Introduction
Pituitary macroadenomas (PM) are a common subtype of
sellar tumors. Considering the gradual extension of human life
expectancy, in the near future, neurosurgeons would be expected to
face an increasing number of PM cases among the elderly population.
Any type of surgical treatment for patients of an advanced age is a
debatable issue, as age is accompanied by significant
comorbidities, and these patients are prone to developing systemic
complications. Thus, a less invasive approach should be used if
symptoms occurring due to PM necessitate surgical treatment. The
endoscopic endonasal transsphenoidal (EET) approach for the
resection of PMs is gradually gaining ground over the standard
microscopic transsphenoidal approaches performed over the past
decades. The better visualization during the surgery (1-3),
the shorter duration of the surgery with fewer intraoperative
complications (4-6),
the more extensive tumor removal (7,8), and
the shorter or equal hospitalization times of patients undergoing
the EET approach compared to patients undergoing the microscopic
transsphenoidal approach are some of the reasons behind the
preference for the use of EET (9-11).
It is also important to mention that the long learning curve of the
EET approach (200 up to 500 cases) proposed in the past to achieve
significantly lower morbidity and mortality (12) and for a number of years constituted
an obstacle to the rapid advancement of the latter approach appears
to be overestimated. Studies have demonstrated improved or at least
comparable results of the EET vs. the microscopic approach after 17
or even fewer surgeries performed using the EET approach (11,13),
if the former approach is performed in a multidisciplinary skull
base center (11). The present
study describes the cases of 6 elderly patients with PM who were
treated with the EET approach at Nicosia General Hospital.
Patients and methods
Patients
The present study included patients >70 years who
presented with pituitary macroadenomas that were treated surgically
using an EET approach. All the patients with a PM that were either
<70 years or treated with a different approach than the EET
approach were excluded from the study. The patients' data were
retrospectively collected and the data obtained included
demographics, the extension of tumor removal, intraoperative and
late complications, and endocrinology and neurological status pre-
and post-operatively. The data were retrieved from the database of
the hospital and accessed in an anonymous manner using unique code
identifiers, while data were handled in accordance with the
protocols of the ethics committee of Nicosia General Hospital
(Nicosia, Cyprus). The patient demographics and clinical data,
including surgical outcomes, are summarized in Table I.
 | Table IDemographics and clinical data of the
patients in the present case series. |
Table I
Demographics and clinical data of the
patients in the present case series.
| Parameter | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|
| Age, years | 76 | 71 | 73 | 74 | 82 | 71 |
| Sex | Female | Female | Female | Male | Male | Female |
| Clinical status | GCS14 | GCS 15 | GCS15 | GCS 14 | GCS12 | GCS15 |
| Pituitary hormonal
status | Normal | Normal | Abnormal | Apoplexy | Apoplexy | Normal |
| Neurological
deficit | Bilateral visual | Bilateral visual | None | Unilateral
visual | Unilateral
visual | None |
| Intraoperative
complication | None | None | Dural tear | None | None | None |
| Late
complication | None | None | CSF leak | None | None | None |
| Outcome | IMP | IMP | Stable (hormonal
replacement) | IMP | IMP (hormonal
replacement) | IMP |
The surgeries were performed between 2017 and 2022
by a team consisting of an attending ENT and a neurosurgeon. The
nasal stages, including the anterior sphenoidectomy, as well as the
final closure, were performed by the ENT surgeon, whereas the
remainder of the surgery was performed by the neurosurgeon. For
each procedure, a combination of 0˚, 30˚ and 45˚ rigid endoscopes
were utilized to achieve adequate exposure and visualization during
tumor removal. Abdominal fat was placed in the tumor bed while
water-tide closure was ensured using a triple layer of artificial
dura, tissue glue and rhino-septal mucosal flaps
(Hadad-Bassagasteguy flap). Neuronavigation was routinely utilized
in all the cases. The mean duration of hospitalization was 1 week.
The hormone levels that are considered ‘normal’ at our institution
are the following: Growth hormone, 0-1 µg/l (males) and 0-10 µg/l
(females); adrenocorticotropic hormone, 4.7-48.8 ng/l;
thyroid-stimulating hormone, 0.35-5.5 mU/l; prolactin, 2.1-17.7
µg/l (males), 2.8-29.2 µg/l (non-pregnant females), 9.7-208 µg/l
(pregnant females) and 1.8-20.3 µg/l (menopausal women);
follicle-stimulating hormone, 1.4-18.1 mU/l (males), 2.5-10.2 mU/l
(females in the follicular phase), 3.4-33.4 mU/l (females in the
ovulatory period), 1.5-9.1 mU/l (females in the luteal phase), and
23-116 mU/l (menopausal women); luteinizing hormone, 1.5-9.3 mU/l
(males), 1.9-12.5 mU/l (females in the follicular phase), 8.7-76.3
mU/l (females in the ovulatory period), 0.5-16.9 mU/l (females in
the luteal phase), and 15.9-54 mU/l (menopausal women).
Results
The clinical data of the 6 patients were as
follows:
Patient 1
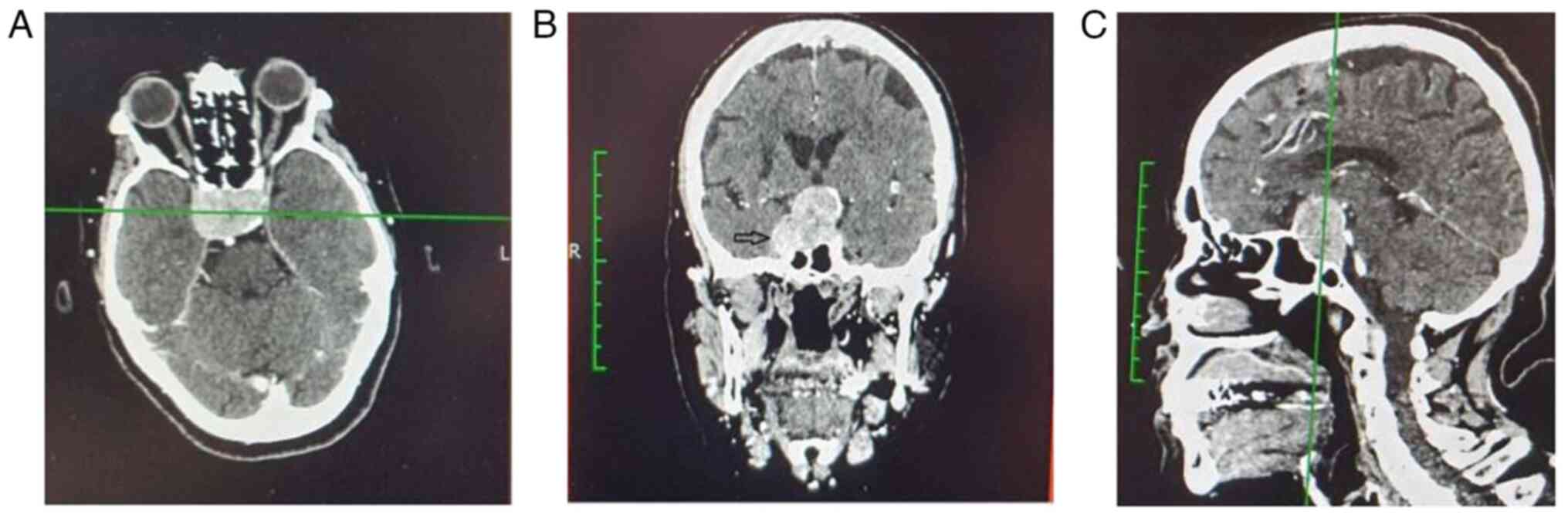
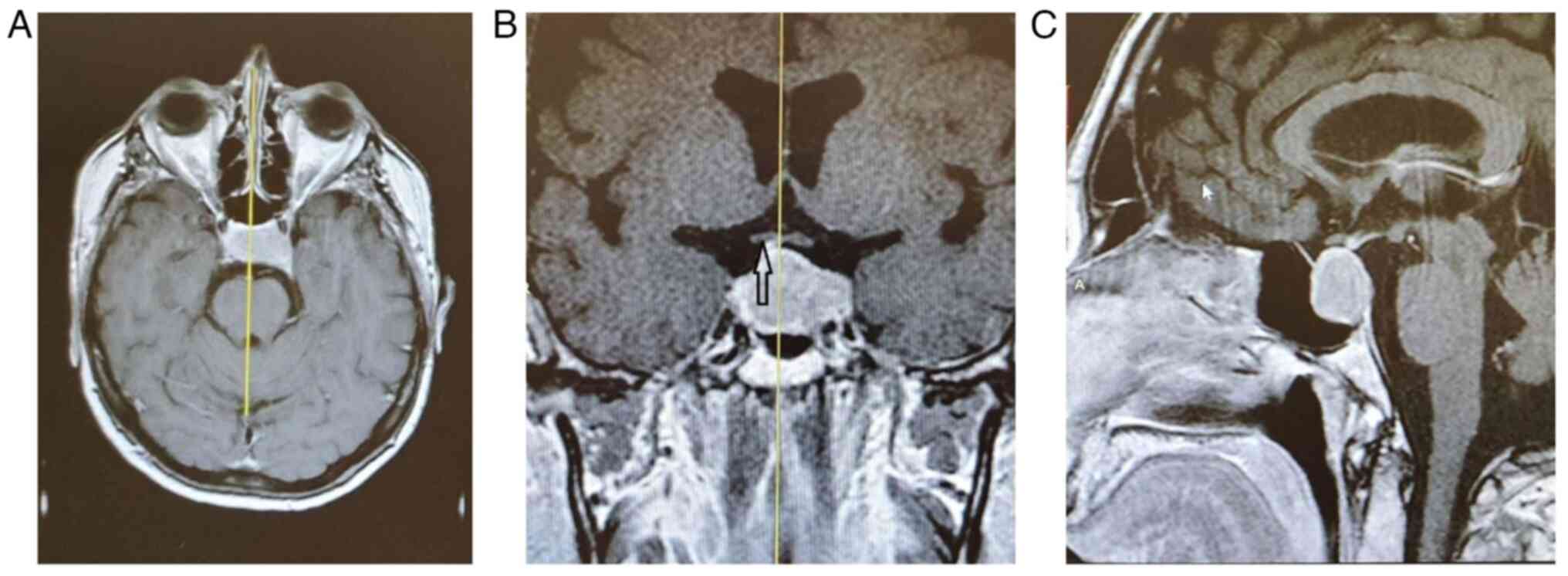
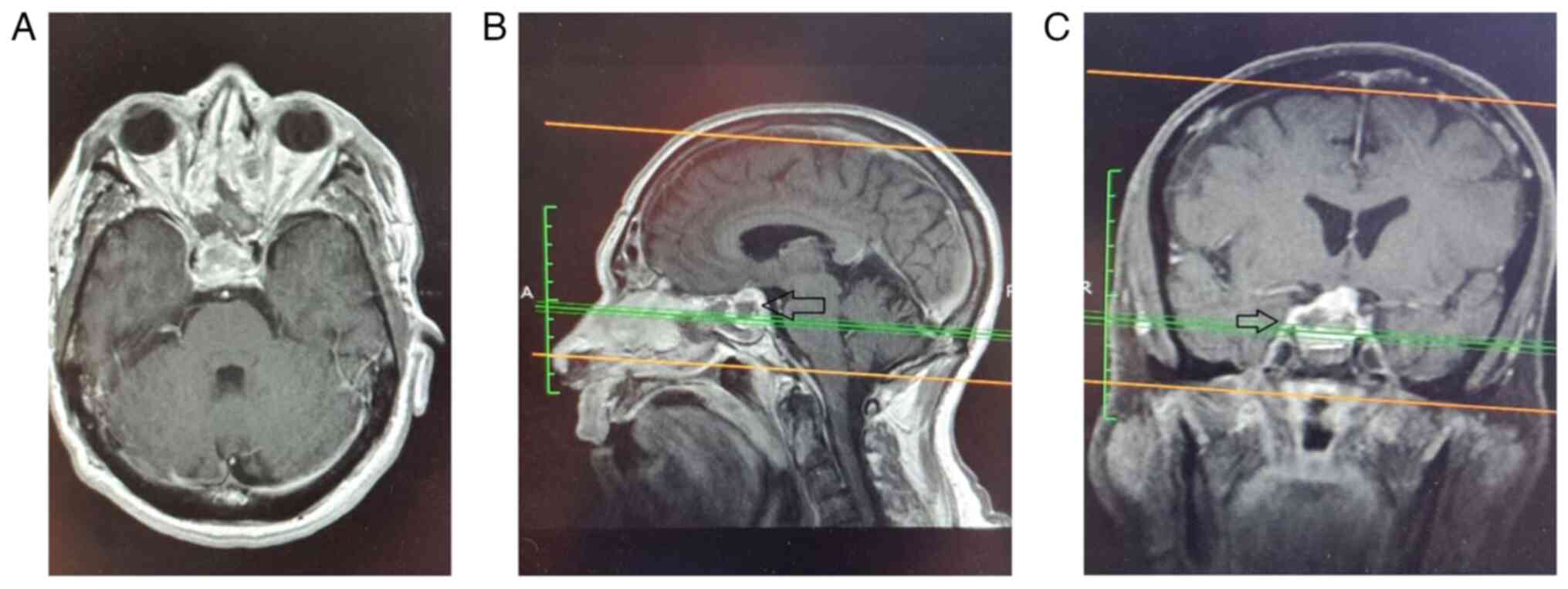
A 76-year-old female patient was admitted to the
Nicosia General Hospital with an acute visual field deficit
(significant bitemporal hemianopia). The levels of prolactin were
increased, while the levels of other hormones were within normal
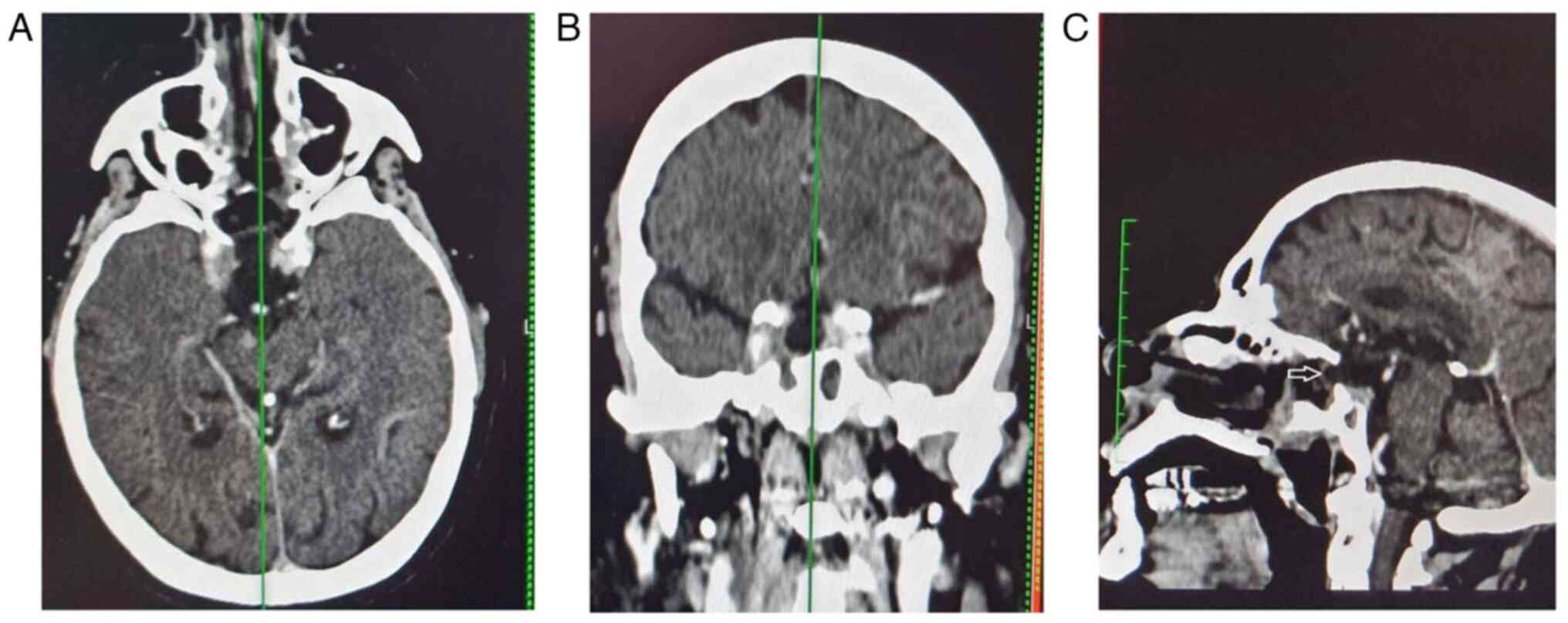
limits. A macroadenoma with lateral extension to the right
cavernous sinus (Knosp grade 3A) was identified in the MRI
(Fig. 1), and it was gross-totally
removed successfully using the EET approach (Fig. 2). The histological examination of
the specimen revealed a prolactinoma. After the surgery, the
patient experienced a notable improvement in bitemporal hemianopia
(mild visual field restriction was observed in the last follow-up,
6 years after the surgery).
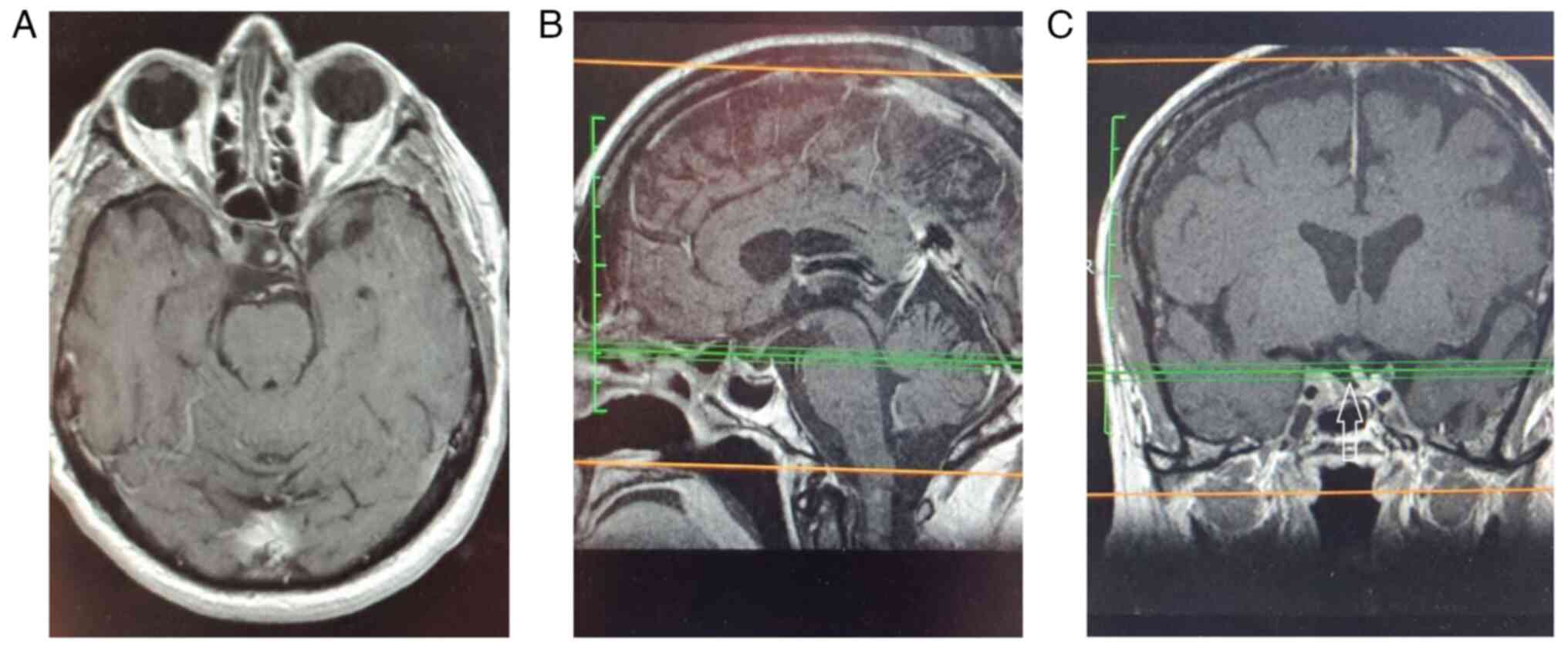
Patient 2
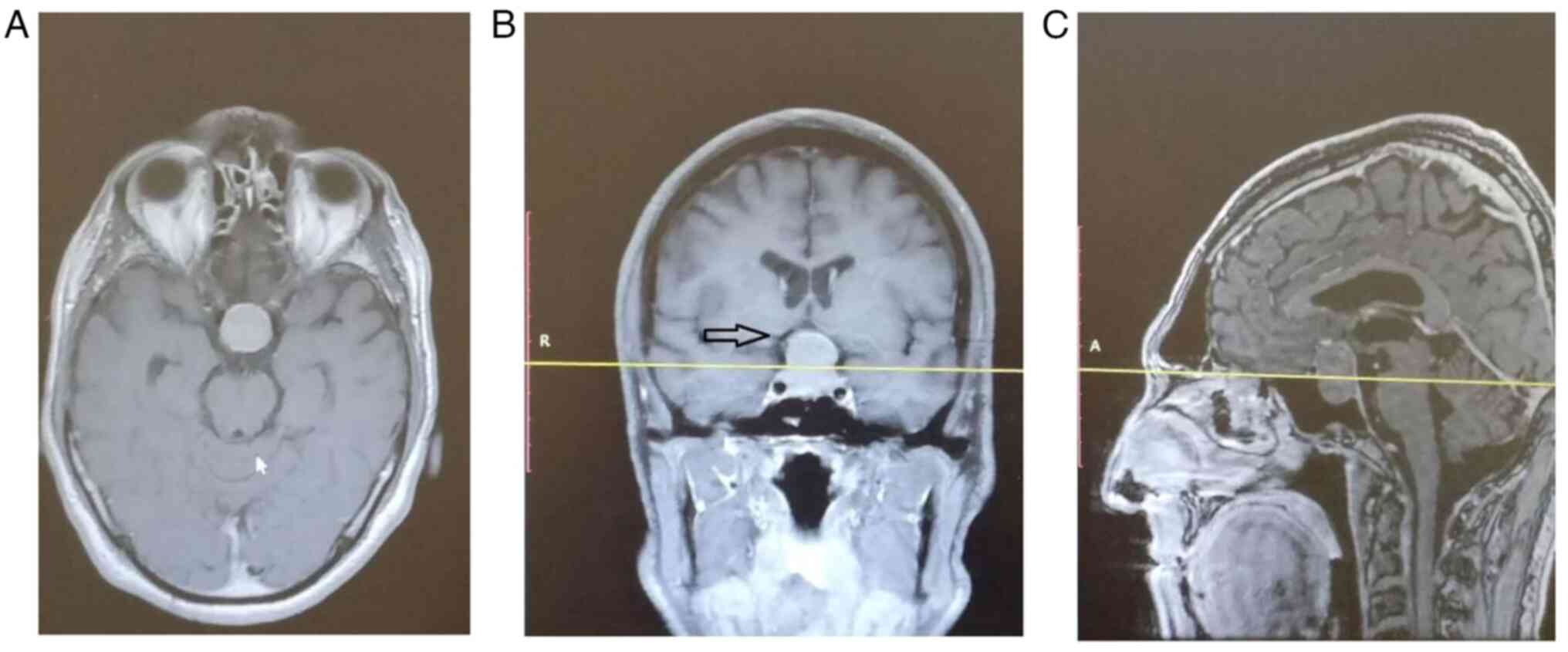
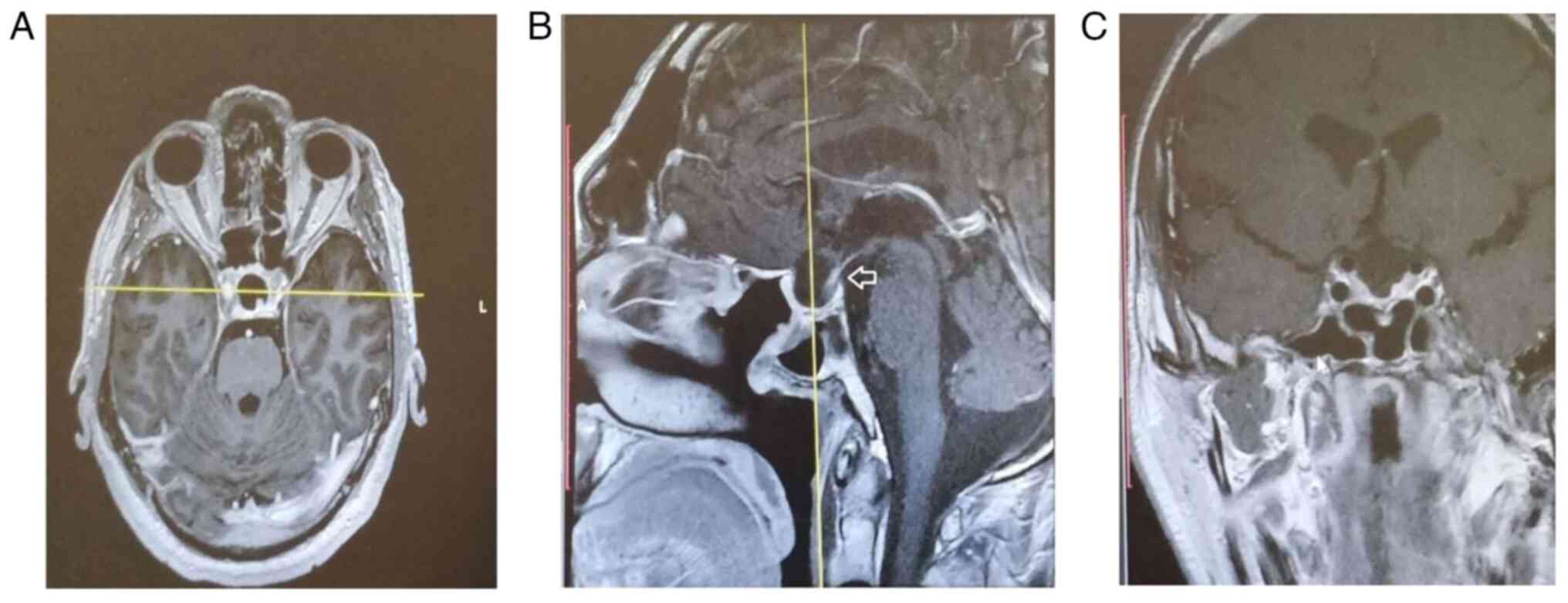
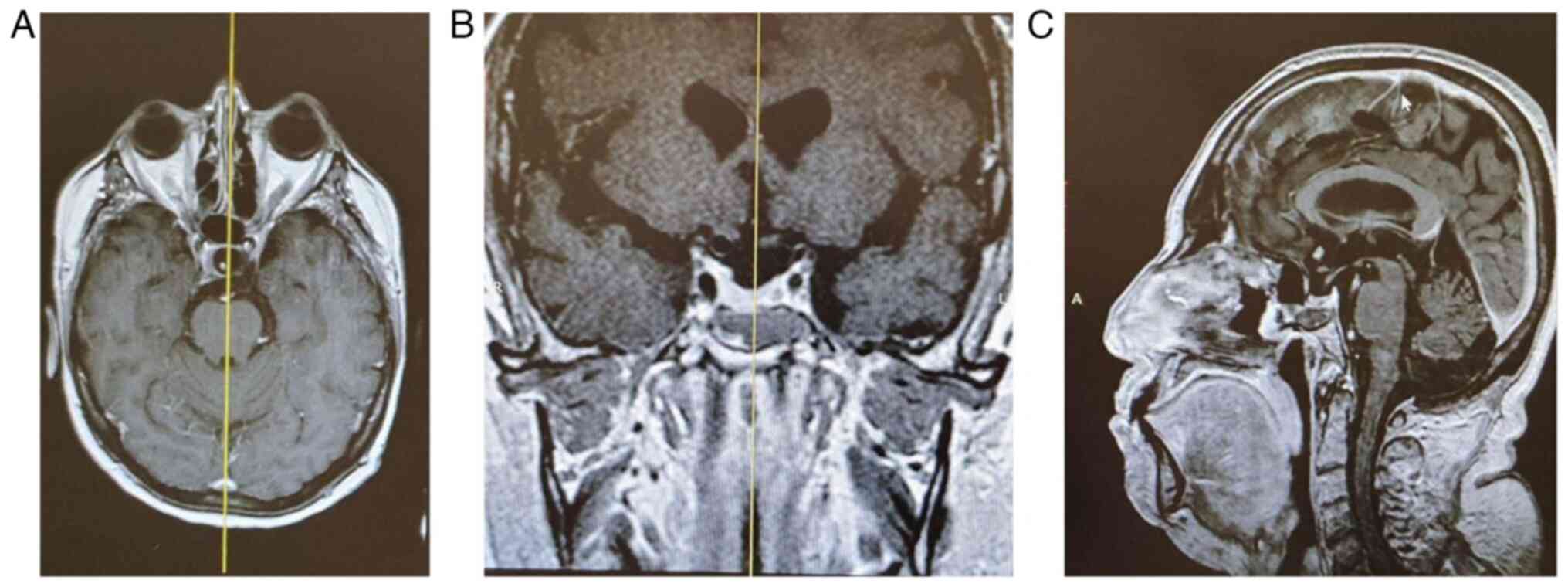
A 71-year-old female patient attended the
neurosurgery outpatient clinic at Nicosia General Hospital due to a
massive, Knosp grade 2 pituitary macroadenoma that was found
incidentally (Fig. 3). In the
neurological evaluation, a mild bilateral hemianopia was
discovered. The pituitary function was normal. The macroadenoma was
endoscopically removed (Fig. 4)
with no intra- or post-operative complications, while the
histological result was a non-secreting adenoma. The patient's
visual fields returned to almost normal levels
post-operatively.
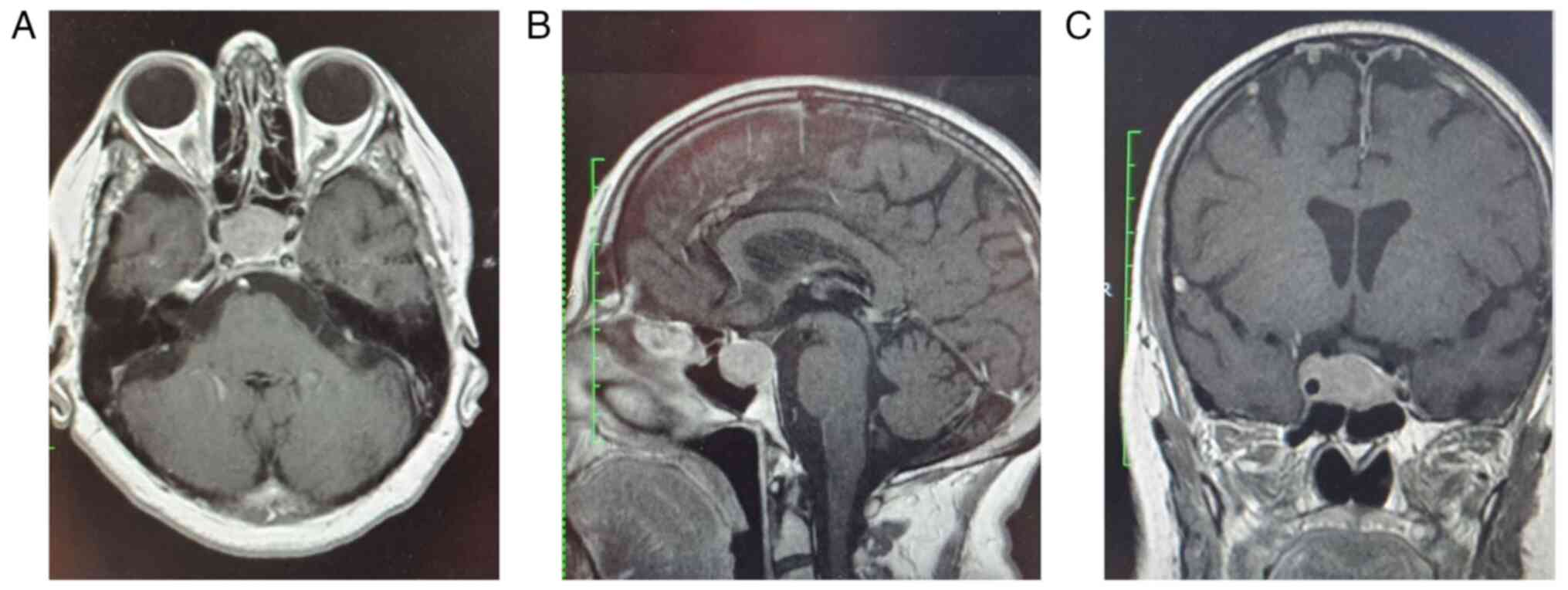
Patient 3
A 73-year-old female patient was referred to the
neurosurgery outpatient clinic at Nicosia General Hospital by her
endocrinologist due to resisting hypothyroidism and
hypocortisolemia. The radiological evaluation revealed a Knosp
grade 2 pituitary macroadenoma (Fig.
5), which was completely extracted using an EET approach
(Fig. 6). The histological
examination of the specimen revealed a non-secreting adenoma. The
patient developed a post-operative cerebrospinal fluid (CSF) leak,
which was successfully treated endoscopically. The patient was
discharged with hormonal replacement therapy, even though in the
long-term follow-up, her needs for replacement were reduced.
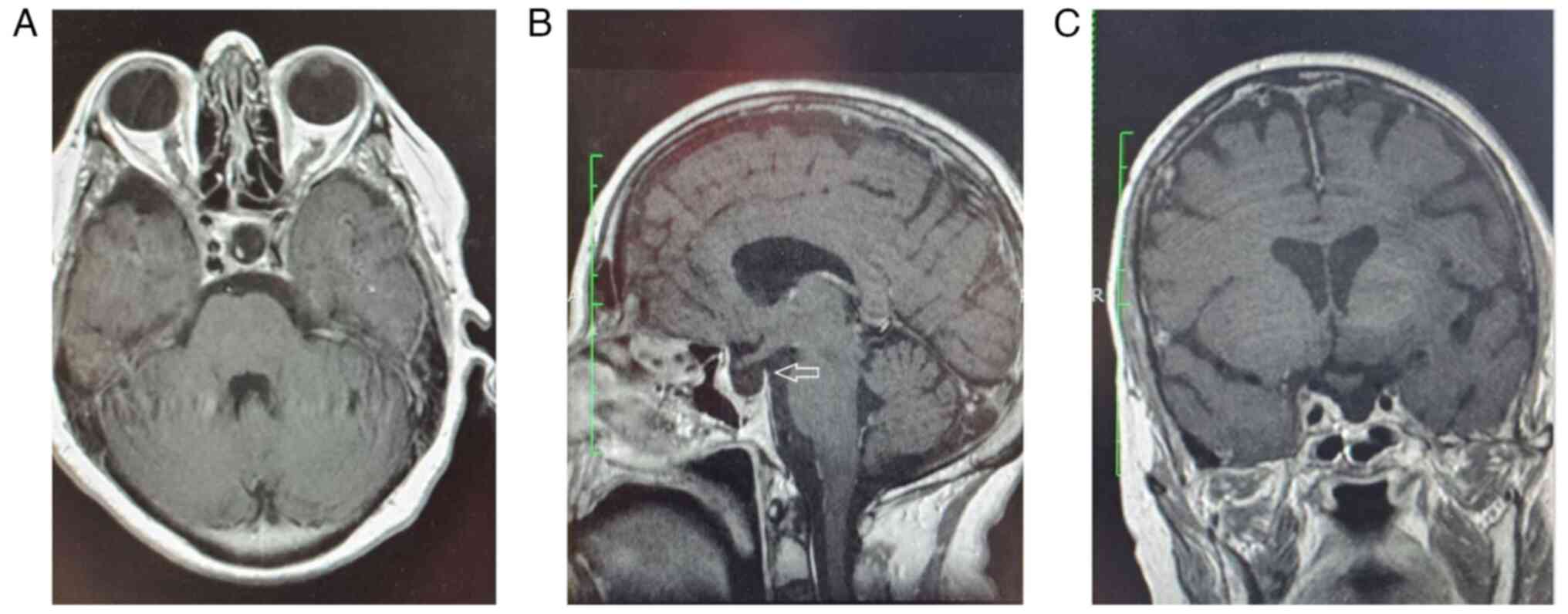
Patient 4
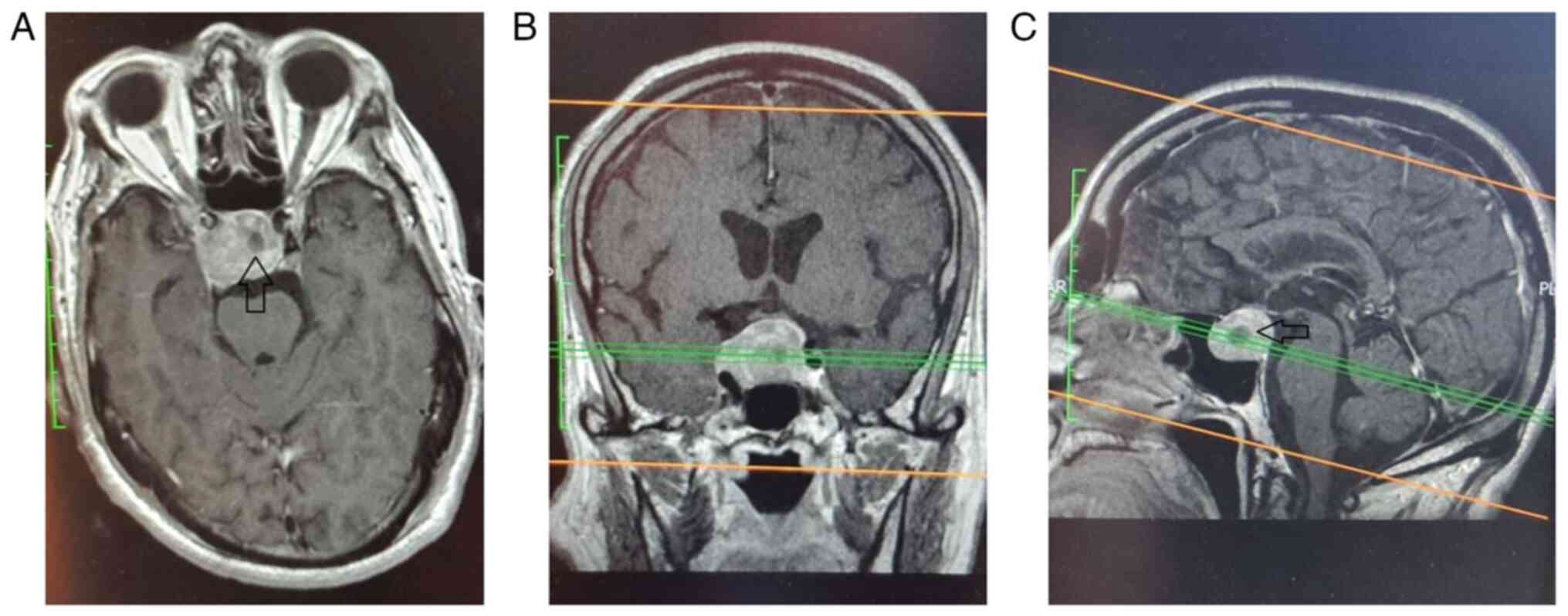
A 74-year-old male patient was urgently transferred
to the ER at Nicosia General Hospital due to pituitary apoplexy. He
experienced an acute unilateral visual loss, while the pituitary
hormone levels were in the lower normal limits. The MRI revealed a
Knosp grade 3A pituitary macroadenoma with internal bleeding
(Fig. 7). The histological
examination of the specimen revealed a non-secreting adenoma. The
lesion was extracted successfully (Fig.
8), and the patient's neurological deficit gradually improved
(he refers to moderate improvement in his vision shortly after the
surgery and a 70% return in vision return 1 year after the
surgery).
Patient 5
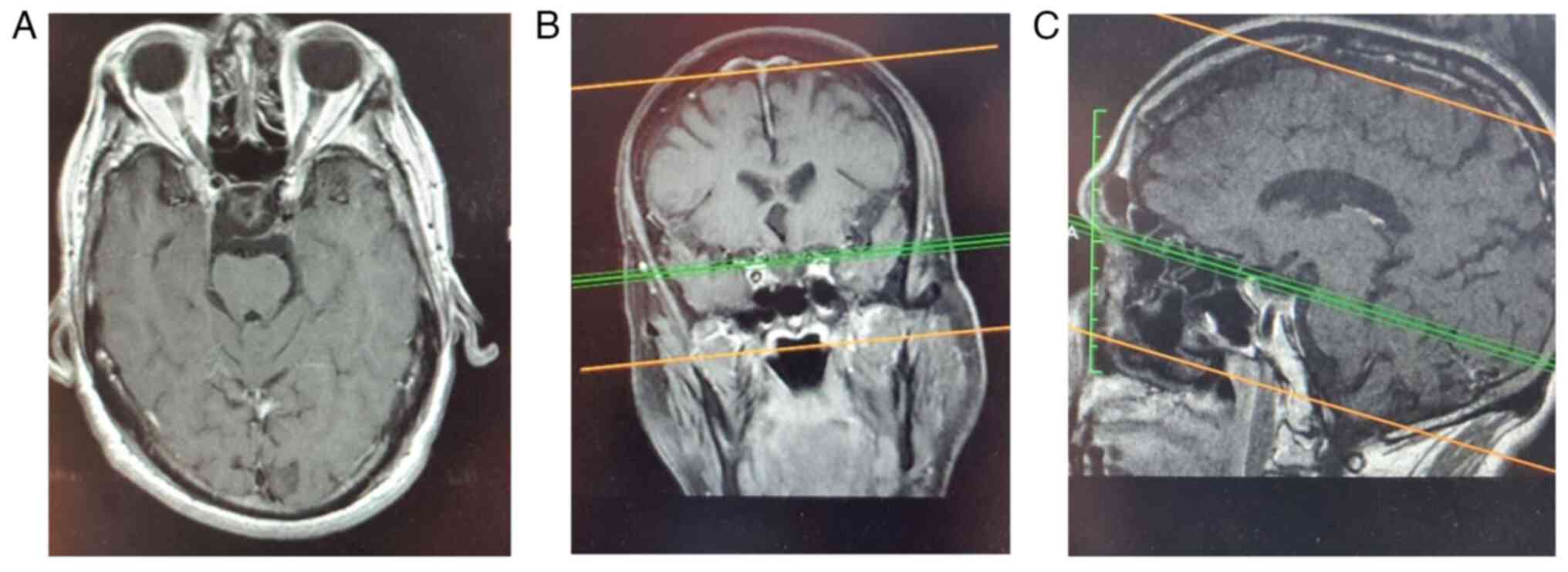
An 82-year-old male patient was transferred to the
ER at Nicosia General Hospital due to an acute change of
consciousness and unilateral blindness. The cortisone level was
below the normal limit. The MRI revealed a large Knosp grade 2 PM,
while signs of blood were also present (Fig. 9). Due to the clinically prominent
pituitary apoplexy, the initial treatment plan was to partially
remove the tumor, decompressing the optic chiasma; however, as the
surgery was uneventful, it was decided to proceed with gross total
resection (Fig. 10). The
histological examination of the specimen revealed a non-secreting
adenoma. The patient's vision gradually improved after the surgery
(he refers to a 50% improvement in his vision at 6 months after the
surgery); however, he still needs replacement therapy for
cortisone.
Patient 6
A 71-year-old female patient presented to the
outpatient clinic at Nicosia General Hospital due to headaches. The
neurological evaluation did not reveal any notable findings, and
the hormonal status was within normal limits. The radiological
evaluation revealed a Knosp grade 3A PM with an extension to the
right cavernous sinus (Fig. 11),
which could not completely explain the patient's symptoms. The
tumor was successfully removed (Fig.
12), while the headaches of the patients were reduced in
frequency. The histological examination of the specimen revealed a
non-secreting adenoma.
Outcomes
All patients experienced a notable improvement in
their neurological deficits. Moreover, their endocrinology status
either normalized or remained stable. The patients were followed-up
in the outpatient clinic after 1 month, 6 months, and then annually
post-operatively. An MRI was performed 3 months after the surgery
and then annually.
Discussion
The EET approach is gradually gaining ground in the
treatment of PMs, compared with the standard microscopic approach.
It offers a wider tumor removal, fewer complications and a shorter
surgery duration (4,6,7). There
is limited literature available on the surgical treatment endpoints
for elderly patients with PMs, and which approach has to be
utilized in each case. Some previous studies have supported the
microscopic transsphenoidal approach for PM resection in patients
>65 years (14,15). Their conclusions were supported by a
recent study by Azab et al (16), who stated that the microscopic
transsphenoidal approach for elderly patients with PM was more
efficacious compared with the EET approach. The latter findings are
in conflict with those of other studies (17-21),
where the EET approach is strongly supported, as it provides a
great panoramic view, the ability to perform meticulous and precise
intra-operative maneuvers, excellent gross total tumor resection,
and improved blood and CSF leak control. Additionally, patients who
undergo an EET approach have been shown to achieve shorter
hospitalization times (18)
compared with patients who undergo a microscopic approach.
Notwithstanding, there is a dispute, even in studies focusing on
the EET approach. In detail, some researchers have found higher
rates of complications in elderly groups (21,22)
compared with groups of younger patients with PM who have been
treated with an EET approach, while in another study, both young
and aged patients had the same complication rates (17). A dispute exists in the duration of
hospitalization as well; for example, Fujimoto et al
(20) found a longer post-operative
hospital duration in the elderly group, while others found the same
duration of hospitalization (17,21,22).
In summary, the current trend in the literature is
to treat patients of different age groups in a tailored manner. The
clear indication for the surgery is either endocrinological,
ophthalmological, or neurosurgical, due to the possible
space-occupying nature of the tumor, although the endpoint of the
treatment may differ. In younger patients with PM, the goal is to
perform aggressive tumor removal; hence, in elderly patients, more
focus is paid to the improvement of any neurological (the visual
deficit is the cardinal target) or hormonal deficit and the
avoidance of any possible complications (18). The partial decompression at such
advanced ages could translate into a reduced surgery duration and a
shorter hospitalization period, with all the complications the
latter carries, even if there is a remnant of the tumor (19). The lower rate of recurrence that is
observed in elderly patients compared with their younger
counterparts supports subtotal tumor removal if it is accompanied
by the decompression of the adjacent structures (17), while the choice of a partial
decompression of the neural structures with a massive PM remnant is
not a viable possibility in younger patients, as the regrowth of
the remaining tumor is highly possible.
The management algorithm in the patients described
herein did not differ. The original aim was a subtotal extraction
of the PM to alleviate the symptoms; notwithstanding, gross total
removal was performed as the procedures were uneventful. The
outcomes of the patients in the present study are also in parallel
with those of the literature, as all the patients with a
pre-operation neurological deficit experienced a notable
improvement in their deficit (4 out of 4 patients, or 100%), their
hormonal status normalized (2 out of 3 patients or 66.6% with
pre-operative abnormal hormonal status were discharged with a
better hormonal status), and the only complication that was
encountered was a post-operative CSF leak (1 out of 6 patients or
16.6%), which was successfully treated endoscopically. Finally, the
surgeries were undertaken in a low-volume hospital. Even if the
literature suggests that a long learning curve is required to
master the EET approach, it is considered that if the surgery is
performed by a multidisciplinary skull base team consisting of ENTs
and neurosurgeons, the outcome could be excellent for the
patient.
Some limitations of present study should be
mentioned. The present study was retrospective in nature, which
makes it prone to reporting and selection bias. Notwithstanding,
all the patients with a PM >70 years of age that were treated
with the EET approach in the given period were included. In
addition, the group was not uniform, as it was composed of patients
with different macroadenoma histologies and clinical presentations.
Finally, the small sample size of the series did not allow for a
solid statistical analysis. Further studies with a greater number
of cases are required the near future in order to allow for a
proper analysis and to extract clearer results.
In conclusion, when a physician manages elderly
patients with PMs, factors such as life expectancy, comorbidity,
neurological deficits and tumor recurrence rate should be taken
into consideration. Hence, the goals of treatment are not the same
as those in younger patients, where the aim is to perform a
complete tumor resection. Considering the low recurrence rate of a
remnant in the geriatric population with PMs and the comorbidity
that is met at such an age, the partial removal of the tumor with
decompression of the neural structures and the normalization of the
hormone status is an acceptable choice. The small case series in
the present study parallels that of the international literature,
supporting EET as an ideal approach for treating PM in patients of
an advanced age. That approach can be applied even in centers with
a low PM-patient influx, as long as these centers are staffed with
a multidisciplinary skull base team. Larger multicenter studies in
the future will provide more cases in order to perform a proper
statistical analysis which will further support the current
findings.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
GF and KF conceptualized the study. KF, GF, AA and
IG advised on patient care and medical treatment, and wrote and
prepared the draft of the manuscript. GF, KF, IGL, AA, IG, VEG, NT,
IT, PP and DAS analyzed the patients' data and provided critical
revisions. GF and KF confirm the authenticity of all the data. All
authors contributed to manuscript revision and have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The data were retrieved from the database of the
hospital and accessed in an anonymous manner using unique code
identifiers, while data were handled in accordance with the
protocols of the ethics committee of the hospital at Nicosia
General Hospital.
Patient consent for publication
Written informed was obtained from the patients for
the publication of their data and any accompanying images.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Jho HD and Carrau RL: Endoscopic endonasal
transsphenoidal surgery: Experience with 50 patients. J Neurosurg.
87:44–51. 1997.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jho HD, Carrau RL, Ko Y and Daly MA:
Endoscopic pituitary surgery: An early experience. Surg Neurol.
47:213–222; discussion 222-3. 1997.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cappabianca P, Alfieri A, Colao A, Ferone
D, Lombardi G and de Divitiis E: Endoscopic endonasal
transsphenoidal approach: An additional reason in support of
surgery in the management of pituitary lesions. Skull Base Surg.
9:109–117. 1999.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Li A, Liu W, Cao P, Zheng Y, Bu Z and Zhou
T: Endoscopic Versus microscopic transsphenoidal surgery in the
treatment of pituitary adenoma: A systematic review and
meta-analysis. World Neurosurg. 101:236–246. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Messerer M, De battista JC, Raverot G,
Kassis S, Dubourg J, Lapras V, Trouillas J, Perrin G and Jouanneau
E: Evidence of improved surgical outcome following endoscopy for
nonfunctioning pituitary adenoma removal. Neurosurg Focus.
30(E11)2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Razak AA, Horridge M, Connolly DJ, Warren
DJ, Mirza S, Muraleedharan V and Sinha S: Comparison of endoscopic
and microscopic trans-sphenoidal pituitary surgery: early results
in a single centre. Br J Neurosurg. 27:40–43. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Guo S, Wang Z, Kang X, Xin W and Li X: A
Meta-Analysis of endoscopic vs. microscopic transsphenoidal surgery
for non-functioning and functioning pituitary adenomas: Comparisons
of efficacy and safety. Front Neurol. 12(614382)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gao Y, Zhong C, Wang Y, Xu S, Guo Y, Dai
C, Zheng Y, Wang Y, Luo Q and Jiang J: Endoscopic versus
microscopic transsphenoidal pituitary adenoma surgery: A
meta-analysis. World J Surg Onc. 12(94)2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Neal JG, Patel SJ, Kulbersh JS, Osguthorpe
JD and Schlosser RJ: Comparison of techniques for transsphenoidal
pituitary surgery. Am J Rhinol. 21:203–206. 2007.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Graham SM, Iseli TA, Karnell LH, Clinger
JD, Hitchon PW and Greenlee JD: Endoscopic approach for pituitary
surgery improves rhinologic outcomes. Ann Otol Rhinol Laryngol.
118:630–635. 2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chatzidakis S, Anagiotos A, Fotakopoulos
G, Georgakopoulou VE, Tarantinos K, Papalexis P,
Aravantinou-Fatorou A, Sklapani P, Mathioudakis N, Trakas N, et al:
Comparison of the endoscopic endonasal to microscopic sublabial
transsphenoidal approach in a case series of pituitary
macroadenomas. Med Int (Lond). 3(6)2023.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ciric I, Ragin A, Baumgartner C and Pierce
D: Complications of transsphenoidal surgery: Results of a National
survey, review of the literature, and personal experience.
Neurosurgery. 40:225–236; discussion 236-7. 1997.PubMed/NCBI View Article : Google Scholar
|
|
13
|
O'Malley BW Jr, Grady MS, Gabel BC, Cohen
MA, Heuer GG, Pisapia J, Bohman LE and Leibowitz JM: Comparison of
endoscopic and microscopic removal of pituitary adenomas:
Single-surgeon experience and the learning curve. Neurosurg Focus.
25(E10)2008.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Locatelli M, Bertani G, Carrabba G,
Rampini P, Zavanone M, Caroli M, Sala E, Ferrante E, Gaini SM,
Spada A, et al: The trans-sphenoidal resection of pituitary
adenomas in elderly patients and surgical risk. Pituitary.
16:146–151. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hong J, Ding X and Lu Y: Clinical analysis
of 103 elderly patients with pituitary adenomas: Transsphenoidal
surgery and follow-up. J Clin Neurosci. 15:1091–1095.
2008.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Azab MA, O'Hagan M, Abou-Al-Shaar H, Karsy
M, Guan J and Couldwell WT: Safety and outcome of transsphenoidal
pituitary adenoma resection in elderly patients. World Neurosurg.
122:e1252–e1258. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Zhan R, Ma Z, Wang D and Li X: Pure
endoscopic endonasal transsphenoidal approach for nonfunctioning
pituitary adenomas in the elderly: Surgical outcomes and
complications in 158 patients. World Neurosurg. 84:1572–1578.
2015.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Marenco HA, Zymberg ST, Santos Rde P and
Ramalho CO: Surgical treatment of non-functioning pituitary
macroadenomas by the endoscopic endonasal approach in the elderly.
Arq Neuropsiquiatr. 73:764–769. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chinezu R, Fomekong F, Lasolle H,
Trouillas J, Vasiljevic A, Raverot G and Jouanneau E: Risks and
benefits of endoscopic transsphenoidal surgery for nonfunctioning
pituitary adenomas in patients of the ninth decade. World
Neurosurg. 106:315–321. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fujimoto K, Yano S, Shinojima N, Hide T
and Kuratsu JI: Endoscopic endonasal transsphenoidal surgery for
patients aged over 80 years with pituitary adenomas: Surgical and
follow-up results. Surg Neurol Int. 8(213)2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gondim JA, Almeida JP, de Albuquerque LA,
Gomes E, Schops M and Mota JI: Endoscopic endonasal transsphenoidal
surgery in elderly patients with pituitary adenomas. J Neurosurg.
123:31–38. 2015.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Wilson PJ, Omay SB, Kacker A, Anand VK and
Schwartz TH: Endonasal endoscopic pituitary surgery in the elderly.
J Neurosurg. 128:429–436. 2018.PubMed/NCBI View Article : Google Scholar
|