1. Introduction
Haemophilia represents an inherited pathological
condition that is X-linked; it is a bleeding disorder due to low
levels of clotting factors: Factor VIII for type A and factor IX
for type B. According to the circulating levels of clotting factor,
the condition may be severe (<1%), moderate (1-5%) or mild
(>5%).
Prophylactic and therapeutic administration of
clotting factors have changed the clinical evolution and life
quality of the haemophilic patient. It was presumed that early
administration of clotting factors (between years 1 and 2 of age)
may prevent or alleviate the development of joint pathology.
However, this was not always the case, due to various factors
(socio-economic and familial factors, inhibitor development,
recurrent trauma).
In the long term, bleeding into the joints is the
common clinical manifestation, affecting ankles, knees and elbows.
Intra-articular bleeding leads to hemosiderin deposits into the
synovium. Intra-articular iron and cytokines (IL-1, TNF-α) have
major roles in chronic proliferative synovitis, hypervascularity,
cartilage damage and bone destruction.
Chronic haemophilic arthropathy features a swollen
joint, with synovial hypertrophy and marginal bony production,
malalignment, reduced mobility and chronic pain. Several
classification systems have been proposed to quantify and monitor
the severity of arthropathy based on clinical and imagistic
findings.
Clinical findings of the physical and functional
examination were included in several scoring systems. In clinical
settings, an early scoring system based on the severity of
arthropathy displays 4 grades. Grade I: Transitory synovitis with
no post-bleeding sequel; the joint goes back to the pre-bleeding
stage once the hemarthrosis has subsided. Grade II: Permanent
synovitis with joint enlargement, synovial thickening and
limitation of movements. Grade III: Chronic arthropathy-in addition
to the symptoms of grade II, there are axial deformities and muscle
atrophy. Grade IV: Fibrous or bony ankylosis (1).
In 1977, Arnold and Hilgartner (2) proposed a classification of knee
haemophilic arthropathy based on plain radiograph. Stage 0: Normal
joint; stage I: No skeletal abnormalities, soft-tissue swelling is
present; stage II: Osteoporosis and overgrowth of the epiphysis, no
cysts, no narrowing of the cartilage space; stage III: Early
subchondral bone cysts, squaring of the patella, widened notch of
the distal femur or humerus, preservation of the cartilage space;
stage IV: Findings of stage III, but more advanced; narrowed
cartilage space; stage V: Fibrous joint contractures, loss of the
joint cartilage space, extensive enlargement of the epiphyses with
substantial disorganization of the joint (2). Conventional X-ray was also used for
the Pettersson score (1980) and covers 8 items with a total of 13
points. Severe cases score 0-3 points, moderate 4-8 and mild
>9(3). Magnetic resonance
imaging (MRI) is a more sensitive tool to detect changes in the
joint; various scoring systems were developed and they need
standardization (4). Ultrasound
examination (gray-scale and color Doppler) has advantages in terms
of costs, availability and accessibility and is able to identify
synovial hypertrophy and hypervascularity. Since 2006, the
Haemophilia Joint Health Score is largely accepted. It scores 3
joints bilaterally (elbow, knee, ankle) and gait, with values up to
124 (the higher the score, the worse).
Chronic arthropathy is subject to conservative and
surgical management. Conservative therapies are the first option
aiming to reduce intra-articular bleeding and provide pain control
and functional improvement. Conservative measures include
physiotherapy, oral drug administration for analgesia and
intra-articular administration of various agents. Synovectomy,
excision or destruction of hypertrophic synovium, may be performed
through different modalities: Open surgery, arthroscopic,
radionuclide or chemical intervention. Surgical therapies may be
explored after the failure of conservative measures and following a
thorough evaluation (5).
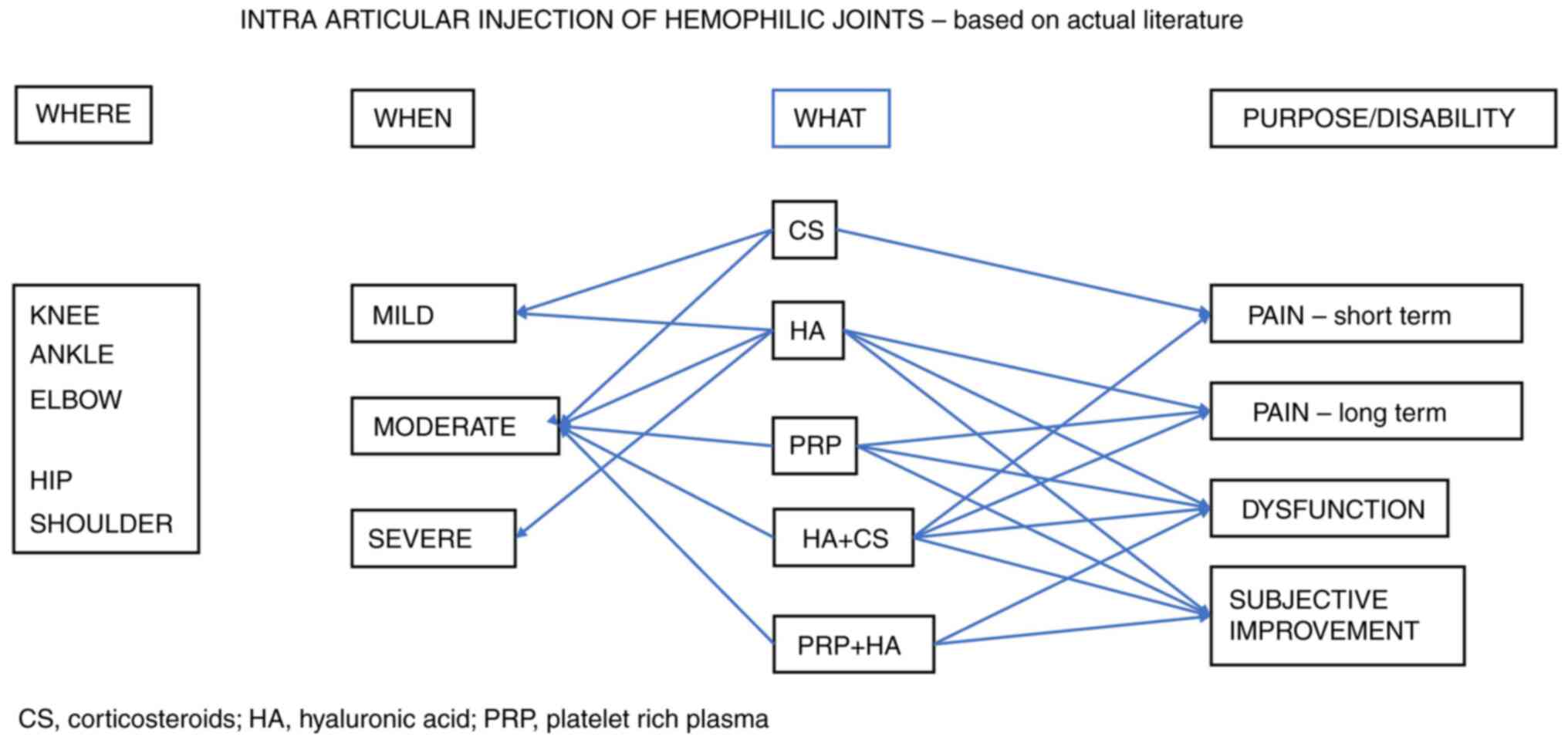
The present study focused on intra-articular
injection of agents to reduce pain, to improve the functional
status and to increase the quality of life. The interest toward
this method arose in the early 1990 and grew as new technologies
came into being. Beginning with corticosteroids (CS) and advancing
to hyaluronic acid (HA) and platelet-rich plasma (PRP), researchers
studied different protocols. The rationale of intra-articular
treatments lies in the assumption that advanced haemophilic
arthropathy is similar to idiopathic osteoarthritis, although it is
clear that the pathologic mechanisms differ.
2. Methods
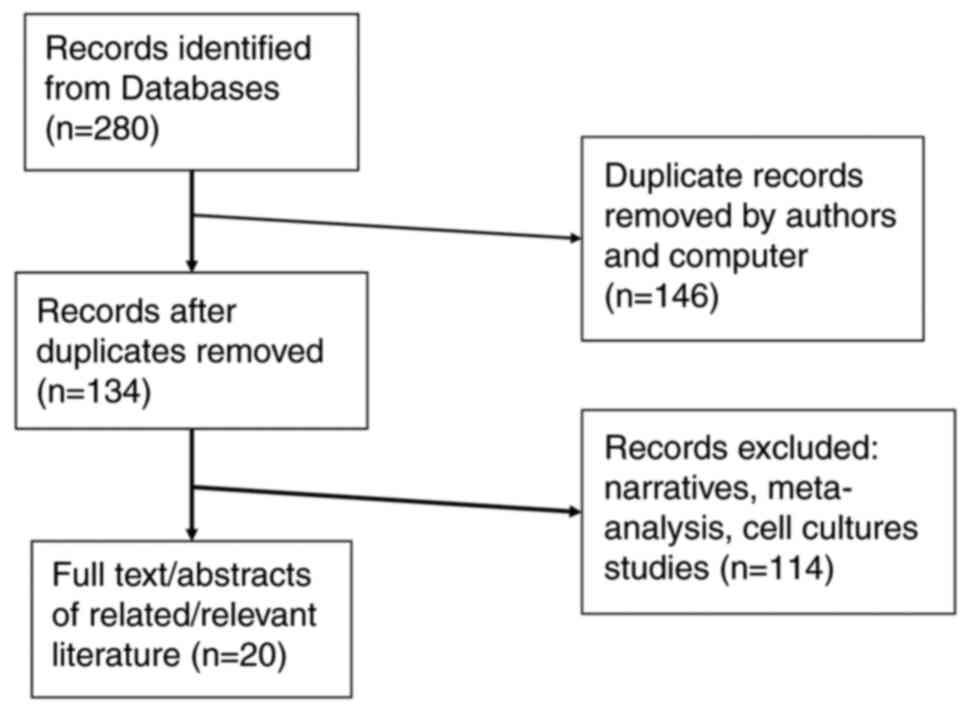
A literature search of studies published until
January 2023 was performed in the electronic databases
PubMed/Medline (https://pubmed.ncbi.nlm.nih.gov/) and Cochrane Library
(https://www.cochranelibrary.com/) and
using the Google Scholar search engine, with the following MeSH
terms: Intra-articular injection AND haemophilia. Two independent
authors (DP and DC) extracted a total of 280 papers, written in the
English language, with available abstracts. After excluding
duplicates, 134 papers were examined. Papers containing
meta-analyses and narratives were removed, as well as studies on
cell cultures and animal models (Fig.
1).
The final research focused on 20 papers, which were
grouped in terms of the following topics: HA, PRP, CS, combined
therapies and comparative studies (summary, see Table I).
 | Table IStudies selected for analysis and
their main characteristics. |
Table I
Studies selected for analysis and
their main characteristics.
| First author,
year | Features | No. of
patients/joints | Protocol | Timing of
evaluation | Evaluation
methods/parameters | Outcome | Comments | (Refs.) |
|---|
| Shupak, 1988 | Pilot study,
prospective, non-randomized, non-controlled | 10 patients, 19
joints (10 knees, 4 elbows, 3 shoulders, 1 ankle, 1 wrist), all
grades of severity | CS
(methylpred-nisolone) 80 mg/knee 40 mg/other joints | 24 h 4 weeks 8
weeks | Subjective
improvement, Frequency of bleeds, Radiological staging, Synovial
fluid analysis | 24 h: 79%
improvement; 8 weeks: 58% continued subjective improvement; 8
weeks: Reduced number of hemarthroses (from 7.7 to 1.9) and of
amount of clotting factor (from 7616 to 2315 units) | | (6) |
| Rodríguez-Merchán,
1994 | Prospective | 10 patients; 10
knees | CS
(methylpred-nisolone) | 1 year | X-ray;
Ultrasound | 4/10 excellent;
3/10 good; 2/10 fair; 1/10 poor | Lack of joint
severity stratification | (7) |
| Fernández-Palazzi,
1997 | Retrospective,
non-controlled, non-randomized | 34 patients; 35
joints (31 knees, 2 ankles, 2 shoulders); Grades III and IV | CS (dexame thasone,
short- and long-acting combination) | 1,5 years mean (1-2
years) | Subjective;
Objective (clinical-pain, ROM, joint thickness; function-ability to
perform ADL) |
Subjective/objective results: Good:
54/63%; Fair: 34/26%; Poor: 11/11% | | (8) |
| Wallny, 2000 | Prospective,
non-controlled, non-randomized | 20 patients; 21
knees | LMWHA (Hyalart 20
mg) x 5 weekly | 3 months; 24
months | Clinical (pain VAS,
WFH); Function (Aichroth score for knee); Imagistic (X-ray
Pettersson score) | 3 months:
Improvement of clinical and functional parameters: 15 out of 21
knees. 24 months: Improvement persisted in 10 knees | Lack of joint
severity strati-fication For 6 out of 21 knees, no pain improvement
was reported at 3 months. 2 patients required arthros-copical
debride ment 14 and 15 months later | (9) |
| Fernández-Palazzi,
2002 | Prospective,
non-randomized, non-controlled | 25 (23 type A; 2
type B haemo-philia); 29 joints (17 knees, 6 shoulders, 4 an-kles,
one elbow, one hip); Grade III arthropathies | HMWHA 3 weekly
injections (Synvisc) | One month; Maximum
10 years; Average 10,5 months | Clinical (pain VAS,
mobility-ROM, use of joint); Joint diameter; Imagistic (X-ray) | Pain relief;
Increase in mobility; Increase n use of the joint; No alteration of
X-ray | Great variability
of follow-up intervals. No improvement in 10,3% | (1) |
| Carulli, 2012 | Prospective,
non-randomized, non-controlled | 46 patients (77
joints, 14 elbows, 30 knees, 32 ankles); 60% with severe
arthropathy | LMWHA (Orthovisc,
Hyalgan, Hyalu-brix) 3-5 weekly injections/cycle, at least 2 yearly
cycles | 6, 12 months, then
yearly (average 6,3 years, 2-11 years) | Clinical (pain
VAS); Imagistic (X-ray, Pettersson score); Functional (ROM, WFH,
SF-36) | Short-term: Pain
relief, functional improvement; Long-term: Regression of the
effect, particularly function | Elbow: After the
first cycle 2/18 needed further treatments (drugs, physiotherapy);
Knee: Long-term 6/30 needed surgery (2-4years) Ankle: Short-term
10/32 needed further treatments (drugs, physiotherapy) | (10) |
| Carulli, 2013 | Case series,
prospective | 27 patients (23
type A; 4 type B haemophilia); 27 knees | LMWHA yearly.
2003-2006: Hyalganx 5/2- week interval; 2007-2010: Hyalubrix x 3/4-
week interval, 2-4 cycles | Short-term: 6 and
12 months Long-term yearly; Following period: 6,7 years (2-8) | Clinical (pain VAS,
WFH); Imagistic (X-rays Pettersson score) Function (WOMAC) Quality
of life (SF-36) | Short-term: All
items, best on WFH, VAS, SF 36; Long-term Small decline, better
than pre-treat, best on WOMAC and ROM flexion) | Lack of joint
severity stratification. 5 patients required total arthroplasty in
a 2-4 year interval after the last administration | (11) |
| Zelada, 2013 | Prospective,
non-randomized, non-controlled 2-4 (Kelgreen Lawrence) | 4 patients, 27
joints (14 knees, 9 ankles, 4 elbows); severity | Intra-articular
lavage (saline), LMWHA + triamcinolone + ropivacaine | 1 and 3 months | Clinical (pain
VAS); Function (WOMAC); Quality of life (SF-36) | Improvement of all
parameters at one month and persistence at 3 months; 10 out of 14
patients were satisfied at 3 months | No stratification
according to joint severity | (12) |
| Teyssler, 2014 | Case series,
prospective | 6 patients (6
ankles); Haemophilia type A; chronic synovitis | PRP, 3-5 ml | 2 months | Clinical (pain,
VAS); Functional (HJHS); MRI | Clinically
significant improvement (pain); HJHS improvement, not significant;
MRI: Mild synovial hypertrophy regression (3 out of 8 joints) | Joint severity
varied from mild to severe | (13) |
| Martin, 2017 | (Retrospective and
prospective arms), Non-randomized, non-controlled | 25 patients, 45
joints (14 ankles, 18 knees, 13 elbows); type A and B haemophilia;
different grades of severity | 40 mg CS
(triamcinolone acetonide) + lidocaine 1%, repeated at least 3
months apart | 4; 8; 12; 16
weeks | Clinical (pain,
VAS, HJHS); X-ray (Pettersson score); Ultrasound exam (greyscale
and color Doppler) | Pain relief in the
first 48 h, up to 4-8 weeks; Reduced hypervascularity within 1-4
weeks | A low Pettersson
score and type B haemophilia were associated with a longer pain
relief period | (14) |
| Rezende, 2017 | Case series,
prospective, non-randomized, non-controlled | 14 patients, 40
joints (knee, ankle, elbow, shoulder); Severe arthropathy | Saline solution
lavage, followed by HA and triamcinolone injection | 1, 3, 6 and 12
months | Functional tests
(balance, speed); Bleeding events | Functional
improvement (symmetry,speed); Reduction of bleeding events at 1
year | 2 knees required
joint replacement after one year | (15) |
| Caviglia, 2017 | Prospective,
non-randomized, non-controlled | 19 patients (17
type A; 1 type B haemophilia); 28 joints (2 ankle, 7 elbow, 19
knee) | PRP, 3-7 ml
according to joint size | 3 and 6 months | Clinical (pain VAS,
ROM);Function (HJHS); MRI (synovial thickening); Number of bleeding
episodes | Decrease in joint
bleeding episodes; Pain relief; ROM improved (not significant for
flexion); MRI: Reduction in thickness of the synovium | Lack of severity
stratification of arthropathy | (16) |
| Patel, 2018 | Retrospective,
non-controlled (poster presentation) | 10 patients (2
knees, 12 ankles); moderate and severe arthropathy | CS (7 joints); CS +
HA (7 joints) | 1 year | Clinical (pain VAS,
HJHS); Bleeding rate; Functional (HAL) | Both groups
improved (pain, function); Bleeding rate unchanged; CS + HA
achieved a significantly better result than CS alone | 4 patients from CS
group required one more CS injection within a year | (17) |
| Poursac, 2018 | Prospective,
non-controlled, non-randomized | 14 patients (16
ankles) | LMWHA single
injection (Hyalgan 20 mg/2 ml) under ultrasound guidance | 3 and 6 months | Clinical (pain
VAS); Function (AOFAS ankle score, WFH); Imagistic (X-ray
Pettersson) | Pain relief in 78%
patients at 3 months; Significant pain relief in 56% at 3 months,
sustainable at 6 months | Lack of joint
severity stratification | (18) |
| Li, 2019 | Prospective,
non-randomized, open-label trial | 22 patients (22
knees), haemophilia type A (n=20), haemophilia type B (n=2) | PRP, 2 ml (11
knees); HA, 2,5 ml, 5 weekly injections (11 knees) | 1, 2, 3 and 6
months | Clinical (pain VAS,
ROM); Functional WOMAC; SF-36; Ultrasound (hyperemia score) | Both were effective
at 6 months; PRP showed better results on pain, ROM, WOMAC,
ultrasound exam; SF-36 was similar | | (19) |
| Liou, 2021 | Case series,
randomized, non-controlled | 5 patients (5
knees) haemophilia type A | Course 1: LMWHA,
PRP or LMWHA + PRP; Course 2: LMWHA + PRP (LMWHA Hya-Joint 2,5 ml;
PRP 2,5 ml) | Monthly, up to 1,5
years | Clinical (pain VAS,
HJHS) X-ray every 3 months (Pettersson score) | Improvement of pain
and HJHS for all regimens | Too small a sample
Discussion about the volume of injectate | (20) |
| Carulli, 2020 | Prospective,
non-randomized, non-controlled | 14 patients, 21
joints (ankles and knees), mild-to-moderate severity | LMWHA (Sinovial
Forte), 3 monthly injections/knee, 2 monthly injections/ankle | 1 year, then every
6 months (median, 20 months) | Clinical (pain VAS,
ROM); X-ray (Pettersson); Ultrasound (synovial status, effusion);
Functional (HJHS); Annual bleeding rate | Pain, HJHS, annual
bleeding rate improved significantly at 1 year; ROM improved, not
statistically significant | | (21) |
| Duan, 2022 | Prospective,
randomized, parallel group, placebo-controlled, double-blinded | 190 patients, 190
patients, | Group I: Three
weekly PRP injections; Group II: Three weekly saline
injections | Up to 24
months | Clinical (pain VAS,
HJHS); Functional (WOMAC); SF-36; MRI | No difference
between groups at all time-points for any parameter | | (22) |
| Landro, 2021 | Prospective,
non-randomized, parallel | 21 patients with
bilateral knee involvement | Right knee: PRP;
Left knee: PRP + LMWHA | 3 and 6 months | Clinical (pain
VAS); Functional (HJHS); Bleeding episodes; Subjective
evaluation | Both knees noted
pain relief and improved function at 3 and 6 months, no difference
between left and right knee; Subjective improv ement in left
knee | | (23) |
| Taylor, 2022 | Pilot study,
non-randomized, non-controlled | 24 patients, 26
ankles | LMWHA (Ostenil
Plus), 2 injections 6 months apart | Every 3 months for
1 year | Clinical (pain
VAS); Functional (HJHS); Quality of life EQ-5D-5L | Significant pain
relief and functional improvement at all time-points; No change in
EQ-5D-5L | Lack of joint
severity stratification | (24) |
Of the 20 studies analyzed (1,6-24),
17 were prospective, two were retrospective (7,16) and
one had two arms, prospective and retrospective (14). A total of 17 studies were available
as full-texts and 3 were only available as abstracts (7,17,18);
however, it was possible to extract the main data to include them
in the current study. In addition, two articles were pilot studies
(6,24) and 4 were case series (12,13,15,20).
None of the studies, except for one (22), were placebo-controlled studies due
to moral considerations, as stated by the authors.
All of the papers reported prophylactic factor
replacement, considering intra-articular injection as a minor
surgery for haemophiliacs. The aim was to increase the patients'
factor level to 50% immediately before and 24 h after the
injection. Under these conditions, the bleeding risks are reduced
and the safety of the procedure is assured, as stated in all of the
papers.
As the main agent for intra-articular injection, 4
papers (109 joints) followed exclusively CS administration
(6,7,8,14), 7
studies (196 joints) HA (1,9-11,18,21)
and 3 studies PRP (243 joints) (13,16,22). A
total of 2 papers focused on CS plus HA (55 joints) (15,17)
and 2 papers on HA plus PRP (48 joints) (20,23).
Furthermore, one paper compared HA with PRP (22 joints) (19). The severity of arthropathy was mild
to moderate in one study (21 joints) (21) and moderate and severe in 4 papers
(127 joints) (1,10,15,17);
the remaining studies included all grades of severity and did not
perform any stratification.
As for the involved joints, most of the cited papers
addressed a variety of affected joints in the same approach (knee,
ankle, shoulder, wrist). A total of 7 papers focused on the knee
(7,9,11,19,20,22,23)
and 3 papers on the ankle (13,18,24).
3. Corticosteroids
Intra-articular administration of CS has a long
record in the literature. A total of 4 papers (109 joints) dating
back from 1988 were found.
A small pilot study on 10 patients (19 joints: Knee,
elbow, shoulder, ankle, wrist) recommended to obey at least one of
the following indications for intra-articular methylprednisolone:
Chronic synovitis of at least 2 months' duration (heat, swelling,
tenderness), recurrent hemarthrosis not responding (coagulation
factor replacement, rest, physiotherapy) or advanced arthropathy
without any signs of active inflammation. Short-term results (24 h,
4 and 8 weeks) indicated a clinically significant subjective
improvement, reduction of the number of hemarthroses and of the
amount of necessary clotting factor at all time-points of the
study. The authors underlined the value of CS in the short-term,
for early stages (prevention of progression) as well as for
advanced stages (6). Another small
prospective study on 10 knees with chronic synovitis with
intra-articular methylprednisolone followed imagistic evolution
(X-ray and ultrasound) at one year. They found excellent and good
evolution for 7 out of 10 knees, fair for 2 out of 10 and poor for
one knee. There was no information on joint severity (7).
A retrospective study on 34 patients (35 joints:
Knee, ankle, shoulder) with severe advanced chronic synovitis
(grades III and IV) received intra-articular dexamethasone (a
combination of short- and long-acting forms).
Subjective and objective outcomes were good (54 and
63%, respectively), fair (34 and 26%, respectively) and poor (both
11%) after an average follow-up period of 1,5 years (8).
One comprehensive study (a retrospective and a
prospective arm) included 45 joints (ankles, knees, elbows; various
grades of severity) to receive intra-articular triamcinolone under
ultrasound guidance. The indications were as follows:
Unresponsiveness, inability, unwillingness or contraindication to
alternative treatment strategies such as physical therapy, oral
pain or anti-inflammatory agents. Pain relief was achieved within
48 h after injection, persisted at least 4 weeks and in certain
patients 4 months. Ultrasound scan demonstrated resolution of
hypervascularity within 1-4 weeks. A low Pettersson score (between
4 and 8) and haemophilia type B were associated with a longer pain
relief period (14).
4. Hyaluronic acid
Of the 7 papers dealing with HA injection, six
studies used low-molecular-weight HA (LMWHA) and one
high-molecular-weight HA (HMWHA). Only two studies used
stratification according to joint severity (1,10).
The first published prospective study from 2020 on
20 patients (21 knees) with 5 weekly injections of LMWHA reported
improvement in the clinical and functional scores at 3 months (15
out of 21 knees), persisting at 24 months in 10 out of 21 knees.
Failure of pain relief at 3 months was noted in 6 out of 21 knees
and arthroscopic debridement was performed in 2 patients after 14
and 15 months. It is important to note that there was no initial
severity assessment or stratification of joint arthropathy
(9).
Intra-articular injection of elbows, knees and
ankles (77 joints) with different LMWHA preparations, according to
specific protocols (3-5 weekly doses/cycle, at least 2 yearly
cycles) offered pain relief and functional improvement in the
short-term and persistence of the benefits in the long-term, but at
a lower level. With 60% of patients with severe joint involvement,
the paper mentioned that there was a need for further therapies
(drugs, physiotherapy) after the first cycle in 2 out of 18 elbows
and in 10 out of 32 ankles. In the long-term (2-4 years), 6 out of
30 knees required surgery. The authors stated that the need for
surgery was delayed (10). The same
study group published another paper on chronic knee arthropathy and
concluded that, in the short-term, all parameters improved, with
the best evolution of pain relief, function (World Federation
Haemophilia score) and quality of life (Short Form-36
questionnaire). In the long-term, there was a small decline in all
items, with better values compared to pre-treatment and best
evolution of functional aspects (Western Ontario and McMaster
Universities arthritis index and range of motion). No joint
severity stratification was performed (11).
A single intra-articular injection of LMWHA into the
ankle (16 joints) under ultrasound guidance was reported to reduce
pain to a certain extent in 78% of cases and this was statistically
significant in 56% of cases at 3 months, persisting at 6 months. No
stratification of joint severity arthropathy was provided (18). Another pilot study on 26 ankles (24
patients) to receive two intra-articular LMWHA injections 6 months
apart reported pain relief and functional improvement over 1 year.
Quality of life remained unchanged (24).
A small prospective study on symptomatic
mild-to-moderate arthropathy of knee and ankles indicated that
LMWHA (specific protocols: 3 monthly injections for knee, 2 monthly
injections for ankle) offered clinically significant pain and
functional improvement and reduction of the bleeding rate at one
year. Ultrasound evaluation of the synovial status and joint
effusion confirmed the clinical evolution. The authors concluded
that early stages of arthropathy were successfully treated with
LMWHA (21).
For severe chronic arthropathy (grade III) of
ankles, knees, hips, shoulders and elbows, 3 weekly injections of
HMWHA offered pain relief and functional improvement at one month,
with a variable period of monitoring (up to 10 years, average 10,5
months). No X-ray modification was noted. 10,3% of joints failed to
improve, mainly due to the high degree of joint involvement
(1).
5. Platelet-rich plasma
A total of 3 papers reported on intra-articular
administration of PRP. In a small case series (6 patients, 8
ankles) an intra-articular injection of 3-5 ml PRP was followed by
clinically significant pain reduction, functional improvement (not
significant) and, in 3 out 8 joints, mild synovial hypertrophy
regression at 2 months (13). A
prospective study on 28 joints (ankle, elbow, knee) that received
3-7 ml PRP (according to joint size) found significant pain and
functional improvement, reduction of number of bleeding events and
reduction in thickness of the synovium (according to MRI) at 3 and
6 months (16). Neither of the
papers reported any complications, suggesting that the procedure
was safe.
One single prospective, parallel-group,
double-blinded, placebo-controlled, randomized clinical trial
included 190 patients (190 knees) to receive three weekly PRP
injections vs. three saline injections and found that, at 24
months, there was no difference in terms of clinical, functional
and quality of life parameters (22).
6. Comparative studies and combination
strategies
A comparative prospective non-randomized study on 22
knees receiving either PRP or HA indicated that both therapies were
effective at 6 months, with better results for PRP in terms of
pain, function and ultrasound imaging (synovial hypertrophy) and a
similar evolution of quality of life (19).
In order to increase the clinical benefits of
intra-articular therapies, researchers combined CS (accredited with
short-time effects) and HA (presumed to have a long-term effect). A
small retrospective study on 14 joints (knee, ankle) comparatively
observed the effect of CS vs. CS and HA administration on moderate
to severe arthropathy. At one year, both strategies offered pain
and functional improvement, with a significantly better evolution
for the combination of CS and HA. A total of 4 out of 7 joints
treated with CCS required a second injection within a year
(17).
Another study suggested that the effect of
viscosupplementation was able to be improved by joint lavage and
the addition of CS. The rationale for lavage was to remove the
intra-articular debris and factors causing inflammation. CS are
known to improve the results of lavage and HA injection in
osteoarthritis (25). A prospective
study on 14 patients (27 joints: Knee, ankle, elbow) with different
grades of severity (II-IV Arnold-Hilgartner) to receive lavage with
saline solution followed by HA and CS administration improved
clinical, functional and quality of life parameters at 1 month. The
changes were obvious at 3 months with a relatively low level of
statistical significance (12). A
case series of 40 joints (knee, ankle, elbow and shoulder) with
severe arthropathy (Arnold-Hilgartner stages III to V) were
subjected to the same technique. At all time-points of observation
of the study (1, 3, 6 and 12 months), there was significant
functional improvement (balance, speed, activities of daily living)
and reduction of the frequency of bleeding episodes. However, 2
knees required total replacement after one year due to persistent
pain (15).
With the same purpose of augmenting the biological
and clinical effects, the association between HA and PRP was tested
in a case series study of 5 knees with chronic arthropathy with
intra-articular courses. The first course consisted of one of the
following: HA, PRP or HA plus PRP; the second course consisted of
HA plus PRP. Up to 1,5 years, pain relief and functional
improvement were noted for all knees, although only limited
conclusions can be drawn on such a small sample. Certain practical
issues arise concerning the mode of combining the two ingredients,
as the concomitant administration may result in a large volume that
is not anatomically normal to fill the joint space. The suggested
procedure for the combined therapy was to administer 3 weekly
injections of HA followed by PRP in the fourth week (20).
A prospective, non-randomized and parallel study on
21 patients with bilateral knee involvement compared one knee
receiving PRP with the contralateral knee receiving PRP + HA. At 3
and 6 months, both knees improved significantly (pain relief,
function, bleeding episodes and quality of life); there was no
difference between them, while there was a subjective better
evolution in the PRP + HA knees (23).
7. Conclusions
In the present review, 20 clinical studies were
analyzed with a total number of 699 joints with chronic haemophilic
arthropathy in different stages of severity, affecting different
joints and receiving various intra-articular therapies, either
unique agents or combinations. Most studies lack the double-blinded
arm due to ethical considerations. The heterogeneity of the
research prevents us from drawing clear-cut conclusions. However,
certain features are to be underlined.
Numerous CS preparations are available for
intra-articular use: Dexamethasone, betamethasone, triamcinolone,
methylprednisolone and hydrocortisone. Triamcinolone (acetonide or
hexacetonide) is preferred due to its decreased solubility and thus
longer intra-articular duration of action. Numerous authors add
lidocaine for numerous reasons: Lidocaine elicits immediate
analgesic effects, which in turn aid in the confirmation of the
correct injection site when ultrasound is not available; it also
reduces the post-injection flare induced by precipitating CS
crystals, as well as CS-associated soft tissue atrophy (26).
Intra-articular administration of CS has a
relatively longer record of study, is safe and able to provide a
short-term benefit in terms of pain relief and functional
improvement, with the necessity to repeat the procedure within one
year. Indications are all grades of severity of joint involvement,
even in advanced stages or refractory cases.
There is an association between the Pettersson score
and pain relief period following CS intra-articular injection
(14). Pain-inducing inflammatory
and angiopoietin changes in CS-responsive subjects may not prevail
in early or late stages and the results of such treatment may be
failure. In the early stages, pain may be induced by joint
malalignment, and in the late stages by scarred tissue. Another
interesting observation was that patients with haemophilia type B
had a longer duration of pain relief than those with type A,
consistent with previous studies. This may be explained by the fact
that patients with haemophilia A have more frequent bleeding events
and more severe forms of arthropathy than those with type B and the
same amount of clotting factor deficiency (27).
Certain researchers have agreed that CS
intra-articular injections are safe, while there is no formal
consensus on the optimal frequency to repeat injections. There is a
common practice to wait 3 months before re-injecting triamcinolone
into the same joint. This may be a reasonable interval to assure at
least 8 weeks of pain relief. Systemic absorption of a fraction of
injected CS may occur, but it is presumed to be of limited
significance, since the intra-articular dose is 40 mg
triamcinolone, equivalent to 50 mg oral prednisolone (14). Triamcinolone (in the form of
acetonide or hexacetonide) is preferred due to its decreased
solubility and a longer intra-articular duration of action
(28). Intra-articular
dexamethasone may follow a course of 3 injections at 3-week
intervals (29).
HA is a linear polysaccharide that constitutes the
major part of the extracellular matrix of human articular
cartilage. It is essential for the viscous-elastic and mechanical
properties of synovial fluid, as it produces shock absorption,
reduces pain and has anti-inflammatory and chondroprotective
effects. The classification of HA preparations includes LMW
(500-2,000 kiloDa) and HMW (6,000-7,000 kDa) agents. LMWHA achieves
maximum concentrations in the joint and reduces inflammation but
has a lower elastoviscosity than native HA. HMWHA agents result in
a better increase in fluid retention into the joint and have a
stronger anti-inflammatory effect (30). On the whole, HA significantly
improved the clinical and functional status. One study indicated
that early stages of arthropathy improved significantly (11) and another paper reported improvement
of severe arthropathy, with a 10% failure rate (1). A low knee X-ray Pettersson score was
associated with a better outcome after treatment (10).
In 2012, a review stated that, taking into account
the papers published by then, potential haemophilic candidates for
HA are young patients, with moderate pain and disability, with no
severe deformities, who are unwilling to accept the risks of a
surgical procedure (31). HA is
accredited by numerous authors to postpone the time-point of
surgical intervention (32).
The application of PRP in haemophilic arthropathy
has raised the interest of researchers, as it contains various
growth factors that promote chondrocyte proliferation and
differentiation, stimulates synovial fibroblasts to synthetize HA,
increases anti-inflammatory factors and decreases pro-inflammatory
mediators (IL-1 and TNF-α) (33,34).
In 2020, Caviglia et al (35) proposed, as an additional mechanism
of PRP, the inhibition of the Fenton reaction. The Fenton reaction
in the haemophilic joint consists of the oxidation of hemoglobin to
methemoglobin and the generation of toxic hydroxyl radicals that
induce chondrocyte death, alter the synthesis and stability of the
cartilaginous matrix and promote synovial hyperplasia and
inflammation.
A small number of studies reported on the use of PRP
in haemophilic arthropathy. They ascertain that, in the short-term
(1-2 months), there may be a clinically significant improvement,
but in the long-term (24 months), there was no benefit.
Combining the above-mentioned agents may lead to
better results. HA and CS, either as one injection or following
joint lavage with saline, were used mainly for severe arthropathy.
The lavage technique must be carried out under anesthesia in the
operating room and the risk of infection is increased, as indicated
by a study on osteoarthritic management (36). Intra-articular lavage with saline
(washout) and CS administration was documented in cases of acute
hemarthrosis in children, preventing the clinical evolution toward
arthropathy. In fact, the joints of haemophilic boys who presented
with acute hemarthrosis and received washout were followed over 11
years and found to be normal (37)
(Fig. 2).
The combination of PRP and HA was used only for knee
involvement in a small number of patients, with statistically
comparable results to those of PRP alone.
The present study focused on intra-articular agents
for chronic haemophilic arthropathy and concluded that there is a
need for extensive studies on this subject, taking into account the
various grades of joint involvement and different regimens of
administration. Results should be provided for both short- and
long-term outcomes, including clinical and functional aspects as
well as subjective outcomes, including quality of life. There are
ethical aspects that prevent the implementation of blinded or
placebo-controlled arms of the studies, making the task more
difficult.
The conservative approach cannot rely only on one
modality, i.e., intra-articular agents, but on a complex
management, adding oral drugs, physiotherapy and therapeutic
exercise.
Acknowledgements
Not applicable.
Funding
Funding: The publication of this paper was supported by the
University of Medicine and Pharmacy Carol Davila, through the
institutional program Publish not Perish.
Availability of data and materials
Not applicable.
Authors' contributions
DP and DC performed the literature search and
selected the studies. MIS extracted the data from the studies. DP,
DC, MIS analysed the data and wrote the manuscript. All authors
have read and approved the final manuscript. Data authentication is
not applicable.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fernández-Palazzi F, Viso R, Boadas A,
Ruiz-Sáez A, Caviglia H and De Bosch NB: Intra-articular hyaluronic
acid in the treatment of haemophilic chronic arthropathy.
Haemophilia. 8:375–381. 2002.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Arnold WD and Hilgartner MW: Hemophilic
arthropathy. Current concepts of pathogenesis and management. J
Bone Joint Surg Am. 59:287–305. 1977.PubMed/NCBI
|
|
3
|
Pettersson H, Ahlberg A and Nilsson IM: A
radiologic classification of hemophilic arthropathy. Clin Orthop
Relat Res. 153–159. 1980.PubMed/NCBI
|
|
4
|
https://radiopaedia.org/articles/haemophilic-arthropathy.
|
|
5
|
Raffini L and Manno C: Modern management
of haemophilic arthropathy. Br J Haematol. 136:777–787.
2007.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Shupak R, Teitel J, Garvey MB and Freedman
J: Intraarticular methylprednisolone therapy in hemophilic
arthropathy. Am J Hematol. 27:26–29. 1988.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rodríguez-Merchán EC, Villar A, Orbe A and
Magallón M: Intra-articular methylprednisolone therapy in chronic
hemophilic synovitis of the knee. Rev Clin Esp. 194:480–482.
1994.PubMed/NCBI(In Spanish).
|
|
8
|
Fernández-Palazzi F, Caviglia HA, Salazar
JR, López J and Aoun R: Intraarticular dexamethasone in advanced
chronic synovitis in hemophilia. Clin Orthop Relat Res. 25–29.
1997.PubMed/NCBI
|
|
9
|
Wallny T, Brackmann HH, Semper H, Schumpe
G, Effenberger W, Hess L and Seuser A: Intra-articular hyaluronic
acid in the treatment of haemophilic arthropathy of the knee.
Clinical, radiological and sonographical assessment. Haemophilia.
6:566–570. 2000.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Carulli C, Civinini R, Martini C, Linari
S, Morfini M, Tani M and Innocenti M: Viscosupplementation in
haemophilic arthropathy: A long-term follow-up study. Haemophilia.
18:e210–e214. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Carulli C, Matassi F, Civinini R, Morfini
M, Tani M and Innocenti M: Intra-articular injections of hyaluronic
acid induce positive clinical effects in knees of patients affected
by haemophilic arthropathy. Knee. 20:36–39. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zelada F, de Almeida AM, Pailo AF,
Bolliger R, Okazaki E and de Rezende MU: Viscosupplementation in
patients with hemophilic arthropathy. Acta Ortop Bras. 21:12–17.
2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Teyssler P, Kolostova K and Bobek V: The
impact of platelet-rich plasma on chronic synovitis in hemophilia.
Acta Orthop Belg. 80:11–17. 2014.PubMed/NCBI
|
|
14
|
Martin EJ, Cooke EJ, Ceponis A, Barnes RF,
Moran CM, Holle S, Hughes TH, Moore RE and von Drygalski A:
Efficacy and safety of point-of-care ultrasound-guided
intra-articular corticosteroid joint injections in patients with
haemophilic arthropathy. Haemophilia. 23:135–143. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Rezende MU, Andrusaitis FR, Silva RT,
Okazaki E, Carneiro JD, Campos GC, Pailo AF, Frucchi R, Pasqualin T
and Villaça PR: Joint lavage followed by viscosupplementation and
triamcinolone in patients with severe haemophilic arthropathy:
Objective functional results. Haemophilia. 23:e105–e115.
2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Caviglia H, Landro ME, Daffunchio C,
Galatro G, Douglas Price AL, Salgado P and Neme D: Platelet rich
plasma for chronic synovitis treatment in patients with
haemophilia. Haemophilia. 23:613–619. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Patel VY, Stephensen D and Jawad A: The
clinical effectiveness of intra articular injections (IAI) in
patients with hemophilia (PWH). Haemophilia. 24:32–135, P027.
2018.
|
|
18
|
Poursac N, Lafarie-Castet S and Loustau C:
Efficacy on pain of a single injection of hyaluronic acid in
hemophilic arthropathy of the ankle: A prospective study.
Haemophilia. 24:32–135, P165. 2018.
|
|
19
|
Li TY, Wu YT, Chen LC, Cheng SN, Pan RY
and Chen YC: An exploratory comparison of single intra-articular
injection of platelet-rich plasma vs hyaluronic acid in treatment
of haemophilic arthropathy of the knee. Haemophilia. 25:484–492.
2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Liou IH, Lu LY, Lin KY, Yu LH, Yang SM,
Tsai MY, Tsai TH, Yeh CH, Hong YC and Yu MS: Combined
intra-articular injections of hyaluronic acid and platelet-rich
plasma for the treatment of haemophilic arthropathy: A case series
study. Haemophilia. 27:e291–e294. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Carulli C, Rizzo AR and Innocenti M,
Civinini R, Castaman G and Innocenti M: Viscosupplementation in
symptomatic haemophilic arthropathy of the knee and ankle:
Experience with a high molecular weight hyaluronic acid.
Haemophilia. 26:e198–e200. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Duan W, Su X, Yu Z, Jiang M, Zhao L,
Giannoudis P and Guo J: No benefit to platelet-rich plasma over
placebo injections in terms of pain or function in patients with
hemophilic knee arthritis: A randomized trial. Clin Orthop Relat
Res. 480:2361–2370. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Landro Carla Daffunchio Guillermo
Cambiaggi Gustavo Galatro Horacio Caviglia ME, Daffunchio C,
Cambiaggi G, Galatro GG and Caviglia H: Platelet-rich plasma vs
platelet-rich plasma plus hyaluronic acid for haemophilic knee
arthropathy treatment. Acta Orthop Belg. 87:705–712.
2021.PubMed/NCBI View
Article : Google Scholar
|
|
24
|
Taylor S, David J, Partington K, Pemberton
S, Mangles S, Wells A and Curry N: A single centre, open label,
pilot study evaluating the effect of intra-articular hyaluronic
acid injection on pain and functionality when injected into the
ankle (tibia-talar and sub-talar) joint in patients with
haemophilic arthropathy. Haemophilia. 28:e181–e188. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
de Campos GC, Rezende MU, Pailo AF,
Frucchi R and Camargo OP: Adding triamcinolone improves
viscosupplementation: A randomized clinical trial. Clin Orthop
Relat Res. 471:613–620. 2013.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Roberts WN: Intraarticular and soft tissue
injection: What agent(s) to inject and how frequently? UpToDate
2016; Accessed January 15, 2016.
|
|
27
|
Escobar M and Sallah S: Hemophilia A and
hemophilia B: Focus on arthropathy and variables affecting bleeding
severity and prophylaxis. J Thromb Haemost. 11:1449–1453.
2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Buccheri E, Avola M, Vitale N, Pavone P
and Vecchio M: Haemophilic arthropathy: A narrative review on the
use of intra-articular drugs for arthritis. Haemophilia.
25:919–927. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Rodriguez-Merchan EC: Intra-articular
corticosteroid injections in haemophilic arthropathy: Are they
recommended? Hosp Pract (1995). 46:1–4. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gigis I, Fotiadis E, Nenopoulos A, Tsitas
K and Hatzokos I: Comparison of two different molecular weight
intra-articular injections of hyaluronic acid for the treatment of
knee osteoarthritis. Hippokratia. 20:26–31. 2016.PubMed/NCBI
|
|
31
|
Rodriguez-Merchan EC: Intra-articular
injections of hyaluronic acid (viscosupplementation) in the
haemophilic knee. Blood Coagul Fibrinolysis. 23:580–583.
2012.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Rodriguez-Merchan EC and Valentino LA:
Joint lavage followed by intra-articular injection of hyaluronic
acid and/or corticosteroids in patients with severe hemophilic
arthropathy of the knee: Is this intervention really effective?
Expert Rev Hematol. 11:449–454. 2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Anitua E, Sánchez M, Nurden AT, Zalduendo
MM, de la Fuente M, Azofra J and Andía I: Platelet-released growth
factors enhance the secretion of hyaluronic acid and induce
hepatocyte growth factor production by synovial fibroblasts from
arthritic patients. Rheumatology (Oxford). 46:1769–1772.
2007.PubMed/NCBI View Article : Google Scholar
|
|
34
|
van Buul GM, Koevoet WL, Kops N, Bos PK,
Verhaar JA, Weinans H, Bernsen MR and van Osch GJ: Platelet-rich
plasma releasate inhibits inflammatory processes in osteoarthritic
chondrocytes. Am J Sports Med. 39:2362–2370. 2011.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Caviglia H, Daffunchio C, Galatro G,
Cambiaggi G, Oneto P, Douglas Price AL, Landro ME and Etulain J:
Inhibition of Fenton reaction is a novel mechanism to explain the
therapeutic effect of intra-articular injection of PRP in patients
with chronic haemophilic synovitis. Haemophilia. 26:e187–e193.
2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Marmor S, Farman T and Lortat-Jacob A:
Joint infection after knee arthroscopy: Medicolegal aspects. Orthop
Traumatol Surg Res. 95:278–283. 2009.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Manners PJ, Price P, Buurman D, Lewin B,
Smith B and Cole CH: Joint aspiration for acute hemarthrosis in
children receiving factor VIII prophylaxis for severe hemophilia:
11-Year safety data. J Rheumatol. 42:885–890. 2015.PubMed/NCBI View Article : Google Scholar
|