Introduction
Obstructive sleep apnea (OSA) is a common disease in
humans. A review on population studies reported that OSA may be
found in both men and women with the highest prevalence rate of 37
and 50%, respectively (1). It is
also known that OSA is related to five major cardiovascular
diseases, including hypertension, heart failure, atrial
fibrillation, coronary artery disease and stroke (2-5).
A sleep cohort study, conducted in the USA, found that untreated
patients with severe sleep disordered breathing presented with
coronary artery disease or heart failure 2.6 times more often
compared with those without OSA (95% CI, 1.1-6.1) (6). The first line treatment for OSA is the
usage of a continuous positive airway pressure (CPAP) machine, as
it is cost effective with 15,915 USD per quality-adjusted life year
gained (7,8).
Other than the improvement in the quality of life,
CPAP therapy, for at least 4 h per night in patients with OSA,
reduces the risks of acute coronary artery disease or heart attack
by 83% (95% CI, 0.03-0.81) (9).
Despite the benefits of CPAP therapy, not all patients with OSA
purchase the machine for personal use. The CPAP purchasing rate in
patients with OSA varies between 33 and 77% (10,11).
There are several predictors for CPAP purchasing in patients with
OSA, such as income, socioeconomic status and health insurance
(9-11).
A study from Mexico (12) found
that patients with OSA and public health insurance had a 1.71 times
higher chance of purchasing a CPAP machine compared with those
without insurance (95% CI, 1.04-2.83), whereas other studies
reported that predictors for CPAP purchasing were age and OSA
severity (11,13). An increase in age, by one year,
showed a 7% higher chance of CPAP purchasing (13). Additionally, a previous study found
that marketing strategies may be valid predictors for CPAP
purchasing (10). Those who
purchased a CPAP machine preferred to have the option of several
CPAP models than those who did not purchase a CPAP machine (3.79
vs. 3.36/5 by Likert scale; P=0.092). As there are several and
inconsistent predictors of CPAP purchasing, the present study aimed
to summarize and identify predictors of CPAP purchasing using
meta-analysis. Furthermore, there is a lack of meta-analyses and
systematic reviews of predictors of CPAP purchasing in patients
with OSA in the literature.
Materials and methods
Study design
The present meta-analysis included factors
associated with the purchase of a CPAP machine in patients with
OSA. The types of studies conducted in adult patients with OSA
included: Randomized controlled trials, observational studies or
descriptive studies comparing factors between those who purchased
CPAP and those who did not. The diagnosis of OSA was made using
polysomnography upon evidence of an apnea-hypopnea index (AHI) or a
respiratory disturbance index (RDI) of five or more events/h. After
being diagnosed with OSA, CPAP trial or CPAP titration was
initiated either in a sleep laboratory or at home. CPAP titration
is performed with the aim of identifying the appropriate CPAP
pressure for each patient. A decision to purchase a CPAP machine is
made after CPAP titration. Studies conducted in adult patients with
OSA that had received CPAP titration either in a sleep laboratory
or at home were included.
Literature search and data
extraction
In the present meta-analysis, five databases were
searched: PubMed (https://pubmed.ncbi.nlm.nih.gov), Central database
(www.cochranelibrary.com/central), Scopus (www.scopus.com), CINAHL Plus (https://web.s.ebscohost.com/) and Web of Science
(www.webofknowledge.com). The search
terms used were ‘obstructive sleep apnea’, ‘sleep apnea syndrome’,
‘predict*’, ‘independent’, ‘factor*’,
‘variable*’, ‘purchase*’, ‘buy’, ‘bought’,
‘pay’, ‘paid’, ‘expend*’ and ‘spend*’, where
‘*’ was used to search for all terms which began with
the preceding letters. The full list of search terms is shown in
Table SI, Table SII, Table SIII, Table SIV and Table V. The final search was performed on
February 8, 2021. After the duplicates were removed, initial
screening was performed for non-relevant articles. Studies were
considered relevant if they had been conducted to evaluate
different factors between patients who purchased a CPAP machine and
those who did not. Data extraction and full text reports were
reviewed by two independent authors (BS and KS). Of these, the
articles that met the study criteria were included in the final
analysis (14).
Studied variables and outcomes
The studied variables included both marketing and
clinical factors. The definitions of the studied variables were as
follows: Average to high income determined in each study, which may
vary among countries; health insurance covering CPAP machine costs,
which indicated cost reimbursement by the insurer; and Epworth
Sleepiness Scale (ESS) score, which is a subjective sleepiness
evaluation method with a value range of 0-24(15). The primary outcome assessed were
factors that varied between patients who purchased a CPAP machine
and those who did not. At least two studies were required to
calculate the differences of the studied variables between the two
groups. The mean differences were calculated between the two groups
with a 95% CI for numerical factors and the odds ratio with 95% CI
for categorical outcomes. Heterogeneity was computed and reported
as I squared (I2). A forest plot of each comparison was
created based on I2. If I2 was ≤75%, fixed
effect was used. For factors displaying an I2 value of
>75%, the random effect was used.
Evaluation of the study quality
The Newcastle-Ottawa Scale, adapted for
cross-sectional studies, was used to evaluate the study quality of
observational studies (16). The
scale comprised three categories: Selection process, comparability
and outcome measurement, with a score of 5, 2 and 3 points,
respectively. The total score was 10 points and classified as very
good (9-10 points), good (7-8 points), satisfactory (5-6 points)
and non-satisfactory (0-4 points). Study quality was evaluated
independently by two authors (BS and CN). Disagreements between
these two authors were discussed and a final decision was made by a
third reviewer (KS). All analyses were performed using Review
Manager 5.4 (Copenhagen, The Nordic Cochrane Centre, The Cochrane
Collaboration, Denmark).
Results
Study inclusion
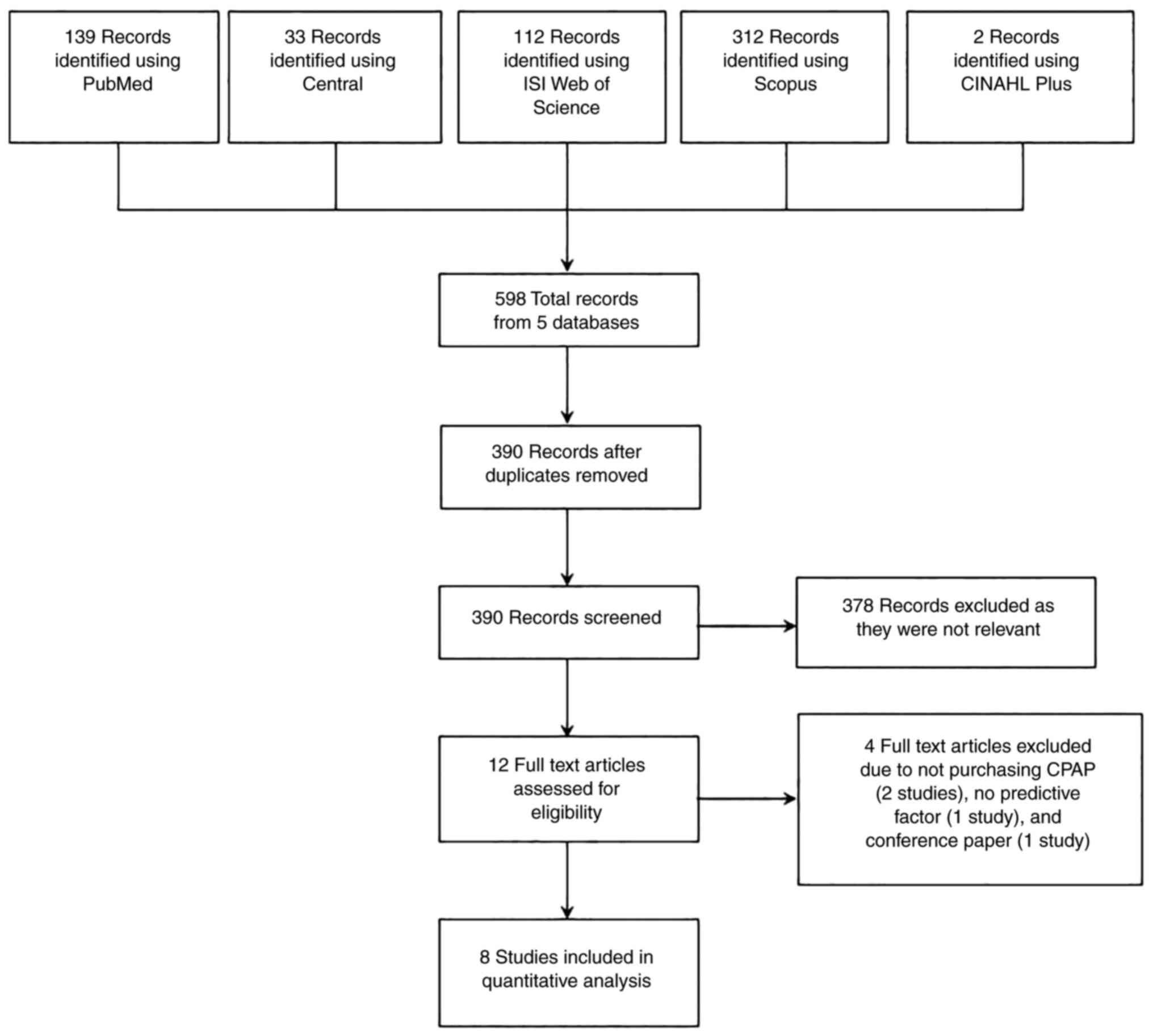
There were 598 articles from five databases, which
met the search criteria (Fig. 1).
After duplicate article removal, 390 articles were included in the
screening process. There were 12 articles found to be eligible for
full text evaluation. A total of four studies were excluded: Two
studies were excluded as CPAP compliance was evaluated, not
purchasing of CPAP machines; one study was excluded as the rate of
CPAP purchasing did not include variable evaluation; and one study
was excluded as only the abstract was available, which was from a
conference. In total, there were eight eligible studies involving
1,605 patients from four countries (6-10,17):
Five studies from Israel (11,16-20),
one from Mexico (12), one from
Poland (17) and one from Thailand
(10). The most recent study was
published in 2018 by Sawunyavisuth (10) from Thailand (Table I).
 | Table IEligible studies for meta-analysis of
patients who purchased a CPAP machine and those who did not. |
Table I
Eligible studies for meta-analysis of
patients who purchased a CPAP machine and those who did not.
| First author/s,
year | Country | Study design | Diagnosis of
OSA | Duration of CPAP
trial | Data | Total cases, n | Purchased, n
(%) | Did not purchase,n
(%) | (Refs.) |
|---|
| Torre Bouscoulet
et al, 2007 | Mexico | NA | AHI >5/h or
desaturation index >15/h | NA | Telephone
contact | 304 | 169 (55.6) | 135 (44.4) | (12) |
| Brin et al,
2005a | Israel |
Cross-sectional | RDI >20/h or RDI
<20/h with EDS and ESS >9 | 2 weeks | Self-administered
questionnaire | 400 | 128(32) | 272(68) | (18) |
| | | | | | | 183b |
128(70)b | 55(30)b | |
| Byśkiniewicz,
2006 | Poland | NA | NA | NA | NA | 184 | 116(63) | 68(37) | (17) |
| Sawunyavisuth,
2018 | Thailand |
Cross-sectional |
Polysomnography | 3 nights | Self-reported
questionnaire | 53 | 41 (77.36) | 12 (22.64) | (10) |
| Shahrabani et
al, 2014a | Israel | NA | NA | Varied | Phone
interview | 194 | 100(52) | 94(48) | (19) |
| Simon-Tuval et
al, 2009a | Israel |
Cross-sectional | NA | 2 weeks | Questionnaire | 162 | 65(40) | 97(60) | (13) |
| Tarasiuk et
al, 2012c,d | Israel | Longitudinal
interventional | AHI >30/h or
>15/h with ESS >10 | 2 weeks | Questionnaire,
telephone survey | 121 (control
group) | 40 (33.1) | 81 (66.9) | (11) |
| | | | (moderate to
severe) | | | 137 (incentive
group) | 65 (47.4) | 72 (52.6) | |
| Tzischinsky et
al, 2011 | Israel | NA | NA | NA | Questionnaire,
telephone interview | 50 | 24(48) | 26(52) | (20) |
Details of the included studies
The most common study design was cross-sectional and
was used in three of the studies (10,13,18).
The diagnosis of OSA was made using polysomnography; however, the
inclusion criteria for OSA were variable, with the highest AHI of
30 events/h (11). The duration of
CPAP titration or trial, prior to CPAP purchase, was a maximum of 2
weeks (11,13,18).
Not all patients with OSA, in three of the studies, underwent CPAP
titration [Brin et al (18),
183/400 patients; Shahrabani et al (19), 150/194 patients; Simon-Tuval et
al (13), 132/162 patients]. In
these three studies, data for analysis were obtained from the total
population in the study. Most studies used self-administered
questionnaires or telephone interviews to record patient
information. The numbers of participating patients varied between
50(20) and 400(18), with an average CPAP purchasing rate
of 49.8%. Only one study evaluated marketing strategies on CPAP
purchasing (10).
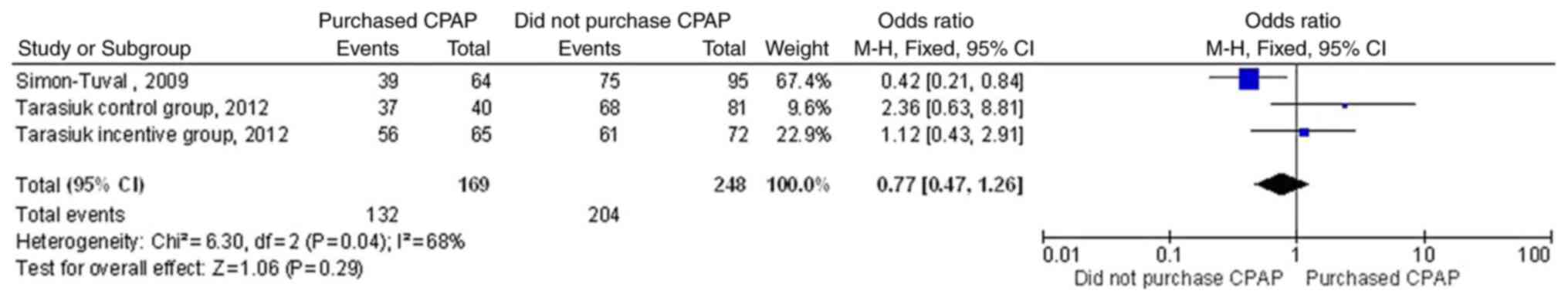
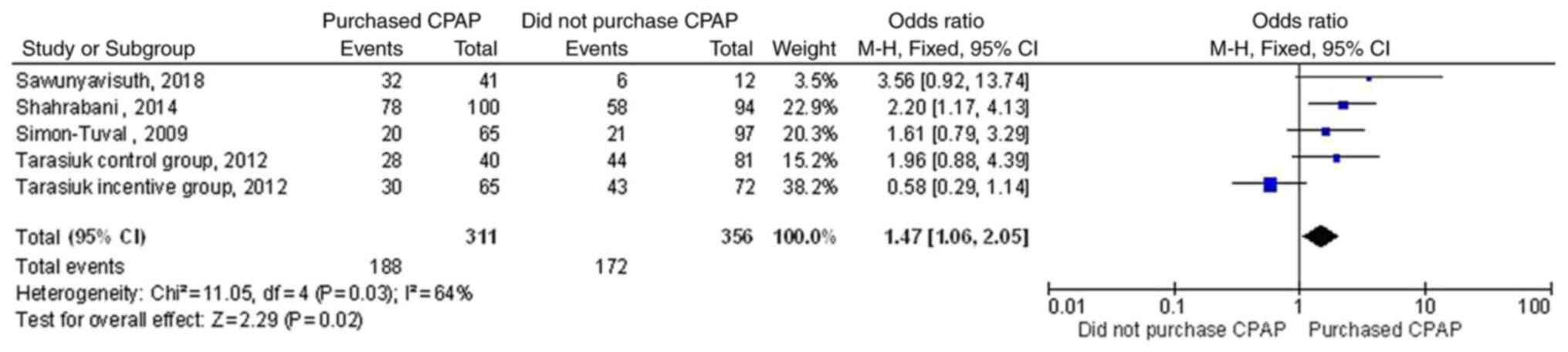
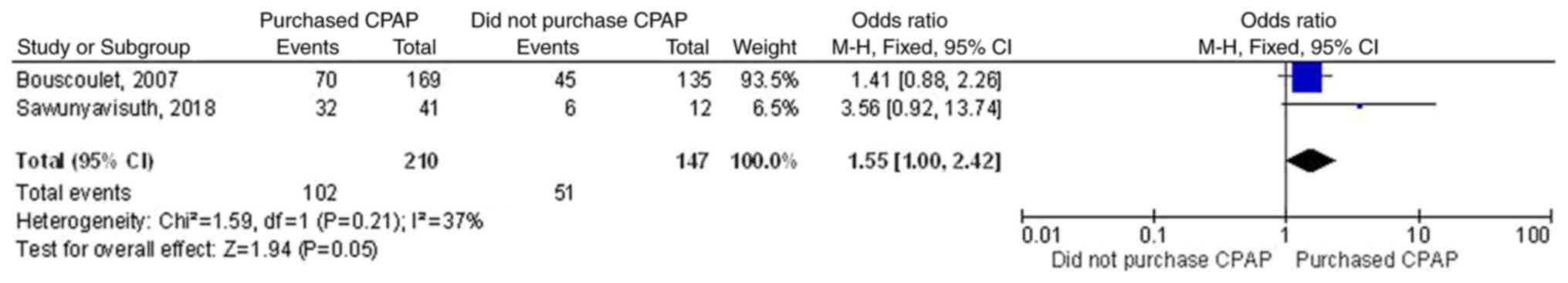
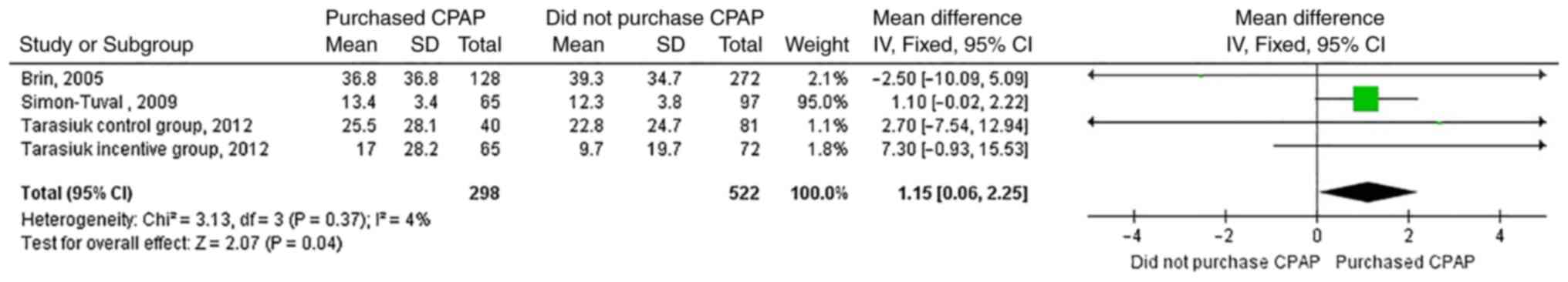
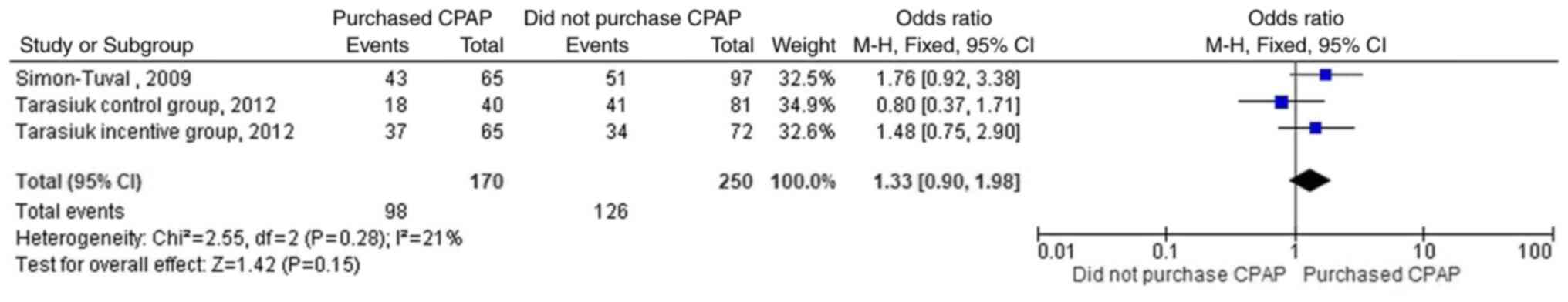
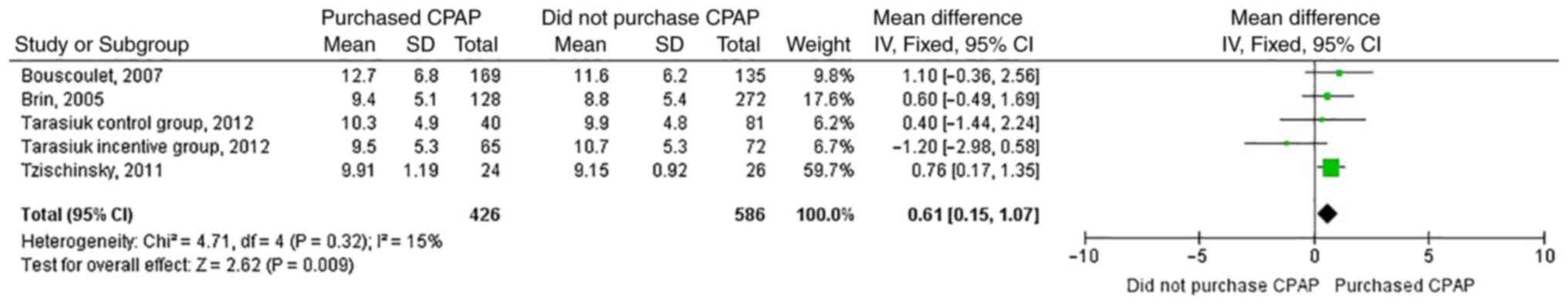
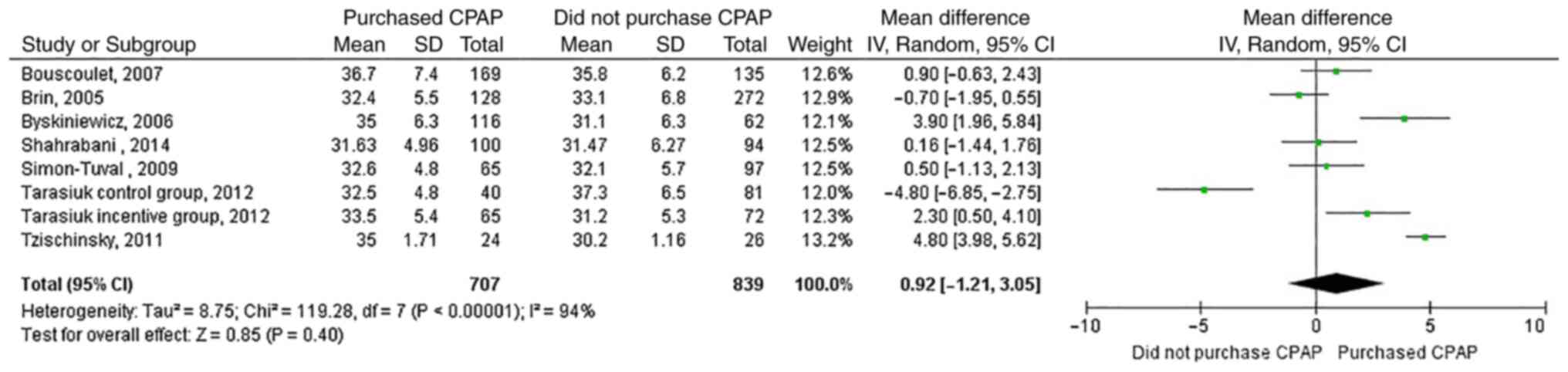
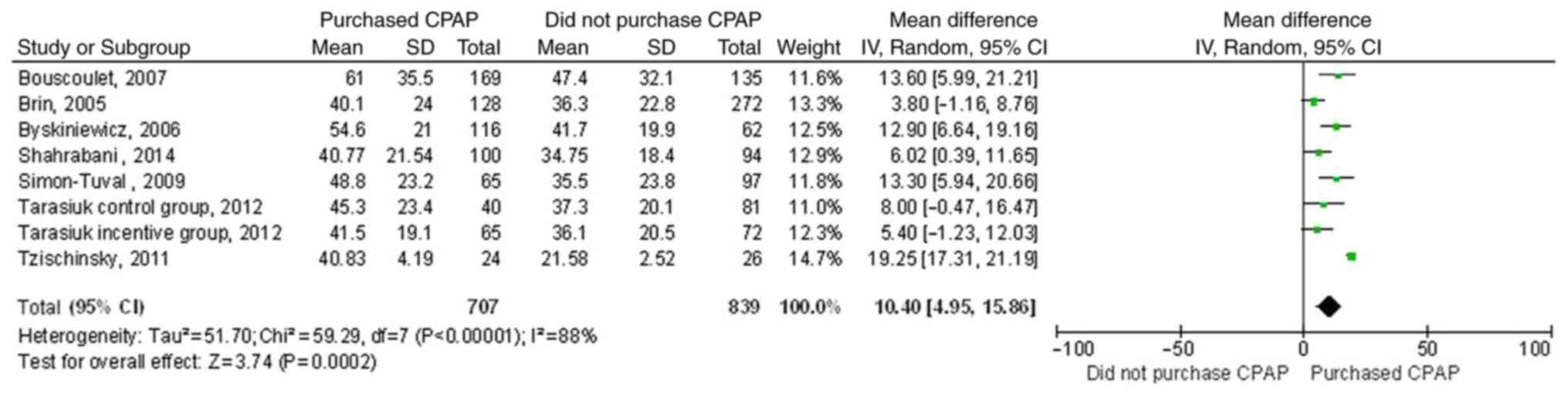
Study outcomes
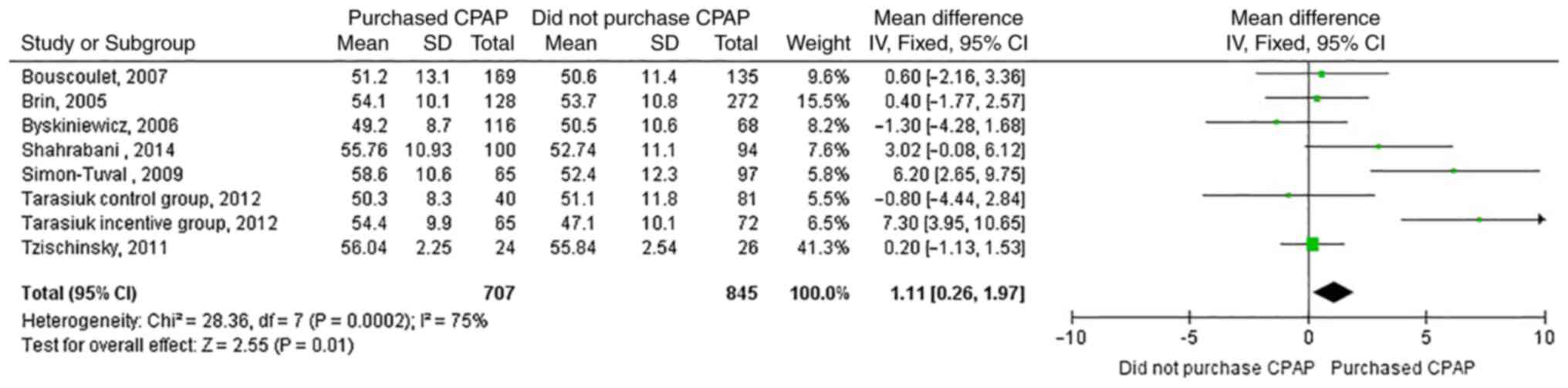
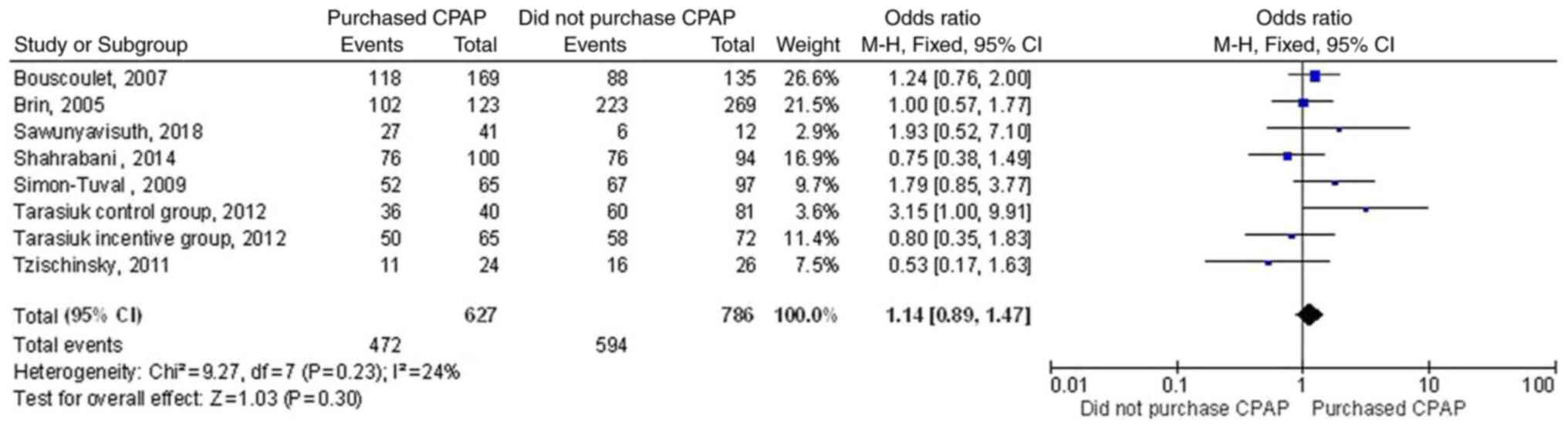
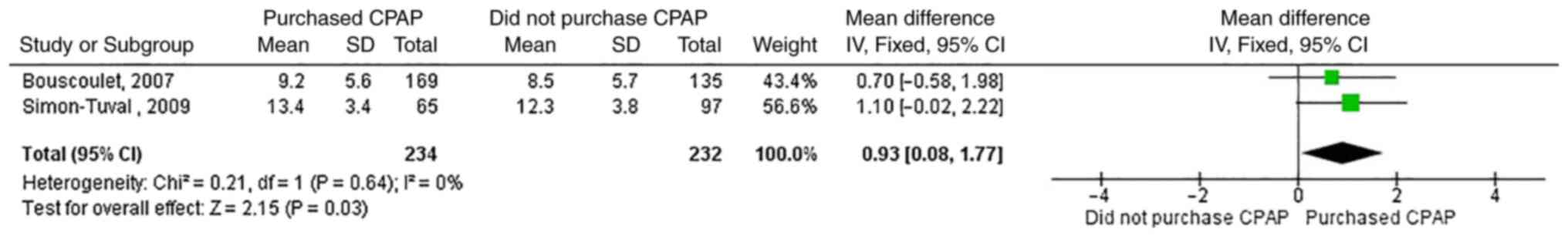
There were 11 variables available for comparison
between patients who purchased a CPAP machine and those who did not
(Fig. 2, Fig. 3, Fig.
4, Fig. 5, Fig. 6, Fig.
7, Fig. 8, Fig. 9, Fig.
10, Fig. 11 and Fig. 12). These factors were age (Fig. 2), sex (Fig. 3), years of education (Fig. 4), living with a partner (Fig. 5), income (Fig. 6), insurance (Fig. 7), smoking (Fig. 8), hypertension/cardiovascular
disease (Fig. 9), ESS (Fig. 10), body mass index (Fig. 11) and AHI/RDI (Fig. 12). A total of six factors were
found to be significantly different between both groups: Age
(Fig. 2), years of education
(Fig. 4), income (Fig. 6), smoking (Fig. 8), ESS (Fig. 10) and AHI/RDI (Fig. 12). AHI/RDI was significantly
different between the two groups with the highest mean difference
of 10.40 events/h (95% CI, 4.95-15.86) as shown in Fig. 12. Patients who purchased a CPAP
machine were older (by 1.11 years), had more years of education
(0.93 years more), were smoking more (by 1.15 pack/year), and had
higher ESS (by 0.61) and AHI/RDI (by 10.40) scores than those who
did not purchase a CPAP machine, as shown in Figs. 2, 4,
8, 10 and 12, respectively. Additionally, those who
purchased a CPAP machine had a 1.47 times higher income than those
who did not (Fig. 6). The quality
of most of the studies was evaluated as satisfactory, except for
the longitudinal study by Tarasiuk et al (11), which was considered as good, with a
score of 7/10 (Table II).
Furthermore, the study by Byśkiniewicz (17) was not scored as it was published in
Polish.
 | Table IIStudy quality evaluation using the
Newcastle-Ottawa Scale adapted for cross-sectional studies of the
included studies. |
Table II
Study quality evaluation using the
Newcastle-Ottawa Scale adapted for cross-sectional studies of the
included studies.
| First author/s,
year | Study design | Selection process
(5) | Comparability
(2) | Outcome measures
(3) | Total (10) | Interpretation | (Refs.) |
|---|
| Torre Bouscoulet
et al, 2007 | NA | 3 | 1 | 1 | 5 | Satisfactory | (12) |
| Brin et al,
2005 |
Cross-sectional | 3 | 1 | 1 | 5 | Satisfactory | (18) |
| Byśkiniewicz,
2006 | NA | NA | NA | NA | NA | NA due to
non-English article | (17) |
| Sawunyavisuth,
2018 |
Cross-sectional | 3 | 1 | 2 | 6 | Satisfactory | (10) |
| Shahrabani et
al, 2014 | NA | 3 | 1 | 2 | 6 | Satisfactory | (19) |
| Simon-Tuval et
al, 2009 |
Cross-sectional | 3 | 1 | 2 | 6 | Satisfactory | (13) |
| Tarasiuk et
al, 2012 | Longitudinal | 4 | 1 | 2 | 7 | Good | (11) |
| Tzischinsky et
al, 2011 | NA | 3 | 1 | 2 | 6 | Satisfactory | (20) |
Discussion
The six significant factors that were compared
between patients with OSA who did or did not purchase a CPAP
machine can be categorized into two groups: Customer-related and
clinical factors. The personal customer factors included age, years
of education and income, while the clinical factors were age,
smoking, ESS and AHI/RDI. In addition, age was included in both
groups as it can be classified as both a personal customer factor
and clinical factor.
There are several customer behavior models, such as
the Nicosia model, Howard Sheth model, or Engel, Blackwell and
Minard model (21,22). The significant factors in the
present study are personal customer factors, which is one factor of
several customer behaviors in the black box consumer behavior model
(23). Additionally, a previous
study from China found that these personal factors are related to
higher chances of purchasing healthcare devices; however, the
purchase of a CPAP machine was not included in the study (24). Patients with OSA who purchased a
CPAP machine were 1.11 years older, had 0.93 years longer education
and, on average, a 1.47 times higher income than those who did not
purchase a CPAP machine. The previous Chinese study found that
older age, higher education (Junior college degree) and higher
income had odds ratios of 6.65, 4.02 and 7.88, respectively
(24). Both studies identified
similar trends for these predictors, but different magnitudes as
this study was more specific to the use of CPAP machines by
summation of several studies. Furthermore, differences in defining
what constitutes high income among countries and currency
differences require a cautious interpretation of CPAP purchase. Of
note, the present meta-analysis indicated that patients with OSA
and health insurance coverage had a 1.55 times higher chance of
purchasing a CPAP machine than those without such coverage (95% CI,
1.00-2.42), as shown in Fig. 7. It
should be noted that insurance almost reached statistical
significance in the present study. The aforementioned coverage
reduces the machine's cost, making it more affordable.
The four clinical factors, which were found to
change significantly between the two groups, were related to
severity of OSA. Older age, smoking and daytime sleepiness are
indicators of severe OSA (25-27).
Older age has been reported to be related to increased severity of
OSA, with a correlation coefficient of 0.331 (P<0.01) (25), whereas smoking was associated with
moderate/severe OSA by 4.4 times (95% CI, 1.5-13) (26). A high ESS score of >10 was found
more often in severe OSA, as compared with mild or moderate OSA
(40.2 vs. 26.7 and 29.6%, respectively; P<0.001) (27). As a result, more patients with more
severe OSA tended to purchase a CPAP machine more often than those
with less severe OSA. In the present study, patients with OSA who
purchased a CPAP machine had a higher AHI by 10.40 events/h than
those who did not purchase a CPAP machine (Fig. 12). Of note, this AHI/RDI mean
difference displayed the highest value among the studied variables.
As previously reported, patients with severe OSA had higher chances
of sudden death or developing cardiovascular diseases, including
coronary artery heart disease, heart failure, left ventricular
hypertrophy, hypertension or atrial fibrillation (28-30).
Those patients with OSA with an AHI score of >20 events/h are
likely to have sudden cardiac death (29). Therefore, patients with severe OSA
may have several cardiovascular diseases, as well as being more
symptomatic, leading to higher chances of purchasing a CPAP
machine.
There are some limitations in the present study.
First, most studies conducted in Israel may have different cultures
or purchasing habits from other countries. Second, some patients
did not undergo a CPAP trial prior to CPAP purchase (8-10).
In addition, the duration of a CPAP titration prior to a decision
of purchasing a CPAP machine varied (Table I). Third, some studied variables,
such as body mass index and AHI, bore high heterogeneity. Fourth,
CPAP compliance or other related conditions of OSA such as CPAP
intervention, exercise intervention, cognitive function, or asthma
were not studied (31-38).
Finally, marketing strategies which may be related to CPAP purchase
were investigated in only one study (10). Therefore, further studies regarding
the roles of marketing strategies in CPAP purchase may be
required.
In conclusion, personal customer factors and
clinical factors were related to the decision of patients with OSA
to purchase a CPAP device.
Supplementary Material
Search strategy for PubMed (retrieved
on February 7, 2021).
Search strategy for Central (retrieved
on February 7, 2021).
Search strategy for ISI Web of science
(retrieved on February 7, 2021).
Search strategy for Scopus (retrieved
on February 8, 2021).
Search strategy for CINAHL Plus
(retrieved on February 8, 2021).
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by the Research and
International Affair, Faculty of Medicine (grant no. SY65101), Khon
Kaen University, Khon Kaen, Thailand.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BS designed the study, extracted the data, evaluated
study quality, performed the statistical analysis, interpreted
data, and wrote the manuscript. CN performed the searches,
evaluated study quality, performed the statistical analysis,
interpreted the data, and reviewed the manuscript. KS evaluated
study quality, performed the statistical analysis, interpreted the
data, and reviewed the manuscript. BS and KS confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Franklin KA and Lindberg E: Obstructive
sleep apnea is a common disorder in the population-a review on the
epidemiology of sleep apnea. J Thorac Dis. 7:1311–1322.
2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Piepoli MF, Hoes AW, Agewall S, Albus C,
Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, et
al: 2016 European guidelines on cardiovascular disease prevention
in clinical practice: The sixth joint task force of the European
society of cardiology and other societies on cardiovascular disease
prevention in clinical practice (constituted by representatives of
10 societies and by invited experts) developed with the special
contribution of the European association for cardiovascular
prevention & rehabilitation (EACPR). Eur Heart J. 37:2315–2381.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Khamsai S, Chootrakool A, Limpawattana P,
Chindaprasirt J, Sukeepaisarnjaroen W, Chotmongkol V, Silaruks S,
Senthong V, Sittichanbuncha Y, Sawunyavisuth B and Sawanyawisuth K:
Hypertensive crisis in patients with obstructive sleep
apnea-induced hypertension. BMC Cardiovasc Disord.
21(310)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Khamsai S, Mahawarakorn P, Limpawattana P,
Chindaprasirt J, Sukeepaisarnjaroen W, Silaruks S, Senthong V,
Sawunyavisuth B and Sawanyawisuth K: Prevalence and factors
correlated with hypertension secondary from obstructive sleep
apnea. Multidiscip Respir Med. 16(777)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Khamsai S, Kachenchart S, Sawunyavisuth B,
Limpawattana P, Chindaprasirt J, Senthong V, Chotmongkol V,
Pongkulkiat P and Sawanyawisuth K: Prevalence and risk factors of
obstructive sleep apnea in hypertensive emergency. J Emerg Trauma
Shock. 14:104–107. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hla KM, Young T, Hagen EW, Stein JH, Finn
LA, Nieto FJ and Peppard PE: Coronary heart disease incidence in
sleep disordered breathing: The Wisconsin sleep cohort study.
Sleep. 38:677–684. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Pietzsch JB, Garner A, Cipriano LE and
Linehan JH: An integrated health-economic analysis of diagnostic
and therapeutic strategies in the treatment of moderate-to-severe
obstructive sleep apnea. Sleep. 34:695–709. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tietjens JR, Claman D, Kezirian EJ, De
Marco T, Mirzayan A, Sadroonri B, Goldberg AN, Long C, Gerstenfeld
EP and Yeghiazarians Y: Obstructive sleep apnea in cardiovascular
disease: A review of the literature and proposed multidisciplinary
clinical management strategy. J Am Heart Assoc.
8(e010440)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Peker Y, Thunström E, Glantz H and
Eulenburg C: Effect of obstructive sleep apnea and CPAP treatment
on cardiovascular outcomes in acute coronary syndrome in the
RICCADSA trial. J Clin Med. 9(4051)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sawunyavisuth B: What are predictors for a
continuous positive airway pressure machine purchasing in
obstructive sleep apnea patients? Asia Pac J Sci Technol.
23(APST-23-03-10)2018.
|
|
11
|
Tarasiuk A, Reznor G, Greenberg-Dotan S
and Reuveni H: Financial incentive increases CPAP acceptance in
patients from low socioeconomic background. PLoS One.
7(e33178)2012.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Torre Bouscoulet L, López Escárcega E,
Castorena Maldonado A, Vázquez García JC, Meza Vargas MS and
Pérez-Padilla R: Continuous positive airway pressure used by adults
with obstructive sleep apneas after prescription in a public
referral hospital in Mexico City. Arch Bronconeumol. 43:16–21.
2007.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
13
|
Simon-Tuval T, Reuveni H, Greenberg-Dotan
S, Oksenberg A, Tal A and Tarasiuk A: Low socioeconomic status is a
risk factor for CPAP acceptance among adult OSAS patients requiring
treatment. Sleep. 32:545–552. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10(ED000142)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Johns MW: A new method for measuring
daytime sleepiness: The Epworth sleepiness scale. Sleep.
14:540–545. 1991.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Sisay M, Mengistu G and Edessa D:
Epidemiology of self-medication in Ethiopia: A systematic review
and meta-analysis of observational studies. BMC Pharmacol Toxicol.
19(56)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Byśkiniewicz K: Factors determining the
decision to initiate nCPAP therapy in patients with obstructive
sleep apnea (OSA). Pneumonol Alergol Pol. 74:45–50. 2006.PubMed/NCBI(In Polish).
|
|
18
|
Brin YS, Reuveni H, Greenberg S, Tal A and
Tarasiuk A: Determinants affecting initiation of continuous
positive airway pressure treatment. Isr Med Assoc J. 7:13–18.
2005.PubMed/NCBI
|
|
19
|
Shahrabani S, Tzischinsky O, Givati G and
Dagan Y: Factors affecting the intention and decision to be treated
for obstructive sleep apnea disorder. Sleep Breath. 18:857–868.
2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tzischinsky O, Shahrabani S and Peled R:
Factors affecting the decision to be treated with continuous
positive airway pressure for obstructive sleep apnea syndrome. Isr
Med Assoc J. 13:413–419. 2011.PubMed/NCBI
|
|
21
|
Goodhope O and Pcon A: Major classic
consumer buying behaviour models: Implications for marketing
decision-making. J Econ Sustain Dev. 4:164–172. 2013.
|
|
22
|
Waykole NH and Bhangale AI: A study of
influence of digital marketing on buying behaviour of mobile phone
consumers. J Inf Comput Sci. 10:411–429. 2020.
|
|
23
|
Schlesinger M, Kanouse DE, Martino SC,
Shaller D and Rybowski L: Complexity, public reporting, and choice
of doctors: A look inside the blackest box of consumer behavior.
Med Care Res Rev. 71 (Suppl 5):38S–64S. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Wang D, Liu S, Wu J and Lin Q: Purchase
and use of home healthcare devices for the elderly: A pilot study
in Shanghai, China. BMC Public Health. 20(615)2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Hongyo K, Ito N, Yamamoto K, Yasunobe Y,
Takeda M, Oguro R, Takami Y, Takeya Y, Sugimoto K and Rakugi H:
Factors associated with the severity of obstructive sleep apnea in
older adults. Geriatr Gerontol Int. 17:614–621. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Krishnan V, Dixon-Williams S and Thornton
JD: Where there is smoke…there is sleep apnea: Exploring the
relationship between smoking and sleep apnea. Chest. 146:1673–1680.
2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kapur VK, Baldwin CM, Resnick HE, Gottlieb
DJ and Nieto FJ: Sleepiness in patients with moderate to severe
sleep-disordered breathing. Sleep. 28:472–477. 2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Soontornrungsun B, Khamsai S,
Sawunyavisuth B, Limpawattana P, Chindaprasirt J, Senthong V,
Chotmongkol V and Sawanyawisuth K: Obstructive sleep apnea in
patients with diabetes less than 40 years of age. Diabetes Metab
Syndr. 14:1859–1863. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Gami AS, Olson EJ, Shen WK, Wright RS,
Ballman KV, Hodge DO, Herges RM, Howard DE and Somers VK:
Obstructive sleep apnea and the risk of sudden cardiac death: A
longitudinal study of 10,701 adults. J Am Coll Cardiol. 62:610–616.
2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sanlung T, Sawanyawisuth K, Silaruks S,
Khamsai S, Limpawattana P, Chindaprasirt J, Senthong V, Kongbunkiat
K, Timinkul A, Phitsanuwong C, Sawunyavisuth B and Chattakul P:
Clinical characteristics and complications of obstructive sleep
apnea in srinagarind hospital. J Med Assoc Thai. 103(36)2020.
|
|
31
|
Sawunyavisuth B: What personal experiences
of CPAP use affect CPAP adherence and duration of CPAP use in OSA
patients? J Med Assoc Thai. 101:S245–S249. 2018.
|
|
32
|
Kaewkes C, Sawanyawisuth K and
Sawunyavisuth B: Are symptoms of obstructive sleep apnoea related
to good continuous positive airway pressure compliance? ERJ Open
Res. 6:00169–2019. 2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Jeerasuwannakul B, Sawunyavisuth B,
Khamsai S and Sawanyawisuth K: Prevalence and risk factors of
proteinuria in patients with type 2 diabetes mellitus. Asia Pac J
Sci Technol. 26(APST-26-04-02)2021.
|
|
34
|
Leethong-in M, Piyawattanapong S,
Sommongkol S, Thiengtham S, Subindee S, Komniyom N, Chotchaisthit P
and Chuen-arom C: The impact of a brain exercise program on
cognitive functions among rural thai older adults: A
quasi-experimental study. Asia Pac J Sci Technol.
26(APST-26-02-08)2021.
|
|
35
|
Sangjumrus N, Chaiear N, Saikaew K,
So-ngern A and Burge PS: Developing a web application to provide
information on common work-related asthma causative agents. Asia
Pac J Sci Technol. 26(APST-26-04-13)2021.
|
|
36
|
Sawunyavisuth B, Ngamjarus C and
Sawanyawisuth K: Any effective intervention to improve CPAP
adherence in children with obstructive sleep apnea: A systematic
review. Glob Pediatr Health. 8(2333794X211019884)2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Hlaing SS, Puntumetakul R, Wanpen S and
Saiklang P: Updates on core stabilization exercise and
strengthening exercise: A review article. Asia Pac J Sci Technol.
26(APST-26-04-12)2021.
|
|
38
|
Manasirisuk P, Chainirun N, Tiamkao S,
Lertsinudom S, Phunikhom K, Sawunyavisuth B and Sawanyawisuth K:
Efficacy of generic atorvastatin in a real-world setting. Clin
Pharmacol. 13:45–51. 2021.PubMed/NCBI View Article : Google Scholar
|