Introduction
The intracranial volume often increases following
trauma owing to a hemorrhage, cerebral edema or hydrocephalus. This
can lead to an injurious shift in the brain, termed herniation
(1). In addition, an increased
volume within the rigid skull can elevate intracranial pressure
(ICP), leading to compartment syndrome, which blocks or prevents
blood flow to the brain (2). Brain
ischemia can eventually lead to disability or mortality. Therefore,
it is critical to dynamically monitor the changes in ICP (2).
Intracerebroventricular catheterization,
intraparenchymal probing and lumbar puncture are considered the
gold standard protocols for the measurement of ICP. However, they
are associated with various risks, including bleeding, infection
and malfunction, and are contraindicated in individuals requiring
prolonged monitoring or having a predisposition to coagulation
disorders or platelet disorders (3). Additionally, lumbar puncture is
strongly discouraged in patients with brain herniation (4). This has prompted to the investigation
of an appropriate ICP assessment method for bedside applications.
Ultrasound has been used as a method for measuring the optic nerve
sheath diameter (ONSD) owing to its portability, feasibility,
safety, reproducibility and the lack of exposure to radiation
hazards or well-known side-effects (5). The optic nerve is wrapped by a sheath,
originating from the meninges and extending toward the orbit
(5). This communication permits
cerebrospinal fluid (CSF) transfer and therefore, similar pressure
changes between the intracranial and orbital subarachnoid spaces
(6,7). Therefore, the ultrasound detection of
a high ICP based on the ONSD is becoming increasingly popular in
trauma, neurosurgery and emergency medicine, although it does not
permit continuous measurement and priming (8).
Meta-analysis studies on ultrasound measurements of
the ONSD for the assessment of ICP have been previously published.
However, there are limitations, including an increased
heterogeneity or a limited number of included studies in the
literature (9,10). This affects the accuracy of the
ultrasound assessment of ICP. In the present systematic review and
meta-analysis, the accuracy of ultrasound for measuring the ONSD
and standard invasive methods for measuring the ICP in patients
with traumatic brain injury (TBI) are discussed. The aim of the
present meta-analysis was to examine the accuracy of ONSD
ultrasonography in the diagnosis of ICP.
Materials and methods
Literature search
The PubMed, Embase, Web of Science and Cochrane
Library databases were systematically searched from database
inception to November, 2022 to identify relevant articles using the
following search terms: ‘Optic nerve’, ‘optic nerve sheath’, ‘optic
nerve sheath diameter’, ‘ONSD’, ‘ultrasound’, ‘ultrasonography’,
‘sonography’, ‘intracranial pressure’, ‘raised intracranial
pressure’, ‘high intracranial pressure’, ‘ICP’, ‘high ICP’ and
‘raised ICP’ (the search strategy used herein is presented in the
file entitled Data S1). The
present meta-analysis was performed in accordance with the
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
(PRISMA) statement (11).
Study selection criteria
The included studies assessed adult patients with
TBI who underwent an ultrasound for the measurement of ONSD and
invasive intracranial monitoring for the measurement of ICP,
without restrictions in language or year of publication. The
exclusion criteria were the following: i) Studies that included
patients aged <18 years; ii) case reports, reviews and
meta-analyses; iii) studies that included pediatric patients or
animals; iv) studies that included non-TBI patients; and v) studies
that did not contain sufficient information (in the supplementary
material and/or original article) to construe the 2x2 contingency
table (true positive, true negative, false positive and false
negative results). If it was not possible to build a table based on
the existing published data, the corresponding author was contacted
to clarify the issue. If no response was obtained, the study was
excluded from the primary outcome analysis. Any disagreements
regarding the included specific studies were solved by reaching a
consensus amongst all the authors involved in the study.
Data abstraction and quality
assessment
From each study, baseline characteristics were
extracted, including the year of publication, author list, study
design, country, sample size, diagnosis, invasive ICP measurement
methods, high ICP thresholds, and the specificity and sensitivity
of index tests. Invasive intracranial monitoring is the gold
standard for measuring ICP (3). One
investigator extracted the data, while another independently
verified the data to construct a 2x2 contingency table. The two
investigators extracted the data from the original study, and any
disagreements were resolved through consultation with a third
independent author. The methodological quality of the studies was
assessed using the Quality Assessment of Diagnostic Accuracy
Studies-2 (QUADAS-2) tool. Of note, two authors performed the
quality assessments, and disagreements were resolved by consensus
in the presence of a third author. An assessment of reporting bias
was attempted using funnel plots (data not shown); however, this
did not proceed due to the lack of relevant studies.
Quantitative data synthesis
Data synthesis was performed using the methods
recommended in the Cochrane Handbook for Systematic Reviews of
Diagnostic Test Accuracy. A bivariate random effects model was used
to analyze and pool the statistics of the diagnostic tests
(sensitivity, specificity, positive likelihood ratio, negative
likelihood ratio and diagnostic odds of ultrasound). A diagnostic
test statistic in the present study referred to the ability of
ultrasound to detect high ICP. Heterogeneity was assessed using the
I2 statistics. Values of P<0.05 or
I2>50% indicated significant heterogeneity.
Hierarchical summary receiver operating characteristics (SROC)
analysis was performed, and an area under the curve of >0.9 was
considered highly accurate in assessing the summary accuracy of
ultrasound. All analyses were performed using Review Manager 5.3 or
Meta-DiSc software 1.4(12).
Results
Search results and study
characteristics
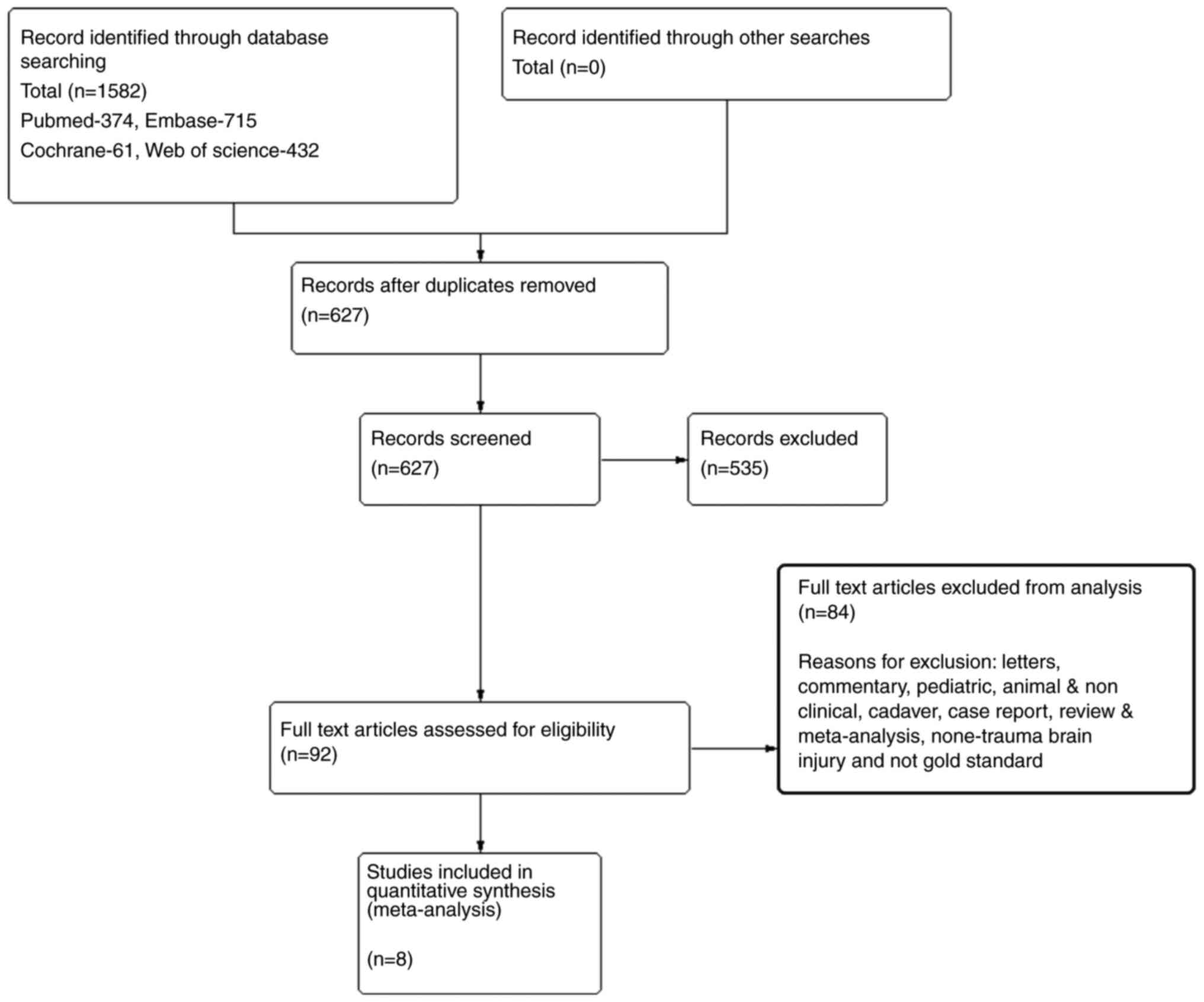
The flow diagram presented in Fig. 1 provides a summary of the PRISMA
format of the literature search (13-20).
A total of 1,582 studies were identified during the preliminary
search. Following the removal of 955 duplicates, the abstracts of
the 627 remaining studies were evaluated by two separate authors.
The full text of 92 articles was reviewed based on the eligibility
criteria, and 84 articles were rejected based on the exclusion
criteria. Ultimately, eight studies with 222 patients with TBI were
included.
Characteristics of the included
studies
The characteristics of the eight included studies
(13-20)
are summarized in Table I. The
studies were performed between 2007 and 2020, and included 10-49
patients. These studies included in the primary outcome analysis
presented with threshold values of ONSD ranging from 5-6.4 mm,
indicating an elevated ICP ranging from 5.0-6.4 mm. In all the
studies analyzed, invasive ICP monitoring was used, including brain
parenchyma and ventricles.
 | Table ICharacteristic of studies included in
the meta-analysis. |
Table I
Characteristic of studies included in
the meta-analysis.
| First author/s, year
of publication | Country | No. of Patients | Age (Years) | Diagnosis | Cut-off of raised
ICP | ICP measurement | Cut-off of ONSD
(mm) | Interval between ICP
and ONSD measurement | Exclusion
criteria | Sensitivity | Specificity | (Refs.) |
|---|
| Geeraerts et
al, 2007 | France | 31 | 38 | TBI, GCS<8 | 20 mmHg | Intraparenchymal
catheter inserted into the frontal lobe | 5.9 | Within 1 h | Ocular trauma and/or
pathology | 0.87 | 0.94 | (15) |
| Maissan et al,
2015 | The Netherlands | 18 | 38 | TBI | 20 mmHg | Intraparenchymal
probe to monitor ICP | 5 | Simultaneous | Ocular trauma | 0.94 | 0.98 | (16) |
| Soldatos et
al, 2008 | Greece | 32 | 49 | Moderate-severe
TBI | 20 mmHg | Invasive measurements
of ICP | 5.7 | Simultaneous | Ocular pathology | 0.74 | 1 | (17) |
| Soliman et al,
2018 | Kingdom of Saudi
Arabia | 40 | 37 | Severe TBI,
GCS<8 | 20 mmHg | A Camino
intraparenchymal catheter to monitor the ICP | 6.4 | Simultaneous | Ocular trauma
and/or pathology | 0.85 | 0.83 | (18) |
| Strumwasser et
al, 2011 | USA | 10 | 43 | Severe TBI,
GCS<8 | 20 mmHg | Insertion of the
intracranial device | 6 | Within 1 h | Ocular pathology,
pregnant, decompressive craniotomy | 0.36 | 0.38 | (19) |
| Širanović et
al, 2011 | Croatia | 20 | 31 | TBI | 20 mmHg | An intraven
tricular catheter to monitor the ICP | 6.1 | Simultaneous | Ocular trauma
and/or pathology | 1 | 0.83 | (20) |
| Du et al,
2020 | P.R. China | 49 | 50 | TBI | 20 mmHg | An ICP probe was
placed in the lateral ventricle | 5.53 | Within 1 h | Previous ocular and
optic nerve diseases or injuries at admission | 0.80 | 0.79 | (13) |
| Altayar et
al, 2021 | Kingdom of Saudi
Arabia | 22 | 40 | TBI | 22 mmHg | External
ventricular drainage system | 6.1 | Within 1 h | Penetrating head
injuries or any associated ocular injuries | 0.85 | 0.67 | (14) |
Quality assessment
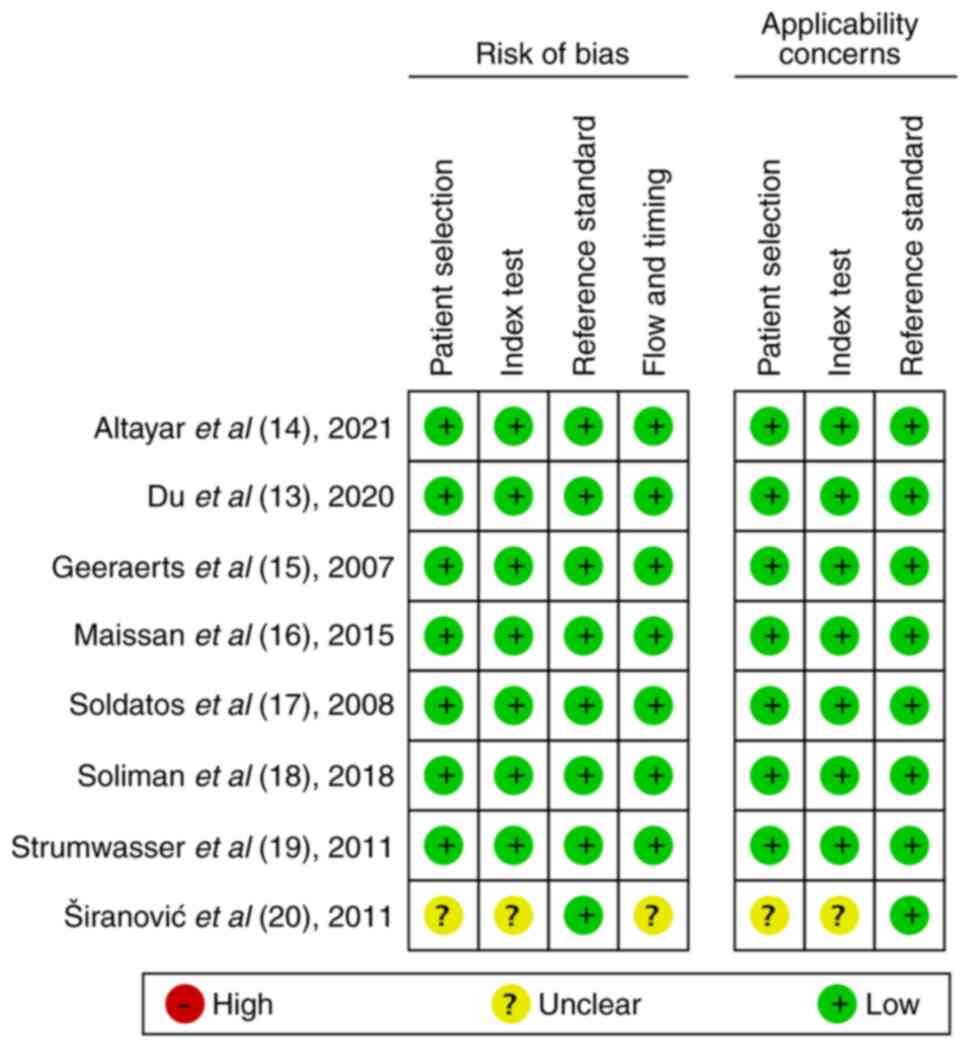
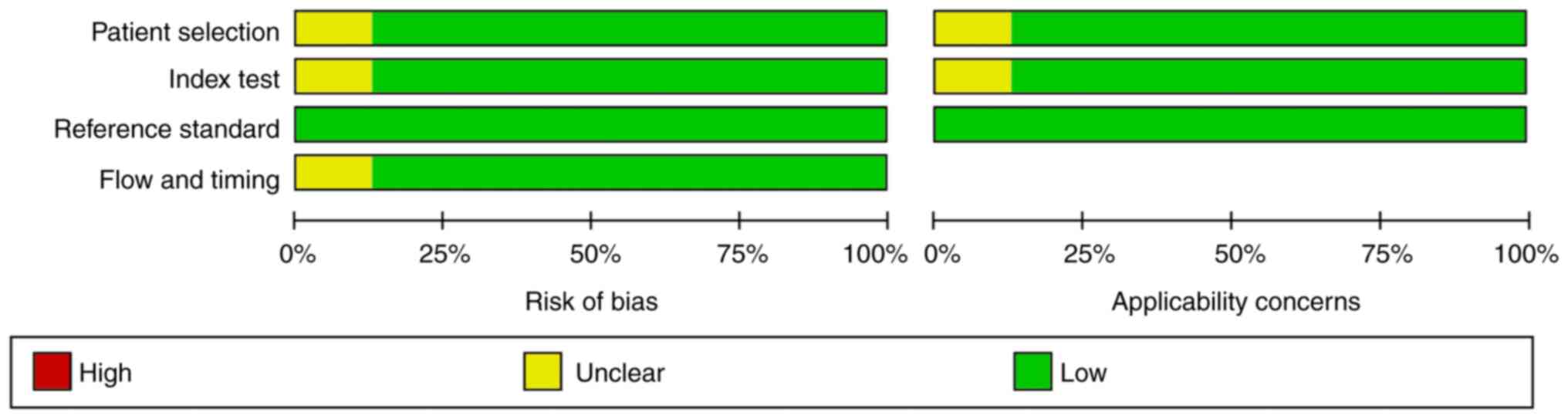
Quality assessment analysis of all the included
studies was performed using the QUADAS-2 tool (Table II). No studies exhibited any risk
of bias or applicability areas. Of note, one study was considered
to be of low quality, since five unclear concerns were documented
(20). The quality assessment of
the included studies is presented in Figs. 2 and 3.
 | Table IIQuality assessment of the included
studies using QUADAS-2 tool. |
Table II
Quality assessment of the included
studies using QUADAS-2 tool.
| | Risk of bias | Applicability
concerns |
|---|
| First author/s,
Year of publication | Patient
selection | Index test | Reference
standard | Flow timing | Patient
selection | Index test | Reference
standard | (Refs.) |
|---|
| Geeraerts et
al, 2007 | Low | Low | Low | Low | Low | Low | Low | (15) |
| Maissan et
al, 2015 | Low | Low | Low | Low | Low | Low | Low | (16) |
| Soldatos et
al, 2008 | Low | Low | Low | Low | Low | Low | Low | (17) |
| Soliman et
al, 2018 | Low | Low | Low | Low | Low | Low | Low | (18) |
| Strumwasser et
al, 2011 | Low | Low | Low | Low | Low | Low | Low | (19) |
| Širanović et
al, 2011 | Unclear | Unclear | Low | Unclear | Unclear | Unclear | Low | (20) |
| Du et al,
2020 | Low | Low | Low | Low | Low | Low | Low | (13) |
| Altayar et
al, 2021 | Low | Low | Low | Low | Low | Low | Low | (14) |
Quantitative data synthesis
results
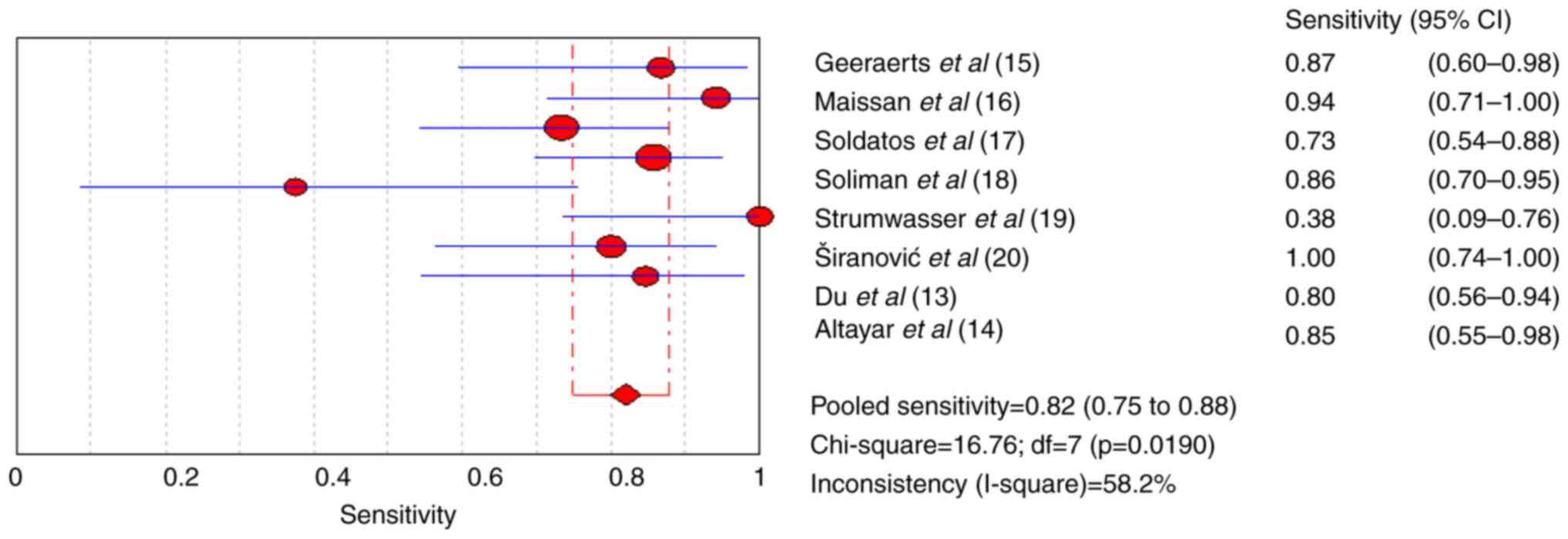
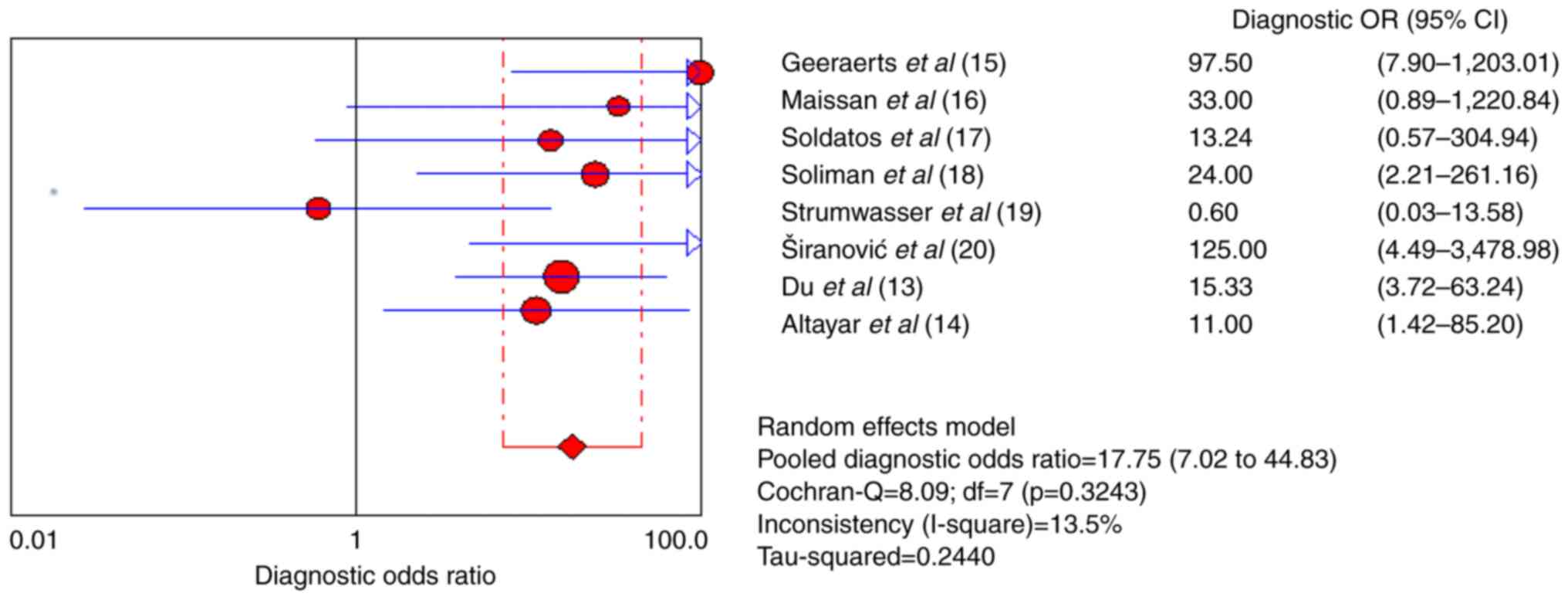
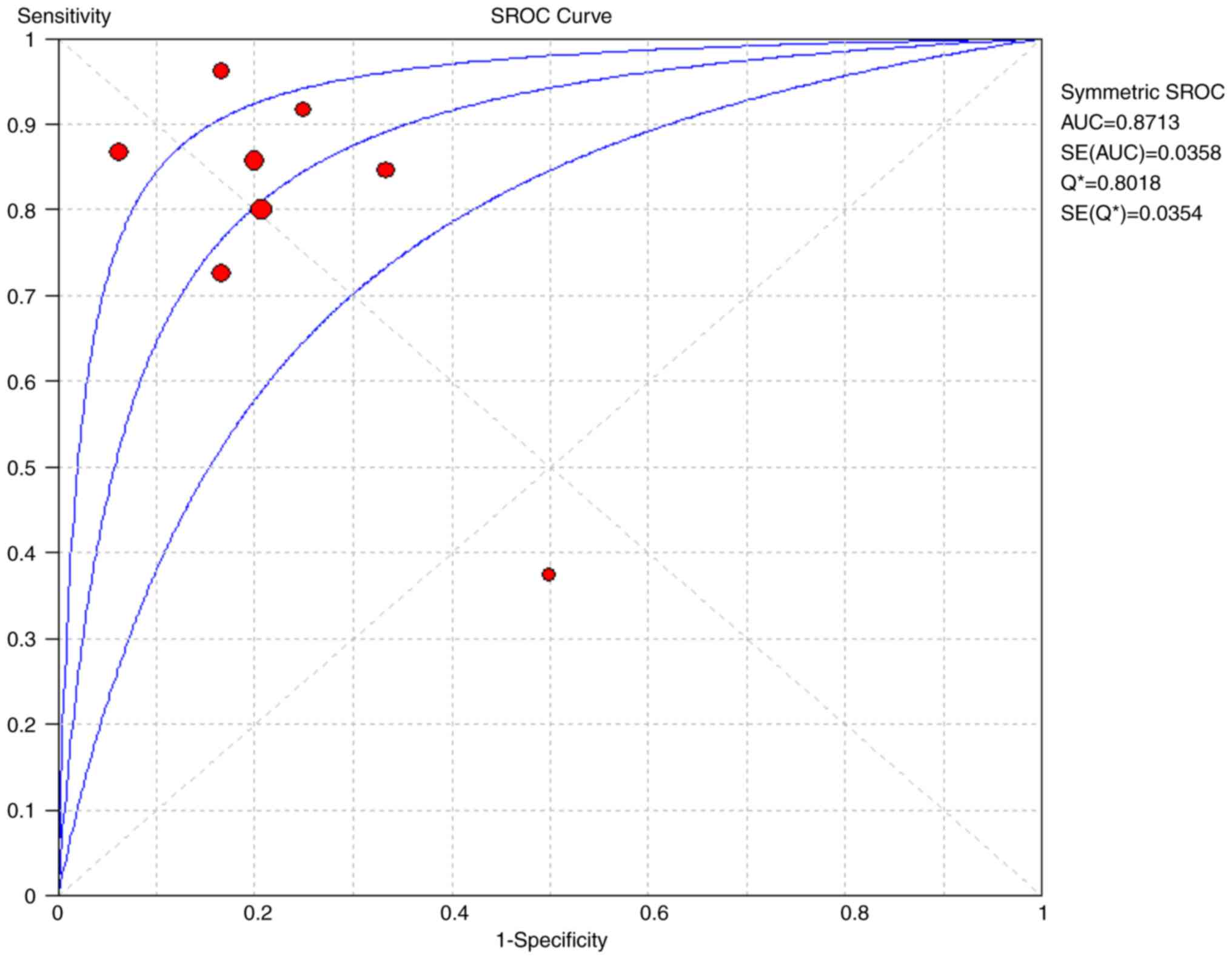
The pooled sensitivity and specificity for increased
ICP detected by ultrasound were 0.82 [95% confidence interval (CI),
0.75-0.88] and 0.82 (95% CI, 0.71-0.90), respectively (Figs. 4 and 5). Furthermore, the diagnostic odds ratio
(DOR) for ultrasound was 17.75 (95% CI: 7.02-44.83; Fig. 6). The area under the SROC curve
analysis revealed an appropriate accuracy of 0.87 (Fig. 7).
Discussion
The present systematic review and meta-analysis of
222 patients with TBI revealed that ultrasonography performed well
in detecting an increased ICP, with an overall pooled sensitivity
of 0.82 (95% CI: 0.75-0.88) and a specificity of 0.82 (95% CI:
0.71-0.90). The DOR of ultrasonography was 17.75, indicating that
the odds of a positive test in patients with an elevated ICP are
>17-fold higher compared with those of a negative test in
patients with normal ICP. The area under the SROC curve, which was
based on predefined criteria, was relatively high (0.87). The
present study confirms the effectiveness of ultrasound as a
complementary method to assess the ICP in patients with TBI.
Moreover, these results are notable, as invasive ICP monitoring is
associated with various risks, including bleeding, infection and
malfunction, and are contraindicated in individuals who require
prolonged monitoring or have a predisposition to coagulation
disorders or platelet disorders (3).
Aletreby et al (9) reported high sensitivity and
specificity of the ONSD method (0.90 and 0.85, respectively), which
were higher than the results of the present study. Due to the
inclusion of various diagnoses, the data in the study by Aletreby
et al (9) are heterogeneous
both clinically and epidemiologically. Lee et al (10) reported the sensitivity and
specificity of the ONSD method (0.91 and 0.77, respectively).
However, the number of studies included was relatively small and
included studies on the computed tomography measurement of optic
nerve sheath diameter (10). In
another review study it was revealed that the combined area under
the ROC curve of ONSD ultrasound was 0.94 (0.91-0.96) (6). The present systematic review and
meta-analysis revealed that ultrasonography performed well in
confirming an elevated ICP, with an overall pooled sensitivity of
0.82 and an overall pooled specificity of 0.82. Robba et al
(21) reported the pooled DOR for
ONSD from the bivariate diagnostic random-effects model return was
67.5 (95% CI 29-135), and the area under the HSROC curve was 0.938,
while the partial AUC was 0.916. This finding is in accord with the
results of previously published studies (6,21). The
conclusions of these studies demonstrated that ONSD can accurately
predict ICP despite the lack of consensus on ONSD thresholds and
operator-dependent issues.
The results of the present study revealed a high
sensitivity and specificity of ONSD in predicting intracranial
hypertension. However, the thresholds for ONSD were inconsistent,
ranging from 5.0-6.4 mm. The results of the meta-analysis by
Montorfano et al (22)
revealed a mean ONSD of 5.82 mm (95% CI 5.58-6.06 mm) in patients
with an increased ICP. The observed differences may be attributed
to differences in the etiology of intracranial hypertension, the
clinical setting in which the ONSD was measured, and the criteria
used to diagnose intracranial hypertension. Experts suggest
following the ONSD trend of the same patient over time, rather than
a fixed threshold; this is crucial, considering the variability of
ONSD described and the different thresholds under pathological
conditions (23). However, in order
for it to be useful at the bedside, it is necessary to define a
percentage change or threshold (24). The ONSD does not shrink immediately
following a marked increase in ICP, since an enlarged ONSD requires
drainage of CSF from the intracranial compartment, which does not
occur immediately in all cases. Thus, this makes the assessment of
trends problematic. Future studies are thus required to focus on
both defined thresholds and the behavior of the ONSD with increased
ICP.
In recent years, the use of ultrasound has markedly
increased due to various factors, including technological advances,
a minimally invasive nature, affordability and the ease of use
(25,26). The use of optic nerve ultrasound as
an accurate, non-invasive, safe, reproducible and cost-effective
ICP tool has recently been validated by the measurement of ONSD,
thereby reducing the potentially deleterious consequences of
invasive transcranial measurements (14,27,28).
Ultrasound of the optic nerve can be used to differentiate between
both normal and elevated ICP and can be a useful screening tool in
resource-limited practices (29).
The present systematic review has several
methodological limitations. The total sample of patients with TBI
was relatively small, with only eight studies with 222 patients
having been included in the analysis. All included studies used
invasive ICP monitoring, possibly combined with debridement
decompression. However, Gao et al (30) reported that the accuracy of invasive
ICP monitoring after debridement decompression was low, which may
have affected the accuracy of the present study. In addition, a
standardized ONSD cut-off value as a criterion for diagnosing an
elevated ICP was not established, since different studies used
various cut-off points and ultrasound techniques. An ONSD detected
by ultrasound does not accurately reflect the ICP values above or
below the threshold of 20 cm H2O; however, the method
can be used to monitor ICP trends and evaluate the response to
therapeutic interventions.
In conclusion, based on the available evidence,
ultrasound determined elevated ICP has reasonable performance
indicators with high sensitivity and specificity in patients with
TBI. This method is a useful complementary monitoring tool in acute
care. The use of ultrasound to assess ICP in TBI is less risky,
more cost-effective and quicker than invasive methods, aiding
towards more accurate clinical decision-making, particularly in
resource-limited settings.
Supplementary Material
Details of search strategy
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WC and PY conceived and designed the study. WC and
XZ wrote and prepared the draft of the manuscript. XY and XZ
collected data. All authors contributed to manuscript revision and
have read and approved the final version of the manuscript. WC and
XZ confirm authenticity all the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hawryluk GWJ, Citerio G, Hutchinson P,
Kolias A, Meyfroidt G, Robba C, Stocchetti N and Chesnut R:
Intracranial pressure: Current perspectives on physiology and
monitoring. Intensive Care Med. 48:1471–1481. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cucciolini G, Motroni V and Czosnyka M:
Intracranial pressure for clinicians: It is not just a number. J
Anesth Analg Crit Care. 3(31)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tavakoli S, Peitz G, Ares W, Hafeez S and
Grandhi R: Complications of invasive intracranial pressure
monitoring devices in neurocritical care. Neurosurg Focus.
43(E6)2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lane BC, Scranton R and Cohen-Gadol AA:
Risk of brain herniation after craniotomy with preoperative lumbar
spinal drainage: A single-surgeon experience of 365 patients among
3000 major cranial cases. Oper Neurosurg (Hagerstown). 20:E77–E82.
2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Montgomery SP, Moore B, Hampton SM, Macy
G, Li W and Bronshteyn YS: Optic nerve sheath point of care
ultrasound: Image acquisition. J Vis Exp. 2023.PubMed/NCBI View
Article : Google Scholar
|
|
6
|
Fernando SM, Tran A, Cheng W, Rochwerg B,
Taljaard M, Kyeremanteng K, English SW, Sekhon MS, Griesdale DEG,
Dowlatshahi D, et al: Diagnosis of elevated intracranial pressure
in critically ill adults: Systematic review and meta-analysis. BMJ.
366(l4225)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sekhon MS, Griesdale DE, Robba C,
McGlashan N, Needham E, Walland K, Shook AC, Smielewski P, Czosnyka
M, Gupta AK and Menon DK: Optic nerve sheath diameter on computed
tomography is correlated with simultaneously measured intracranial
pressure in patients with severe traumatic brain injury. Intensive
Care Med. 40:1267–1274. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Jimenez Restrepo JN, León OJ and Quevedo
Florez LA: Ocular ultrasonography: A useful instrument in patients
with trauma brain injury in emergency service. Emerg Med Int.
2019(9215853)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Aletreby W, Alharthy A, Brindley PG,
Kutsogiannis DJ, Faqihi F, Alzayer W, Balhahmar A, Soliman I,
Hamido H, Alqahtani SA, et al: Optic nerve sheath diameter
ultrasound for raised intracranial pressure: A literature review
and meta-analysis of its diagnostic accuracy. J Ultrasound Med.
41:585–595. 2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lee SH, Kim HS and Yun SJ: Optic nerve
sheath diameter measurement for predicting raised intracranial
pressure in adult patients with severe traumatic brain injury: A
meta-analysis. J Crit Care. 56:182–187. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Moher D, Shamseer L, Clarke M, Ghersi D,
Liberati A, Petticrew M, Shekelle P and Stewart LA: PRISMA-P Group.
Preferred reporting items for systematic review and meta-analysis
protocols (PRISMA-P) 2015 statement. Syst Rev. 4(1)2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zamora J, Abraira V, Muriel A, Khan K and
Coomarasamy A: Meta-DiSc: A software for meta-analysis of test
accuracy data. BMC Med Res Methodol. 6(31)2006.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Du J, Deng Y, Li H, Qiao S, Yu M, Xu Q and
Wang C: Ratio of optic nerve sheath diameter to eyeball transverse
diameter by ultrasound can predict intracranial hypertension in
traumatic brain injury patients: A prospective study. Neurocrit
Care. 32:478–485. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Altayar AS, Abouelela AZ, Abdelshafey EE,
Mohammed KSS, Hassan AA, Khattab MA, Alhabashy W, Gomaa W, Mohammed
AF and Umerani MS: Optic nerve sheath diameter by ultrasound is a
good screening tool for high intracranial pressure in traumatic
brain injury. Ir J Med Sci. 190:387–393. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Geeraerts T, Launey Y, Martin L, Pottecher
J, Vigué B, Duranteau J and Benhamou D: Ultrasonography of the
optic nerve sheath may be useful for detecting raised intracranial
pressure after severe brain injury. Intensive Care Med.
33:1704–1711. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Maissan IM, Dirven PJAC, Haitsma IK, Hoeks
SE, Gommers D and Stolker RJ: Ultrasonographic measured optic nerve
sheath diameter as an accurate and quick monitor for changes in
intracranial pressure. J Neurosurg. 123:743–747. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Soldatos T, Karakitsos D, Chatzimichail K,
Papathanasiou M, Gouliamos A and Karabinis A: Optic nerve
sonography in the diagnostic evaluation of adult brain injury. Crit
Care. 12(R67)2008.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Soliman I, Johnson GGRJ, Gillman LM,
Zeiler FA, Faqihi F, Aletreby WT, Balhamar A, Mahmood NN, Ahmad
Mumtaz S, Alharthy A, et al: New optic nerve sonography quality
criteria in the diagnostic evaluation of traumatic brain injury.
Crit Care Res Pract. 2018(3589762)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Strumwasser A, Kwan RO, Yeung L, Miraflor
E, Ereso A, Castro-Moure F, Patel A, Sadjadi J and Victorino GP:
Sonographic optic nerve sheath diameter as an estimate of
intracranial pressure in adult trauma. J Surg Res. 170:265–271.
2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Širanović M, Magdić Turković T, Gopčević
A, Kelečić M, Kovač N, Kovač J, Rode B and Vučić M: Comparison of
ultrasonographic measurement of optic nerve sheath diameter (ONSD)
versus direct measurement of intracranial pressure (ICP) in
traumatic brain injury patients. Signa Vitae. 6:33–35. 2011.
|
|
21
|
Robba C, Santori G, Czosnyka M, Corradi F,
Bragazzi N, Padayachy L, Taccone FS and Citerio G: Optic nerve
sheath diameter measured sonographically as non-invasive estimator
of intracranial pressure: A systematic review and meta-analysis.
Intensive Care Med. 44:1284–1294. 2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Montorfano L, Yu Q, Bordes SJ,
Sivanushanthan S, Rosenthal RJ and Montorfano M: Mean value of
B-mode optic nerve sheath diameter as an indicator of increased
intracranial pressure: A systematic review and meta-analysis.
Ultrasound J. 13(35)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hansen HC and Helmke K: Optic nerve sheath
responses to pressure variations. Intensive Care Med. 45:1840–1841.
2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Robba C, Santori G, Czosnyka M, Corradi F
and Citerio G: Optic nerve sheath diameter: The next steps.
Intensive Care Med. 45:1842–1843. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liao SF, Chen PJ, Chaou CH and Lee CH:
Top-cited publications on point-of-care ultrasound: The evolution
of research trends. Am J Emerg Med. 36:1429–1438. 2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wu XL, Wang JJ, Yuan DQ and Chen WT:
Ultrasound-guided radial artery catheterization at different sites:
A prospective and randomized study. Eur Rev Med Pharmacol Sci.
26:415–421. 2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Bhandari D, Udupi Bidkar P, Adinarayanan
S, Narmadhalakshmi K and Srinivasan S: Measurement of changes in
optic nerve sheath diameter using ultrasound and computed
tomography scan before and after the ventriculoperitoneal shunt
surgery in patients with hydrocephalus-A prospective observational
trial. Br J Neurosurg. 33:125–130. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Cho BI, Lee H, Shin H, Kim C, Choi HJ and
Kang BS: The prognostic value of optic nerve sheath
diameter/eyeball transverse diameter ratio in the neurological
outcomes of out-of-hospital cardiac arrest patients. Medicina
(Kaunas). 58(1233)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Aduayi OS, Asaleye CM, Adetiloye VA,
Komolafe EO and Aduayi VA: Optic nerve sonography: A noninvasive
means of detecting raised intracranial pressure in a
resource-limited setting. J Neurosci Rural Pract. 6:563–567.
2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gao Y, Li Q, Wu C, Liu S and Zhang M:
Diagnostic and prognostic value of the optic nerve sheath diameter
with respect to the intracranial pressure and neurological outcome
of patients following hemicraniectomy. BMC Neurol.
18(199)2018.PubMed/NCBI View Article : Google Scholar
|