Introduction
Coronavirus disease 2019 (COVID-19) continues to be
a worldwide health problem, and the number of reported cases in
Indonesia continues to increase. In Indonesia, an upsurge in
COVID-19 cases was documented from May to August 2020. Due to a
lack of consistent information and policies on COVID-19, various
doubts concerning the risk factors associated with the mortality
and severity of this disease, have arisen. COVID-19 has several
clinical spectrums, ranging from asymptomatic infection to
development of severe and critical illness. The asymptomatic stage
is the first stage of infection where severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) enters the body infecting the
host cell through angiotensin-converting enzyme 2 (ACE2) receptor.
The diagnosis is made by analyzing the viral load using reverse
transcription-quantitative polymerase chain reaction (RT-qPCR). It
is well known that asymptomatic carriers can transmit SARS-CoV-2.
Cases with mild to moderate infection exhibit cold-like symptoms,
new loss of taste or smell, nausea or vomiting, and diarrhea.
Severe and critical cases exhibit worsening of symptoms and require
hospitalization or even invasive mechanical ventilation. Symptoms
encountered in these stages include worsening dyspnea and
refractory hypoxemia (1,2).
Furthermore, frequency of COVID-19 and preexisting
comorbidities increase the risk of mortality. Hypertension is the
most prevalent comorbidity among COVID-19 patients, followed by
diabetes (3). Its prevalence varies
by nation, ranging from 7 to 21% in China (4) to 36% in Italy (5). Type 2 diabetes mellitus (T2DM)
increases the severity of COVID-19. A meta-analysis of 40 studies
with 18,012 COVID-19 patients, associated T2DM to COVID-19 severity
(RR, 2.45; P=0.001; I2, 45%) (6). Hyperglycemia, reduced immune function,
vascular problems, and concomitant diseases such as hypertension,
dyslipidemia, and cardiovascular disease increase the risk of
infection and severity of COVID-19 in individuals with T2DM
(7). Chronic hyperglycemia also
increases proinflammatory and prothrombotic cytokines, aggravating
the hypercoagulable condition in T2DM patients with COVID-19
infection, increasing the risk of bleeding (8). Patients with type 2 diabetes have
therefore become a major concern during the COVID-19 pandemic.
Some of the factors contributing to the severity of
COVID-19 in patients with T2DM have been previously reported, and
include obesity, hypertension, cardiovascular disease, and
dyslipidemia. Other factors include age, extended hyperglycemia,
high ACE expression, hypoalbuminemia, and increased inflammation
(8-10).
Increased inflammatory indicators, including the
neutrophil-lymphocyte ratio (NLR), have been revealed both in
patients with T2DM and in infections such as COVID-19. However,
there is no well-defined NLR cut-off value predicting the severity
of COVID-19 in T2DM patients (11,12).
According to Zhang et al (13), a reduction in CD4+
lymphocytes and an increase in serum amyloid A, upon hospital
admission, were independent risk factors for COVID-19 individuals
with T2DM. In addition, having fasting blood glucose levels ≥7.0
mmol/λ (14) or >180 mg/dl
(15) was demonstrated to be an
independent risk factor for progression to critical disease among
COVID-19 patients with T2DM. Individuals with HbA1c levels >9%
were more prone to have severe COVID-19 symptoms (16,17).
In fact, poor glycaemic management and a markedly higher immune
inflammatory response in patients with T2DM were revealed to be
associated with worse clinical outcomes among COVID-19 cases with
T2DM (18).
The present study investigated the clinical
characteristics of COVID-19 patients with T2DM at Dr Soetomo
General Hospital (Surabaya, Indonesia). The characteristics
associated with severity of COVID-19 in newly diagnosed COVID-19
patients with T2DM were also examined. The NLR cut-off value for
severity of COVID-19 in individuals with T2DM was also
identified.
Patients and methods
Research design and subjects
From May 1 to August 31, 2020, at Dr Soetomo General
Hospital (Surabaya, Indonesia), a cross-sectional analytical
observational study was performed using the medical records of
patients with COVID-19 and T2DM. The COVID-19 variants circulating
during the time of the study were alpha and beta, however, genetic
analysis was not performed to determine the COVID-19 variant in
each subject. The Research Ethics Committee of Dr Soetomo General
Hospital authorized the present study (ref. no.
0182/LOE/301.4.2/XI/2020). All patients provided written informed
consent prior to the data collection.
The research included all adult patients (≥18 years
old) treated for COVID-19 (RT-qPCR, nasopharyngeal swab) and T2DM
(ICD-10) at Dr Soetomo General Hospital. The participants had not
been vaccinated at the time of the study. Moreover, it was
compulsory for the medical records of patients to include all
variables analyzed, such as diagnostic, clinical, and laboratory
data, at the time of first hospital admission, and for COVID-19
symptoms to be <7 days. Those with type 1 diabetes mellitus,
hemoglobin levels <10 g/dl, pregnant women or women on
estrogen/progesterone hormone therapy were excluded, as were those
with autoimmune disease, malignancy, or lung disease (asthma, COPD,
or tuberculosis), diagnosed prior to COVID-19 infection.
Data collection methods and
definitions of variables
The sampling method used in the present study was
total sampling. Through patient medical records, the variables
studied included age, sex, hypertension, chronic complications of
diabetes, duration of diabetes, glycemic control (HbA1c),
hyperglycemic conditions (random blood sugar), inflammatory markers
(NLR) and hypoalbumin. These variables were analyzed in relation to
the severity of COVID-19.
COVID-19 admissions were classified as either severe
or non-severe based on their severity. According to WHO in 2020,
severe cases were defined as those with indications of pneumonia
(fever, cough, shortness of breath, and rapid breathing) plus any
of the following symptoms including a free oxygen saturation level
of ≤90% in room air, a respiratory rate of ≥30 breaths/min, and a
PaO2/FiO2 ratio ≤300 mmHg. When
PaO2 data was not available, ARDS was indicated by an
SpO2/FiO2 ratio of ≤315(19). According to JNC 8 hypertension
guidelines, hypertension was defined as having a systolic blood
pressure of ≥140 mmHg and/or a diastolic blood pressure of ≥90 mmHg
or being on antihypertensive medication (20). According to the American Diabetes
Asociation, the chronic complications of T2DM were macrovascular
and microvascular complications, which were coded as (ICD X) I25.9
(chronic ischemic heart disease); I73.9 (peripheral vascular
disease); I60-I69 (cerebrovascular disease); E11.21 (diabetic
nephropathy); E11.40 (diabetic neuropathy); and E11.31 (diabetic
retinopathy) (21).
The duration of T2DM was defined as the period from
when the patient was first diagnosed with diabetes mellitus to the
time of assessment, with a cutoff of >10 years indicating a
severe disease in T2DM patients with COVID-19. Glycemic control
using HbA1c with an ≥8% cutoff indicated severe COVID-19 in
patients (22). HbA1c was measured
during hospitalization with DCA Vantage equipment and the reagent
kit (supplied by Siemens Healthineers Indonesia; manufactured by
Siemens Healthcare Diagnostic Manufacturing Ltd.), Siemens DCA
HbA1c (supplied by Siemens Healthineers Indonesia; manufactured by
Siemens Healthcare Diagnostic Manufacturing Ltd.), which uses the
immunoagglutination technique. Hyperglycemia, according to the
Indonesian Society of Endocrinology, in 2019, was defined as a
random blood sugar level of >200 mg/dl that was measured at the
time of admission (23).
The NLR is a measure of inflammation that is
determined by dividing total neutrophils by total lymphocytes
(12). A complete blood count was
used to acquire NLR data. Hypoalbumin was defined as serum albumin
of <3.5 g/dl, as measured by the Siemens Dimension EXL
instrument (supplied by Siemens Healthineers Indonesia;
manufactured by Siemens Healthcare Diagnostic Manufacturing Ltd.)
at Dr Soetomo General Hospital.
Statistical analysis
For categorical data types (nominal and ordinal),
descriptive data included frequency and percentage, whereas for
continuous data types the mean ± SD or median (IQR) were used
(interval and ratio). The Chi Square test was used for bivariate
analysis of variables associated with extreme severity of COVID-19
in the present research. By combining all variables with P-value of
<0.25 in the bivariate analysis, a multivariate logistic
regression analysis was used to determine the dominating factor of
severe COVID-19. The findings were expressed as an odds ratio (OR),
with a P-value <0.05 considered to indicate a statistically
significant difference, and the 95% confidence interval (CI) was
calculated. The cut-off value, sensitivity, and specificity of NLR
were determined using a receiver operating characteristic (ROC)
curve. Statistical Package for the Social Sciences (SPSS) version
25.0 was used to examine all data (IBM Corp.).
Results
An overview of the characteristics of
the study participants at the time of their admittance to
hospital
The research subjects were classified as severe and
non-severe cases of COVID-19 according to their medical records.
From the 201 study subjects included in the present study, 108
patients (53.7%) were defined as severe and 93 patients (46.3%) as
non-severe COVID-19 (Table I). The
general characteristics of COVID-19 patients with T2DM who were
treated at Dr Soetomo General Hospital, included an average age of
55.69±9.47 years with the majority being <60 years old (70.1%),
and males (52.7%). In addition, 67.7% were non-referral patients.
Furthermore, for the majority of patients, diabetes onset was
<10 years (76.1%) (Table
II).
 | Table ISeverity of COVID-19 among research
subjects. |
Table I
Severity of COVID-19 among research
subjects.
| Patients | n (%) |
|---|
| Severe
COVID-19 | 108 (53.7%) |
| Non-severe
COVID-19 | 93 (46.3%) |
 | Table IIGeneral characteristics of research
subjects with COVID-19 at admission to hospital. |
Table II
General characteristics of research
subjects with COVID-19 at admission to hospital.
| Variables | Total (%), total
N=201 patients |
|---|
| Age, years (mean ±
SD) (min-max) | 55.69±9.47
(27-81) |
|
<60 | 141 (70.1%) |
|
≥60 | 60 (29.9%) |
| Sex | |
|
Male | 106 (52.7%) |
|
Female | 95 (47.3%) |
| Admitted to
hospital | |
|
Without
referral | 136 (67.7%) |
|
With
referral | 65 (32.3%) |
| Diabetes mellitus
onset | |
|
<10
years | 153 (76.1%) |
|
≥10
years | 48 (23.9%) |
T2DM patients treated in an isolation room at Dr
Soetomo General Hospital had an average of 4.3±1.92 days from onset
of symptoms until admission to the hospital. The most prevalent
clinical symptoms noted in the medical records of the patients were
dry cough (79.6%), shortness of breath (69.2%), and fever (66.7%),
with 114 individuals having concomitant hypertension (56.7%)
(Table III).
 | Table IIIClinical profile of research subjects
with COVID-19 at admission to hospital. |
Table III
Clinical profile of research subjects
with COVID-19 at admission to hospital.
| Variables | Total (%), total
N=201 patients |
|---|
| From the onset of
symptoms to the time of admission, mean ± SD (min-max) | 4.3±1.92 (1-7)
days |
| Clinical
symptoms | |
|
Dry
cough | 160 (79.6%) |
|
Short of
breath | 139 (69.2%) |
|
Fever | 134 (66.7%) |
|
Sore
throat | 80 (39.8%) |
|
Decreased
appetite | 76 (37.8%) |
|
Tired
easily | 48 (23.9%) |
|
Cough with
phlegm | 22 (10.9%) |
|
Diarrhea | 21 (10.4%) |
|
Loss of
consciousness | 17 (8.5%) |
|
Runny
nose | 17 (6%) |
|
Anosmia | 9 (4.5%) |
|
Muscle
aches | 8 (4%) |
| Hypertension | |
|
Yes | 114 (56.7%) |
|
No | 87 (43.3%) |
| Chronic
complications | |
|
Yes | 42 (20.9%) |
|
No | 159 (79.1%) |
| Vital Signs
(median, range) | |
|
Systolic
blood pressure (mmHg) | 140 (77-209) |
|
Diastolic
blood pressure (mmHg) | 82 (50-116) |
|
Pulse
(x/min) | 98 (69-132) |
|
Respiratory
rate (x/min) | 2 (18-40) |
|
SpO2
(%) | 92 (60-100) |
The median hemoglobin, hematocrit, leukocytes,
platelets, serum creatinine, sodium, potassium, chloride, and
procalcitonin levels of the study participants were all in the
normal range. In addition, the median neutrophil, SGOT, baseline
blood sugar, HbA1c, and CRP levels were significantly higher than
the normal values. Lymphocytes, BUN, and albumin median values were
all below the normal range, with a median NLR of 7.96. The majority
of the study participants had albumin levels of <3.5 g/dl
(71.6%), blood sugar levels of ≥200 mg/dl (62.2%), and HbA1c levels
≥8% (61.7%). The chest X-rays revealed that the majority of the
abnormalities were bilateral pulmonary disorders (85.57%) (Table IV).
 | Table IVAdditional findings of research
subjects with COVID-19 admitted to hospital. |
Table IV
Additional findings of research
subjects with COVID-19 admitted to hospital.
| Parameters | Median | Min-max | Frequency, n
(%) | Normal |
|---|
| Laboratory
findings | | | | |
|
Hemoglobin
(g/dl) | 13.5 | 10-17.4 | | 11-15 |
|
Hematocrit
(%) | 39.5 | 30.1-53.4 | | 33-47 |
|
Leukocytes
(x109/l) | 8.91 | 3.69-49.6 | | 4-10 |
|
Neutrophils
(x109/l) | 7.71 | 1.95-45.38 | | 2-7 |
|
Lymphocytes
(x109/l) | 0.98 | 0.22-3.85 | | 1-4 |
|
Platelets
(x109/l) | 257 | 26.7-881 | | 150-450 |
|
BUN
(mg/dl) | 19 | 7-141 | | 20-67 |
|
Creatinine
(mg/dl) | 1.1 | 0.4-8.76 | | 0.4-1.2 |
|
eGFR | 73 | 7-141 | | 60 |
|
SGOT | 54 | 14-779 | | 20-50 |
|
SGPT | 46 | 10-338 | | 25-70 |
|
CRP
(mg/l) | 10.7 | 0.1-76 | | <10 |
|
Sodium | 136 | 107-163 | | 135-145 |
|
Potassium | 4.1 | 2.6-6.6 | | 3.5-5.5 |
|
Chloride | 98 | 68-134 | | 96-126 |
|
Procalcitonin
(ng/ml) | 0.2 | 0.1-100 | | <0.5 |
|
NLR | 7.96 | 1.48-62.81 | | |
|
Albumin
(g/dl) | 3.16 | 2.14-3.93 | | 3.5-5.4 |
|
<3.5 | | | 144 (71.6%) | |
|
≥3.5 | | | 57 (28.4%) | |
|
Blood sugar
(mg/dl) | 242 | 61-989 | | <200 |
|
<200 | | | 76 (37.8%) | |
|
≥200 | | | 125 (62.2%) | |
|
HbA1c
(%) | 8.8 | 6-16.5 | | <7 |
|
<8% | | | 77 (38.3%) | |
|
≥8% | | | 124 (61.7%) | |
| Radiology findings
(lung chest X-ray) | | | | |
|
No
abnormalities | | | 11 (5.5%) | |
|
Bilateral
lung disorders | | | 172 (85.57%) | |
|
Unilateral
lung disorders | | | 18 (8.93%) | |
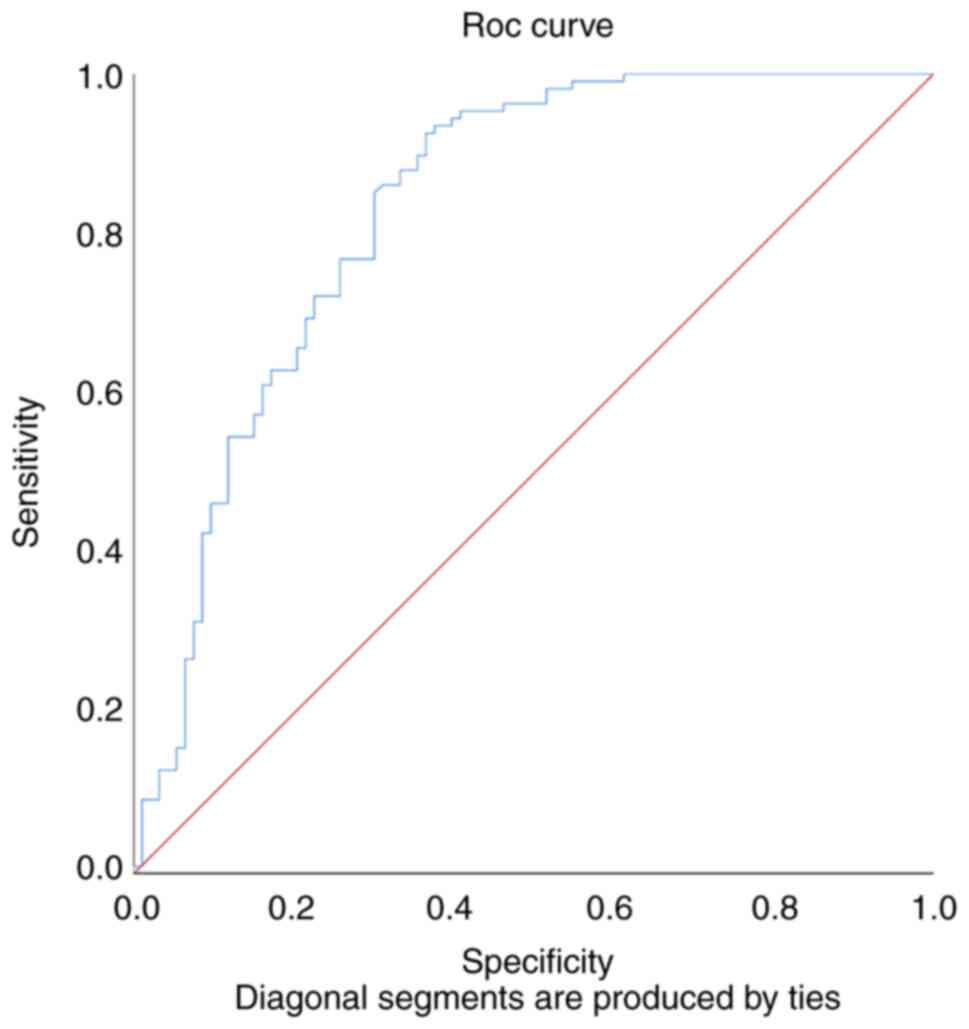
The ROC analysis (Fig.
1) revealed an AUC of 0.833 (P<0.0001) and the NLR cut-off
value was 7.36 to evaluate the severity of COVID-19 in patients
with T2DM. The NLR value was 79.6% sensitive and 74.24% specific in
determining the severity of COVID-19 individuals with T2DM using
this cut-off value.
Bivariate analysis of factors
associated with the severity of COVID-19 at admission of study
subjects to hospital
The results of a bivariate chi-square study of
factors linked with the severity of COVID-19 in patients with T2DM
are presented in Table V. Age
(P=0.002), sex (P=0.015), onset of diabetes mellitus (P=0.011),
presence of hypertension (P<0.001), NLR (P<0.001), and HbA1c
(P=0.002) were found to be associated with the severity of
COVID-19. These factors were further assessed using multivariate
analysis.
 | Table VBivariate analysis of factors
associated with severity of COVID-19 in study subjects admitted to
hospital. |
Table V
Bivariate analysis of factors
associated with severity of COVID-19 in study subjects admitted to
hospital.
| | 95% CI |
|---|
|
Characteristics | Severe [n (%)] | Non-severe [n
(%)] | P-value | OR | Lower limit | Upper limit |
|---|
| Age, years | | | | | | |
|
≥60 | 43 (21.4%) | 17 (8.5%) | 0.002 | 2.96 | 1.54 | 5.68 |
|
<60 | 65 (32.3%) | 76 (37.8%) | | | | |
| Sex | | | | | | |
|
Male | 66 (32.8%) | 40 (19.9%) | 0.015 | 2.08 | 1.18 | 3.66 |
|
Female | 42 (20.9%) | 53 (26.4%) | | | | |
| Diabetes mellitus
onset | | | | | | |
|
≥10
years | 34 (16.9%) | 14 (7%) | 0.011 | 2.5 | 1.3 | 5.2 |
|
<10
years | 74 (36.8%) | 79 (39.3%) | | | | |
| Hypertension | | | | | | |
|
Yes | 78 (38.8%) | 36 (17.9%) | <0.001 | 4.12 | 2.28 | 7.45 |
|
No | 30 (14.9%) | 57 (28.4%) | | | | |
| Chronic
complications | | | | | | |
|
Yes | 26 (12.9%) | 16 (8%) | 0.307 | 1.53 | 0.76 | 3.06 |
|
No | 82 (40.8%) | 77 (38.3%) | | | | |
| NLR | | | | | | |
|
≥7.36 | 79 (39.3%) | 28 (13.9%) | <0.001 | 6.32 | 3.4 | 11.69 |
|
<7.36 | 29 (14.4%) | 65 (32.2%) | | | | |
| Albumin (g/dl) | | | | | | |
|
<3.5 | 84 (41.8%) | 60 (29.9%) | 0.054 | 1.93 | 1.03 | 3.58 |
|
≥3.5 | 24 (11.9%) | 33 (16.4%) | | | | |
| Blood sugar
(mg/dl) | | | | | | |
|
≥200 | 71 (35.3%) | 54 (26.9%) | 0.33 | 1.39 | 0.78 | 2.46 |
|
<200 | 37 (18.4%) | 39 (19.4%) | | | | |
| HbA1c (%) | | | | | | |
|
≥8% | 78 (38.8%) | 47 (23.4%) | 0.002 | 2.67 | 1.48 | 4.77 |
|
<8% | 30 (14.9%) | 46 (22.9%) | | | | |
Multivariate analysis of parameters
associated with severity of COVID-19 at admission of study
participants to hospital
As revealed in Table
VI, the logistic regression coefficient for the NLR ≥7.36
factor was 1.85, with an OR or exp (B) value of 6.39. For the
occurrence of hypertension, the logistic regression coefficient was
1.4, with an OR or exp (B) value of 4.07. The logistic regression
coefficient for HbA1c ≥8% was 1.27 with an OR or exp (B) value of
3.55. For the factor with regard to age ≥60 years, the logistic
regression coefficient was 1.07, with an OR or exp (B) value of
2.92. For the male sex factor, the logistic regression coefficient
was 0.73, with an OR or exp (B) value of 2.07.
 | Table VIEstimation results of the severity
risk logistics model for COVID-19 patients with type 2 diabetes
mellitus. |
Table VI
Estimation results of the severity
risk logistics model for COVID-19 patients with type 2 diabetes
mellitus.
| | 95% CI |
|---|
| Factors | B
(coefficient) | P-value | OR | Lower limit | Upper limit |
|---|
| Diabetes mellitus
onset 10 years | 0.002 | 0.996 | 1.01 | 0.41 | 2.47 |
| Albumin <3.5
g/dl | 0.66 | 0.094 | 1.93 | 0.9 | 4.16 |
| Male sex | 0.73 | 0.042a | 2.07 | 1.03 | 4.17 |
| Age ≥60 years
old | 1.07 | 0.008a | 2.92 | 1.32 | 6.5 |
| HbA1c ≥8% | 1.27 | 0.001a | 3.55 | 1.68 | 7.52 |
| Hypertension | 1.4 |
<0.001a | 4.07 | 2.01 | 8.26 |
| NLR ≥7.36 | 1.85 |
<0.001a | 6.39 | 3.14 | 12.99 |
Discussion
In the present study, multivariate analysis revealed
that the presence of an NLR ≥7.36, hypertension, an HbA1c ≥8%, age
≥60 years, and male sex were significantly associated with severe
COVID-19 in patients with type 2 diabetes. Consequently, these
factors may aid clinicians in identifying the severity of COVID-19
infection more rapidly and provide more aggressive treatment, as
well as become a target for prevention, particularly in the
management of hypertension and glycemic control, in order to reduce
the severity of disease in COVID-19-infected T2DM patients. In a
previous study it was revealed that there was a slightly increased
antibiotic usage in the diabetic group, but there was no
significant difference in treatment provided to non-diabetic
COVID-19 infections and the non-diabetic control group (24).
Furthermore, it was identified that age (≥60 years)
was associated with severity of COVID-19 in patients with T2DM. In
addition, the research subjects had a mean age of 55.69±9.47 with a
median of 56 years and an age range of 27-81 years, similar to the
findings of previous studies conducted in China in which the median
age of COVID-19 patients with T2DM was 54-58 years (25,26). A
meta-analysis of 3,027 COVID-19 patients in China revealed that age
(>65 years) was a risk factor for severe COVID-19 development
(OR 6.06; P=0.00001) (27). Another
meta-analysis of studies conducted in China, France, Germany,
Singapore, and the USA found that age (≥60 years) was likewise
associated with severe COVID-19 (OR 3; 95% CI: 1.4-6) (26). Du et al (28), also revealed a significant
association between older age and the degree of severity in
COVID-19 patients (OR 2.62; I2=0%; n=2). In patients
with T2DM, COVID-19 is more severe as they get older. This is due
to a number of factors, including the fact that people >60 years
of age are more likely to have diabetes for a long period of time,
resulting in complications; diabetes in the elderly is closely
associated with various other comorbidities such as cardiovascular
disease, hypertension, and obesity; and, in addition, there are
defects in the function of T and B cells, as well as overproduction
of proinflammatory cytokines (29-33).
In the present study, the severity of COVID-19 was not compared
between diabetic and non-diabetic groups, however, a study
conducted by Zhang et al (24) revealed that patients with diabetes
and secondary hyperglycemia were of greater risk (2.5 fold) of more
severe COVID-19 infections compared to non-diabetic patients.
In the present study, male sex was also revealed to
be associated with the severity of COVID-19 in patients with T2DM.
This finding was in line with other research which linked male sex
with severity of COVID-19 in individuals with T2DM (13,22,34).
Men are at a higher risk of severe COVID-19 due to lifestyle
factors such as smoking addiction, which is more prevalent in men
than in women, and the presence of estrogen, an immune-regulating
gene encoded by the X chromosome that is present in women and plays
a protective role in SARS by not only activating the immune
response but also suppressing SARS-CoV replication, allowing
estrogen to regulate ACE2 expression (35,36).
Additionally, in an animal model, it was revealed that males have
higher ACE2 receptor activity due to increased enzyme velocity
(37).
In the present study, most participants (79.1%) had
no chronic complications (both macrovascular and microvascular) as
revealed by their medical records, while in a study conducted by
Zhang et al (24) it was
identified that at the time of admission to hospital, 57.7% of
COVID-19 patients with T2DM had chronic diabetic complications.
Chronic complications were noted in only 20.9% of the patients in
the present study, most likely due to the facts that diabetes
mellitus onset for the majority was <10 years and most patients
were aged <60 years. The longer a patient has T2DM, the more
vascular complications there are, particularly cardiovascular
complications (38). A study
performed in Israel on 5,869 COVID-19 individuals with T2DM
revealed that for the majority of patients T2DM onset was >10
years (22). According to the 2019
statistics from the International Diabetes Federation (IDF),
Indonesia ranks fifth in terms of patients with predicted
undiagnosed diabetes. It has been reported that as many as 50% of
individuals with T2DM in the population do not know that they have
T2DM (remain undiagnosed) (39).
Moreover, in the present study the majority of
subjects had HbA1c levels of ≥8% and random blood glucose levels of
≥200 mg/dl upon admission to hospital. Research performed in China
on a COVID-19 population with T2DM revealed a median HbA1c of 8.7%
and a median blood glucose level of 147.74 mg/dl, respectively
(13). According to the CORONADO
trial, the mean HbA1c in COVID-19 patients with T2DM was 8.1±1.9%,
and the median baseline blood sugar level was 165.77 (IQR
122.52-227.39) mg/dl (40). Various
studies have revealed that the HbA1c and random blood glucose (RBG)
levels of diabetes mellitus patients infected with COVID-19 are
still higher than the Indonesian Society of Endocrinology and ADA
objectives of <7% and <200, respectively (21,23).
In the present study, diabetes onset of ≥10 years
was associated with severe COVID-19 in patients with T2DM admitted
to hospital. In comparison with onset of ≤5 years and 6-10 years,
diabetes onset of >10 years was significantly associated
(P<0.001) with severity of COVID-19 at first hospital admission
(22). Vascular endothelial damage
is more common in patients with long-term T2DM (26). Varga et al (41), also demonstrated that SARS CoV-2 can
infect endothelial cells directly, indicating that in patients with
endothelial disorders, such as T2DM, the severity of COVID-19 is
exacerbated, thereby increasing susceptibility to infection and
thereby increasing the severity of patients infected with SARS
CoV-2.
In addition, in the present study, hypertension was
associated with the severity of COVID-19 in patients with T2DM.
These findings are consistent with a study by Hayek et al
(22), which revealed that
hypertension was significantly more prevalent in the severely ill
COVID-19 group than in the non-severely ill COVID-19 group (85.5
vs. 68.7%; P<0.001). By contrast, research by Zhang et al
(42), revealed no significant
correlation between concomitant hypertension and severity of
COVID-19. Conversely, hypertension was the comorbidity most
commonly associated with an increased risk of severity in
individuals with COVID-19 (27,28,43-55).
Immune system disruption in patients with T2DM and hypertension
increases the risk of infection with COVID-19(46). Hypertension is hypothesized to
exacerbate the inflammatory process associated with COVID-19
infection in patients with T2DM, which is characterized by higher
levels of inflammatory markers such as TNF-α and IL-6 in patients
with severe COVID-19(47).
Additionally, individuals with T2DM whose conditions are
exacerbated by hypertension have a weakened immune system
(TCD8+ cell malfunction) and are under chronic stress
(27,45,48).
It has been revealed that the structure of blood vessels of
individuals who have diabetes and hypertension, for an extended
period of time, undergoes damage, rendering these individuals more
susceptible to complications if infected with COVID-19(27). Additionally, hypertension may result
in a reduction in ACE2 expression, resulting in an increase in
angiotensin 2 and a decrease in angiotensin 1-7 levels, as well as
renin-angiotensin system dysfunction, affecting fluid-electrolyte
balance and, of course, blood pressure (8,30).
In the present study, an NLR ≥7.36 was associated
with severe COVID-19 in patients with T2DM admitted to hospital.
This finding is in line with a study by Liu et al (34), which revealed that the higher the
NLR, the greater the severity of COVID-19. It is possible that the
chronic inflammation associated with T2DM, as well as with COVID-19
infection, may increase NLR (42,49).
Because both neutrophils and lymphocytes are involved in the immune
response, virus-induced inflammation increases NLR. Neutrophils are
the first and most abundant cell population to reach the site of
infection, and their number is increased due to inflammatory
factors, whereas lymphopenia occurs due to immune system
suppression of cellular immunity. A secondary immune response may
occur 4-7 days following the first symptoms of COVID-19, thus
worsening the condition of the patient, consistent with the
findings in the present the study which revealed that the median
time for hospital admission since the first symptoms was 4 days
(44,50).
As aforementioned, in the present study, an HbA1c
value of ≥8% was associated with the severity of COVID-19 in
patients with T2DM admitted to hospital. A recent study revealed
that an HbA1c of 8% was a risk factor for severe COVID-19 with
intubation or death after 7 days of therapy (OR 2.26; P<0.05)
(51). In patients with T2DM, an
HbA1c >9% was revealed to be an independent predictor of
multiple organ damage (OR 2.98; P=0.043) (17). Additionally, diabetic patients with
poor glycemic control (HbA1c >8%) exhibited significantly
reduced lung function as a result of chronic low-grade inflammation
and microangiopathy of pulmonary vascular tissue, impairing lung
connective tissue metabolism and causing basement membrane and
alveolar epithelium thickening (52,53).
As a result, it was determined that COVID-19 in T2DM patients
results in a deterioration of the glycemic profile, which further
weakens the innate immune response and increases proinflammatory
cytokines, whereupon a vicious cycle is created (54,55).
In the present study, albumin levels of ≤3.5 g/dl
did not indicate a significant correlation with severe COVID-19 in
patients with T2DM admitted to hospital. However, a study by Zhang
et al (13) revealed that in
severe COVID-19 patients with T2DM, a lower median albumin level
(3.13 vs. 3.85 g/dl; P<0.001) was observed compared with
non-severe COVID-19 patients with T2DM. A previous study, involving
various research centers in China and 482 COVID-19 patients
revealed that hypoalbumin was a risk factor for severe COVID-19
(OR: 2,121; 95% CI: 1,258-3,577; P=0.005) (56). A high albumin value upon admission
to hospital, is a strong predictor of a better prognosis in
patients with COVID-19(10). The
majority of patients in the present study had albumin levels below
normal, with a median of 3.5 g/dl. Albumin has physiological
features such as anti-inflammatory, antioxidant, anticoagulant, and
antiplatelet action, as well as colloid osmotic activity (10,56).
Hypoalbuminemia may arise in COVID-19 patients with T2DM as a
result of inflammation-mediated capillary leakage, reduced albumin
production in hepatocytes, or as a result of chronic consequences
of diabetes or direct kidney injury. Hypoalbumin increases the
occurrence of acute respiratory failure from ARDS due to plasma
leakage causing changes in osmotic pressure and decreased ability
to combat oxidative stress (10,56).
The present study has some limitations that may have
an impact on the findings. First, this is a centralized research
performed at one of the main referral hospitals of East Java
(Indonesia). Therefore, non-severe patients may be underrepresented
since they self-isolate at home or visit local government-prepared
health facilities such as field hospitals. Second, this research
used a cross sectional design and secondary data from medical
records, such as medication history, D-dimer and BMI were excluded.
Third, this study was performed from May to August 2020, excluding
the delta variant period. Fourth, comparison of the severity of the
disease between diabetic and non-diabetic groups was not
performed.
The present study may be useful in providing
insights into the severity of COVID-19 and comorbities,
particularly T2DM. Several studies found a correlation between
severity of COVID-19 and increased inflammatory responses (34,42,45,48,49),
while other studies determined that glycemic control was associated
with patient outcome (24,51-53),
and certain others found that there is a correlation between
hypertension, diabetes and COVID-19 infection (22,27,28,43-45).
The aforementioned are independent studies, and while they support
each other and the findings of the present study, to the best of
our knowledge, research comparing a combination of several factors
has yet to be performed. The present research contributes to the
future development of preventative measures by managing various
parameters (NLR, albumin level, blood sugar level and
hypertension), resulting in a reduction in the number of severe
COVID-19 patients with T2DM as well as other comorbidities.
In the present study, it can be concluded that
variables including age, sex, diabetes onset, hypertension, NLR,
albumin, and HbA1c are associated with severity of COVID-19.
Patients with T2DM who were infected by COVID-19 were more likely
to have severe symptoms if they had an NLR ≥7.36, hypertension, an
HbA1c of ≥8%, were aged ≥60 years, and were of the male sex. These
characteristics may assist clinicians in diagnosing, controlling,
and avoiding morbidity and mortality of COVID-19 patients with
T2DM. In addition, studies using a multicenter design and a larger
sample size are required. Further research which involves more of
the SARS CoV-2 virus variant is also warranted.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used during the present study are
available from the corresponding author upon reasonable
request.
Authors' contributions
All authors (HN, SAS, UH, AP, CC and NS) conceived
and designed the study, acquired and analyzed the data as well as
drafted the manuscript and revised it, and confirm the authenticity
of all the raw data. All authors read and approved the final
manuscript.
Ethical approval and consent to
participate
The present study was approved (ref. no.
0182/LOE/301.4.2/XI/2020) by the Research Ethics Committee of Dr
Soetomo General Hospital (Surabaya, Indonesia). All patients
provided written informed consent prior to the data collection.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cordon-Cardo C, Pujadas E, Wajnberg A,
Sebra R, Patel G, Firpo-Betancourt A, Fowkes M, Sordillo E,
Paniz-Mondolfi A, Gregory J, et al: COVID-19: Staging of a new
disease. Cancer Cell. 38:594–597. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ucciferri C, Vecchiet J and Falasca K:
Role of monoclonal antibody drugs in the treatment of COVID-19.
World J Clin Cases. 8:4280–4285. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Singh AK, Gupta R, Ghosh A and Misra A:
Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and
practical considerations. Diabetes Metab Syndr. 14:303–310.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huang I, Lim MA and Pranata R: Diabetes
mellitus is associated with increased mortality and severity of
disease in COVID-19 pneumonia-A systematic review, meta-analysis,
and meta-regression. Diabetes Metab Syndr. 14:395–403.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Onder G, Rezza G and Brusaferro S:
Case-Fatality rate and characteristics of patients dying in
relation to COVID-19 in Italy. JAMA. 323:1775–1776. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
de Almeida-Pititto B, Dualib PM,
Zajdenverg L, Dantas JR, de Souza FD, Rodacki M and Bertoluci MC:
Brazilian Diabetes Society Study Group (SBD). Severity and
mortality of COVID 19 in patients with diabetes, hypertension and
cardiovascular disease: A meta-analysis. Diabetol Metab Syndr.
12(75)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Jeong IK, Yoon KH and Lee MK: Diabetes and
COVID-19: Global and regional perspectives. Diabetes Res Clin
Pract. 166(108303)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rajpal A, Rahimi L and Ismail-Beigi F:
Factors leading to high morbidity and mortality of COVID-19 in
patients with type 2 diabetes. J Diabetes. 12:895–908.
2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
McGurnaghan SJ, Weir A, Bishop J, Kennedy
S, Blackbourn LAK, McAllister DA, Hutchinson S, Caparrotta TM,
Mellor J, Jeyam A, et al: Risks of and risk factors for COVID-19
disease in people with diabetes: A cohort study of the total
population of Scotland. Lancet Diabetes Endocrinol. 9:82–93.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kheir M, Saleem F, Wang C, Mann A and Chua
J: Higher albumin levels on admission predict better prognosis in
patients with confirmed COVID-19. PLoS One.
16(e0248358)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kalbhande JG and Kuldeep V: Lymphopenia in
COVID-19 patients & its association with uncontrolled diabetes,
obesity and elderly: A perspective review. J Med Sci Clin Res.
8:398–401. 2020.
|
|
12
|
Man MA, Rajnoveanu RM, Motoc NS, Bondor
CI, Chis AF, Lesan A, Puiu R, Lucaciu SR, Dantes E, Gergely-Domokos
B and Fira-Mladinescu O: Neutrophil-to-lymphocyte ratio,
platelets-to-lymphocyte ratio, and eosinophils correlation with
high-resolution computer tomography severity score in COVID-19
patients. PLoS One. 16(e0252599)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhang Q, Wei Y, Chen M, Wan Q and Chen X:
Clinical analysis of risk factors for severe COVID-19 patients with
type 2 diabetes. J Diabetes Complications.
34(107666)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wu J, Zhang J, Sun X, Wang L, Xu Y, Zhang
Y, Liu X and Dong C: Influence of diabetes mellitus on the severity
and fatality of SARS-CoV-2 (COVID-19) infection. Diabetes, Obes
Metab. 22:1907–1914. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Singh AK and Khunti K: Assessment of risk,
severity, mortality, glycemic control and antidiabetic agents in
patients with diabetes and COVID-19: A narrative review. Diabetes
Res Clin Pract. 165(108266)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Vijayam B, Balaji MS, Balaji T, Veerasamy
S and Devaraj S: Predicting the coronavirus disease 2019 severity
in patients with diabetes using hemoglobin A1c. Int J Sci Study.
9:64–67. 2021.
|
|
17
|
Merzon E, Green I, Shpigelman M, Vinker S,
Raz I, Golan-Cohen A and Eldor R: Haemoglobin A1c is a predictor of
COVID-19 severity in patients with diabetes. Diabetes Metab Res
Rev. 37(e3398)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Elnaem MH and Cheema E: Caring for
patients with diabetes during COVID-19 pandemic: Important
considerations for pharmacists. Res Soc Adm Pharm. 17:1938–1941.
2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
World Health Organization (WHO):
Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
Accessed September 16, 2020.
|
|
20
|
James PA, Oparil S, Carter BL, Cushman WC,
Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML,
MacKenzie TD, Ogedegbe O, et al: 2014 Evidence-based guideline for
the management of high blood pressure in adults report from the
panel members appointed to the Eighth Joint National Committee (JNC
8). JAMA. 311:507–520. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
American Diabetes Association (ADA).
Standards of Medical Care in Diabetes-2017. Diabetes Care. 40
(Suppl 1):S1–S2. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hayek S, Ben-Shlomo Y, Balicer R, Byrne K,
Katz M, Kepten E, Raz I, Roitman E, Zychma M, Barda N, et al:
Preinfection glycaemic control and disease severity among patients
with type 2 diabetes and COVID-19: A retrospective, cohort study.
Diabetes, Obes Metab. 23:1995–2000. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Rudianto A, Soewondo P, Waspadji S, Yunir
E and Purnamasari D: The Indonesian Society of Endocrinology’s
Summary Article of Diabetes Mellitus National Clinical Practice
Guidelines. J ASEAN Fed Endocr Soc. 26(17)2011.
|
|
24
|
Zhang Y, Li H, Zhang J, Cao Y, Zhao X, Yu
N, Gao Y, Ma J, Zhang H, Zhang J, et al: The clinical
characteristics and outcomes of patients with diabetes and
secondary hyperglycaemia with coronavirus disease 2019: A
single-centre, retrospective, observational study in Wuhan.
Diabetes, Obes Metab. 22:1443–1454. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,
Xiang J, Wang Y, Song B, Gu X, et al: Clinical course and risk
factors for mortality of adult inpatients with COVID-19 in Wuhan,
China: A retrospective cohort study. Lancet. 395:1054–1062.
2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wang F, Yang Y, Dong K, Yan Y, Zhang S,
Ren H, Yu X and Shi X: Clinical characteristics of 28 Patients with
diabetes and COVID-19 in Wuhan, China. Endocr Pract. 26:668–674.
2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng
J, Li Q, Jiang C, Zhou Y, Liu S, et al: Risk factors of critical
& mortal COVID-19 cases: A systematic literature review and
meta-analysis. J Infect. 81:e16–e25. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Du P, Li D, Wang A, Shen S, Ma Z and Li X:
A systematic review and meta-analysis of risk factors associated
with severity and death in COVID-19 patients. Can J Infect Dis Med
Microbiol. 2021(6660930)2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Setiati S, Harimurti K, Safitri ED,
Ranakusuma RW, Saldi SRF, Azwar MK, Marsigit J, Pitoyo Y and
Widyaningsih W: Risk factors and laboratory test results associated
with severe illness and mortality in COVID-19 patients: A
systematic review. Acta Med Indones. 52:227–245. 2020.PubMed/NCBI
|
|
30
|
Tay MZ, Poh CM, Rénia L, MacAry PA and Ng
LFP: The trinity of COVID-19: Immunity, inflammation and
intervention. Nat Rev Immunol. 20:363–374. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Apicella M, Campopiano MC, Mantuano M,
Mazoni L, Coppelli A and Del Prato S: COVID-19 in people with
diabetes: Understanding the reasons for worse outcomes. Lancet
Diabetes Endocrinol. 8:782–792. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Opal SM, Girard TD and Ely EW: The
immunopathogenesis of sepsis in elderly patients. Clin Infect Dis.
41 (Suppl 7):S504–S512. 2005.PubMed/NCBI View
Article : Google Scholar
|
|
33
|
Petrie JR, Guzik TJ and Touyz RM:
Diabetes, hypertension, and cardiovascular disease: Clinical
insights and vascular mechanisms. Can J Cardiol. 34:575–584.
2018.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Liu Z, Bai X, Han X, Jiang W, Qiu L, Chen
S and Yu X: The association of diabetes and the prognosis of
COVID-19 patients: A retrospective study. Diabetes Res Clin Pract.
169(108386)2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Gagliardi I, Patella G, Michael A, Serra
R, Provenzano M and Andreucci M: COVID-19 and the kidney: From
epidemiology to clinical practice. J Clin Med.
9(2506)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Conti P and Younes A: Coronavirus
COV-19/SARS-CoV-2 affects women less than men: Clinical response to
viral infection. J Biol Regul Homeost Agents. 34:339–343.
2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Liu J, Ji H, Zheng W, Wu X, Zhu JJ, Arnold
AP and Sandberg K: Sex differences in renal angiotensin converting
enzyme 2 (ACE2) activity are 17β-oestradiol-dependent and sex
chromosome-independent. Biol Sex Differ. 1(6)2010.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Benjamin BK, Qiu C, Han Z, Lu W, Sun G,
Qin X, Wang X, Wang X, Li R and Pan L: The association between
type-2 diabetes duration and major adverse cardiac events after
percutaneous coronary intervention. J Diabetes Res. 2021:1–9.
2021.
|
|
39
|
International Diabetes Federation: IDF
Diabetes Atlas, ninth edition 2019. https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf.
|
|
40
|
Cariou B, Hadjadj S, Wargny M, Pichelin M,
Al-Salameh A, Allix I, Amadou C, Arnault G, Baudoux F, Bauduceau B,
et al: Phenotypic characteristics and prognosis of inpatients with
COVID-19 and diabetes: The CORONADO study. Diabetologia.
63:1500–1515. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Varga Z, Flammer AJ, Steiger P, Haberecker
M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka
F and Moch H: Endothelial cell infection and endotheliitis in
COVID-19. Lancet. 395:1417–1418. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Zhang N, Wang C, Zhu F, Mao H, Bai P, Chen
LL, Zeng T, Peng MM, Qiu KL, Wang Y, et al: Risk factors for poor
outcomes of diabetes patients with COVID-19: A single-center,
retrospective study in early outbreak in China. Front Endocrinol
(Lausanne). 11(571037)2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Pranata R, Lim MA, Huang I, Raharjo SB and
Lukito AA: Hypertension is associated with increased mortality and
severity of disease in COVID-19 pneumonia: A systematic review,
meta-analysis and meta-regression. J Renin Angiotensin Aldosterone
Syst. 21(1470320320926899)2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo
Q, Ji R, Wang H, Wang Y and Zhou Y: Prevalence of comorbidities and
its effects in patients infected with SARS-CoV-2: A systematic
review and meta-analysis. Int J Infect Dis. 94:91–95.
2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Mudatsir M, Fajar JK, Wulandari L,
Soegiarto G, Ilmawan M, Purnamasari Y, Mahdi BA, Jayanto GD,
Suhendra S, Setianingsih YA, et al: Predictors of COVID-19
severity: A systematic review and meta-analysis. F1000Research.
9(1107)2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Callender LA, Curran M, Bates SM, Mairesse
M, Weigandt J and Betts CJ: The Impact of Pre-existing
Comorbidities and Therapeutic Interventions on COVID-19. Front
Immunol. 11(1991)2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Azevedo RB, Botelho BG, Hollanda JVG,
Ferreira LVL, Junqueira de Andrade LZ, Oei SSML, Mello TS and
Muxfeldt ES: Covid-19 and the cardiovascular system: A
comprehensive review. J Hum Hypertens. 35:4–11. 2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Colussi G, Da Porto A and Cavarape A:
Hypertension and type 2 diabetes: Lights and shadows about
causality. J Hum Hypertens. 34:91–93. 2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian
C, Qin R, Wang H, Shen Y, Du K, et al: Diabetes is a risk factor
for the progression and prognosis of COVID-19. Diabetes Metab Res
Rev. 36(e3319)2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Siddiqi HK and Mehra MR: COVID-19 illness
in native and immunosuppressed states: A clinical-therapeutic
staging proposal. J Hear Lung Transplant. 39:405–407.
2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Windham S, Wilson MP, Fling C, Sheneman D,
Wand T, Babcock L, MaWhinney S and Erlandson KM: Elevated
glycohemoglobin is linked to critical illness in COVID-19: A
retrospective analysis. Ther Adv Infect Dis.
8(20499361211027390)2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Klein OL, Krishnan JA, Glick S and Smith
LJ: Systematic review of the association between lung function and
type 2 diabetes mellitus. Diabet Med. 27:977–987. 2010.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Maan HB, Meo SA, Al Rouq F, Meo IMU,
Gacuan ME and Alkhalifah JM: Effect of glycated hemoglobin (HbA1c)
and duration of disease on lung functions in type 2 diabetic
patients. Int J Environ Res Public Health. 18(6970)2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Gautret P, Lagier JC, Parola P, Hoang VT,
Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE,
et al: Hydroxychloroquine and azithromycin as a treatment of
COVID-19: Results of an open-label non-randomized clinical trial.
Int J Antimicrob Agents. 56(105949)2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Chou HW, Wang JL, Chang CH, Lee JJ, Shau
WY and Lai MS: Risk of severe dysglycemia among diabetic patients
receiving levofloxacin, ciprofloxacin, or moxifloxacin in Taiwan.
Clin Infect Dis. 57:971–980. 2013.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Chen C, Zhang Y, Zhao X, Tao M, Yan W and
Fu Y: Hypoalbuminemia-an indicator of the severity and prognosis of
COVID-19 patients: A multicentre retrospective analysis. Infect
Drug Resist. 14:3699–3710. 2021.PubMed/NCBI View Article : Google Scholar
|