Introduction
Severe Acute Respiratory Syndrome-Coronavirus-2
(SARS-CoV-2) has been shown to increase the risk of thrombotic
events due to induction of a hypercoagulable state (1). Moreover, the virus enters type II
pneumocytes, vascular endothelial cells, and cortical neurons and
glia due to its ability to bind to the Angiotensin-Converting
Enzyme 2 (ACE-2) (2). ACE-2 is an
outer membrane enzyme that hydrolyzes angiotensin-II to
angiotensin, the latter of which has a vasodilatory effect
(3). During SARS-CoV-2 infection,
ACE-2 levels on the cell surface drop (2). Therefore, the vasodilatory effect of
ACE-2 products is reduced (4,5).
In the present report, the case of a 59-year-old
woman who was admitted to the emergency room (ER) of the ARNAS
‘Garibaldi’, in Catania, Italy, for dyspnea, was found to be
positive for SARS-CoV2 following a nasopharyngeal-swab, exhibited
COVID-19-induced pneumonia and developed a myocardial infarction
following admission, which was successfully treated with
percutaneous coronary intervention (PCI) is described (6,7).
Case report
A 59-year-old woman was referred to the ARNAS
‘Garibaldi’, in Catania, Italy, for dyspnea. The woman was affected
by hypertension that was controlled with angiotensin-II receptor
blockers and calcium channel blockers, as well as well-monitored
insulin-dependent diabetes and dyslipidemia. She entered lockdown
on March 10th, and never left her home since that day, but she was
visited by her son and grandson.
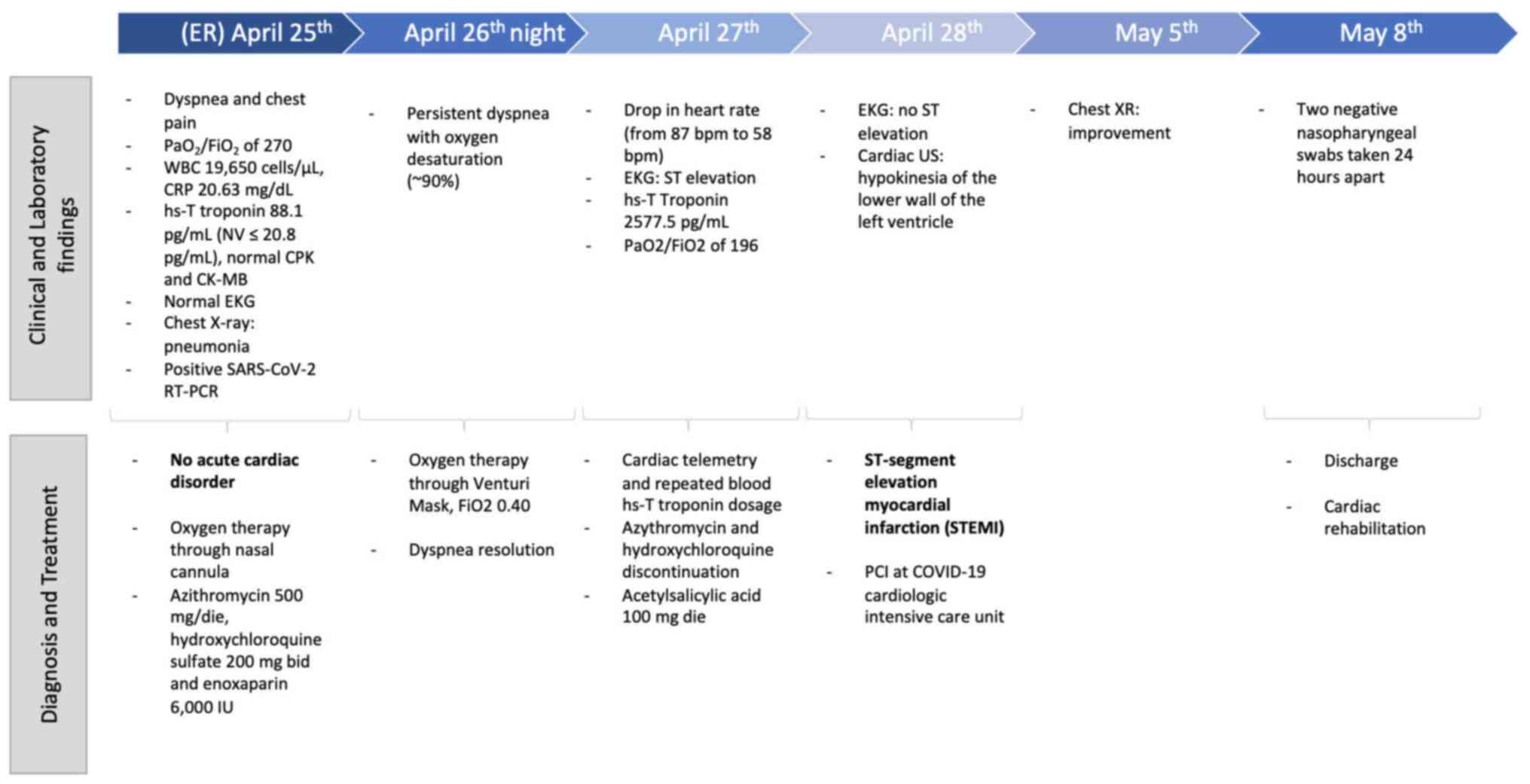
At the ER, she was put on oxygen therapy
administered through nasal cannula, for a
PaO2/FiO2 of 270 as shown by the arterial
blood gas (ABG) analysis. Her blood tests showed an increased white
blood cell count [19,650 cells/µl; normal value (NV), <11,000
cells/µl], with a normal differential, increased C reactive protein
levels (20.63 mg/dl; NV<0.05 mg/dl) and a slightly increased
high-sensitivity (hs)-T troponin level (88.1 pg/ml, NV≤20.8 pg/ml),
with normal creatine phosphokinase and creatine kinase MB levels.
She was assessed by a specialistic cardiologic consultant, which
reported no acute cardiac disorder. The chest X-ray showed right
medio-basal lung consolidation with a serious perivascular
interstitial thickening. Thorax CT scan was not performed, but a
nasopharyngeal swab for SARS-CoV-2 was performed, which provided a
positive result following a PCR test (Allplex 2019-nCoV assay). At
the ER anti-SARS-CoV-2 treatment, which included the standard of
care in Italy in that period (2020) (8), with azithromycin 500 mg once daily,
hydroxychloroquine sulfate 200 mg b.i.d and enoxaparin 6,000
international units (IU) was started. Corticosteroids treatment
were not administered at the beginning due to the patient's
diabetes (9), and there were no
other standardized therapeutic options at that time (10,11).
The patient was admitted to the COVID center. During
the first night, the patient showed persistent dyspnea with oxygen
desaturation (~90%) responding to oxygen therapy (Venturi Mask,
FiO2 0.40). The ABG analysis performed on the second day
of admission showed a PaO2/FiO2 of 196. An
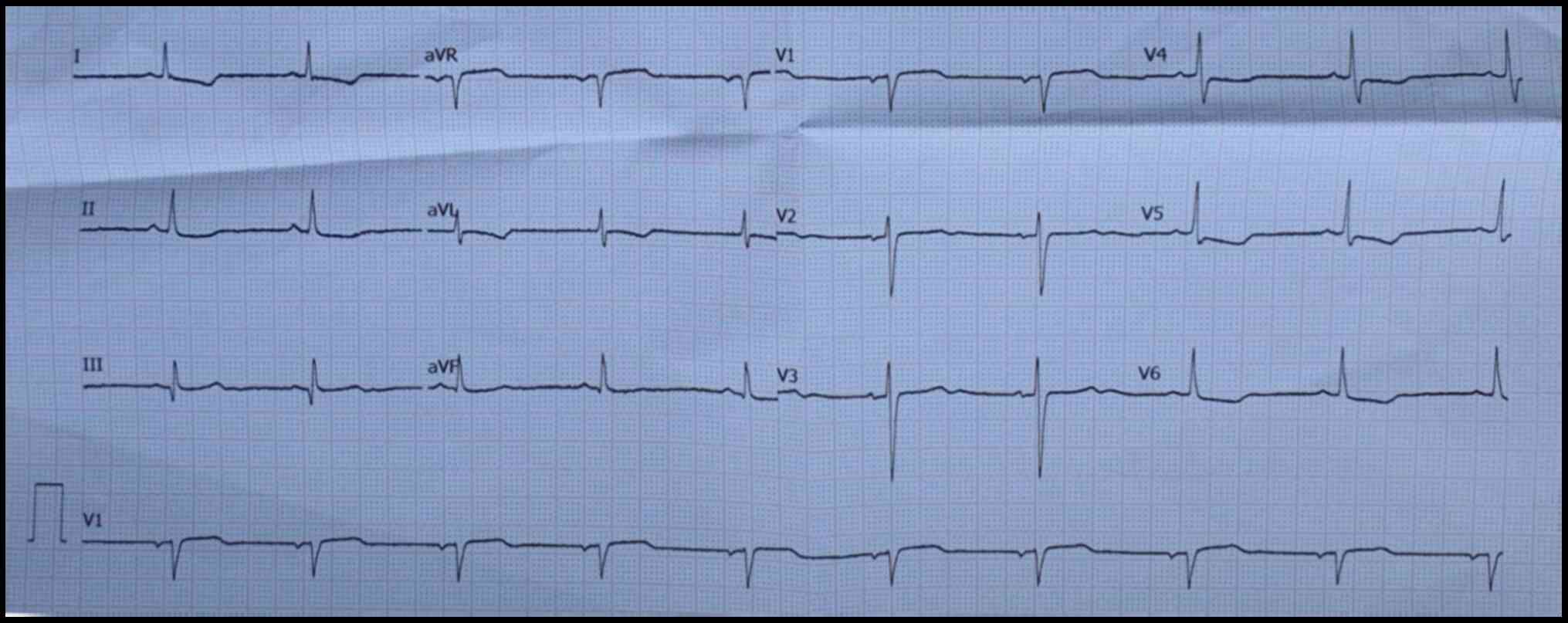
electrocardiogram (EKG) was performed due to a drop in her heart
rate (from 87 bpm, as stated by the cardiologic consultant, to 58
bpm), and the EKG showed ST elevation (Fig. 1). Hs-T Troponin levels were found to
be very high (2,577.5 pg/ml). Due to the difficulties linked to the
COVID-19 patients being under isolation, continuous monitoring of
her heart rhythm with cardiac telemetry and repeated blood hs-T
troponin dosage assessment was performed. Azythromycin and
hydroxychloroquine sulfate were stopped after only 3
administrations, and a treatment with acetylsalicylic acid 100 mg
once daily was then started. After 1 day of monitoring, a
specialistic cardiologic consultation with a cardiac ultrasound was
required. At the time of the specialistic consultation, the EKG did
not show an ST elevation anymore, but the cardiac US highlighted an
hypokinesia of the lower wall of the left ventricle, and an
ST-segment elevation myocardial infarction (STEMI) was diagnosed.
She was then transferred to the COVID-19 cardiologic intensive care
unit of the provincial COVID-net where she underwent a PCI. After
one week she came back to the Infectious Diseases ward of the ARNAS
‘Garibaldi’, in Catania, where she was considered to have recovered
from COVID-19 both clinically, as her chest XR showed an
improvement of both the consolidation and interstitial thickening,
and virologically, as two nasopharyngeal swabs taken 24 h apart
showed negative results, according to the current European
definition of recovery (10).
She was discharged on May 8th and is currently
undergoing cardiac rehabilitation (Fig.
2).
Discussion
The SARS-CoV-2 pandemic has proven to be more
clinically varied and challenging than what was initially
predicted. Dermatologic, neurologic and vascular manifestations
were found to frequently accompany the more noteworthy respiratory
syndrome.
Moreover, a hypercoagulable state and thrombotic
disorders were highlighted in certain patients. Asymptomatic
patients were considered fortuitous, and the only problem connected
with their infection was the increased spread of the infection.
However, there are now an increasing number of studies being
reported on asymptomatic patients showing pulmonary lesions
consistent with COVID-19-induced pneumonia (12,13).
Several studies have highlighted the
cardio-pathogenic potential of SARS-CoV-2. Myocardial inflammatory
involvement has been shown by Inciardi et al (7), whereas Loghin et al (14) reported on a 29-year-old patient with
a pseudo acute myocardial infarction. In addition, Chapman et
al (15) reviewed the use of
high-sensitivity cardiac troponin as a marker of severity of
COVID-19, highlighting how an increase in troponin is likely
multifactorial in patients with COVID-19.
It is has been shown that respiratory infections are
associated with cardiovascular events, particularly with coronary
syndromes, due to two primary mechanisms: Hypoxemia and a
proinflammatory state (16).
The former, caused by respiratory failure,
contributes to activation of the sympathetic system increasing
heart rate and cardiac contractility, and thus raising myocardial
oxygen demand; the latter of which is caused by the interaction
between the pathogen and the host immune system, and seems to
increase the inflammatory activity within the atheromatic plaque
contributing to its destabilization (17,18).
Moreover, inflammation promotes a prothrombotic state via several
molecular mechanisms (19,20).
Here, the case of a patient developing symptoms
after a non-datable infection with SARS-CoV-2, who therefore did
not undergo anticoagulant prophylaxis and developed ischemic heart
damage is described. The patient came to the ER complaining of
dyspnea and chest pain. She underwent a chest X-ray and ABG
analysis, after excluding an acute cardiac disorder from
differential diagnosis. She was therefore tested for SARS-CoV-2 and
found to be positive, and thus admitted to the COVID-hospital, and
after less than 24 h she showed signs of a myocardial infarction. A
limitation of the reported case is the lack of a thorax CT scan,
not performed by the ER, but this would have assisted in the dating
and staging of the SARS-CoV2 infection.
Furthermore, the patient's cardiac conditions
deteriorated considerably rapidly, thus there was insufficient time
to perform other imaging examinations or to administer specific
anti-inflammatory drugs, such as tocilizumab or anakinra, or
antiviral therapy, such as remdesivir along with baricitinib. In
addition, the patient's hyperglycemia limited the use of
corticosteroids.
Literature findings suggested that although patients
with SARS-CoV-2 infection may exhibit prolonged RNA shedding for up
to 83 days in the upper respiratory tract, no live virus was
isolated from culture beyond day 9 of symptoms, despite
persistently high viral RNA loads (15,21-24).
The patient cleared the virus within 2 weeks of admission. This
relatively quick clearance may be a sign of an old infection and
the STEMI represented a long COVID-19 vascular complication.
Currently, there are no quick and clinically
relevant methods to date an infection. Serology is still not
reliable if not for epidemiologic purposes (24) and PCR only highlights the presence
of small segments of viral RNA, not distinguishing between viable
and non-viable virus.
Stefanini et al (25) performed an observational study on a
small number of cases of STEMI in patients affected by COVID-19,
which, in 85.7% of their cases was the first manifestation of
COVID-19. They commented on their data stating that STEMI may be a
long-term sequela of COVID-19. The present case suggests that they
may have been correct in suspecting that the incidence of STEMI may
surge in the post-pandemic phase.
A particularity of the present case was the use of
cardiac telemetry (26). Continuous
monitoring with cardiac telemetry assisted the cardiologists in
understanding if their intervention was required, thus reducing the
risk for healthcare workers, whilst not delaying any
intervention.
In conclusion, the present case highlights the
association between respiratory infection and, in particular,
SARS-CoV2 infection, with cardiovascular diseases, especially with
Acute Coronary Syndrome, and the need for mass screening of
SARS-CoV-2 infection not only for acute presentations, but also for
long term complications to prevent potentially deadly consequences
if left unrecognized. Moreover, it also highlights the need for
novel diagnostic instruments able to distinguish between an old,
non-transmissible infection and a new one (27). The long-term effects of SARS-CoV-2
will continue to be assessed, even when the pandemic slows down,
due to its multifaceted complications, which are not completely
understood.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MC and AM contributed to drafting of the manuscript.
FC, VM and BMC performed the literature search. MG and RB collected
the data and assisted in drafting the case report section. MC, EVR,
GN and BSC critically revised the manuscript. All authors confirm
the authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Marino A, Pampaloni A, Scuderi D,
Cosentino F, Moscatt V, Ceccarelli M, Gussio M, Celesia BM, Bruno
R, Borraccino S, et al: High flow nasal cannula oxygenation and
tocilizumab administration in patients critically ill with COVID
19: A report of three cases and a literature review. World Acad Sci
J. 2:1. 2020.
|
|
2
|
Marino A, Cosentino F, Pampaloni A,
Scuderi D, Moscatt V, Gussio M, Onorante A, Zagami A, Torrisi S,
Grasso S, et al: Role of tocilizumab and high flow nasal cannula in
the clinical management of severe Covid 19. J Clin Trials.
10(427)2020.
|
|
3
|
Spiezia L, Boscolo A, Poletto F, Cerruti
L, Tiberio I, Campello E, Navalesi P and Simioni P:
COVID-19-Related Severe Hypercoagulability in Patients Admitted to
Intensive Care Unit for Acute Respiratory Failure. Thromb Haemost.
120:998–1000. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ceccarelli M, Berretta M, Venanzi Rullo E,
Nunnari G and Cacopardo B: Differences and similarities between
Severe Acute Respiratory Syndrome (SARS)-CoronaVirus (CoV) and
SARS-CoV-2. Would a rose by another name smell as sweet? Eur Rev
Med Pharmacol Sci. 24:2781–2783. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Setti L, Kirienko M, Dalto SC, Bonacina M
and Bombardieri E: FDG-PET/CT findings highly suspicious for
COVID-19 in an Italian case series of asymptomatic patients. Eur J
Nucl Med Mol Imaging. 47:1649–1656. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Aghagoli G, Gallo Marin B, Soliman LB and
Sellke FW: Cardiac involvement in COVID-19 patients: Risk factors,
predictors, and complications: A review. J Card Surg. 35:1302–1305.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Inciardi RM, Lupi L, Zaccone G, Italia L,
Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, et al:
Cardiac Involvement in a Patient With Coronavirus Disease 2019
(COVID-19). JAMA Cardiol. 5:819–824. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Katia F, Myriam DP, Ucciferri C, Auricchio
A, Di Nicola M, Marchioni M, Eleonora C, Emanuela S, Cipollone F
and Vecchiet J: Efficacy of canakinumab in mild or severe COVID-19
pneumonia. Immun Inflamm Dis. 9:399–405. 2021.PubMed/NCBI View
Article : Google Scholar
|
|
9
|
D'Ardes D, Pontolillo M, Esposito L,
Masciarelli M, Boccatonda A, Rossi I, Bucci M, Guagnano MT,
Ucciferri C, Santilli F, et al: Duration of COVID-19: Data from an
Italian Cohort and Potential Role for Steroids. Microorganisms.
8(1327)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ucciferri C, Vecchiet J and Falasca K:
Role of monoclonal antibody drugs in the treatment of COVID-19.
World J Clin Cases. 8:4280–4285. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Beigel JH: JH. What is the role of
remdesivir in patients with COVID-19? Curr Opin Crit Care.
27:487–492. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sadiq Z, Rana S, Mahfoud Z and Raoof A:
Systematic review and meta-analysis of chest radiograph (CXR)
findings in COVID-19. Clin Imaging. 80:229–238. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Pang C, Hou Q, Yang Z and Ren L: Chest
computed tomography as a primary tool in COVID-19 detection: An
update meta-analysis. Clin Transl Imaging. 9:341–351.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Loghin C, Chauhan S and Lawless SM:
Pseudo-Acute Myocardial Infarction in a Young COVID-19 Patient.
JACC Case Rep. 2:1284–1288. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chapman AR, Bularga A and Mills NL:
High-Sensitivity Cardiac Troponin Can Be an Ally in the Fight
Against COVID-19. Circulation. 141:1733–1735. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Musher DM, Abers MS and Corrales-Medina
VF: Acute Infection and Myocardial Infarction. N Engl J Med.
380:171–176. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Mihatov N, Januzzi JL Jr and Gaggin HK:
Type 2 myocardial infarction due to supply-demand mismatch. Trends
Cardiovasc Med. 27:408–417. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sandoval Y and Jaffe AS: Type 2 Myocardial
Infarction: JACC Review Topic of the Week. J Am Coll Cardiol.
73:1846–1860. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Schiavone M, Gobbi C, Biondi-Zoccai G,
D'Ascenzo F, Palazzuoli A, Gasperetti A, Mitacchione G, Viecca M,
Galli M, Fedele F, et al: Acute Coronary Syndromes and Covid-19:
Exploring the Uncertainties. J Clin Med. 9(1683)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Marino A, Munafò A, Zagami A, Ceccarelli
M, Di Mauro R, Cantarella G, Bernardini R, Nunnari G and Cacopardo
B: Ampicillin Plus Ceftriaxone Regimen against Enterococcus
faecalis Endocarditis: A Literature Review. J Clin Med.
10(4594)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cevik M, Tate M, Lloyd O, Maraolo AE,
Schafers J and Ho A: SARS-CoV-2, SARS-CoV, and MERS-CoV viral load
dynamics, duration of viral shedding, and infectiousness: A
systematic review and meta-analysis. Lancet Microbe. 2:e13–e22.
2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Yan D, Zhang X, Chen C, Jiang D, Liu X,
Zhou Y, Huang C, Zhou Y, Guan Z, Ding C, et al: Characteristics of
Viral Shedding Time in SARS-CoV-2 Infections: A Systematic Review
and Meta-Analysis. Front Public Health. 9(652842)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lo IL, Lio CF, Cheong HH, Lei CI, Cheong
TH, Zhong X, Tian Y and Sin NN: IL. Evaluation of SARS-CoV-2 RNA
shedding in clinical specimens and clinical characteristics of 10
patients with COVID-19 in Macau. Int J Biol Sci. 16:1698–1707.
2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zhou B, She J, Wang Y and Ma X: Duration
of Viral Shedding of Discharged Patients With Severe COVID-19. Clin
Infect Dis. 71:2240–2242. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Stefanini GG, Montorfano M, Trabattoni D,
Andreini D, Ferrante G, Ancona M, Metra M, Curello S, Maffeo D,
Pero G, et al: ST-Elevation Myocardial Infarction in Patients With
COVID-19: Clinical and Angiographic Outcomes. Circulation.
141:2113–2116. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Stoltzfus KB, Bhakta M, Shankweiler C,
Mount RR and Gibson C: Appropriate utilisation of cardiac telemetry
monitoring: A quality improvement project. BMJ Open Qual.
8(e000560)2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Campanella E, Marino A, Urso S, Insalaco
M, Emmanuele C, Uccello G, Cosentino F, Moscatt V, Ceccarelli M,
Caruso A, et al: The role of the SARS-COV 2 pandemic on the delay
of diagnosis in a case of multiple myeloma associated with AL
amyloidosis in HIV-HBV positive patient on antiretroviral
treatment. Eur J Mol Clin Med (Lond). 8:3564–3569. 2021.
|