Introduction
Cryptococcus, which comprises ~70 species and
genera, belongs to the Cryptococcaceae family and Fungi kingdom.
Currently, only Cryptococcus neoformans and Cryptococcus
gattii are known to cause diseases in humans (1). Cryptococcosis is a globally widespread
invasive fungal disease. Cryptococcal infections are uncommon in
individuals with normal immune function (2). The lungs and central nervous system
(CNS) are the most commonly affected areas by cryptococcal
infections (3). Approximately 5-10%
of patients with disseminated cryptococcal disease develop
cryptococcal osteomyelitis; however, there are few reports of
infection in the bone and joint areas and of cryptococcal arthritis
in the older adult population (3,4). To
the best of our knowledge, there are only nine reports of joint
infection due to cryptococcal infection (5). Additional clinical data indicate that
patients with compromised immunity (such as those with acquired
immunodeficiency syndrome) are highly susceptible to cryptococcal
infection, irrespective of sex and age (6,7).
However, cryptococcal lesions of the skeletal system are rare and
primarily manifest as localized swelling, pain and joint movement
disorders. Certain patients also exhibit systemic symptoms, such as
fever and chills (8). Imaging often
reveals local or multiple osteolytic lesions that extend to the
joints; some patients may also present with peripheral abscesses
and soft tissue mass formation (9).
The present study reported a case of knee joint infection caused by
C. neoformans in China.
Case report
A 56-year-old man was diagnosed with primary
myelofibrosis and severe anemia at the Hematology Hospital of the
Chinese Academy of Medical Sciences (Tianjin, China), in October
2021. In February 2023, the patient experienced coughing after
catching a cold. The inflammatory indicators of the patient
revealed high-sensitivity C-reactive protein (hs-CRP) levels of 46
mg/l↑ (normal range: 0-3 mg/l) and procalcitonin (PCT) levels of
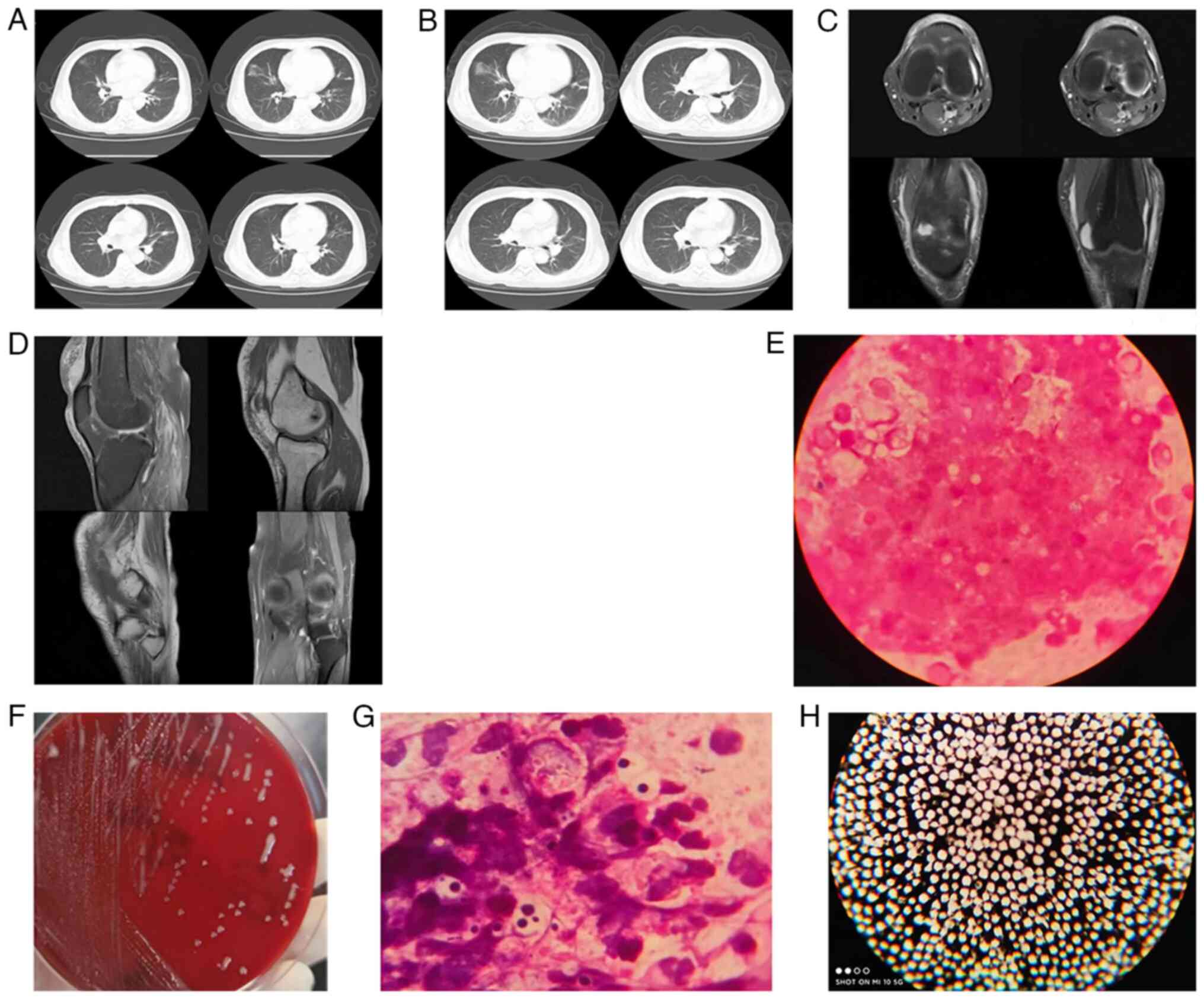
0.085 ng/ml↑ (normal range: 0.02-0.046 ng/l). A chest computed
tomography (CT) scan (Fig. 1A)
revealed inflammation in the middle lobe of the right lung with
cord shadows, interstitial changes in both lungs and micronodules
in the middle lobe of the right lung. Due to the patient's mild
cough symptoms, negligible phlegm and lack of cooperation with
bronchoalveolar lavage sample collection, the patient was treated
with an intravenous infusion of ceftazidime (1 g q8 h) and a
conventional dose of levofloxacin. After three days, the patient's
cough symptoms markedly improved. After 10 days, the patient was
discharged. However, due to regular blood transfusions for severe
anemia, intense swelling and pain in the left knee joint (new
symptoms), the patient was admitted to The General Medicine
Department of Baoding Hospital, Guang'anmen Hospital, China Academy
of Chinese Medical Sciences (Baoding, China) in April 2023.
Upon admission, the patient was conscious with a
moderate mental state and mild cough symptoms. The patient did not
have any recurrent fever, obvious dizziness, headache, nausea,
vomiting, acid reflux, heartburn, chest tightness, chest pain,
abdominal pain, diarrhea or lack of appetite. He had normal sleep
at night and normal bowel movements but had severe swelling and
pain in the left knee joint, limited mobility, and high skin
temperature at the swollen knee joint. The patient had no history
of hypertension or coronary heart disease and had not come into
contact with any birds, such as pigeons, or their droppings.
Admission examination revealed a body temperature of 36.2˚C, pulse
rate of 86 beats/min, breathing rate of 18 times/min and blood
pressure of 102/72 mm Hg, all within normal ranges. The patient had
an anemic appearance and exhibited thick respiratory sounds in both
lungs, audible moist rales, and no obvious murmurs in the
auscultation area of each valve. The abdomen was full without any
obvious tenderness, rebound pain or muscle tension. The liver was
not palpable under the ribs, the spleen was enlarged and percussion
pain was observed in the spleen. No edema was found in either of
the lower limbs; however, there were new symptoms of severe
swelling and pain in the left knee joint. Laboratory examination
results were as follows: White blood cell count,
5.96x109/l (normal range: 3.5-9.5x109/l);
neutrophil percentage, 58.7% (normal range: 40-75%); lymphocyte
percentage, 25.9% (normal range: 20-50%); monocyte percentage,
12.7% [elevated (↑), normal range: 3-11%]; red blood cell count,
1.99x1012/l [decreased (↓), normal range:
4.3-5.8x1012/l]; hemoglobin level, 5.6 g/l (↓, normal
range: 13.0-17.5 g/l); PCT level, 0.052 ng/ml (↑); hs-CRP level,
19.7 mg/l (↑); and human immunodeficiency virus (-). A chest CT
scan (Fig. 1B) revealed
inflammation in the middle lobe of the right lung with a cord
shadow (same as previously), interstitial changes in both lungs
(same as previously) and micronodules in the middle lobe of the
right lung (same as previously). Magnetic resonance imaging of the
left knee joint (Fig. 1C and
D) revealed the following: i) Joint
degeneration, ii) joint cavity and suprapatellar capsule effusion,
and iii) a left anterior superior patellar soft tissue cystic
lesion. Based on the patient's previous diagnosis, treatment and
clinical experience, and considering pneumonia and arthritis, an
intravenous infusion of ceftazidime (1 g q8 h) was administered,
with a conventional amount of levofloxacin. Simultaneously, for
diagnostic purposes, knee joint pus was discharged through needle
aspiration (closed suction, no rupture); a gray, white purulent
liquid was obtained, with a total discharge of ~20 ml. In April
2023, a sample of the knee joint pus was submitted for
culture-based diagnosis. The original smear on the same day showed
a moderate number of yeast-like spores (Fig. 1E). The growth status of the 48-h
blood plate is presented in Fig. 1F
and the ink staining result is displayed in Fig. 1H. After three days, the isolated
strain was identified as C. neoformans using DL-96FUNGUS
plate identification (DL: Zhuhai DL Biotech Co., Ltd.; equipment
model: DL-96II), with an identification rate of 99.8% (Table I). The identification rate is the
identification result of the instrument; it indicates the certainty
of bacterial identification. A capsular antigen test for C.
neoformans was sent to Shijiazhuang KingMed Diagnostics
Laboratory Co., Ltd. for examination and the result was positive.
To investigate the source of the infection, the microbiological
laboratory recommended submitting lower respiratory tract samples
and blood cultures for examination. The results of the sputum
smear, as presented in Fig. 1G, and
isolation identification were the same as those shown in Table I; however, the blood culture was
negative. The pathogenic microorganism was C. neoformans for
the knee joint and pulmonary infections. The first dose of
fluconazole was 400 mg/day, which was decreased to 200 mg/day from
the second day. After 10 days, knee joint symptoms had
substantially improved. After 12 days of hospitalization, the
patient was discharged and instructed to continue taking
fluconazole 200 mg/day orally for 4 months. After 23 days of
follow-up, the patient reported occasional coughing and phlegm,
improved knee joint symptoms and no swelling or pain. One month
later, the patient was re-examined at the hospital and was in a
good mental state, the knee joint was in good condition, no
swelling was detected, the patient did not report any pain, and no
symptoms of cough or phlegm were present. Therefore, the treatment
was deemed effective. Regarding the follow-up treatment effect and
recurrence, the microbiological laboratory will cooperate with the
clinician to monitor the case for 1 month. The patient continues to
undergo regular follow-ups (every other month) to screen for the
spread of infection in the blood, nervous system and other parts of
the body via examinations including physical examination and blood
culture. The patient's medication compliance will also be
monitored.
 | Table IAntimicrobial susceptibility results
of C. neoformans. |
Table I
Antimicrobial susceptibility results
of C. neoformans.
| Antimicrobial
agent | MIC, µg/ml | MIC breakpoints | Interpretive
categories |
|---|
| Fluorocytosine | ≤4 | S≤4; I=8-16;
R≥32 | S |
| Amphotericin | 2 | S≤2; R≥4 | S |
| Fluconazole | ≤8 | S≤8; SDD=16-32;
R≥64 | S |
|
Itraconazolea | 0.5 | S≤0.125;
SDD=0.25-0.5; R≥1 | SDD |
| Voriconazole | ≤0.125 | S≤1; S-DD=2; R≥4 | S |
Discussion
Cryptococcus comprises ~70 species and
genera. At present, only C. neoformans and C. gattii
are known to cause diseases in humans (1). Cryptococcal infection is uncommon in
individuals with normal immune function (2) and the lungs and CNS are the most
commonly affected areas (3).
Immunosuppressed patients may develop disseminated
Cryptococcus (6).
Approximately 5-10% of patients with disseminated cryptococcal
disease develop cryptococcal osteomyelitis, but there are few
reports of infection at the bone and joint sites and few reports of
cryptococcal arthritis in the elderly (4). There are also reports linking
cryptococcal arthritis with immune deficiency states (7). In addition, direct hematogenous
dissemination and lymphatic transmission are important sources of
joint infections (10).
The patient of the present study had no obvious
cause of knee joint infection with C. neoformans and the
source of the infection remains elusive. The infection may be
related to the patient's long-term use of immunosuppressants;
immunosuppressed patients may acquire disseminated C.
neoformans infections (6). The
chest CT scans consistently showed pulmonary inflammation without
improvement, suggesting that the lungs may have been the initial
source of infection. Bloodstream or lymphatic transmission may have
also occurred.
Cryptococcal infections of the joints most commonly
affect the knee joint and mainly manifest as local swelling, pain
and joint movement disorders. Certain patients also experience
systemic symptoms, such as fever and chills (2,4-6,8,11).
Imaging frequently reveals local or multiple osteolytic lesions
that extend to the joints and certain patients may present with
peripheral abscesses and soft tissue mass formation (8,9,12). The
present case of C. neoformans infection of the knee joint
exhibited similar symptoms. Clinical practice guidelines for the
management of cryptococcal disease suggest that non-meningeal,
non-pulmonary cryptococcosis should be treated with fluconazole
[400 mg (6 mg/kg) per day orally] for 6-12 months (11,13,14).
However, drug selection and duration of therapy also depend on
disease severity, response to therapy and host immune status, as
studies for specific body sites, except for the lung and CNS, are
unavailable (15). In the present
case, considering the patient's severe anemia, surgical treatment
was deemed unsuitable (16).
Therefore, the treatment applied was reasonable and effective. In
clinical practice, the specific medication regimen is generally
personalized and mainly determined based on the patient's basic
immune status and the presence of related complications (15). Simultaneously, antifungal drugs that
can eradicate infections for >6 months are necessary to prevent
recurrence (11,13).
In the present case study, the patient had a left
knee joint infection; given this infection, along with the
pulmonary imaging data and personal medication history, the patient
was considered to have a possible bloodstream or lymphatic
disseminated infection caused by immune suppression. Due to the
patient's severe anemia, surgical treatment was not recommended
(16). According to the Expert
Consultation on the Diagnosis and Treatment of Cryptococcal
Infection (14), the prognosis is
favorable after local puncture drainage and strict antifungal
treatment. We will continue to monitor the treatment efficacy and
recurrence in this patient.
In summary, the clinical and imaging manifestations
of cryptococcal infection in the joints lack specificity and are
difficult to differentiate from those of other diseases, such as
tumors and tuberculosis. Therefore, when clinically suspected,
puncture fluid or tissue pathogen testing should be performed as
early as possible to avoid misdiagnosis, delayed treatment or
spread to the CNS, which may result in serious consequences.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of supporting data
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
JM analyzed the study's findings, wrote the
manuscript and was the main responsible person for the final
approval of the pending version; YZ and JD were involved in data
acquisition and analysis; YZN participated in the writing of the
manuscript, critically reviewed its microbiological content and
made significant contributions to the conception of the study; ZQW
participated in data analysis and was responsible for conducting
appropriate investigation and resolution of any issues regarding
the completeness of any part of the manuscript, as well as jointly
deciding with JM and YZN on the final approval of the manuscript
for publication; JD and ZQW checked and confirmed the authenticity
of any original data reported in the manuscript. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient and his family for the publication of this case report and
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Li SS and Mody CH: Cryptococcus. Proc Am
Thorac Soc. 7:186–189. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ok Atılgan A, Özdemir BH, Kırnap M, Akdur
A, Yılmaz Akçay E, Akar Özkan E and Haberal M: Invasive fungal
infections in liver transplant recipients. Exper Clin Transplant.
12 (Suppl 1):S110–S116. 2014.PubMed/NCBI
|
|
3
|
Poenaru SM, Rofaiel R and
Hosseini-Moghaddam SM: Cryptococcus neoformans osteomyelitis
and intramuscular abscess in a liver transplant patient. BMJ Case
Rep. 2017(bcr2017221650)2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Gil LG, Foster BC, Neira QO, Palma CS,
Basualdo AJ, Heredia PC, Fernández VA, Juliet LC and Tapia A JC:
Cryptococcus neoformans arthritis in elderly adult: Case
report and review. Rev Chilena Infectol. 23:330–335.
2006.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
5
|
Li S, Xiao Z, Guo H, Yan L, Liao Y, Wang
W, Zhang J, Li J, Su L and Tang F: Cryptococcus neoformans
infection in hip joint after liver transplantation: One case report
and literature review. J Infect Chemother. 22:60–64. 2022.
|
|
6
|
Kozic H, Riggs K, Ringpfeil F and Lee JB:
Disseminated Cryptococcus neoformans after treatment with
infliximab for rheumatoid arthritis. J Am Acad Dermatol. 58 (Suppl
1):S95–S96. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Alobaidi D, Mahgoub AE, Bachuwa G and
Osterholzer D: Cryptococcus neoformans var. grubii septic
arthritis in an immunocompromised patient on haemodialysis with
history of splenectomy and sarcoidosis. BMJ Case Rep.
15(e248217)2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Geller DS, Pope JB, Thornhill BA and
Dorfman HD: Cryptococcal pyarthrosis and sarcoidosis. Skelet
Radiol. 38:721–727. 2009.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Stead KJ, Klugman KP, Painter ML and
Koornhof HJ: Septic arthritis due to Cryptococcus
neoformans. J Infect. 17:139–145. 1988.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bruno KM, Farhoomand L, Libman BS, Pappas
CN and Landry FJ: Cryptococcal arthritis, tendinitis,
tenosynovitis, and carpal tunnel syndrome: Report of a case and
review of the literature. Arthritis Rheum. 47:104–108.
2002.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Huang H, Pan J, Yang W, Lin J, Han Y, Lan
K, Zeng L, Liang G and Liu J: First case report of Cryptococcus
laurentii knee infection in a previously healthy patient. BMC
Infect Dis. 20(681)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yan T and Huoyan L: Experimental diagnosis
of left iliac joint infection with Cryptococcus neoformans.
Chin J Lab Med. 35:756–757. 2012.(In Chinese).
|
|
13
|
Johannsson B and Callaghan JJ: Prosthetic
hip infection due to Cryptococcus neoformans: Case report.
Diagn Microbiol Infect Dis. 64:76–79. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Editorial committee of the Chinese Journal
of Mycology. Expert consensus on the diagnosis and treatment of
cryptococcal infections. Chin J Mycol. 5:65–68, 86. 2010.(In
Chinese).
|
|
15
|
Clinical practice guidelines for the
management of cryptococcal diseases: 2010 American Society of
Infectious Diseases update. Translated by Zhou Y and Li G. Chin J
Infect Chemother. 10:161–166. 2010.(In Chinese).
|
|
16
|
Zhou HX, Ning GZ, Feng SQ, Jia HW, Liu Y,
Feng HY and Ruan WD: Cryptococcosis of lumbar vertebra in a patient
with rheumatoid arthritis and scleroderma: case report and
literature review. BMC Infect Dis. 13(128)2013.PubMed/NCBI View Article : Google Scholar
|