | Genetic model | | | | | |
| |
Dominant | 97 (63.4) | 22 (56.4) | 1.338 | 0.656-2.731 | 0.422 |
| |
Recessive | 136 (88.9) | 36 (92.3) | 0.667 | 0.185-2.401 | 0.533 |
Polymorphism at base pair (bp) 1298 of
the MTHFR gene
The genotype frequency of MTHFR A1298C
polymorphism of the patients, patients' fathers and mothers, and
controls were in agreement with the HWE: P=1.00, P=0.40, P=0.79,
and P=1.00, respectively. There were no significant differences in
the allele frequencies of A and C at bp 1298 of the MTHFR
gene between the patients and controls. The genotype frequency also
showed no significant difference between the patients and controls
(Table III). The dominant or
recessive genetic model for A1298C was tested to investigate the
association of genotypes and CL/P, although the results revealed no
association (Table III).
 | Table IIIPolymorphism of the MTHFR
A1298C. |
Table III
Polymorphism of the MTHFR
A1298C.
| | Odds ratio |
|---|
| Group | Polymorphism | Cases (n=240) n
(%) | Controls (n=68) n
(%) | OR | 95% CI | P-value |
|---|
| Patient | Genotype | | | | | |
| |
AA | 155 (64.6) | 43 (63.2) | 1.000 | | |
| |
AC | 77 (32.1) | 22 (32.4) | 0.971 | 0.552-1.382 | 0.921 |
| |
CC | 8 (3.30) | 3 (4.40) | 0.740 | 0.223-2.050 | 0.665 |
| | Allele | | | | | |
| |
A | 232 (73.2) | 65 (72.2) | 1.000 | | |
| |
C | 85 (26.8) | 25 (27.8) | 0.927 | 0.603-1.288 | 0.753 |
| | Genetic model | | | | | |
| |
Dominant | 85 (35.4) | 25 (36.8) | 0.943 | 0.557-1.357 | 0.838 |
| |
Recessive | 232 (96.7) | 65 (95.6) | 1.338 | 0.293-2.274 | 0.672 |
| Type of cleft | | | | | | |
|
CLA | Genotype | | | | | |
| |
AA | 51 (69.9) | 43 (63.2) | 1.000 | | |
| |
AC | 21 (28.8) | 22 (32.4) | 0.766 | 0.430-1.437 | 0.474 |
| |
CC | 1 (1.40) | 3 (4.40) | 0.562 | 0.124-2.533 | 0.533 |
| | Allele | | | | | |
| |
A | 72 (76.6) | 65 (72.2) | 1.000 | | |
| |
C | 22 (23.4) | 25 (27.8) | 0.759 | 0.485-1.336 | 0.369 |
| | Genetic model | | | | | |
| |
Dominant | 22 (30.1) | 25 (36.8) | 0.742 | 0.435-1.406 | 0.404 |
| |
Recessive | 71 (97.3) | 65 (95.6) | 1.638 | 0.201-3.074 | 0.592 |
|
CLP | Genotype | | | | | |
| |
AA | 73 (58.9) | 43 (63.2) | 1.000 | | |
| |
AC | 45 (36.3) | 22 (32.4) | 1.205 | 0.575-1.483 | 0.564 |
| |
CC | 6 (4.80) | 3 (4.40) | 0.356 | 0.142-1.930 | 0.165 |
| | Allele | | | | | |
| |
A | 118 (69.8) | 65 (72.2) | 1.000 | | |
| |
C | 51 (30.2) | 25 (27.8) | 1.151 | 0.638-1.370 | 0.589 |
| | Genetic model | | | | | |
| |
Dominant | 51 (41.1) | 25 (36.8) | 1.202 | 0.589-1.461 | 0.554 |
| |
Recessive | 118 (95.2) | 65 (95.6) | 0.908 | 0.232-2.191 | 0.894 |
|
CLA+CLP | Genotype | | | | | |
| |
AA | 124 (62.9) | 43 (63.2) | 1.000 | | |
| |
AC | 65 (33.0) | 22 (32.4) | 1.025 | 0.557-1.407 | 0.936 |
| |
CC | 8 (4.10) | 3 (4.40) | 0.925 | 0.245-2.141 | 0.911 |
| | Allele | | | | | |
| |
A | 189 (72.1) | 65 (72.2) | 1.000 | | |
| |
C | 73 (27.9) | 25 (27.8) | 0.998 | 0.617-1.313 | 0.994 |
| | Genetic model | | | | | |
| |
Dominant | 73 (37.1) | 25 (36.8) | 1.013 | 0.568-1.385 | 0.966 |
| |
Recessive | 189 (95.9) | 65 (95.6) | 1.090 | 0.267-2.190 | 0.900 |
|
CP | Genotype | | | | | |
| |
AA | 31 (72.1) | 43 (63.2) | 1.000 | | |
| |
AC | 11 (25.6) | 22 (32.4) | 0.694 | 0.362-1.517 | 0.402 |
| |
CC | 1 (2.30) | 3 (4.40) | 0.462 | 0.071-3.194 | 0.504 |
| | Allele | | | | | |
| |
A | 42 (77.8) | 65 (72.2) | 1.000 | | |
| |
C | 12 (22.2) | 25 (27.8) | 1.369 | 0.513-1.672 | 0.443 |
| | Genetic model | | | | | |
| |
Dominant | 12 (27.9) | 25 (36.8) | 0.666 | 0.366-1.480 | 0.335 |
| |
Recessive | 42 (97.7) | 65 (95.6) | 1.938 | 0.134-4.153 | 0.566 |
| Parents | | | | | | |
|
Father | Genotype | | | | | |
| |
AA | 63 (61.2) | 18 (62.1) | 1.000 | | |
| |
AC | 33 (32.0) | 10 (34.5) | 0.943 | 0.404-1.627 | 0.896 |
| |
CC | 7 (6.80) | 1 (3.40) | 2.000 | 0.156-3.867 | 0.522 |
| | Allele | | | | | |
| |
A | 158 (76.7) | 46 (79.3) | 1.000 | | |
| |
C | 48 (23.3) | 12 (20.7) | 1.133 | 0.517-1.533 | 0.731 |
| | Genetic model | | | | | |
| |
Dominant | 40 (38.8) | 11 (37.9) | 1.039 | 0.435-1.628 | 0.930 |
| |
Recessive | 96 (93.2) | 28 (96.6) | 0.490 | 0.087-2.928 | 0.504 |
|
Mother | Genotype | | | | | |
| |
AA | 104(68) | 25 (64.1) | 1.000 | | |
| |
AC | 44 (28.8) | 12 (30.8) | 0.881 | 0.437-1.512 | 0.749 |
| |
CC | 5 (3.30) | 2 (5.10) | 0.601 | 0.147-2.372 | 0.553 |
| | Allele | | | | | |
| |
A | 252 (82.4) | 62 (79.5) | 1.000 | | |
| |
C | 54 (17.6) | 16 (20.5) | 0.830 | 0.495-1.374 | 0.558 |
| | Genetic model | | | | | |
| |
Dominant | 49 (32.0) | 14 (35.9) | 0.841 | 0.444-1.469 | 0.646 |
| |
Recessive | 148 (96.7) | 37 (94.9) | 1.600 | 0.229-2.825 | 0.580 |
Polymorphism of the MTHFR gene in each
cleft type
Since the onset mechanism of each cleft type
differs, we compared the polymorphisms of the MTHFR gene in
the patients with cleft lip, those with cleft lip with palate, and
those with cleft palate only. Our analyses revealed that there were
no significant differences in the allele frequency or genotype
frequencies at either bp 677 or bp 1,298 of the MTHFR gene
(Tables II and III). The dominant or recessive genetic
model also did not reveal an association to each cleft type.
TDT
We investigated 28 families in which both parents
had heterozygous C677T polymorphism (677CT) and nine families with
heterozygous A1298C polymorphism (1298AC). No significant
transmission disequilibrium was revealed in 677CT or 1298AC by the
TDT results (Table IV).
 | Table IVResults of the transmission
disequilibrium test (TDT) of MTHFR C677T and A1298C
polymorphisms. |
Table IV
Results of the transmission
disequilibrium test (TDT) of MTHFR C677T and A1298C
polymorphisms.
| Allele | Transmitted | Not
transmitted | P-value |
|---|
| 677C | 33 | 23 | 0.181 |
| 677T | 23 | 33 | |
| 1298A | 8 | 10 | 0.637 |
| 1298C | 10 | 8 | |
Haplotype analysis
The haplotype analysis showed no linkage
disequilibrium between C677T and A1298C (Table V). The haplotype estimation
determined three types: C_A, T_A, and C_C. The frequency of
haplotypes was similar to those reported in the Japanese population
from the 1000 Genome Project: C_A, 44.2%; T_A, 38.0%; C_C, 17.8%;
T_C, not detected in the Japanese population (21). We detected a rare haplotype (T_C) in
one patient. No significant between-group differences were observed
except for the rare case of T_C (Table
V).
 | Table VHaplotype analysis results for
MTHFR 677 and 1,298 polymorphisms. |
Table V
Haplotype analysis results for
MTHFR 677 and 1,298 polymorphisms.
| Linkage
disequilibrium analysis |
|---|
| | C677T | A1298C | | | |
|---|
| C677T | - | D=-0.0663 | | | |
| | | D'=0.8814 | | | |
| | | r=-0.3428 | | | |
| A1298C | - | - | | | |
| Haplotype frequency
estimation (n=308) and association analysis |
| Haplotype | Total | Controls | Patients | OR (95% CI) | P-value |
| C_A | 0.4316 | 0.4412 | 0.4287 | 1.00 | |
| T_A | 0.3709 | 0.3529 | 0.3754 | 1.09
(0.71-1.070) | 0.69 |
| C_C | 0.1891 | 0.2059 | 0.1838 | 0.93
(0.55-1.57) | 0.79 |
| T_C | 0.0089 | 0 | 0.0121 | 38636069.94 | <0.0001
(38636069.93-38636069.95) |
Discussion
As one of the most common congenital abnormalities,
cleft lip with or without cleft palate (CL/P) is a multifactorial
genetic disorder that involves multiple genetic and environmental
factors. Folic acid deficiency in mothers causes developmental
defects in human fetuses and increases the risk of a malformed
fetus, and folic acid supplementation has been reported to prevent
the onset of cleft palate (6,7). Folic
acid is a member of the vitamin B family that is involved in the
synthesis of DNA, RNA, and amino acids. Folic acid is also involved
in the reaction in which homocysteine is methylated and converted
to methionine (8). In addition,
folic acid is thought to play important roles in organogenesis
(22).
Single-nucleotide polymorphisms of C677T and A1298C
in MTHFR were shown to change the serum folic acid
concentration (13). Genotype 677TT
or 1298CC would decrease the enzyme activity of MTHFR and
lower the production of 5-methyl tetrahydrofolic acid (5-methyl
THF). The 5-methyl THF regulates the methylation of homocysteine to
methionine as a coenzyme, and a decrease in 5-methyl THF disturbs
this process and increases the serum level of homocysteine.
Hyperhomocysteinemia is known to be involved in neural tube defects
by affecting neural crest cells. It is believed that in such a
scenario, mesenchymal cells derived from neural crest cells would
also be affected, thus ultimately resulting in CL/P (9,11,22). To
date, there have been no studies investigating MTHFR C677T
polymorphism in relation to cleft types in Japanese subjects. The
present study is the first to analyze MTHFR A1298C
polymorphism together with MTHFR C677T polymorphism in
Japanese patients with CL/P.
Contrary to our expectations, there was no
significant difference in A1298C or in C677T of the MTHFR
gene among the patients with any cleft type and the healthy control
subjects. In addition, there was no significant transmission
disequilibrium in either 677CT or 1298AC. The haplotype analysis
also revealed no significant difference. Tolarova and Harris
reported that MTHFR C677T polymorphism is involved in the
onset of CL/P, and Martinelli et al noted that they observed
no notable differences of MTHFR C677T polymorphism between
patient and parent groups, but they did observe marked differences
in the allele frequency between the mothers and the control group,
and the frequency of T allele was high (10,23). In
their study of mothers with low folic acid intake during pregnancy,
van Rooij et al reported that the onset of CL/P was
correlated with MTHFR C677T and A1298C polymorphisms
(24). However, Shaw et al
observed no correlations between C677T polymorphism and the
development of cleft lip or cleft lip and palate (11), and Kanno et al documented no
correlation between MTHFR C677T polymorphism and the
development of CL/P in a Japanese series (25). According to a study by Pezzetti et
al, MTHFR C677T polymorphism was correlated with the
development of cleft lip with or without cleft palate, while A1298C
polymorphism was not (4). With these
conflicting results, no conclusions can be drawn regarding the
relationship between the development of CL/P and MTHFR C677T
or A1298C polymorphisms.
During the years 2007 to 2020, there were 15
meta-analyses concerning MTHFR C677T and A1298C
polymorphisms and CL/P. Among them, 12 studies concerned C677T;
nine studies suggested an increased risk for CL/P (26-34),
whereas the other three studies denied the association (35-37).
Most studies have thus suggested that the C677T polymorphism is
likely to increase the risk for CL/P, which disagrees with our
findings. Regarding the A11298C polymorphism, there are seven
studies and six of them suggested no association with CL/P
(27,29,34,36,38,39),
which is consistent with our findings. There is a single study that
suggested an association between A1298C and CL/P (30). Most of the studies mentioned the
heterogeneity of the association due to the different ethnicities
of the subjects. They also noted that environmental factors such as
alcohol consumption, smoking habits, and maternal folic acid
supplementation are important (37,38,40).
According to the meta-analyses conducted to date, in Asians, C677T
T allele or recessive genotype TT tends to be a risk for CL/P.
Ethnic differences in the distribution of
MTHFR C677T and A1298C polymorphisms have been reported
(13,41). Yoshida reported that the distribution
of polymorphisms in Vietnamese and Mongolians differed from that in
other Asians (41), and there are
differences in distribution between our findings in Japanese and
the frequency of MTHFR C677T polymorphism in Vietnamese. We
also collected other cohorts by searching PubMed. We identified 21
matches reporting the prevalence of MTHFR C677T and A1298C
in various ethnic populations, and there were some differences in
allele frequencies. For example, genotype CC at bp 677 is likely to
be dominant in Moroccan patients (42) whereas genotype TT in 677 is dominant
in Chinese patients and Iranian patients (43,44).
Some ethnicities even showed higher frequencies of a functionally
superior genotype of MTHFR C677T and A1298C in the patient
groups, which is the opposite of our hypothesis. This discrepancy
may be due in part to the multiplicity of the enzymes, including
MTHFR, that regulate the serum level of folic acid. In
addition, it is known that folic acid nutritional supplementation
can overcome the decreased activity of, at least, MTHFR.
There is also a possibility that if the mother's folic acid serum
level is sufficient, the child may overcome the recessive
genotype.
Concerning the nutritional status of Japanese women,
it has been reported that although their daily intake of folic acid
is not sufficient, their serum concentrations are higher compared
to women in other countries due to the tendency of Japanese women's
dietary behavior during pregnancy (45). They tend to adopt healthy behaviors
such as eating more colored vegetables instead of meat, which
results in their consumption of folic acid as a highly bioavailable
natural food (46). In the earlier
study (45), even without a folic
acid-fortified diet, most of the subjects exhibited a folic acid
concentration that was sufficient to prevent neural tube
defects.
A few studies have investigated gene-environment
interactions; one study conducted in Caucasians demonstrated a
reduced effect of maternal folic acid supplementation on the
development of CL/P, although there was no association with C677T
genetic status (37). Although,
there have been no investigations of gene-environment interactions,
especially maternal folic acid supplementation, in Asian
populations including Japanese. The gene-environment interactions
in these populations remain to be elucidated in future studies.
It is possible that our present sample size was not
large enough to observe the association, and we therefore combined
the patients examined by Tohoku University in a previous Japanese
cohort with our present results in order to increase the sample
number (26). We observed no
significant difference in the allele frequencies or dominant
genetic model frequency (C vs. T, case n=411, control n=317, odds
ratio=0.954, 95% CI: 0.845-1.076, P-value=0.694; dominant model,
cases n=205, control n=162, odds ratio=0.984, 95% CI: 0.830-1.168,
P-value=0.926).
Concerning the meta-analysis data, C677T mutation
might be a risk for CL/P development in Asian population. However,
we could not observe such an association neither C677T nor A1298C
in the Japanese population. It is likely that MTHFR C677T
and A1298C polymorphisms have less impact on CL/P development in
Japanese populations. Part of the reason for this may be because of
the typical diet consumed by pregnant Japanese women, which may be
the reason that we did not observe significant differences in the
present case-control study. In this context, it is necessary to
investigate both serum levels of vitamins, other major
environmental factors including folic acid supplementation,
smoking, alcohol consumption, and genetic factors at the same time
points in order to determine whether decreased folic acid
metabolism and/or gene polymorphisms of metabolic enzymes are risk
factors for the development of CL/P.
Acknowledgements
We express our deepest gratitude to Dr Yutaka Imai
for encouraging us to conduct this study, and to Dr Kazumoto Kimura
of the Medical Information Center for his guidance concerning the
statistical analysis.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
CK and WY performed and analyzed the RFLP-PCR. YK
and CK interpreted the data and were the major contributors to the
manuscript's writing, and they contributed equally to this work. NN
and HK contributed to the presentation of the data and the
manuscript's revision. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by both the Clinical
Research Ethics Committee of Dokkyo University Hospital (approval
no. R-33-22J), and the Research Ethics Committee of Aichi-Gakuin
University School of Dentistry (approval no. 55). The consent of
the patients and controls for publication was obtained before their
participation in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cooper ME, Ratay JS and Marazita ML: Asian
oral-facial cleft birth prevalence. Cleft Palate Craniofac J.
43:580–589. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
2
|
Vieira AR: Genetic and environmental
factors in human cleft lip and palate. Front Oral Biol. 16:19–31.
2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Dixon MJ, Marazita ML, Beaty TH and Murray
JC: Cleft lip and palate: Understanding genetic and environmental
influences. Nat Rev Genet. 12:167–178. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Pezzetti F, Martineli M, Scapolo L,
Carinci F, Palmieri A, Marchesini J, Carinci P, Caramelli E, Rullo
R, Gombos F and Tognon M: Maternal MTHFR variant forms increase the
risk in offspring of isolated nonsyndromic cleft lip with or
without cleft palate. Hum Mutat. 24:104–105. 2004.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sato F: Candidate gene analysis of
non-syndromic cleft lip with or without cleft palate and isolated
cleft palate in Japanese families. Nihon Koku Geka Gakkai Zasshi.
46:1–8. 2000.(In Japanese).
|
|
6
|
Milunsky A, Jick H, Jick SS, Bruell CL,
MacLaughlin DS, Rothman KJ and Willett W: Multivitamin/folic acid
supplementation in early pregnancy reduces the prevalence of neural
tube defects. JAMA. 262:2847–2852. 1989.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Werler MM, Shapiro S and Mitchell AA:
Periconceptional folic acid exposure and risk of occurrent neural
tube defects. JAMA. 269:1257–1261. 1993.PubMed/NCBI
|
|
8
|
Bailey LB and Gregory JF III: Folate
metabolism and requirements. J Nutr. 129:779–782. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Niimi T: Experimental study on effects of
folic acid on cleft lip and/or palate, thymic anomalies and
cardiovascular anomalies. Aichi Gakuin Shigakkai Shi. 36:663–669.
1998.(In Japanese).
|
|
10
|
Tolarova M and Harris J: Reduced
recurrence of orofacial clefts after periconceptional
supplementation with high-dose folic acid and multivitamins.
Teratology. 51:71–78. 1995.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Shaw GM, Rozen R, Finnell RH, Todoroff K
and Lammer EJ: Infant C677T mutation in MTHFR, maternal
periconceptional vitamin use, and cleft lip. Am J Med Genet.
80:196–198. 1998.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Goyette P, Sumner JS, Milos R, Duncan AM,
Rosenblatt DS, Matthews RG and Rozen R: Human
methylenetetrahydrofolate reductase: Isolation of cDNA mapping and
mutation identification. Nat Genet. 7:195–200. 1994.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hiraoka M, Kato K, Saito Y, Yasuda K and
Kagawa Y: Gene-nutrient and gene-gene interactions of controlled
folate intake by Japanese women. Biochem Biophys Res Commun.
316:1210–1216. 2004.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tolarova M, Van Rooij I, Pastor M, van der
Put NMJ, Goldberg AC, Hol F, Capozzi A, Thomas CMG, Pastor L, Mosby
T, et al: A common mutation in the MTHFR gene is a risk factor for
nonsyndromic cleft lip and palate anomalies. Am J Hum Genet.
63(A27)1998.
|
|
15
|
Frosst P, Blom HJ, Milos R, Goyette P,
Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA,
van den Heuvel LP, et al: A candidate genetic risk factor for
vascular disease: A common mutation in methylenetetrahydrofolate
reductase. Nat Genet. 10:111–113. 1995.PubMed/NCBI View Article : Google Scholar
|
|
16
|
van der Put NM, Gabreëls F, Stevens EM,
Smeitink JA, Trijbels FJ, Eskes TK, van den Heuvel LP and Blom HJ:
A second common mutation in the methylenetetrahydrofolate reductase
gene: An additional risk factor for neural-tube defects? Am J Hum
Genet. 62:1044–1051. 1998.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Laird NM and Lange C: Family-based designs
in the age of large-scale gene-association studies. Nat Rev Genet.
7:385–394. 2006.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Solé X, Guinó E, Valls J, Iniesta R and
Moreno V: SNPStats: A web tool for the analysis of association
studies. Bioinformatics. 22:1928–1929. 2006.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Graffelman J: Exploring diallelic genetic
markers: The hardyweinberg package. J Stat Softw. 64:1–23.
2015.
|
|
20
|
R Core Team: R: A language and environment
for statistical computing. R Foundation for Statistical Computing,
Vienna, 2016. urihttps://www.R-project.org/simplehttps://www.R-project.org/.
|
|
21
|
The 1000 Genomes Project Consortium. Auton
A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, Marchini
JL, McCarthy S, McVean GA and Abecasis GR. A global reference for
human genetic variation. Nature. 526:68–74. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Selhub J and Rosenberg IH: Folic acid. In:
International Life Sciences Institute-Nutrition Foundation. Present
Knowledge in Nutrition. Ziegler EE and Filer LJ Jr (eds). 7th
edition. ILSI Press, International Life Sciences Institute
Nutrition Foundation, Washington, DC, pp206-219, 1996.
|
|
23
|
Martinelli M, Scapoli L, Pezzetti F,
Carinci F, Stabellini G, Bisceglia L, Gombos F and Tognon M: C677T
variant form at the MTHFR gene and CL/P: A risk factor for mothers?
Am J Med Genet. 98:357–360. 2001.PubMed/NCBI View Article : Google Scholar
|
|
24
|
van Rooij IA, Vermeij-Keers C, Kluijtmans
LA, Ocké MC, Zielhuis GA, Goorhuis-Brouwer SM, van der Biezen JJ,
Kuijpers-Jagtman AM and Steegers-Theunissen R: Does the interaction
between maternal folate intake and the methylenetetrahydrofolate
reductase polymorphisms affect the risk of cleft lip with or
without cleft palate? Am J Epidemiol. 157:583–591. 2003.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kanno K, Yamada A, Suzuki Y and Matsubara
Y: C677T Polymorphism at the MTHFR gene and cleft lip with/ without
cleft palate. J Jpn Soc Plast Reconst Surg. 21:690–694. 2001.
|
|
26
|
Amooee A, Dastgheib SA, Niktabar SM,
Noorishadkam M, Lookzadeh MH, Mirjalili SR, Heiranizadeh N and
Neamatzadeh H: Association of Fetal MTHFR 677C > T polymorphism
with non-syndromic cleft lip with or without palate risk: A
systematic review and meta-analysis. Fetal Pediatr Pathol: 1-17,
2019.
|
|
27
|
Pan X, Wang P, Yin X, Liu X, Li D, Li X,
Wang Y, Li H and Yu Z: Association between maternal MTHFR
polymorphisms and nonsyndromic cleft lip with or without cleft
palate in offspring, a meta-analysis based on 15 case-control
studies. Int J Fertil Steril. 8:463–480. 2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Luo YL, Cheng YL, Ye P, Wang W, Gao XH and
Chen Q: Association between MTHFR polymorphisms and orofacial
clefts risk: A meta-analysis. Birth Defects Res A Clin Mol Teratol.
94:237–244. 2012.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zhao M, Ren Y, Shen L, Zhang Y and Zhou B:
Association between MTHFR C677T and A1298C polymorphisms and NSCL/P
risk in Asians: A meta-analysis. PLoS One. 9(e88242)2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Pan Y, Zhang W, Ma J, Du Y, Li D, Cai Q,
Jiang H, Wang M, Zhang Z and Wang L: Infants'MTHFR polymorphisms
and nonsyndromic orofacial clefts susceptibility: A meta-analysis
based on 17 case-control studies. Am J Med Genet A. 58A:2162–2169.
2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Jiang C, Yin N, Zhao Z, Wu D, Wang Y, Li H
and Song T: Lack of association between MTHFR, MTR, MTRR, and TCN2
genes and nonsyndromic CL±P in a Chinese population: Case-control
study and meta-analysis. Cleft Palate Craniofac J. 52:579–587.
2015.PubMed/NCBI View
Article : Google Scholar
|
|
32
|
Verkleij-Hagoort A, Bliek J,
Sayed-Tabatabaei F, Ursem N, Steegers E and Steegers-Theunissen R:
Hyperhomocysteinemia and MTHFR polymorphisms in association with
orofacial clefts and congenital heart defects: A meta-analysis. Am
J Med Genet A. 143A:952–960. 2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Li Q, Xu L, Jia X, Saleem K, Zaib T, Sun W
and Fu S: SNPs in folate pathway are associated with the risk of
nonsyndromic cleft lip with or without cleft palate, a
meta-analysis. Biosci Rep. 40(BSR20194261)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Rai V: Strong association of C677T
polymorphism of methylenetetrahydrofolate reductase gene with
nonsyndromic cleft lip/palate (nsCL/P). Indian J Clin Biochem.
33:5–15. 2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Imani MM, Golchin N, Safaei M, Rezaei F,
Abbasi H, Sadeghi M, Lopez-Jornet P, Mozaffari HR and Sharifi R:
Methylenetetrahydrofolate reductase C677T polymorphism is not
associated with the risk of nonsyndromic cleft lip/palate: An
updated meta-analysis. Sci Rep. 10(1531)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Assis Machado R, de Toledo IP,
Martelli-Júnior H, Reis SR, Neves Silva Guerra E and Coletta RD:
Potential genetic markers for nonsyndromic oral clefts in the
Brazilian population: A systematic review and meta-analysis. Birth
Defects Res. 110:827–839. 2018.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Johnson CY and Little J: Folate intake,
markers of folate status and oral clefts: Is the evidence
converging? Int J Epidemiol. 37:1041–1058. 2008.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Niktabar SM, Aarafi H, Dastgheib SA,
Noorishadkam M, Mirjalili SR, Lookzadeh MH, Akbarian-Bafghi MJ,
Morovati-Sharifabad M and Neamatzadeh H: Association of MTHFR 1298A
> C polymorphism with susceptibility to non-syndromic cleft lip
with or without palate: A case-control study and meta-analysis.
Fetal Pediatr Pathol: Nov 4, 2019 (Epub ahead of print).
|
|
39
|
Imani MM, Rezaei F, Mire H, Delavarian M,
Sadeghi M, Safaei M and Mozaffari HR: A meta-analysis and
meta-regression of association between MTHFR A1298C polymorphism
and nonsyndromic cleft lip/palate risk: An evaluation based on five
genetic models. Int Orthod. 18:191–202. 2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Butali A, Little J, Chevrier C, Cordier S,
Steegers-Theunissen R, Jugessur A, Oladugba B and Mossey PA: Folic
acid supplementation use and the MTHFR C677T polymorphism in
orofacial clefts etiology: An individual participant data
pooled-analysis. Birth Defects Res A Clin Mol Teratol. 97:509–514.
2013.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Yoshida W: A study of
5,10-methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism
on cleft lip and/or palate in the Vietnamese. Aichi Gakuin J Dent
Sci. 43:421–437. 2005.(In Japanese).
|
|
42
|
Rafik A, Rachad L, Kone AS and Nadifi S:
MTHFR C677T polymorphism and risk of nonsyndromic cleft lip with or
without cleft palate in the Moroccan population. Appl Clin Genet.
12:51–54. 2019.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Wang W, Jiao XH, Wang XP, Sun XY and Dong
C: MTR, MTRR, MTHFR gene polymorphisms and susceptibility to
nonsyndromic cleft lip with or without cleft palate. Genet test Mol
Biomarkers. 20:297–303. 2016.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Ebadifar A, Ameli N, Khorramkhorshid HR,
Salehi Zeinabadi4 M, Kamali K and Khoshbakht T: Incidence
assessment of MTHFR C677T and A1298C polymorphisms in Iranian
nonsyndromic cleft lip and/or palate patients. J Dent Res Dent Clin
Dent Prospects. 9:101–104. 2015.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Mito N, Takimoto H, Umegaki K, Ishiwaki A,
Kusama K, Fukuoka H, Ohta S, Abe S, Yamawaki M, Ishida H and
Yoshiike N: Folate intakes and folate biomarker profiles of
pregnant Japanese women in the first trimester. Eur J Clin Nutr.
61:83–90. 2007.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Takimoto H, Yoshiike N, Katagiri A, Ishida
H and Abe S: Nutritional status of pregnant and lactating women in
Japan: A comparison with non-pregnant/non-lactating controls in the
national nutrition survey. J Obstet Gynaecol Res. 29:96–103.
2003.PubMed/NCBI View Article : Google Scholar
|